Multiple Chemical Sensitivity Syndrome: First Symptoms and Evolution of the Clinical Picture: Case-Control Study/Epidemiological Case-Control Study
Abstract
1. Introduction
- It is an acquired syndrome following documented environmental exposure that has objectively produced negative health effects.
- Symptoms affect multiple organs or systems and vary in magnitude depending on environmental stimuli.
- The symptoms are related to the levels of chemical agents directly, measurable levels and well below those considered toxicologically harmful.
- No evidence of organic damage is present.
2. Materials and Methods
2.1. Design
2.2. Scale 3 Questionnaire, QEESI—Initial Symptoms of MCS
2.3. Study Framework
2.4. Definition of the Study Population
2.5. Data Collection
2.6. Variables of Interest
- Demographic variables: age and sex.
- QEESI questionnaire variables, Scale 3: severity of symptoms (Table 2). Each item was evaluated on a numerical scale from 1 to 10 according to severity, with 1 representing the least severity and 10 the most severity, as in the QEESI questionnaire scale [31]. The item scores were divided into four intervals from least to most severe (Table A1 and Table A2).
- Variables of questionnaire Initial symptoms of MCS: in the group of cases, the variables related to the symptoms suffered at the onset of the disease were also studied (Table 2).
2.7. Statistical Analysis
2.8. Ethical Considerations
3. Results
3.1. Description of the Sample Population
3.2. Symptoms
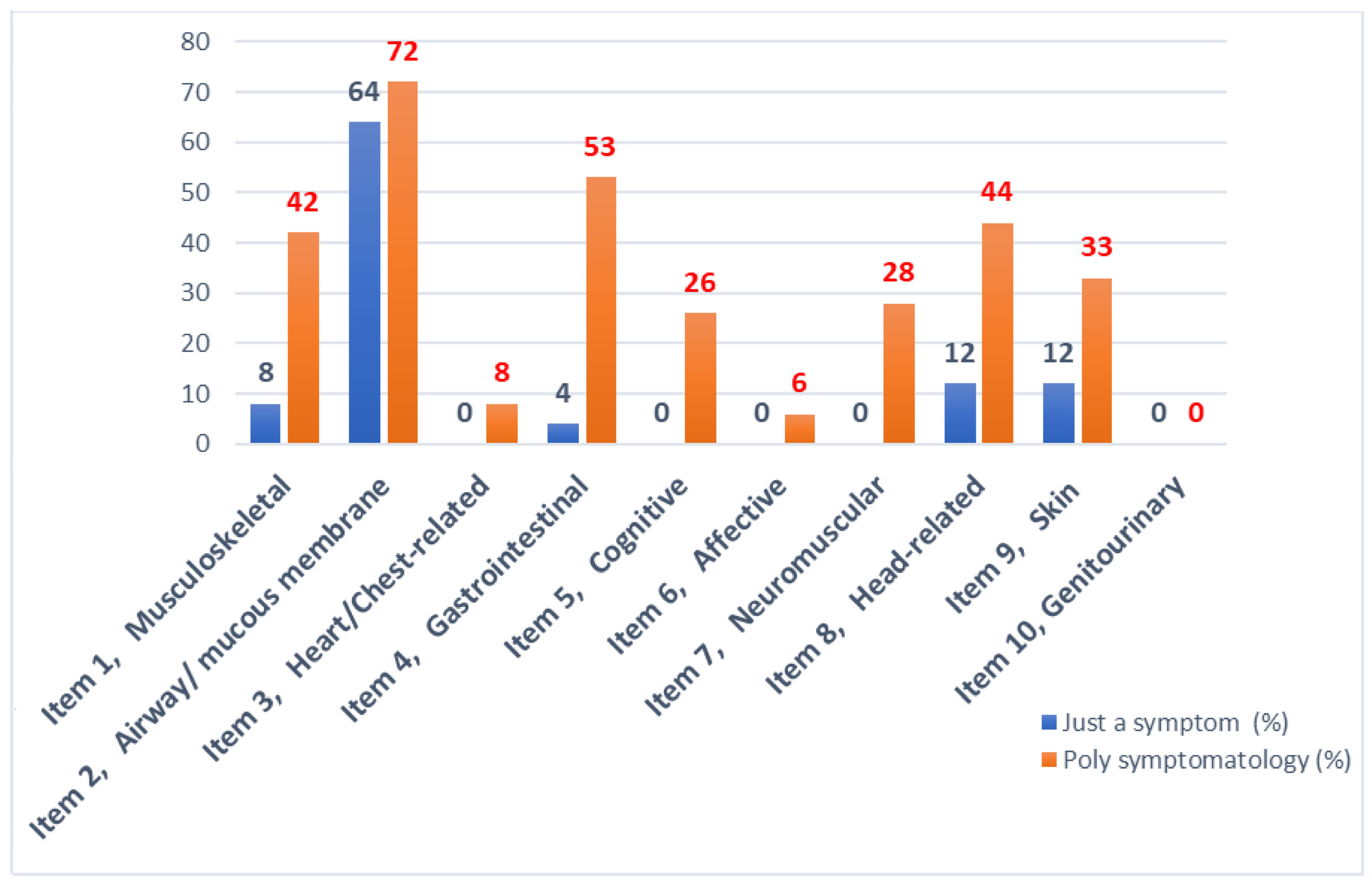
Initial Disease Profile
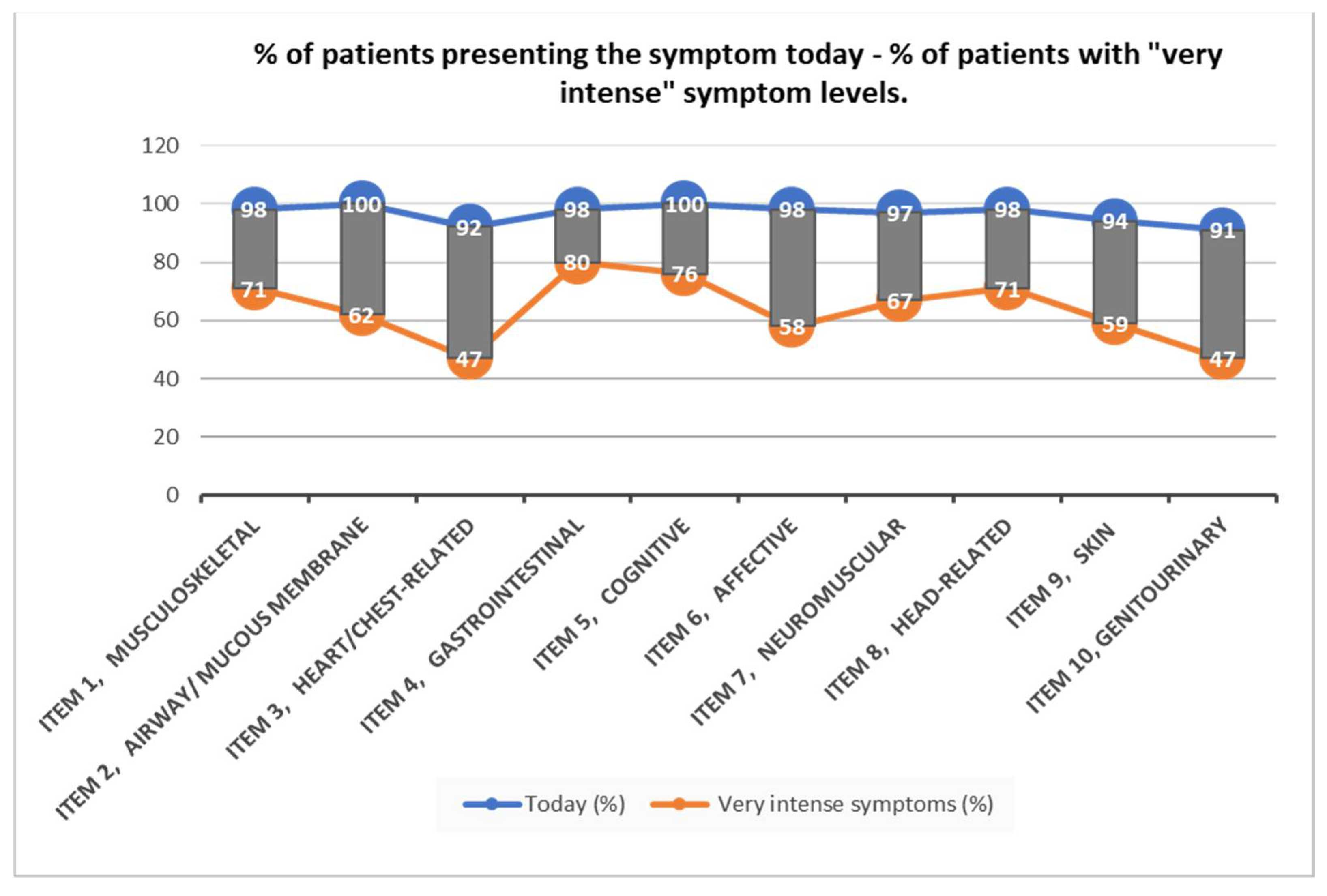
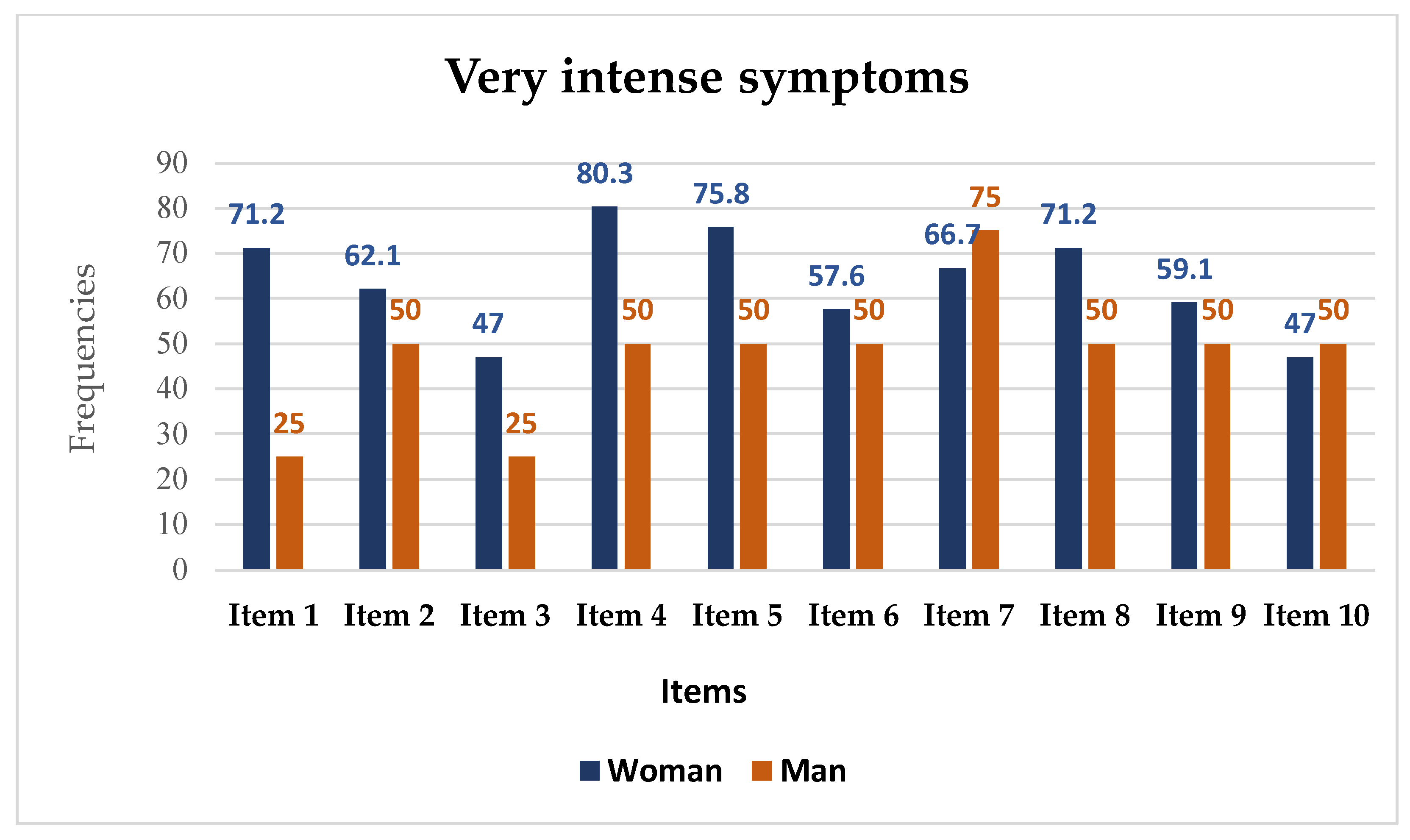
3.3. Severity of the Symptom
3.4. Bivariate Analysis
4. Discussion
5. Strength and Limitation of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| CASES | CONTROLS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom Intensity | Woman | 31–40 | 41–50 | 51–60 | ≥61 | Woman | 31–40 | 41–50 | 51–60 | ≥61 | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| 66 (100) | 7 (10.6) | 29 (43.9) | 20 (30.3) | 10 (15.2) | 132 (100) | 14 (10.6) | 58 (43.9) | 40 (30.3) | 20 (15.2) | ||
| Item 1 | No symptoms | 1 (1.5) | - | - | 1 (5.0) | - | 24 (18.2) | 3 (21.4) | 10 (17.2) | 7 (17.5) | 4 (20.0) |
| Mild symptomatology | 3 (4.5) | 1 (14.3) | 2 (6.9) | - | - | 38 (28.8) | 3 (21.4) | 19 (32.8) | 8 (20.0) | 8 (40.0) | |
| Moderate symptomatology | 15 (22.7) | 2 (28.6) | 7 (24.1) | 4 (20.0) | 2 (20.0) | 49 (37.1) | 6 (42.9) | 19 (32.8) | 18 (45.0) | 6 (30.0) | |
| Very intense symptoms | 47 (71.2) | 4 (57.1) | 20 (69.0) | 15 (75.0) | 8 (80.0) | 21 (15.9) | 2 (14.3) | 10 (17.2) | 7 (17.5) | 2 (10.0) | |
| Item 2 | No symptoms | - | - | - | - | - | 32 (24.2) | 3 (21.4) | 9 (15.5) | 13 (32.5) | 7 (35.0) |
| Mild symptomatology | 6 (9.1) | 1 (14.3) | 2 (6.9) | 1 (5.0) | 2 (20.0) | 45 (34.1) | 5 (35.7) | 25 (43.1) | 12 (30.0) | 3 (15.0) | |
| Moderate symptomatology | 19 (28.8) | 2 (28.6) | 8 (27.6) | 7 (35.0) | 2 (20.0) | 35 (26.5) | 3 (21.4) | 16 (27.6) | 10 (25.0) | 6 (30.0) | |
| Very intense symptoms | 41 (62.1) | 4 (57.1) | 19 (65.5) | 12 (60.0) | 6 (60.0) | 20 (15.2) | 3 (21.4) | 8 (13.8) | 5 (12.5) | 4 (20.0) | |
| Item 3 | No symptoms | 5 (7.6) | - | 2 (6.9) | 2 (10.0) | 1 (10.0) | 64 (48.5) | 5 (35.7) | 32 (55.2) | 18 (45.0) | 9 (45.0) |
| Mild symptomatology | 11 (16.7) | 2 (28.6) | 5 (17.2) | 3 (15.0) | 1 (10.0) | 39 (29.5) | 6 (42.9) | 17 (29.3) | 12 (30.0) | 4 (20.0) | |
