Review of Importance of Weather and Environmental Variables in Agent-Based Arbovirus Models
Abstract
1. Introduction
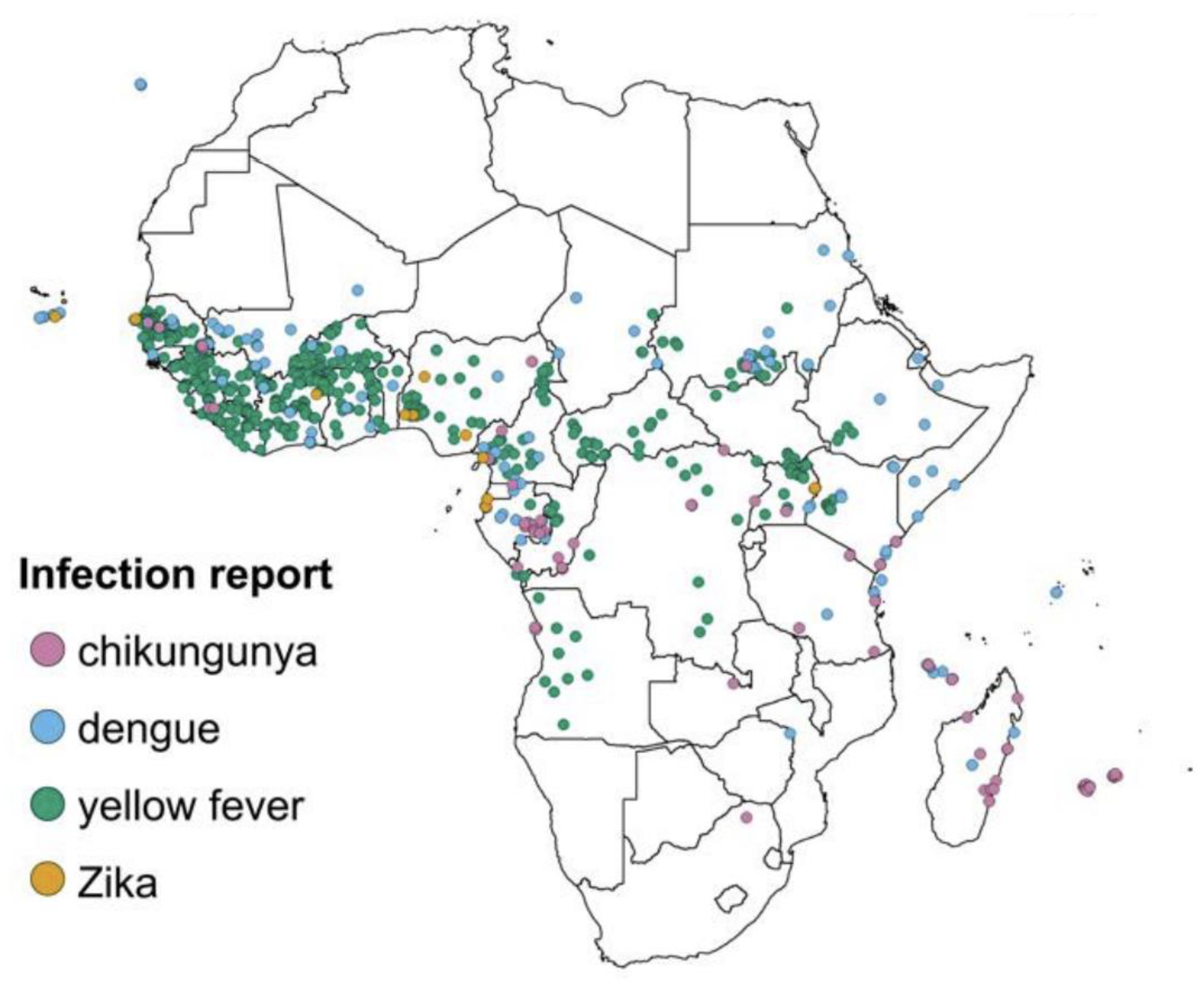
1.1. Background Concepts
1.1.1. Dengue Fever
1.1.2. Agent-Based Modeling
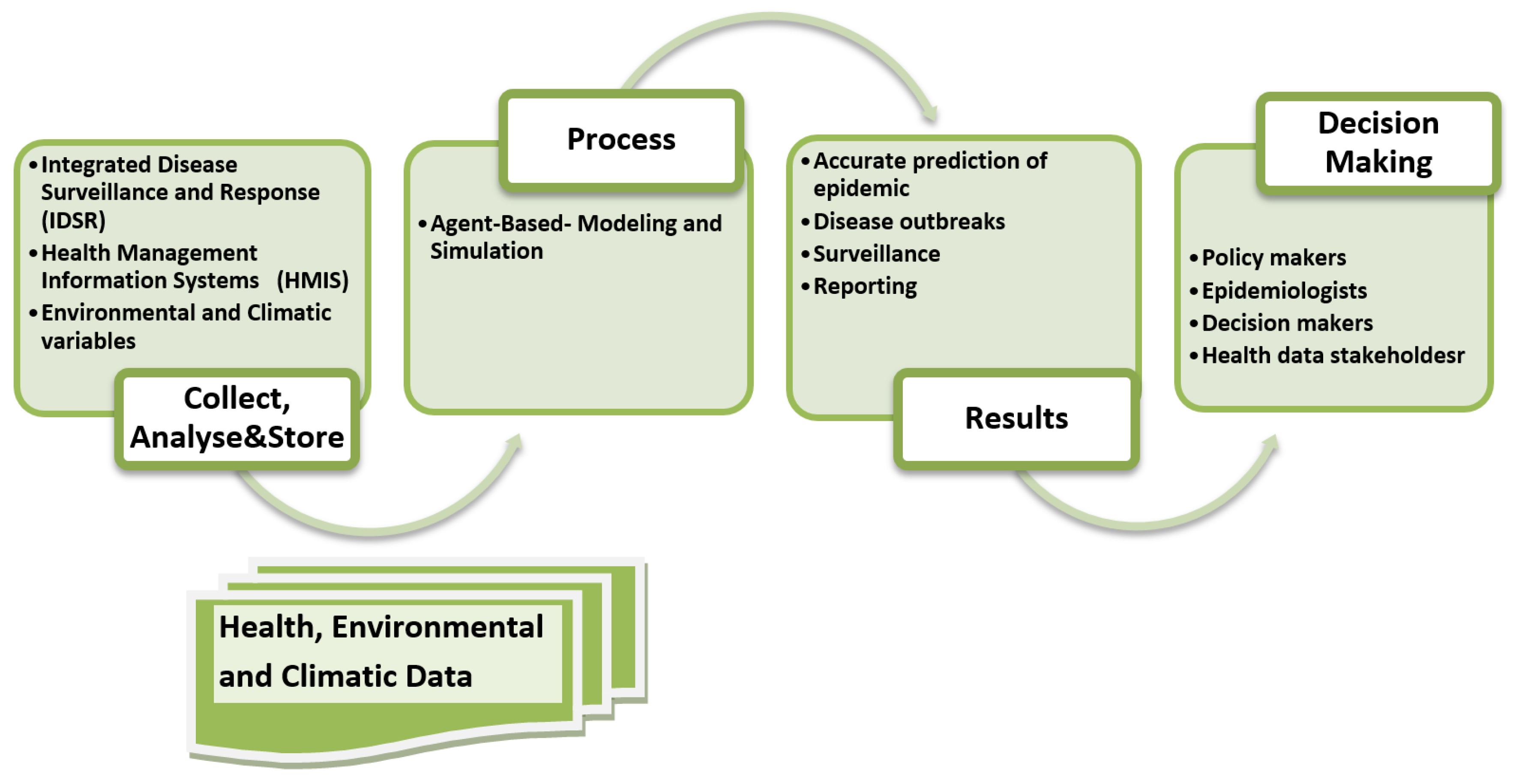
2. Materials and Methods
2.1. PubMed Search
2.2. SCOPUS Search
2.3. Research4Life Search
2.4. Google Scholar Search
2.5. Inclusion Criteria
- i.
- Those that investigated the effects of climatic factors or environmental factors (for example rainfall, temperature, humidity, landscape type, mosquito habitats) on the incidence, transmission, and modeling of infectious diseases.
- ii.
- Those related to arboviruses, especially in Africa.
- iii.
