A Reliability of Active and Passive Knee Joint Position Sense Assessment Using the Luna EMG Rehabilitation Robot
Abstract
1. Introduction
- -
- The assessment of knee JPS in active and passive mode using a new device is sufficiently reliable for clinical practice;
- -
- The assessment on only one side (most often the dominant side) and considering the results as equal to both limbs is correct, or whether proprioception on the dominant and non-dominant side does not work identically and both limbs should always be tested.
2. Materials and Methods
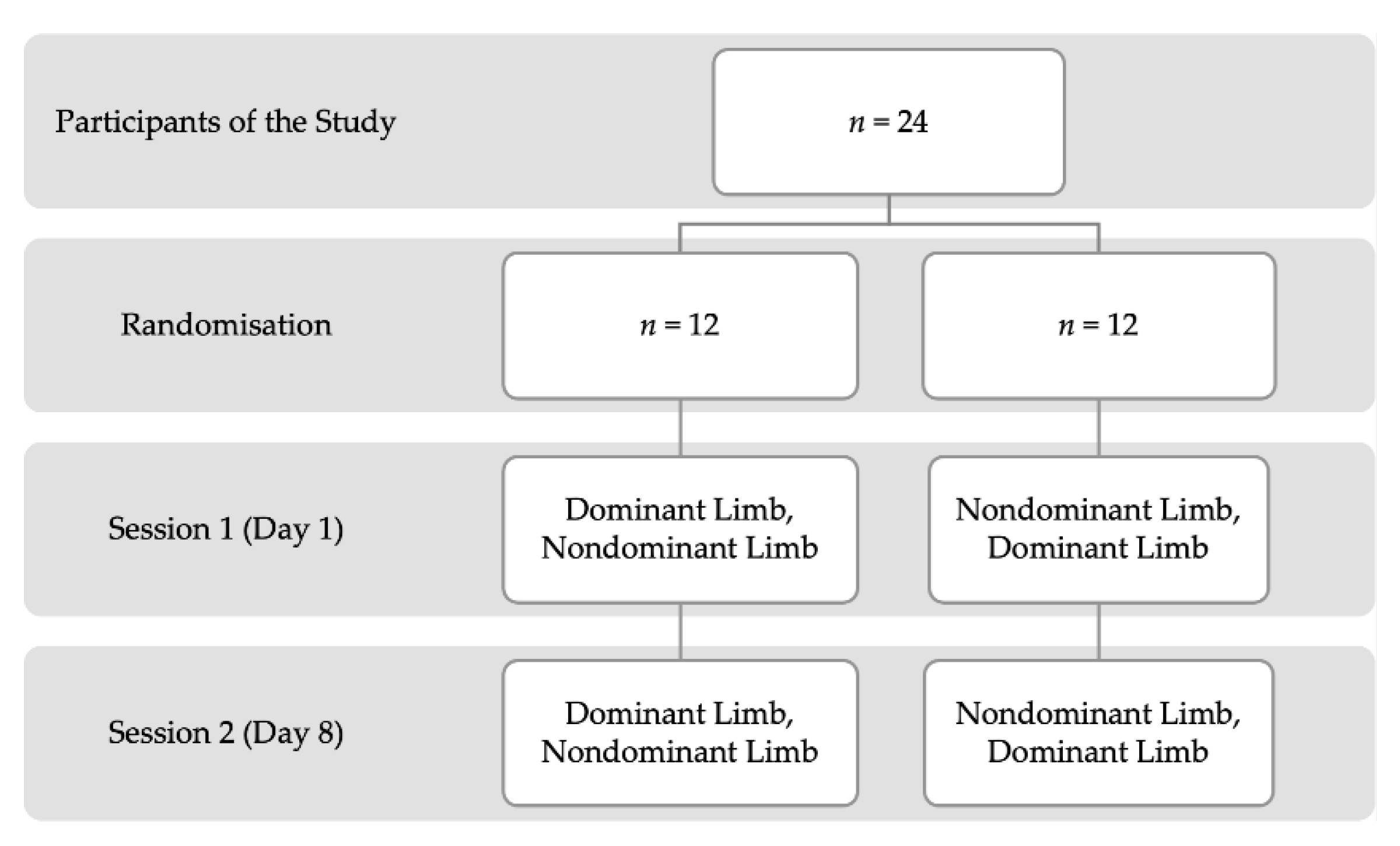
2.1. Study Design
2.2. Characteristics of Study Participants
2.3. Joint Position Sense Measurement Procedure
2.3.1. Joint Position Sense (JPS) Measurement in Active Mode
2.3.2. Joint Position Sense (JPS) Measurement in Passive Mode
2.4. Statistical Analysis
3. Results
3.1. Reliability of Active and Passive Modes of Joint Position Sense (JPS)
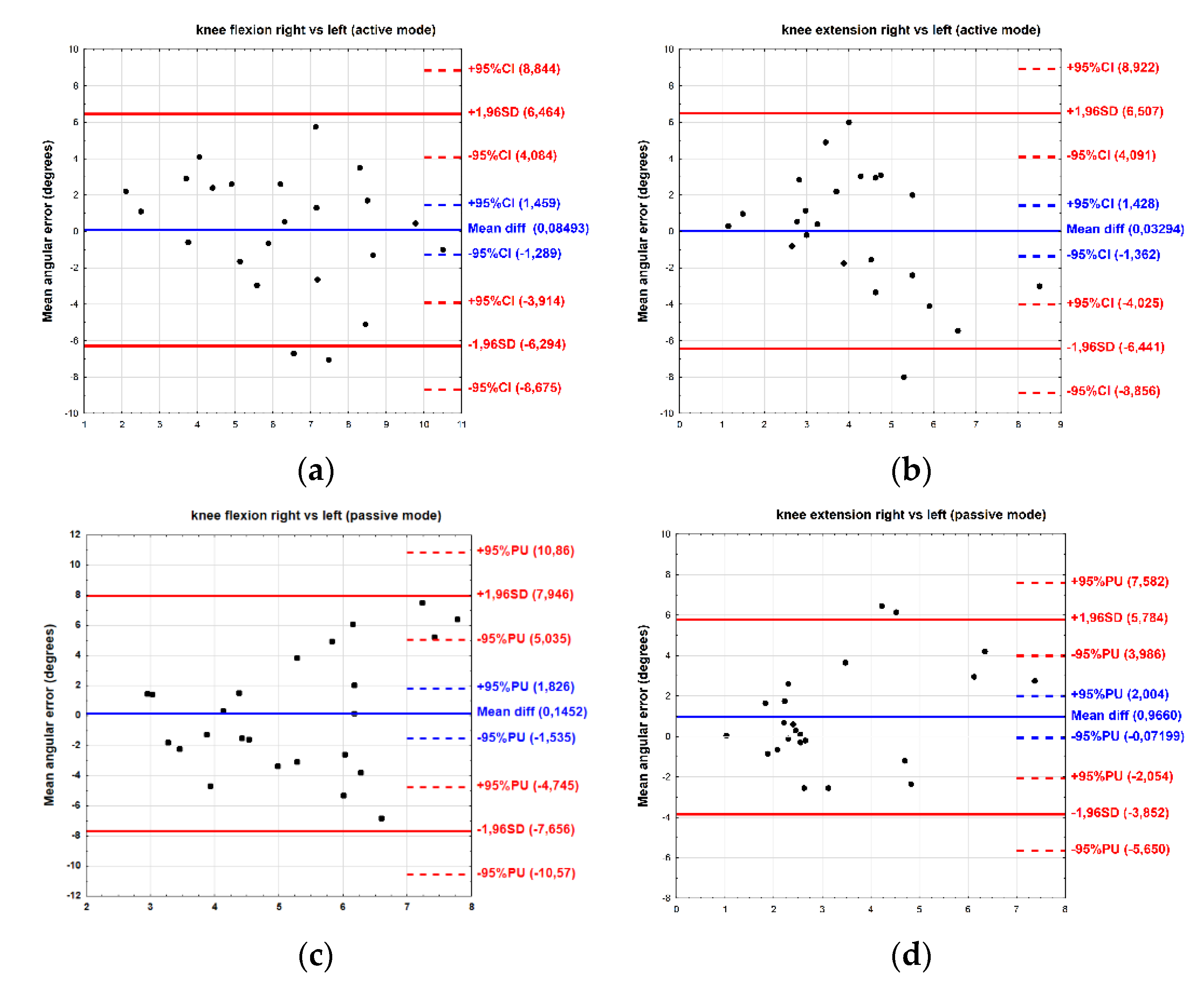
3.2. Comparison of Right and Left Sides of Joint Position Sense (JPS)
3.3. Comparison of Active and Passive Modes of Joint Position Sense (JPS)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Romero-Franco, N.; Montaño-Munuera, J.A.; Fernández-Domínguez, J.C.; Jiménez-Reyes, P. Validity and Reliability of a Digital Inclinometer to Assess Knee Joint Position Sense in an Open Kinetic Chain. J. Sport Rehabil. 2019, 28, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.O.; Davies, L.; Hing, C.B. A systematic review to determine the reliability of knee joint position sense assessment measures. Knee 2013, 20, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Romero-Franco, N.; Jiménez-Reyes, P.; González-Hernández, J.M.; Fernández-Domínguez, J.C. Assessing the concurrent validity and reliability of an iPhone application for the measurement of range of motion and joint position sense in knee and ankle joints of young adults. Phys. Ther. Sport 2020, 44, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, Y.; Iwaki, D.; Kawae, T.; Fudeyasu, K.; Kimura, H. Reliability of joint position sense measured in the knee using the level function of the iPhone “Measure” application. PLoS ONE 2021, 16, e0256561. [Google Scholar] [CrossRef] [PubMed]