| Moderate symptomatology | 19 (28.8) | 3 (42.9) | 8 (27.6) | 5 (25.0) | 3 (30.0) | 24 (18.2) | 1 (7.1) | 8 (13.8) | 8 (20.0) | 7 (35.0) | |
| Very intense symptoms | 31 (47.0) | 2 (28.6) | 14 (48.3) | 10 (50.0) | 5 (50.0) | 5 (3.8) | 2 (14.3) | 1 (1.7) | 2 (5.0) | - | |
| Item 4 | No symptoms | 1 (1.5) | - | 1 (3.4) | - | - | 33 (25.0) | 2 (14.3) | 18 (31.0) | 8 (20.0) | 5 (25.0) |
| Mild symptomatology | 4 (6.1) | - | 1 (3.4) | 2 (10.0) | 1 (10.0) | 43 (32.6) | 4 (28.6) | 19 (32.8) | 12 (30.0) | 8 (40.0) | |
| Moderate symptomatology | 8 (12.1) | 2 (28.6) | 3 (10.3) | 1 (5.0) | 2 (20.0) | 32 (24.2) | 4 (28.6) | 12 (20.7) | 11 (27.5) | 5 (25.0) | |
| Very intense symptoms | 53 (80.3) | 5 (71.4) | 24 (82.8) | 17 (85.0) | 7 (70.0) | 24 (18.2) | 4 (28.6) | 9 (15.5) | 9 (22.5) | 2 (10.0) | |
| Item 5 | No symptoms | - | - | - | - | - | 40 (30.3) | 3 (21.4) | 19 (32.8) | 9 (22.5) | 9 (45.0) |
| Mild symptomatology | 3 (4.5) | - | 1 (3.4) | 1 (5.0) | 1 (10.0) | 44 (33.3) | 6 (42.9) | 20 (34.5) | 14 (35.0) | 4 (20.0) | |
| Moderate symptomatology | 13 (19.7) | 2 (28.6) | 5 (17.2) | 5 (25.0) | 1 (10.0) | 36 (27.3) | 4 (28.6) | 13 (22.4) | 12 (30.0) | 7 (35.0) | |
| Very intense symptoms | 50 (75.8) | 5 (71.4) | 23 (79.3) | 14 (70.0) | 8 (80.0) | 12 (9.1) | 1 (7.1) | 6 (10.3) | 5 (12.5) | - | |
| Item 6 | No symptoms | 1 (1.5) | - | 1 (3.4) | - | - | 41 (31.1) | 5 (35.7) | 19 (32.8) | 10 (25.0) | 7 (35.0) |
| Mild symptomatology | 5 (7.6) | 2 (28.6) | - | 1 (5.0) | 2 (20.0) | 42 (31.8) | 4 (28.6) | 20 (34.5) | 12 (30.0) | 6 (30.0) | |
| Moderate symptomatology | 22 (33.3) | 2 (28.6) | 11 (37.9) | 7 (35.0) | 2 (20.0) | 28 (21.2) | 3 (21.4) | 6 (10.3) | 13 (32.5) | 6 (30.0) | |
| Very intense symptoms | 38 (57.6) | 3 (42.9) | 17 (58.6) | 12 (60.0) | 6 (60.0) | 21 (15.9) | 2 (14.3) | 13 (22.4) | 5 (12.5) | 1 (5.0) | |
| Item 7 | No symptoms | 2 (3.0) | 1 (14.3) | - | 1 (5.0) | - | 50 (37.9) | 5 (35.7) | 20 (34.5) | 16 (40.0) | 9 (45.0) |
| Mild symptomatology | 3 (4.5) | 1 (14.3) | 1 (3.4) | - | 1 (10.0) | 42 (31.8) | 5 (35.7) | 20 (34.5) | 13 (32.5) | 4 (20.0) | |
| Moderate symptomatology | 17 (25.8) | 3 (42.9) | 9 (31.0) | 3 (15.0) | 2 (20.0) | 28 (21.2) | 2 (14.3) | 10 (7.6) | 9 (6.8) | 7 (35.0) | |
| Very intense symptoms | 44 (66.7) | 2 (28.6) | 19 (65.5) | 16 (80.0) | 7 (70.0) | 12 (9.1) | 2 (14.3) | 8 (13.8) | 2 (5.0) | - | |
| Item 8 | No symptoms | 1 (1.5) | - | - | 1 (5.0) | - | 34 (25.8) | 2 (14.3) | 15 (25.9) | 13 (32.5) | 4 (20.0) |
| Mild symptomatology | 3 (4.5) | 1 (14.3) | 1 (3.4) | 1 (5.0) | - | 51 (38.6) | 6 (42.9) | 23 (39.7) | 13 (32.5) | 9 (45.0) | |
| Moderate symptomatology | 15 (22.7) | 1 (14.3) | 8 (27.6) | 3 (15.0) | 3 (30.0) | 32 (24.2) | 3 (21.4) | 12 (20.7) | 10 (25.0) | 7 (35.0) | |
| Very intense symptoms | 47 (71.2) | 5 (71.4) | 20 (69.0) | 15 (75.0) | 7 (70.0) | 15 (11.4) | 3 (21.4) | 8 (13.8) | 4 (10.0) | - | |
| Item 9 | No symptoms | 4 (6.1) | 1 (14.3) | - | 2 (10.0) | 1 (10.0) | 27 (20.5) | 2 (14.3) | 11 (19.0) | 6 (15.0) | 8 (40.0) |
| Mild symptomatology | 6 (9.1) | 2 (28.6) | 1 (3.4) | 2 (10.0) | 1 (10.0) | 44 (33.3) | 5 (35.7) | 22 (37.9) | 11 (27.5) | 6 (30.0) | |
| Moderate symptomatology | 17 (25.8) | 2 (28.6) | 5 (17.2) | 7 (35.0) | 3 (30.0) | 36 (27.3) | 3 (21.4) | 11 (19.0) | 17 (42.5) | 5 (25.0) | |
| Very intense symptoms | 39 (59.1) | 2 (28.6) | 23 (79.3) | 9 (45.0) | 5 (50.0) | 25 (18.9) | 4 (28.6) | 14 (24.1) | 6 (15.0) | 1 (5.0) | |
| Item 10 | No symptoms | 6 (9.1) | - | 1 (3.4) | 3 (15.0) | 2 (20.0) | 55 (41.7) | 5 (35.7) | 26 (44.8) | 15 (37.5) | 9 (45.0) |