- Those that involved modeling of arbovirus disease.
- iv.
- Studies that were published in any year.
- v.
- Articles that were published in English.
3. Results
3.1. Temperature
3.2. Precipitation
3.3. Humidity
3.4. Environmental Factors
4. Discussion
- (i)
- Through the review, it has been identified that ABM in Africa is mostly implemented for other diseases such as malaria, Ebola, rift valley fever, west Nile virus, tuberculosis, human immunodeficiency virus, and other dominant diseases rather than dengue disease [62,63,64,65,66,67,68]. This shows that there is a lack of sufficient literature on ABM for dengue disease in Africa and thus points to a need for further research on dengue and ABM and simulation in the African context.
- (ii)
- Dengue modeling in ABM is extensively conducted in non-African countries, and although extensively researched in these non-African countries, few studies have considered the influence of climatic and environmental factors. The context of non-African countries into which climatic and environmental conditions have been incorporated into dengue disease modeling is different from the African context.
- (iii)
- Agent-based model frameworks that have been implemented in the reviewed studies included NetLogo, Repast, AnyLogic, EMOD, MESA, MASON, Mlab, Swarm, StarLogo, and Spark. Other recent and more capable ABM tools such as JADE, GAMA, WALK, MARS, and Vigueras were not found in the reviewed works of literature. Advances in technology and computing power have made emerging new tools such as MARS offer a promising output in ABM and simulation. The MARS framework developed for multi-agent research and simulations can simulate a large number of agents’ interactions using a local machine or a cloud-native environment [91,92,93]. The MARS framework allows the implementation of layered architecture and allows spatio-temporal data integration in which raster- and vector-based data can efficiently be handled. A study by Glake et al. [92] identifies that it is important to evaluate the spatio-temporal data model of the MARS framework with real-world cases.
- (iv)
- To the authors’ knowledge, there are no available reviews that have specifically studied and modeled dengue disease and the influence of climatic and environmental factors using the MARS framework for ABM in the SSA context. Therefore, this review is crucial to enlighten a need for more studies on dengue modeling in Tanzania’s context and explore the effects of climatic, environmental, and spatio-temporal factors on dengue disease outbreaks, transmission, and surveillance.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
Appendix C
| Serial # | Author, Article Type, Diseases Studied | Climatic Factor Temperature, Rainfall/Precipitation, Humidity/Relative Humidity) | Environmental Factors | The Modeling Approach Used (Agent-Based, Compartmental Models, Machine Learning, Time Series, etc.) | Research Settings (Africa, Global, Country-Specific, etc.) | Study Objective and Results |
|---|---|---|---|---|---|---|
| 1. | Wearing et al. [69], Review paper, Dengue and chikungunya. | Effects of humidity, temperature, and rainfall on egg diapause and adult survival. | Vector density/ population dynamics, urbanization, availability of man-made containers, vegetation index. | Review of different models: process-based models, statistical models, mathematical models. | Global | The study observed that when a suitable mosquito vector (Ae. Albopictus/Aegypti) coupled with suitable conditions for their survival and transmission was required for the occurrence of a mosquito-borne virus in a population. The study also revealed that the virus was introduced from external sources and conditions amenable to its transmission. |
| 2. | Talaga et al. [24], Experimental. Paper, Ae. Aegypti. | Daily precipitation, air temperature, wind, and relative humidity. | Artificial water containers (such as CDC ovitraps, and car tires), natural water containers (such as native tank bromeliads, dry stamps of bamboo), size of aquatic habitat, and an abundance of Ae. Aegypti immatures. | Multi-model inference approach. | French Guiana (Kourou which is a small Neotropical), October 2013–October 2014. | The relative influence of biotic and abiotic parameters on the immature population of Ae. Aegypti was explored using four different types of water containers and three urbanized sites. The study found that artificial water containers, size of aquatic habitat, amount of precipitation, temperature, and relative humidity positively influenced the number of Ae. Aegypti immatures. The study presented co-existence of Ae. Aegypti with predators and competitors on the abundance of immatures. |