- Genoves, G.G.; Cruz, C.F.; Doná, F.; Andrade, T.A.M.; Ferraz, H.B.; Barela, J.A. Detection of passive movement in lower limb joints is impaired in individuals with Parkinson’s disease. Neurophysiol. Clin. 2021, 51, 279–285. [Google Scholar] [CrossRef]
- Zia, S.; Cody, F.; O’Boyle, D. Joint position sense is impaired by Parkinson’s disease. Ann. Neurol. 2000, 47, 218–228. [Google Scholar] [CrossRef]
- Köprülüoğlu, M.; Naz, İ.; Solmaz, D.; Akar, S. Hand functions and joint position sense in patients with psoriatic arthritis- a comparison with rheumatoid arthritis and healthy controls. Clin. Biomech. 2022, 95, 105640. [Google Scholar] [CrossRef]
- Ulutatar, F.; Unal-Ulutatar, C.; Duruoz, M.T. Cervical proprioceptive impairment in patients with rheumatoid arthritis. Rheumatol. Int. 2019, 39, 2043–2051. [Google Scholar] [CrossRef]
- Ettinger, L.R.; Boucher, A.; Simonovich, E. Patients with type 2 diabetes demonstrate proprioceptive deficit in the knee. World J. Diabetes 2018, 9, 59–65. [Google Scholar] [CrossRef]
- Maras, O.; Dulgeroglu, D.; Cakci, A. Ankle Proprioception in Patients with Type 2 Diabetes Mellitus. J. Am. Podiatr. Med. Assoc. 2021, 111, 8. [Google Scholar] [CrossRef]
- Hillier, S.; Immink, M.; Thewlis, D. Assessing Proprioception: A Systematic Review of Possibilities. Neurorehabil. Neural Repair. 2015, 29, 933–949. [Google Scholar] [CrossRef]
- Wingert, J.R.; Burton, H.; Sinclair, R.J.; Brunstrom, J.E.; Damiano, D.L. Joint-position sense and kinesthesia in cerebral palsy. Arch. Phys. Med. Rehabil. 2009, 90, 447–453. [Google Scholar] [CrossRef]
- Dover, G.; Powers, M.E. Reliability of Joint Position Sense and Force-Reproduction Measures During Internal and External Rotation of the Shoulder. J. Athl. Train. 2003, 38, 304–310. [Google Scholar]
- Relph, N.; Herrington, L. Criterion-related validity of knee joint-position-sense measurement using image capture and isokinetic dynamometry. J. Sport Rehabil. 2015, 24. [Google Scholar] [CrossRef]
- Relph, N.; Herrington, L. Interexaminer, intraexaminer and test-retest reliability of clinical knee joint-position-sense measurements using an image-capture technique. J. Sport Rehabil. 2015, 24, 2013-0134. [Google Scholar] [CrossRef]