| Mild symptomatology | 10 (15.2) | - | 4 (13.8) | 3 (15.0) | 3 (30.0) | 40 (30.3) | 3 (21.4) | 17 (29.3) | 14 (35.0) | 6 (30.0) | |
| Moderate symptomatology | 19 (28.8) | 4 (57.1) | 8 (27.6) | 5 (25.0) | 2 (20.0) | 26 (19.7) | 3 (21.4) | 11 (19.0) | 8 (20.0) | 4 (20.0) | |
| Very intense symptoms | 31 (47.0) | 3 (42.9) | 16 (55.2) | 9 (45.0) | 3 (30.0) | 11 (8.3) | 3 (21.4) | 4 (6.9) | 3 (7.5) | 1 (5.0) | |
| CASES | CONTROLS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom Intensity | Man | 31–40 | 41–50 | 51–60 | >61 | Man | 31–40 | 41–50 | 51–60 | >61 | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| 4 (100) | - | 2 (50.0) | - | n (%) | 8 (100) | - | 4 (50.0) | - | 4 (50.0) | ||
| Item 1 | No symptoms | - | - | - | - | - | 3 (37.5) | - | 2 (50.0) | - | 1 (25.0) |
| Mild symptomatology | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | 3 (37.5) | - | 2 (50.0) | - | 1 (25.0) | |
| Moderate symptomatology | 1 (25.0) | - | - | - | 1 (50.0) | 1 (12.5) | - | - | - | 1 (25.0) | |
| Very intense symptoms | 1 (25.0) | - | 1 (50.0) | - | - | 1 (12.5) | - | - | - | 1 (25.0) | |
| Item 2 | No symptoms | - | - | - | - | - | 3 (37.5) | - | 2 (50.0) | - | 1 (25.0) |
| Mild symptomatology | - | - | - | - | - | 2 (25.0) | - | 1 (25.0) | - | 1 (25.0) | |
| Moderate symptomatology | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | 3 (37.5) | - | 1 (25.0) | - | 2 (50.0) | |
| Very intense symptoms | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | - | - | - | - | - | |
| Item 3 | No symptoms | - | - | - | - | - | 5 (62.5) | - | 3 (75.0) | - | 2 (50.0) |
| Mild symptomatology | - | - | - | - | - | 1 (12.5) | - | 1 (25.0) | - | - | |
| Moderate symptomatology | 3 (75.0) | - | 1 (50.0) | - | 2 (100.0) | 2 (25.0) | - | - | - | 2 (50.0) | |
| Very intense symptoms | 1 (25.0) | - | 1 (50.0) | - | - | - | - | - | - | - | |
| Item 4 | No symptoms | - | - | - | - | - | 2 (25.0) | - | 1 (25.0) | - | 1 (25.0) |
| Mild symptomatology | - | - | - | - | - | 3 (37.5) | - | 2 (50.0) | - | 1 (25.0) | |
| Moderate symptomatology | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | - | - | - | - | - | |
| Very intense symptoms | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | 3 (37.5) | - | 1 (25.0) | - | 2 (50.0) | |
| Item 5 | No symptoms | - | - | - | - | - | 2 (25.0) | - | 1 (25.0) | - | 1 (25.0) |
| Mild symptomatology | 1 (25.0) | - | - | - | 1 (50.0) | 2 (25.0) | - | 1 (25.0) | - | 1 (25.0) | |
| Moderate symptomatology | 1 (25.0) | - | 1 (50.0) | - | - | 4 (50.0) | - | 2 (50.0) | - | 2 (50.0) | |
| Very intense symptoms | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | - | - | - | - | - | |
| Item 6 | No symptoms | - | - | - | - | - | 3 (37.5) | - | 2 (50.0) | - | 1 (25.0) |
| Mild symptomatology | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | 2 (25.0) | - | 1 (25.0) | - | 1 (25.0) | |
| Moderate symptomatology | - | - | - | - | - | 2 (25.0) | - | - | - | 2 (50.0) | |
| Very intense symptoms | 2 (50.0) | - | 1(50.0) | - | 1 (50.0) | 1 (12.5) | - | 1 (25.0) | - | - | |
| Item 7 | No symptoms | - | - | - | - | - | 4 (50.0) | - | 3 (75.0) | - | 1 (25.0) |
| Mild symptomatology | - | - | - | - | - | 1 (12.5) | - | - | - | 1 (25.0) | |
| Moderate symptomatology | 1 (25.0) | - | 1 (50.0) | - | - | 2 (25.0) | - | - | - | 2 (50.0) | |
| Very intense symptoms | 3 (75.0) | - | 1 (50.0) | - | 2 (100.0) | 1 (12.5) | - | 1 (25.0) | - | - | |
| Item 8 | No symptoms | 1 (25.0) | - | 1 (50.0) | - | - | 4 (50.0) | - | 3 (75.0) | - | 1 (25.0) |