| 3. | Center [72], Annual Meeting Report, Female and male Ae. Aegypti, Malaria parasites. | Temperature (low 19 °C and high 30 °C). | 288 Vegetation zones, 93 urban zones, breeding spots, 50 households. | ABM | Key West, Florida with an area of approximately 30,000 m2 with around 50 households. | An ABM coupled with a geographic information system for identifying zones with resources necessary for the survival of both male and female Ae. Aegypti and modeling possible breeding site locations. Results showed that the spatial distribution of the vegetation zones, urban zones, and breeding spots together with the temperature, constrained the population of Ae. Aegypti to a mean high of around 2000 during the fall season and around 600 in the late winter season. |
| Tropical climate, weather. | Demographics data. | ABM (EMOD framework). | SSA | EMOD is a proprietary epidemiological modeling software package that is used to determine the best combination of interventions that will eventually eradicate the disease. EMOD is a human, mosquito, and parasite modeling program that takes mosquito, weather, demographic, and parasite parameters as input. | ||
| 4. | Ingabire and Kimura [63], Journal Article, Malaria (Anopheles gambaie). | Temperature (minimum 10 °C and maximum 29 °C), humidity (30–97%), rainfall. | N/A | Mathematical SIR/IR model. | Rwanda meteorology data for 2017 was used. | The research focused on climate effects on the sensitivity of a reproduction rate, death rate, and infection rate, focusing on the life cycle of mosquitoes based on the change in temperature and humidity. Mosquito reproduction increased when humidity was more than 80%. Thus, the high birth rate during hot and high humidity season could accelerate the increase in mosquitoes and enhance the spread of infection. Simulation with real data showed that the number of mosquitoes and the number of patients changed exponentially was mainly caused by humidity change. |
| 5. | Anders [73,83,84], Ph.D. Thesis, Journal articles, Dengue. | Temperature, rainfall, humidity. | Breeding sites, mosquito density, human population density, water storage needs, and practices. | Mathematical modeling. | Clinically diagnosed dengue cases that were admitted between 1996 and 2009 in three hospitals in Ho Chi Minh City, Southern Vietnam. | The study sought to characterizethe distribution of dengue fever as well as the factors that influence individual and population-level infection risk and disease outcome. Heterogeneity in dengue incidence in space and time is studied. Dengue is found to be sensitive to climatic conditions, which influence virus replication, development, and vector survival. Non-climatic variables such as environmental changes, population growth and human movement, work hand in hand with the climatic variables. |
| 6. | Liu [25,97,98], Ph.D. Thesis, Journal articles Dengue, Zika. | Temperature (daily, min, max, average), precipitation, relative humidity. | N/A | Multivariate Exponentially Weighted Moving Average (MEWMA) model with a forward feature selection (FFS) algorithm (MEWMA-FFS) framework, machine learning. | Detection of large dengue outbreaks in San Juan-Puerto Rico 2004–2017, Iquitos-Peru 2004–2013, Mexico country 2004–2013. | The study focused on two aspects of emerging and re-emerging infectious disease surveillance systems, with the goal of developing a method for detecting emerging and re-emerging outbreaks as early and accurately as possible, and the study has assessed the tradeoff between the complexity of the model and prediction reliability. The results showed that in Mexico, a subset of the climate-relevance time series model was the best option for early detection of large dengue outbreaks, as was the case in San Juan, where the climate system’s performance was more robust across cross-validation and out-of-sample testing periods. In Iquitos Peru, due to its location, experienced a tropical rainforest climate that lacks a distinct dry season demonstrating that climate was not a good predictor for large dengue outbreaks. |