- Rahlf, A.L.; Petersen, E.; Rehwinkel, D.; Zech, A.; Hamacher, D. Validity and Reliability of an Inertial Sensor-Based Knee Proprioception Test in Younger vs. Older Adults. Front. Sports Act. Living 2019, 1, 27. [Google Scholar] [CrossRef]
- Ravi, B.; Kapoor, M.; Player, D. Feasibility and reliability of a web-based smartphone application for joint position measurement. J. Rehabil. Med. 2021, 53, jrm00188. [Google Scholar] [CrossRef]
- Tian, F.; Zhao, Y.; Li, J.; Wang, W.; Wu, D.; Li, Q.; Guo, L.; Wang, S. Test-Retest Reliability of a New Device Versus a Long-Arm Goniometer to Evaluate Knee Proprioception. J. Sport Rehabil. 2022, 31, 368–373. [Google Scholar] [CrossRef]
- Osama Al Saadawy, B.; Abdo, N.; Embaby, E.; Rehan Youssef, A. Validity and reliability of smartphones in measuring joint position sense among asymptomatic individuals and patients with knee osteoarthritis: A cross-sectional study. Knee 2021, 29, 313–322. [Google Scholar] [CrossRef]
- Grob, K.R.; Kuster, M.S.; Higgins, S.A.; Lloyd, D.G.; Yata, H. Lack of correlation between different measurements of proprioception in the knee. J. Bone Jt. Surg. Br. 2002, 84, 614–618. [Google Scholar] [CrossRef]
- Marks, R. Repeatability of position sense measurements in persons with osteoarthritis of the knee: A pilot study. Clin. Rehabil. 1995, 9, 314–319. [Google Scholar] [CrossRef]
- Pincivero, D.M.; Bachmeier, B.; Coelho, A.J. The effects of joint angle and reliability on knee proprioception. Med. Sci. Sports Exerc. 2001, 33, 1708–1712. [Google Scholar] [CrossRef] [PubMed]
- Jung, I.G.; Yu, I.Y.; Kim, S.Y.; Lee, D.K.; Oh, J.S. Reliability of ankle dorsiflexion passive range of motion measurements obtained using a hand-held goniometer and Biodex dynamometer in stroke patients. J. Phys. Ther. Sci. 2015, 27, 1899–1901. [Google Scholar] [CrossRef] [PubMed]
- Stańczyk, K.; Poświata, A.; Roksela, A.; Mikulski, M. Assessment of Muscle Fatigue, Strength and Muscle Activation During Exercises with the Usage of Robot Luna EMG, Among Patients with Multiple Sclerosis. In Information Technology in Biomedicine; Springer International Publishing: Cham, Switzerland, 2019. [Google Scholar]