| Mild symptomatology | - | - | - | - | - | 1 (12.5) | - | - | - | 1 (25.0) | |
| Moderate symptomatology | 1 (25.0) | - | 1 (50.0) | - | - | 1 (12.5) | - | - | - | 1 (25.0) | |
| Very intense symptoms | 2 (50.0) | - | - | - | 2 (100.0) | 2 (25.0) | - | 1 (25.0) | - | 1 (25.0) | |
| Item 9 | No symptoms | - | - | - | - | - | 2 (25.0) | - | 1 (25.0) | - | 1 (25.0) |
| Mild symptomatology | - | - | - | - | - | 3 (37.5) | - | 2 (50.0) | - | 1 (25.0) | |
| Moderate symptomatology | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | 3 (37.5) | - | 1 (25.0) | - | 2 (50.0) | |
| Very intense symptoms | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | - | - | - | - | - | |
| Item 10 | No symptoms | 1(25.0) | - | 1 (50.0) | - | - | 4 (50.0) | - | 3 (75.0) | - | 1 (25.0) |
| Mild symptomatology | 1 (25.0) | - | - | - | 1 (50.0) | - | - | - | - | - | |
| Moderate symptomatology | - | - | - | - | - | 4 (50.0) | - | 1 (25.0) | - | 3 (75.0) | |
| Very intense symptoms | 2 (50.0) | - | 1 (50.0) | - | 1 (50.0) | - | - | - | - | - | |
References
- Del Casale, A.; Ferracuti, S.; Mosca, A.; Pomes, L.M.; Fiaschè, F.; Bonanni, L.; Borro, M.; Gentile, G.; Martelletti, P.; Simmaco, M. Multiple Chemical Sensitivity Syndrome: A Principal Component Analysis of Symptoms. Int. J. Environ. Res. Public Health 2020, 17, 6551. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Lu, X.; Hiura, M.; Oda, M.; Miyazaki, W.; Katoh, T. Evaluation of Genetic Polymorphisms in Patients with Multiple Chemical Sensitivity. PLoS ONE 2013, 8, e73708. [Google Scholar] [CrossRef] [PubMed]
- Cullen, M.R. The Worker with Multiple Chemical Sensitivities: An Overview. Occup. Med. (Chic. III) 1987, 2, 655–661. [Google Scholar]
- Castillo, E.; Marqués, F. Síndrome de Sensibilidad Múltiple a Sustancias Químicas: Un Problema Ambiental Emergente. Rev. Salud Ambient. 2001, 1, 92–96. [Google Scholar]
- Yunus, M.B. Send Orders for Reprints to Reprints@benthamscience.Ae Editorial Review: An Update on Central Sensitivity Syndromes and the Issues of Nosology and Psychobiology. Curr. Rheumatol. Rev. 2015, 11, 70–85. [Google Scholar] [CrossRef]
- Fernández Solà, J. Síndromes de Sensibilización Central: Hacia La Estructuración de Un Concepto Multidisciplinar. Med. Clin. 2018, 151, 68–70. [Google Scholar] [CrossRef]
- Tran, M.T.D.; Arendt-Nielsen, L.; Kupers, R.; Elberling, J. Multiple Chemical Sensitivity: On the Scent of Central Sensitization. Int. J. Hyg. Environ. Health 2013, 216, 202–210. [Google Scholar] [CrossRef]
- Mosca, A.; Del Casale, A.; Borro, M.; Gentile, G.; Pomes, L.M.; Padovano, A.; Fiaschè, F.; Pinzone, V.; Rapinesi, C.; Zoppi, T.; et al. PON1 Polymorphisms Can Predict Generalized Anxiety and Depressed Mood in Patients with Multiple Chemical Sensitivity. Pers. Med. 2021, 3, 255–267. [Google Scholar] [CrossRef]
- Hojo, S.; Mizukoshi, A.; Azuma, K.; Okumura, J.; Ishikawa, S.; Miyata, M.; Mizuki, M.; Ogura, H.; Sakabe, K. Survey on Changes in Subjective Symptoms, Onset/Trigger Factors, Allergic Diseases, and Chemical Exposures in the Past Decade of Japanese Patients with Multiple Chemical Sensitivity. Int. J. Hyg. Environ. Health 2018, 221, 1085–1096. [Google Scholar] [CrossRef]
- Nogué, S.; Fernández-Solá, J.; Rovira, E.; Montori, E.; Fernández-Huerta, J.M.; Munné, P. Sensibilidad Química Múltiple: Análisis de 52 Casos. Med. Clin. 2007, 129, 96–99. [Google Scholar] [CrossRef]