| 7. | Deza-Cruz [70], Ph.D. Thesis, Dengue, chikungunya, Zika. | Humidity, temperature, rainfall, wind speed. | Household (water supply, air-conditioning, intact mosquito screens, construction materials, number of residents in the house, number of rooms in the house), mosquito larval habitat (Trash collection, Pools water, Storage water, Debris around house, Plant pots). | Machine learning. | University students at St. Kitts and Nevis between September 2014–May and 2015. | The study found that arbovirus transmission was associated with climatic variables connected to seasonality, which are temperature and rainfall. Humidity and temperature had a positive influence on disease transmission, rainfall had a dual effect (much rain caused a flushing effect, and moderate rain had a positive effect). At the mean temperature of 26 °C and 29 °C large number of mosquitoes were captured, while the number declined at 31 °C. |
| 8. | Trewin [32,33,99], Ph.D. Thesis, Journal Articles, Ae. Aegypti. | Temperature, rainfall, the humidity of the water in the rainwater tanks and the buckets. | Rainwater tanks, buckets. | ABM (Repast Simphony 2.4.0) | Datasets from Brisbane city council 2012, Queensland government 2017 and Australian Bureau of Statistics 2011. | The model aimed at understanding the implications of mosquito spread between rainwater tanks and identifying risk areas in Brisbane. The number of rainwater tanks in the landscape was principally responsible for the risk. |
| 9. | Tourre et al. [65], Journal article, Malaria. | Temperature (minimum, maximum), rainfall, relative humidity. | N/A | Impact model to evaluate the influence of climate conditions on malaria risk. | Nouna region in northern Burkina Faso. Rainfall, temperature, and relative humidity data for the period of 1983–2011 were used. | Climate impact model for malaria risk. Total rainfall for three months was found to be a confounding factor for the malaria vector density. It was discovered that there is a substantial relationship between risk for malaria and low-frequency rainfall variability related to the Atlantic Multi-decadal Oscillation (AMO). |
| 10. | Borges et al. [74], Conference paper, Dengue (Ae. Aegypti pupal productivity). | N/A | Type of container. | ABM using NetLogo. | The model is simulated 1500 times each simulated 100 days. | ABM for evaluating the Pupal Productivity of Ae. Aegypti in containers. The model took into account the pupae production capability of each container in which the mosquitoes laid eggs. The model results were compared to the simulation’s average percentage of pupae per container and the percentage of container productivity defined in Brito-Arduino 2014. |
| 11. | Mukhtar et al. [66], Journal Article, Malaria (Anopheles gambiae). | Temperature, rainfall. | N/A | Mathematical models. | Two regions in South Sudan. | Climate-driven dynamics model was used to evaluate the impact of rainfall and temperature on the dynamics of the mosquito population in a specific region of South Sudan. Daily temperatures ranged 20 °C to 35°C and rainfall ranged 17 mm to 20 mm were ideal for mosquito progression which facilitated malaria spread. Thus, the warmer temperature might lead to disease intensification. |
| 12. | Rumisha et al. [67], Journal Article, Malaria (Anopheles funestus, Anopheles gambiae, Anopheles arabiensis). | Rainfall, temperature. | N/A | Bayesian spatio-temporal binomial and zero-inflated negative binomial regression models, Machine learning model. | Data are collected for three years by Demographic Surveillance System (DSS) in Rufiji Tanzania. | The study aimed to assess spatial-temporal variation and heterogeneity of malaria transmission in the Rufiji DSS site using a large geo-referenced biweekly entomological dataset collected over three years (October 2001–September 2004) and rigorous Bayesian geostatistical models. Results depicted temporal and seasonal variation in entomological inoculation rate along the study period and study area. |
| 13. | Kang and Aldstadt [26], Journal Article, Dengue. | N/A | Mosquito habitats, the spatial configuration of buildings (model environment had 4 schools, 20 workplaces and 895 houses). | ABM using AnyLogic. | A portion of Kamphaeng Phet Province (KPP), Thailand. Parts of a registered residents dataset of KPP in 2009 were used. | The study sought to shed light on the significance of specifying building spatial configurations and mosquito habitats. The experiments’ findings revealed a significant influence on human residential and mosquito population patterns. |
| 14. | Maneerat and Daudé [75], Journal Article, Dengue (Ae. Aegypti female mosquito). | Daily time, hourly temperature and daily rainfall. | Urban landscape. | ABM-Model of Mosquito Aedes (MOMA). | Hauz Rani is a neighborhood in south Delhi (India). Meteorological data of June 2008 is used for performing the simulations. | A behavioral model MOMA of the Ae. Aegypti mosquito aimed to study the effects of factors such as breeding site density, human density, and topology at a neighborhood level on the dynamics of mosquito population. MOMA investigated mosquito population dynamics in a variety of urban settings. The findings revealed a link between human density, urban topology, and adult mosquito flight. |