- Hart, S.; Gabbard, C. Examining the stabilising characteristics of footedness. Laterality 1997, 2, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Anson, J.; Waddington, G.; Adams, R. Proprioceptive performance of bilateral upper and lower limb joints: Side-general and site-specific effects. Exp. Brain Res. 2013, 226, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Oleksy, Ł.; Mika, A.; Kielnar, R.; Grzegorczyk, J.; Marchewka, A.; Stolarczyk, A. The influence of pelvis reposition exercises on pelvic floor muscles asymmetry: A randomized prospective study. Medicine 2019, 98, e13988. [Google Scholar] [CrossRef]
- Bullock-Saxton, J.E.; Wong, W.J.; Hogan, N. The influence of age on weight-bearing joint reposition sense of the knee. Exp. Brain Res. 2001, 136, 400–406. [Google Scholar] [CrossRef]
- Bakhtiari, R.A. Evaluation of Static and Dynamic Balance and Knee Proprioception in Young Professional Soccer Players. Ann. Biol. Res. 2012, 3, 2867–2873. [Google Scholar]
- van Melick, N.; Meddeler, B.M.; Hoogeboom, T.J.; Nijhuis-van der Sanden, M.W.G.; van Cingel, R.E.H. How to determine leg dominance: The agreement between self-reported and observed performance in healthy adults. PLoS ONE 2017, 12, e0189876. [Google Scholar] [CrossRef]
- Springer, S.; Kelman, D.; Brand, M.; Gottlieb, U. Knee position sense: Does the time interval at the target angle affect position accuracy? J. Phys. Ther. Sci. 2017, 29, 1760–1765. [Google Scholar] [CrossRef]
- Daneshjoo, A.; Mokhtar, A.H.; Rahnama, N.; Yusof, A. The effects of comprehensive warm-up programs on proprioception, static and dynamic balance on male soccer players. PLoS ONE 2012, 7, e51568. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163, Erratum in J. Chiropr. Med. 2017, 16, 346. [Google Scholar] [CrossRef]
- Bujang, M.A.; Baharum, N. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: A review. Arch. Orofac. Sci. 2017, 12, 1–11. [Google Scholar]
- Callaghan, M.J.; Selfe, J.; Bagley, P.J.; Oldham, J.A. The Effects of Patellar Taping on Knee Joint Proprioception. J. Athl. Train. 2002, 37, 19–24. [Google Scholar] [CrossRef][Green Version]
- Selfe, J.; Callaghan, M.; McHenry, A.; Richards, J.; Oldham, J. An investigation into the effect of number of trials during proprioceptive testing in patients with patellofemoral pain syndrome. J. Orthop. Res. 2006, 24, 1218–1224. [Google Scholar] [CrossRef]