- Dantoft, T.M.; Nordin, S.; Andersson, L.; Petersen, M.W.; Skovbjerg, S.; Jørgensen, T. Multiple Chemical Sensitivity Described in the Danish General Population: Cohort Characteristics and the Importance of Screening for Functional Somatic Syndrome Comorbidity-The DanFunD Study. PLoS ONE 2021, 16, e0246461. [Google Scholar] [CrossRef]
- Skovbjerg, S.; Christensen, K.B.; Ebstrup, J.F.; Linneberg, A.; Zachariae, R.; Elberling, J. Negative Affect Is Associated with Development and Persistence of Chemical Intolerance: A Prospective Population-Based Study. J. Psychosom. Res. 2015, 78, 509–514. [Google Scholar] [CrossRef]
- Berg, N.D.; Linneberg, A.; Dirksen, A.; Elberling, J. Prevalence of Self-Reported Symptoms and Consequences Related to Inhalation of Airborne Chemicals in a Danish General Population. Int. Arch. Occup. Environ. Health 2008, 81, 881–887. [Google Scholar] [CrossRef]
- Blanco, E.L.; Ferrando, J.P.; Enríquez, M.R.; Gento, L.A.; Coll, J.S.; Portell, M.R.P. Multiple Chemical Sensitivity: Clinical Evaluation of the Severity and Psychopathological Profile. Med. Clínica 2016, 146, 108–111. [Google Scholar] [CrossRef]
- Caress, S.M.; Steinemann, A.C. Prevalence of Multiple Chemical Sensitivities: A Population-Based Study in the Southeastern United States. Am. J. Public Health 2004, 94, 746–747. [Google Scholar] [CrossRef]
- Meggs, W.J.; Dunn, K.A.; Bloch, R.M.; Goodman, P.E.; Davidoff, A.L. Prevalence and Nature of Allergy and Chemical Sensitivity in a General Population. Arch. Environ. Health 1996, 51, 275–282. [Google Scholar] [CrossRef]
- Hojo, S.; Mizukoshi, A.; Azuma, K.; Okumura, J.; Mizuki, M.; Miyata, M. New Criteria for Multiple Chemical Sensitivity Based on the Quick Environmental Exposure and Sensitivity Inventory Developed in Response to Rapid Changes in Ongoing Chemical Exposures among Japanese. PLoS ONE 2019, 14, e0215144. [Google Scholar] [CrossRef]
- Palmer, R.F.; Jaén, C.R.; Perales, R.B.; Rincon, R.; Forster, J.N.; Miller, C.S. Three Questions for Identifying Chemically Intolerant Individuals in Clinical and Epidemiological Populations: The Brief Environmental Exposure and Sensitivity Inventory (BREESI). PLoS ONE 2020, 15, e0238296. [Google Scholar] [CrossRef]
- Katerndahl, D.A.; Bell, I.R.; Palmer, R.F.; Miller, C.S. Chemical Intolerance in Primary Care Settings: Prevalence, Comorbidity, and Outcomes. Ann. Fam. Med. 2012, 10, 357–365. [Google Scholar] [CrossRef]
- Azuma, K.; Uchiyama, I.; Tanigawa, M.; Bamba, I.; Azuma, M.; Takano, H.; Yoshikawa, T.; Sakabe, K. Association of Odor Thresholds and Responses in Cerebral Blood Flow of the Prefrontal Area during Olfactory Stimulation in Patients with Multiple Chemical Sensitivity. PLoS ONE 2016, 11, e0168006. [Google Scholar] [CrossRef]
- Azuma, K.; Uchiyama, I.; Katoh, T.; Ogata, H.; Arashidani, K.; Kunugita, N. Prevalence and Characteristics of Chemical Intolerance: A Japanese Population-Based Study. Arch. Environ. Occup. Health 2015, 70, 341–353. [Google Scholar] [CrossRef] [PubMed]
- Hausteiner, C.; Bornschein, S.; Hansen, J.; Zilker, T.; Förstl, H. Self-Reported Chemical Sensitivity in Germany: A Population-Based Survey. Int. J. Hyg. Environ. Health 2005, 208, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Información y Estadísticas Sanitarias 2020; Ministerio de Sanidad Consumo y Bienestar Social; Ministerio de la Presidencia Relaciones con las Cortes e Igualdad; Boletín Oficial del Estado. CIE 10 ES Clasificación Internacional de Enfermedades 10a. Revisión Modificación Clínica; Diagnósticos: Madrid, Spain, 2020; Volume I, ISBN 978-84-340-2592-9.