| 15. | Dommar et al. [71], Journal Article, Chikungunya. | Precipitation. | N/A | ABM | An agent-based model, 2 years (28 March 2005–12 February 2006) daily precipitation data for La Réunion. | The researchers created an ABM to investigate the spatiotemporal heterogeneity of an infectious vector-borne disease outbreak. The impact of precipitation-dependent vector populations and the structure of the underlying network topology on epidemiological dynamics was investigated using a model. Results indicated that precipitation was the dominant factor influencing the spatio-temporal transmission. |
| 16. | Mulyani et al. [76], Journal Article, Dengue. | Temperature, humidity. | N/A | ABM-NetLogo. | Data and information from the national meteorology, climatology and geophysics agency were used. Community health data of Bogor, a region in Dramaga for two periods, January–June 2015 and July–December 2015 were used. | The paper has focused on the simulation behavior of the agent, agent interactions, and agent-environment interactions. Temperature and humidity variables have been used. Results showed that with optimal parameters of temperature and humidity the percentage of infected humans increased as well as mosquito count increased. With low parameters, the percentage of infected humans was steady or did not happen, while the number of mosquitoes decreased. Meanwhile, with fluctuated parameter values, the infection of humans and mosquitoes also fluctuated. |
| 17. | Deng et al. [77], Conference Paper, Dengue. | Wind direction | Landscape roughness, population, and land use type. | ABM developed with VB6.0 | Virtual environment. | The spreading mechanism of dengue is explained through agent-agent and agent-environment interactions. |
| 18. | Mahmood et al. [14], Book Chapter, Dengue. | Temperature, rainfall, humidity. | Water bodies, Mosquito density. | ABM using AnyLogic university edition. | Dengue outbreak data from Islamabad city in Pakistan, 2013. | Results showed that dengue transmission was dependent on temperature, when temperature increased, the biting rate of Ae. Aegypti increased which resulted in increased dengue cases. |
| 19. | Rodríguez [78], Ph.D. Thesis, Dengue. | Temperature, precipitation. | Socio-economic, demographic variables. | Dengue Fever ABM (DFABM) was developed using the Java programming language and open-source MASON simulator, a multi-threaded agent-based simulation platform. | Datasets on monthly reported dengue cases, weather predictors (temperature and precipitation), socio-economic and demographics measures of the population of Central Valley of Costa Rica from 1993 to 2008. | The spread of dengue fever in ABM was simulated using GIS in an urban setting while also taking into account individual interactions in a geospatial context. The variables of temperature, precipitation, socioeconomic status, and demographics were examined. The results showed that high temperatures with heavy precipitation affected the greatest proportion of reported dengue cases. In general, high temperatures, poor housing conditions, and male predominance during warm seasonal rainy periods created ideal conditions for mosquito outbreaks and, as a result, occurrences and rates of dengue cases. |
| 20. | Colón-González et al. [68], Journal Article, Malaria. | Air temperature, rainfall. | Urbanization, rural districts, socioeconomic indicators. | Time series cross-validation algorithm. | Malaria incidences in Rwanda and Uganda from 2002 to 2011. | The study looked at the short-term effects of rainfall, air temperature, and socioeconomic indicators on malaria incidence. It emphasized the importance of using climatic information in the analysis of malaria surveillance data and demonstrated the potential for the development of climate-informed malaria early warning systems. |
References
- Brauer, F. Mathematical epidemiology: Past, present, and future. Infect. Dis. Model. 2017, 2, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Boyce, M.R.; Katz, R.; Standley, C.J. Risk factors for infectious diseases in urban environments of sub-Saharan Africa: A systematic review and critical appraisal of evidence. Trop. Med. Infect. Dis. 2019, 4, 123. [Google Scholar] [CrossRef] [PubMed]