- Fatoye, F.A.; Palmer, S.T.; Macmillan, F.; Rowe, P.J.; van der Linden, M.L. Repeatability of joint proprioception and muscle torque assessment in healthy children and in children diagnosed with hypermobility syndrome. Musculoskelet. Care 2008, 6, 108–123. [Google Scholar] [CrossRef]
- Relph, N.; Herrington, L. The effects of knee direction, physical activity and age on knee joint position sense. Knee 2016, 23, 393–398. [Google Scholar] [CrossRef]
- Stillman, B.C.; McMeeken, J.M.; Macdonell, R.A. Aftereffects of resisted muscle contractions on the accuracy of joint position sense in elite male athletes. Arch. Phys. Med. Rehabil. 1998, 79, 1250–1254. [Google Scholar] [CrossRef]
- Relph, N.; Herrington, L. The effect of conservatively treated acl injury on knee joint position Sense. Int. J. Sport. Phys. Ther. 2016, 11, 536–543. [Google Scholar]
- Petterson, S.C.; Barrance, P.; Buchanan, T.; Binder-Macleod, S.; Snyder-Mackler, L. Mechanisms underlying quadriceps weakness in knee osteoarthritis. Med. Sci. Sport. Exerc. 2008, 40, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Drouin, J.M.; Valovich-mcLeod, T.C.; Shultz, S.J.; Gansneder, B.M.; Perrin, D.H. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur. J. Appl. Physiol. 2004, 91, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Roos, E.M.; Herzog, W.; Block, J.A.; Bennell, K.L. Muscle weakness, afferent sensory dysfunction and exercise in knee osteoarthritis. Nat. Rev. Rheumatol. 2011, 7, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Zazulak, B.T.; Hewett, T.E.; Reeves, N.P.; Goldberg, B.; Cholewicki, J. The effects of core proprioception on knee injury: A prospective biomechanical-epidemiological study. Am. J. Sport. Med. 2007, 35, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Adamo, D.E.; Alexander, N.B.; Brown, S.H. The influence of age and physical activity on upper limb proprioceptive ability. J. Aging Phys. Act. 2009, 17, 272–293. [Google Scholar] [CrossRef]
- Ashton-Miller, J.A. Proprioceptive thresholds at the ankle: Implications for the prevention of ligament injury. In Proprioception and Neuromuscular Control in Joint Stability; Lephart, S.M., Fu, F.H., Eds.; Human Kinetics Publisher: Champaign, IL, USA, 2000; pp. 279–289. [Google Scholar]