- Bartha, L.; Baumzweiger, W.; Buscher, D.S.; Callender, T.; Dahl, K.A.; Davidoff, A.; Donnay, A.; Edelson, S.B.; Elson, B.D.; Elliott, E.; et al. Multiple Chemical Sensitivity: A 1999 Consensus. Arch. Environ. Health 1999, 54, 147–149. [Google Scholar] [CrossRef]
- Palmer, R.F.; Walker, T.; Kattari, D.; Rincon, R.; Perales, R.B.; Jaén, C.R.; Grimes, C.; Sundblad, D.R.; Miller, C.S. Validation of a Brief Screening Instrument for Chemical Intolerance in a Large U.S. National Sample. Int. J. Environ. Res. Public Health 2021, 18, 8714. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.S.; Prihoda, T.J. The Environmental Exposure and Sensitivity Inventory (EESI): A Standardized Approach for Measuring Chemical Intolerances for Research and Clinical Applications. Toxicol. Ind. Health 1999, 15, 370–385. [Google Scholar] [CrossRef]
- Hojo, S.; Sakabe, K.; Ishikawa, S.; Miyata, M.; Kumano, H. Evaluation of Subjective Symptoms of Japanese Patients with Multiple Chemical Sensitivity Using QEESI. Environ. Health Prev. Med. 2009, 14, 267–275. [Google Scholar] [CrossRef][Green Version]
- García-Sierra, R.; Álvarez-Moleiro, M. Evaluation of Suffering in Individuals with Multiple Chemical Sensitivity. Clin. Salud 2014, 25, 95–103. [Google Scholar] [CrossRef]
- Jeong, I.; Kim, I.; Park, H.J.; Roh, J.; Park, J.W.; Lee, J.H. Allergic Diseases and Multiple Chemical Sensitivity in Korean Adults. Allergy Asthma Immunol. Res. 2014, 6, 409–414. [Google Scholar] [CrossRef]
- Skovbjerg, S.; Berg, N.D.; Elberling, J.; Christensen, K.B. Evaluation of the Quick Environmental Exposure and Sensitivity Inventory in a Danish Population. J. Environ. Public Health 2012, 2012, 304314. [Google Scholar] [CrossRef]
- Mena, G.; Sequera, V.G.; Nogué-Xarau, S.; Ríos, J.; Bertran, M.J.; Trilla, A. Traducción y Adaptación Transcultural Del Cuestionario Quick Environmental Exposure and Sensitivity Inventory a La Población Española. Med. Clin. 2013, 140, 302–304. [Google Scholar] [CrossRef]
- Hojo, S.; Ishikawa, S.; Kumano, H.; Miyata, M.; Sakabe, K. Clinical Characteristics of Physician-Diagnosed Patients with Multiple Chemical Sensitivity in Japan. Int. J. Hyg. Environ. Health 2008, 211, 682–689. [Google Scholar] [CrossRef]
- Caress, S.M.; Steinemann, A.C. A Review of a Two-Phase Population Study of Multiple Chemical Sensitives. Environ. Health Perspect. 2003, 111, 1490–1497. [Google Scholar] [CrossRef]
- Vuokko, A.; Karvala, K.; Lampi, J.; Keski-Nisula, L.; Pasanen, M.; Voutilainen, R.; Pekkanen, J.; Sainio, M. Environmental Intolerance, Symptoms and Disability among Fertile-Aged Women. Int. J. Environ. Res. Public Health 2018, 15, 293. [Google Scholar] [CrossRef]
- Georgellis, A.; Lindelöf, B.; Lundin, A.; Arnetz, B.; Hillert, L. Multiple Chemical Sensitivity in Male Painters; a Controlled Provocation Study. Int. J. Hyg. Environ. Health 2003, 206, 531–538. [Google Scholar] [CrossRef]
- Damiani, G.; Alessandrini, M.; Caccamo, D.; Cormano, A.; Guzzi, G.; Mazzatenta, A.; Micarelli, A.; Migliore, A.; Piroli, A.; Bianca, M.; et al. Italian Expert Consensus on Clinical and Therapeutic Management of Multiple Chemical Sensitivity (Mcs). Int. J. Environ. Res. Public Health 2021, 18, 11294. [Google Scholar] [CrossRef]
- Palmieri, B.; Corazzari, V.; Vadala, M.; Vallelunga, A.; Morales-Medina, J.C.; Iannitti, T. The Role of Sensory and Olfactory Pathways in Multiple Chemical Sensitivity. Rev. Environ. Health 2021, 36, 319–326. [Google Scholar] [CrossRef]
- Pérez, A.O. «Sensibilidad a Múltiples Compuestos», Una Enfermedad Comúnmente Inadvertida. Med. Clin. 2005, 125, 257–262. [Google Scholar] [CrossRef]
- Ayza, M. Sensibilidad Química Múltiple y Trabajo, Descripción de Un Caso Sospechoso. Revista de la Asociación Española de Especialistas en Medicina del Trabajo 2017, 26, 271–274. [Google Scholar]
- Gibson, P.R. Life Indicators, Illness Characteristics, and Psychosocial Concomitants of Self-Reported Multiple Chemical Sensitivity: A Two-Year Longitudinal Study. J. Nurs. Educ. Pract. 2014, 4, 204–216. [Google Scholar] [CrossRef]
- Gibson, P.R.; Vogel, V.M. Sickness-Related Dysfunction in Persons with Self-Reported Multiple Chemical Sensitivity at Four Levels of Severity. J. Clin. Nurs. 2009, 18, 72–81. [Google Scholar] [CrossRef]
- Bioética, R.C. De Annual Congress of the Austrian and German Societies of Hematology and Oncology. Vienna, October 6–9, 1985. Blut 1985, 51, 145–239. [Google Scholar] [CrossRef]
- Estado, J.D.E.L. Ley Orgánica, de 13 de diciembre, de Protección de Datos de Carácter Personal. Boletín Oficial del Estado 1999, 14, 43088–43099. [Google Scholar]
- Samper, M.B. Ley Orgánica 3/2018, de 5 de diciembre, De Protección De Datos Personales Y Garantía De Los Derechos Digitales. Protección datos Pers. 2020, 145–252. [Google Scholar] [CrossRef]
- Genuis, S.J. Sensitivity-Related Illness: The Escalating Pandemic of Allergy, Food Intolerance and Chemical Sensitivity. Sci. Total Environ. 2010, 408, 6047–6061. [Google Scholar] [CrossRef]
- Storino, V.; Muñoz-Ortiz, J.; Villabona-Martinez, V.; Villamizar-Sanjuán, J.D.; Rojas-Carabali, W.; De-la-Torre, A. An Unusual Case of Multiple Food Allergies Comorbid with Multiple Chemical Sensitivity: A Case Report. J. Asthma Allergy 2021, 14, 317–323. [Google Scholar] [CrossRef]
- de Luca, C.; Raskovic, D.; Pacifico, V.; Thai, J.C.S.; Korkina, L. The Search for Reliable Biomarkers of Disease in Multiple Chemical Sensitivity and Other Environmental Intolerances. Int. J. Environ. Res. Public Health 2011, 8, 2770–2797. [Google Scholar] [CrossRef]
- Alobid, I.; Nogué, S.; Izquierdo-Dominguez, A.; Centellas, S.; Bernal-Sprekelsen, M.; Mullol, J. Multiple Chemical Sensitivity Worsens Quality of Life and Cognitive and Sensorial Features of Sense of Smell. Eur. Arch. Oto-Rhino-Laryngol. 2014, 271, 3203–3208. [Google Scholar] [CrossRef]