- Ngatu, N.R.; Kayembe, N.J.M.; Phillips, E.K.; Okech-Ojony, J.; Patou-Musumari, M.; Gaspard-Kibukusa, M.; Madone-Mandina, N.; Godefroid-Mayala, M.; Mutaawe, L.; Manzengo, C.; et al. Epidemiology of ebolavirus disease (EVD) and occupational EVD in health care workers in Sub-Saharan Africa: Need for strengthened public health preparedness. J. Epidemiol. 2017, 27, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Gwenzi, W.; Sanganyado, E.; Gwenzi, W.; Sanganyado, E. Recurrent cholera outbreaks in sub-saharan africa: Moving beyond epidemiology to understand the environmental reservoirs and drivers. Challenges 2019, 10, 1. [Google Scholar] [CrossRef]
- Jindal, A.; Rao, S. Agent-based modeling and simulation of mosquito-borne disease transmission. In Proceedings of the 16th International Conference on Autonomous Agents and Multiagent Systems, São Paulo, Brazil, 8–12 May 2017; pp. 426–435. [Google Scholar]
- Singh, S.; Herng, L.C.; Sulaiman, L.H.; Wong, S.F.; Jelip, J.; Mokhtar, N.; Harpham, Q.; Tsarouchi, G.; Gill, B.S. The Effects of Meteorological Factors on Dengue Cases in Malaysia. Int. J. Environ. Res. Public Health 2022, 19, 6449. [Google Scholar] [CrossRef] [PubMed]
- dos Santos Souza Marinho, R.; Duro, R.L.S.; Mota MT de, O.; Hunter, J.; Diaz, R.S.; Kawakubo, F.S.; Komninakis, S.V. Environmental Changes and the Impact on the Human Infections by Dengue, Chikungunya and Zika Viruses in Northern Brazil, 2010–2019. Int. J. Environ. Res. Public Health 2022, 19, 12665. [Google Scholar] [CrossRef]
- Dodero-Rojas, E.; Ferreira, L.G.; Leite, V.B.P.; Onuchic, J.N.; Contessoto, V.G. Modeling Chikungunya control strategies and Mayaro potential outbreak in the city of Rio de Janeiro. PLoS ONE 2020, 15, e0222900. [Google Scholar] [CrossRef]
- Lutz, W.; KC, S. Dimensions of global population projections: What do we know about future population trends and structures? Philos. Trans. R. Soc. B Biol. Sci. 2010, 365, 2779–2791. [Google Scholar] [CrossRef]
- Marchi, S.; Trombetta, C.M.; Montomoli, E. Emerging and Re-emerging Arboviral Diseases as a Global Health Problem. In Public Health—Emerging and Re-emerging Issues; InTech: Winchester, UK, 2018. [Google Scholar]
- Lim, J.T.; Dickens, B.S.; Tan, K.W.; Koo, J.R.; Seah, A.; Ho, S.H.; Ong, J.; Rajarethinam, J.; Soh, S.; Cook, A.R.; et al. Hyperendemicity associated with increased dengue burden. J. R. Soc. Interface 2021, 18, 20210565. [Google Scholar] [CrossRef]
- Weetman, D.; Kamgang, B.; Badolo, A.; Moyes, C.L.; Shearer, F.M.; Coulibaly, M.; Pinto, J.; Lambrechts, L.; McCall, P.J. Aedes mosquitoes and Aedes-borne arboviruses in Africa: Current and future threats. Int. J. Environ. Res. Public Health 2018, 15, 220. [Google Scholar] [CrossRef]
- Hossain, M.S.; Raihan, M.E.; Hossain, M.S.; Syeed, M.M.M.; Rashid, H.; Reza, M.S. Aedes Larva Detection Using Ensemble Learning to Prevent Dengue Endemic. BioMedInformatics 2022, 2, 405–423. [Google Scholar] [CrossRef]
- Mahmood, I.; Jahan, M.; Groen, D.; Javed, A.; Shafait, F. An agent-based simulation of the spread of dengue fever. In Computational Science—ICCS 2020; Springer: Cham, Switzerland, 2020; pp. 103–117. [Google Scholar] [CrossRef]
- Ward, T.; Samuel, M.; Maoz, D.; Runge-Ranzinger, S.; Boyce, R.; Toledo, J.; Velayudhan, R.; Horstick, O. Dengue data and surveillance in Tanzania: A systematic literature review. Trop. Med. Int. Health 2017, 22, 960–970. [Google Scholar] [CrossRef] [PubMed]
- Mordecai, E.A.; Ryan, S.J.; Caldwell, J.M.; Shah, M.M.; LaBeaud, A.D. Climate change could shift disease burden from malaria to arboviruses in Africa. Lancet Planet Health 2020, 4, e416–e423. [Google Scholar] [CrossRef]
- Ahmed, A.; Ali, Y.; Mohamed, N.S. Arboviral diseases: The emergence of a major yet ignored public health threat in Africa. Lancet Planet Health 2020, 4, e555. [Google Scholar] [CrossRef] [PubMed]
- Kajeguka, D.C.; Desrochers, R.E.; Mwangi, R.; Mgabo, M.R.; Alifrangis, M.; Kavishe, R.A.; Mosha, F.W.; Kulkarni, M.A. Knowledge and practice regarding dengue and chikungunya: A cross-sectional study among Healthcare workers and community in Northern Tanzania. Trop. Med. Int. Health 2017, 22, 583–593. [Google Scholar] [CrossRef] [PubMed]
- Okada, K.; Morita, R.; Egawa, K.; Hirai, Y.; Kaida, A.; Shirano, M.; Kubo, H.; Goto, T.; Yamamoto, S.P. Dengue virus type 1 infection in traveler returning from Tanzania to Japan. Emerg. Infect. Dis. 2019, 25, 1782. [Google Scholar] [CrossRef]
- Rweyemamu, M.; Otim-Nape, W.; Serwadda, D. Foresight; Infections Diseases: Preparing for the Future: Africa; Office of Science and Innovation: London, UK, 2006.