- Piriyaprasarth, P.; Morris, M.E.; Delany, C.; Winter, A.; Finch, S. Trials needed to assess knee proprioception following stroke. Physiother. Res. Int. 2009, 14, 6–16. [Google Scholar] [CrossRef]
- Iwańska, D.; Karczewska, M.; Madej, A.; Urbanik, C. Symmetry of proprioceptive sense in female soccer players. Acta Bioeng. Biomech. 2015, 17, 155–163. [Google Scholar]
- Carson, R.G.; Elliott, D.; Goodman, D.; Dickinson, J. Manual asymmetries in the reproduction of a 3-dimensional spatial location. Neuropsychologia 1990, 28, 99–103. [Google Scholar] [CrossRef]
- Adamo, D.E.; Martin, B.J. Position sense asymmetry. Exp. Brain Res. 2009, 192, 87–95. [Google Scholar] [CrossRef][Green Version]



| Knee Movement | Flexion | Extension | Flexion | Extension |
|---|---|---|---|---|
| Mode | Active | Active | Passive | Passive |
| Consecutive tests | Test 1 | Test 2 | Test 3 | Test 4 |
| Baseline knee joint position (°) | 0 | 90 | 0 | 90 |
| Target knee joint position (°) | 60 | 30 | 60 | 30 |
| Time duration for target position (s) | 5 | 5 | 5 | 5 |
| Time duration for baseline position (s) | 3 | 3 | 3 | 3 |
| Number of repetitions | 2 | 2 | 2 | 2 |
| Right Side | Left Side | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome Measure | ICC (Cl 95%) | Mean ± SD (CI 95%) | CV | SEM | ICC | Mean ± SD (CI 95%) | CV | SEM | |
| 1st | Flexion active (°) | 0.866 (0.765–0.951) | 6.29 ± 2.40 (5.28–7.31) | 38.16 | 0.49 | 0.945 (0.897–0.980) | 6.28 ± 3.12 (4.96–7.60) | 49.79 | 0.63 |
| 2nd | 6.31 ± 2.34 (5.32–7.29) | 37.12 | 0.47 | 6.22 ± 3.06 (4.93–7.52) | 49.26 | 0.62 | |||
| 1st | Extension active (°) | 0.922 (0.801–0.962) | 4.43 ± 1.98 (3.56–5.27) | 44.82 | 0.40 | 0.962 (0.949–0.987) | 3.79 ± 2.40 (2.77–4.80) | 63.40 | 0.49 |
| 2nd | 4.04 ± 1.77 (3.29–4.79) | 43.79 | 0.36 | 4.01 ± 2.85 (2.80–5.21) | 71.03 | 0.58 | |||
| 1st | Flexion passive (°) | 0.982 (0.959–0.992) | 5.34 ± 2.98 (4.06–6.61) | 55.87 | 0.60 | 0.949 (0.927–0.973) | 5.37 ± 1.95 (4.55–6.20) | 36.35 | 0.39 |
| 2nd | 5.28 ± 2.81 (4.10–6.47) | 53.15 | 0.57 | 5.14 ± 2.00 (4.29–5.98) | 39.08 | 0.41 | |||
| 1st | Extension passive (°) | 0.945 (0.877–0.975) | 3.57 ± 2.65 (2.45–4.69) | 74.12 | 0.54 | 0.980 (0.952–0.991) | 2.75 ± 1.54 (2.09–3.40) | 56.26 | 0.31 |