- Andersson, L.; Johansson, Å.; Millqvist, E.; Nordin, S.; Bende, M. Prevalence and Risk Factors for Chemical Sensitivity and Sensory Hyperreactivity in Teenagers. Int. J. Hyg. Environ. Health 2008, 211, 690–697. [Google Scholar] [CrossRef]
- Österberg, K.; Persson, R.; Karlson, B.; Ørbæk, P. Annoyance and Performance of Three Environmentally Intolerant Groups during Experimental Challenge with Chemical Odors. Scand. J. Work. Environ. Health 2004, 30, 486–496. [Google Scholar] [CrossRef]
- Österberg, K.; Ørbæk, P.; Karlson, B.; Åkesson, B.; Bergendorf, U. Annoyance and Performance during the Experimental Chemical Challenge of Subjects with Multiple Chemical Sensitivity. Scand. J. Work. Environ. Health 2003, 29, 40–50. [Google Scholar] [CrossRef]
- Baldwin, C.M.; Bell, I.R. Increased Cardiopulmonary Disease Risk in a Community-Based Sample with Chemical Odor Intolerance: Implications for Women’s Health and Health-Care Utilization. Arch. Environ. Health 1998, 53, 347–353. [Google Scholar] [CrossRef]
- McFetridge-Durdle, J.A.; Routledge, F.S.; Sampalli, T.; Fox, R.; Livingston, H.; Adams, B. Hemodynamic Response to Postural Shift in Women with Multiple Chemical Sensitivities. Biol. Res. Nurs. 2009, 10, 267–273. [Google Scholar] [CrossRef]
- Skovbjerg, S.; Rasmussen, A.; Zachariae, R.; Schmidt, L.; Lund, R.; Elberling, J. The Association between Idiopathic Environmental Intolerance and Psychological Distress, and the Influence of Social Support and Recent Major Life Events. Environ. Health Prev. Med. 2012, 17, 2–9. [Google Scholar] [CrossRef][Green Version]
- Johansson, Å.; Brämerson, A.; Millqvist, E.; Nordin, S.; Bende, M. Prevalence and Risk Factors for Self-Reported Odour Intolerance: The Skövde Population-Based Study. Int. Arch. Occup. Environ. Health 2005, 78, 559–564. [Google Scholar] [CrossRef] [PubMed]
| Criteria for Diagnosis of MCS [24] | |
|---|---|
| 1. | The symptoms are reproducible with (repeated chemical) exposure. |
| 2. | The condition is chronic. |
| 3. | Low levels of exposure (lower than previously or commonly tolerated) result in manifestations of the syndrome. |
| 4. | The symptoms improve or resolve when the incitants are removed. |
| 5. | Responses occur to multiple chemically unrelated substances. |
| 6. | Symptoms involve multiple organ systems. |
| Scale 3, QEESI Questionnaire (Symptoms) | |
|---|---|
| Item | Definition |
| Item 1 | Problems with your muscles or joint, such as pain, aching, cramping, stiffness or weakness |
| Item 2 | Problems with burning or irritation of your eyes, or problems with your airway or breathing, such as feeling short of breath, coughing or having a lot of mucus, post-nasal drainage or respiratory infections |
| Item 3 | Problems with your heart or chest, such as a fast or irregular heart rate, skipped beats, your heart pounding or chest discomfort |
| Item 4 | Problems with your stomach or digestive tract, such as abdominal pain or cramping, abdominal swelling or bloating, nausea, diarrhea or constipation |
| Item 5 | Problems with your ability to think, such as difficulty concentrating or remembering things, feeling spacey or having trouble making decisions |
| Item 6 | Problems with your mood such as feeling tense or nervous, irritable, depressed, having spells of crying or rage or loss of motivation to do things that used to interest you |
| Item 7 | Problems with balance or coordination, with numbness or tingling in your extremities or with focusing your eyes |
| Item 8 | Problems with your head, such as headaches or a feeling of pressure or fullness in your face or head |
| Item 9 | Problems with your skin, such as a rash, hives or dry skin |
| Item 10 | Problems with your urinary tract or genitals, such as pelvic pain or frequent or urgent urination (For women: or discomfort or other problems with your menstrual period) |
| Initial Symptoms of MCS | |
| Question | Definition |
| 1 | At what age did the symptoms appear? |
| 2 | In what intensity? |
| 3 | What were the symptoms? |
| Inclusion Criteria | |
|---|---|
| Cases | Controls |
| People of both sexes | People of both sexes |
| ≥18 years | ≥18 years |
| Patients with diagnosed MCS | Patients without diagnosed MCS |
| With explicit informed consent of the person | With explicit informed consent of the person |
| Cases n = 70 | Controls n = 140 | |||
|---|---|---|---|---|
| Gender n (%) n (%) | ||||
| Females | 66 (94.3) | 132 (94.3) | ||
| Males | 4 (5.7) | 8 (5.7) | ||
| Median Age (Years) ± SD | 51.01 ± 8.98 | 51.03 ± 9.07 | ||
| Age (years) grouped n (%) n (%) | ||||
| 31–40 | 7 (10.0) | 14 (10.0) | ||
| 41–50 | 31 (44.3) | 62 (44.3) | ||
| 51–60 | 20 (28.6) | 40 (28.6) | ||
| ≥61 | 12 (17.1) | 24 (17.1) | ||
| Females n = 66 | Males n = 4 | Females n = 132 | Males n = 8 | |
| Median Age (Years) ± SD | 50.67 ± 8.76 | 56.75 ± 12.12 | 50.64 ± 8.78 | 57.50 ± 11.89 |
| Age (years) grouped n (%) n (%) | ||||
| 31–40 | 7 (10.6) | 0 | 14 (10.6) | 0 |
| 41–50 | 29 (43.9) | 2 (50.0) | 58 (43.9) | 4 (50.0) |
| 51–60 | 20 (30.3) | 0 | 40 (30.3) | 0 |
| ≥61 | 10 (15.2) | 2 (50.0) | 20 (15.2) | 4 (50.0) |
| Scale 3, QEESI | ||||
| Median (Q1–Q3) | 77.0 (65.0–89.0) | 65.5 (43.0–80.0) | 27.0 (14.0–47.0) | 15.0 (5.7–60.2) |
| Woman | Total | 0–10 Years | 11–20 Years | 21–30 Years | 31–40 Years | 41–50 Years | 51–60 Years | ≥61 Years |
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| 61 (100%) | 2 (3.3%) | 8 (13.1%) | 11 (18.0%) | 20 (32.8%) | 16 (26.2%) | 4 (6.6%) | 0 | |
| Item 1 | 17 (27.9) | 1 (50.0) | 1 (12.5) | 5 (45.5) | 5 (25.0) | 4 (25.0) | 1 (25.0) | 0 |
| Item 2 | 42 (68.9) | 0 | 5 (62.5) | 8 (72.7) | 15 (75.0) | 11 (68.8) | 3 (75.0) | 0 |
| Item 3 | 3 (4.9) | 0 | 0 | 1 (9.1) | 2 (10.0) | 0 | 0 | 0 |
| Item 4 | 20 (32.8) | 1 (50.0) | 2 (25.0) | 5 (45.5) | 7 (35.0) | 3 (18.8) | 2 (50.0) | |
| Item 5 | 9 (14.8) | 0 | 1 (12.5) | 4 (36.4) | 1 (5.0) | 3 (18.8) | 0 | 0 |
| Item 6 | 2 (3.3) | 0 | 0 | 1 (9.1) | 1 (5.0) | 0 | 0 | 0 |
| Item 7 | 10 (16.4) | 0 | 1 (12.5) | 2 (18.2) | 3 (15.0) | 4 (25.0) | 0 | 0 |
| Item 8 | 19 (31.1) | 1 (50.0) | 2 (25.0) | 3 (27.3) | 8 (40.0) | 4 (25.0) | 1 (25.0) | 0 |
| Item 9 | 15 (24.6) | 1 (50.0) | 3 (37.5) | 5 (45.5) | 3 (15.0) | 3 (18.8) | 0 | 0 |
| Item 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Single symptom | 25 (41.0) | 1 (50.0) | 3 (37.5) | 2(18.2) | 10 (50.0) | 7 (43.8) | 2 (50.0) | 0 |
| Polysymptomatic | 36 (59.0) | 1 (50.0) | 5 (62.5) | 9 (81.8) | 10 (50.0) | 9 (56.2) | 2 (50.0) | 0 |
| Total | 0–10 | 11–20 | 21–30 | 31–40 | 41–50 | 51–60 | ≥61 | |
| Man | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| 4 (100%) | 0 | 0 | 1 (25%) | 0 | 1 (25%) | 1 (25%) | 1 (25%) | |
| Item 1 | 2 (50.0) | 0 | 0 | 0 | 0 | 0 | 1 (100) | 1 (100) |
| Item 2 | 2 (50.0) | 0 | 0 | 0 | 0 | 1 (100) | 1 (100) | 0 |
| Item 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Item 4 | 2 (50.0) | 0 | 0 | 0 | 0 | 0 | 1 (100) | 1 (100) |
| Item 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Item 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Item 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Item 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Item 9 | 1 (25.0) | 0 | 0 | 1 (100) | 0 | 0 | 0 | 0 |
| Item 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Single symptom | 25 (50.0) | 0 | 0 | 1 (100) | 0 | 1(100) | 0 | 0 |
| Polysymptomatic | 2 (50.0) | 0 | 0 | 0 | 0 | 0 | 1 (100) | 1 (100) |
| Women | Item | Symptom Scale 3 | Cases 66 (%) | Controls 132 (%) | OR (CI 95%) | p Value |
|---|---|---|---|---|---|---|
| Totals | Item 1 | Musculoskeletal | 71.2% | 15.9% | 13.07 (6.44–26.54) | 0.000 |
| Item 2 | Airway/mucous membrane | 62.1% | 15.2% | 9.18 (4.61–18.27) | 0.000 | |
| Item 3 | Heart/Chest-related | 47% | 3.8% | 22.49 (8.14–62.13) | 0.000 | |
| Item 4 | Gastrointestinal | 80.3% | 18.2% | 18.34 (8.66–38.86) | 0.000 | |
| Item 5 | Cognitive | 75.8% | 9.1% | 31.25 (13.79–70.80) | 0.000 | |
| Item 6 | Affective | 57.6% | 15.9% | 7.17 (3.65–14.09) | 0.000 | |
| Item 7 | Neuromuscular | 66.7% | 9.1% | 20.00 (9.13–43.78) | 0.000 | |
| Item 8 | Head-related | 71.2% | 11.4% | 19.29 (9.05–41.12) | 0.000 | |
| Item 9 | Skin | 59.1% | 18.9% | 6.18 (3.20–11.91) | 0.000 | |
| Item 10 | Genitourinary | 47% | 8.3% | 9.74 (4.44–21.33) | 0.000 | |
| 31–40 years | Item 5 | Cognitive | 71.40% | 7.1% | 32.50 (2.38–443.14) | 0.002 |
| 41–50 years | Item 1 | Musculoskeletal | 69% | 17.2% | 10.66 (3.76–30.20) | 0.000 |
| Item 2 | Airway/mucous membrane | 65.5% | 13.8% | 11.87 (4.07–34.59) | 0.000 | |
| Item 3 | Heart/Chest-related | 48.3% | 1.7% | 53.20 (6.46–437.48) | 0.000 | |
| Item 4 | Gastrointestinal | 82.80% | 15.5% | 26.13 (7.89–86.53) | 0.000 | |
| Item 5 | Cognitive | 79.3% | 10.3% | 33.22 (9.67–114.05) | 0.000 | |
| Item 7 | Neuromuscular | 65.5% | 13.8% | 11.87 (4.07–34.59) | 0.000 | |
| Item 8 | Head-related | 69% | 13.8% | 13.88 (4.69–41.07) | 0.000 | |
| Item 9 | Skin | 79.30% | 24.1% | 12.04 (4.08–35.51) | 0.000 | |
| Item 10 | Genitourinary | 55.2% | 6.9% | 16.61 (4.75–58.10) | 0.000 | |
| 51–60 years | Item 1 | Musculoskeletal | 75% | 17.5% | 14.14 (3.85–51.88) | 0.000 |
| Item 2 | Airway/mucous membrane | 60% | 12.5% | 10.50 (2.87–38.35) | 0.000 | |
| Item 3 | Heart/Chest-related | 50% | 5% | 19.00 (3.57–100.96) | 0.000 | |
| Item 4 | Gastrointestinal | 85% | 22.5% | 19.51 (4.65–81.91) | 0.000 | |
| Item 5 | Cognitive | 70% | 12.5% | 16.33 (4.28–62.31) | 0.000 | |
| Item 6 | Affective | 60% | 12.5% | 10.50 (2.87–38.35) | 0.000 | |
| Item 7 | Neuromuscular | 80% | 5% | 76.00 (12.62–457.51) | 0.000 | |
| Item 8 | Head-related | 75% | 10% | 27.00 (6.35–114.66) | 0.000 | |
| Item 10 | Genitourinary | 45% | 7.5% | 10.09 (2.32–43.88) | 0.001 | |
| ≥61 years | Item 1 | Musculoskeletal | 80% | 10% | 36.00 (4.28–302.80) | 0.000 |
| Item 4 | Gastrointestinal | 70% | 10% | 21.00 (2.86–153.75) | 0.001 | |
| Item 6 | Affective | 60% | 5% | 28.50 (2.64–306.63) | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fares-Medina, S.; Díaz-Caro, I.; García-Montes, R.; Corral-Liria, I.; García-Gómez-Heras, S. Multiple Chemical Sensitivity Syndrome: First Symptoms and Evolution of the Clinical Picture: Case-Control Study/Epidemiological Case-Control Study. Int. J. Environ. Res. Public Health 2022, 19, 15891. https://doi.org/10.3390/ijerph192315891
Fares-Medina S, Díaz-Caro I, García-Montes R, Corral-Liria I, García-Gómez-Heras S. Multiple Chemical Sensitivity Syndrome: First Symptoms and Evolution of the Clinical Picture: Case-Control Study/Epidemiological Case-Control Study. International Journal of Environmental Research and Public Health. 2022; 19(23):15891. https://doi.org/10.3390/ijerph192315891
Chicago/Turabian StyleFares-Medina, Sandra, Isabel Díaz-Caro, Rebeca García-Montes, Inmaculada Corral-Liria, and Soledad García-Gómez-Heras. 2022. "Multiple Chemical Sensitivity Syndrome: First Symptoms and Evolution of the Clinical Picture: Case-Control Study/Epidemiological Case-Control Study" International Journal of Environmental Research and Public Health 19, no. 23: 15891. https://doi.org/10.3390/ijerph192315891
APA StyleFares-Medina, S., Díaz-Caro, I., García-Montes, R., Corral-Liria, I., & García-Gómez-Heras, S. (2022). Multiple Chemical Sensitivity Syndrome: First Symptoms and Evolution of the Clinical Picture: Case-Control Study/Epidemiological Case-Control Study. International Journal of Environmental Research and Public Health, 19(23), 15891. https://doi.org/10.3390/ijerph192315891