| 2nd | 3.68 ± 2.45 (2.64–4.71) | 66.60 | 0.50 | 2.71 ± 1.61 (2.03–3.39) | 59.25 | 0.32 | |||
| Outcome Measure | r | Mean ± SD | ||||
|---|---|---|---|---|---|---|
| 1st Session | 2nd Session | 1st Session R/L | p | 2nd Session R/L | p | |
| Flexion active (°) | 0.29 | 0.29 | 6.62 ± 2.40/6.28 ± 3.12 | n.s. | 6.31 ± 2.34/6.22 ± 3.06 | n.s. |
| Extension active (°) | 0.30 | 0.30 | 4.43 ± 1.98/3.79 ± 2.40 | n.s. | 4.04 ± 1.77/4.01 ± 2.85 | n.s. |
| Flexion passive (°) | 0.30 | 0.34 | 5.34 ± 2.98/5.37 ± 1.95 | n.s. | 5.28 ± 2.81/5.14 ± 2.00 | n.s. |
| Extension passive (°) | 0.21 | 0.32 | 3.57 ± 2.65/2.75 ± 1.54 | n.s. | 3.68 ± 2.45/2.71 ± 1.61 | n.s. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oleksy, Ł.; Królikowska, A.; Mika, A.; Reichert, P.; Kentel, M.; Kentel, M.; Poświata, A.; Roksela, A.; Kozak, D.; Bienias, K.; et al. A Reliability of Active and Passive Knee Joint Position Sense Assessment Using the Luna EMG Rehabilitation Robot. Int. J. Environ. Res. Public Health 2022, 19, 15885. https://doi.org/10.3390/ijerph192315885
Oleksy Ł, Królikowska A, Mika A, Reichert P, Kentel M, Kentel M, Poświata A, Roksela A, Kozak D, Bienias K, et al. A Reliability of Active and Passive Knee Joint Position Sense Assessment Using the Luna EMG Rehabilitation Robot. International Journal of Environmental Research and Public Health. 2022; 19(23):15885. https://doi.org/10.3390/ijerph192315885
Chicago/Turabian StyleOleksy, Łukasz, Aleksandra Królikowska, Anna Mika, Paweł Reichert, Monika Kentel, Maciej Kentel, Anna Poświata, Anna Roksela, Dominika Kozak, Katarzyna Bienias, and et al. 2022. "A Reliability of Active and Passive Knee Joint Position Sense Assessment Using the Luna EMG Rehabilitation Robot" International Journal of Environmental Research and Public Health 19, no. 23: 15885. https://doi.org/10.3390/ijerph192315885
APA StyleOleksy, Ł., Królikowska, A., Mika, A., Reichert, P., Kentel, M., Kentel, M., Poświata, A., Roksela, A., Kozak, D., Bienias, K., Smoliński, M., Stolarczyk, A., & Mikulski, M. (2022). A Reliability of Active and Passive Knee Joint Position Sense Assessment Using the Luna EMG Rehabilitation Robot. International Journal of Environmental Research and Public Health, 19(23), 15885. https://doi.org/10.3390/ijerph192315885