- Hoogeveen, J.; Croke, K.; Dabalen, A.; Demombynes, G.; Giugale, M. Collecting high frequency panel data in Africa using mobile phone interviews. Can. J. Dev. Stud. Can. Détudes Dév. 2014, 35, 186–207. [Google Scholar] [CrossRef]
- Pascoe, L.; Mwangoka, J.W. A smartphone-based reporting application for routine health data: System requirements, analysis and design. Int. J. Telemed. Clin. Pract. 2016, 1, 323–344. [Google Scholar] [CrossRef]
- Sambo, L.G.; WHO. The Health of the People: What Works: The African Regional Health Report; World Health Organization: Geneva, Switzerland, 2014.
- Talaga, S.; Dejean, A.; Azémar, F.; Dumont, Y.; Leroy, C. Impacts of biotic and abiotic parameters on immature populations of Aedes aegypti. J. Pest Sci. 2020, 93, 941–952. [Google Scholar] [CrossRef]
- Liu, K. Improving Surveillance and Prediction of Emerging and Re-Emerging Infectious Diseases; The University of Texas at Austin: Austin, TX, USA, 2019; Available online: https://repositories.lib.utexas.edu/handle/2152/80616 (accessed on 6 April 2022).
- Kang, J.Y.; Aldstadt, J. The influence of spatial configuration of residential area and vector populations on dengue incidence patterns in an individual-level transmission model. Int. J. Environ. Res. Public Health 2017, 14, 792. [Google Scholar] [CrossRef]
- Marti, R.; Li, Z.; Carty, T.; Roux, E.; Mangeas, M.; Handschumacher, P.; Gaudart, J.; Tran, A.; Demagistri, L.; Faure, J.-F.; et al. A Mapping Review on Urban Landscape Factors of Dengue Retrieved from Earth Observation Data, GIS Techniques, and Survey Questionnaires. Remote Sens. 2020, 12, 932. [Google Scholar] [CrossRef]
- Cattarino, L.; Rodriguez-Barraquer, I.; Imai, N.; Cummings, D.A.T.; Ferguson, N.M. Mapping global variation in dengue transmission intensity. Sci. Transl. Med. 2020, 12, eaax4144. [Google Scholar] [CrossRef] [PubMed]
- Chipwaza, B.; Mugasa, J.P.; Selemani, M.; Amuri, M.; Mosha, F.; Ngatunga, S.D.; Gwakisa, P.S. Dengue and Chikungunya Fever among Viral Diseases in Outpatient Febrile Children in Kilosa District Hospital, Tanzania. PLoS Negl. Trop. Dis. 2014, 8, e3335. [Google Scholar] [CrossRef] [PubMed]
- Saravanabavan, V.; Balaji, D.; Reshma, C.U.; Sheheersha, S.K.; Sudharsan, R.; Vimala Vinnarasi, J.; Ganesan, J.; Nisha, R.R.; Eswari, S.; Balasubramani, K. Urban disease ecology and its spatial variation of Chikungunya in Madurai City, Tamilnadu, India: A geo-medical study. GeoJournal 2020, 86, 2335–2350. [Google Scholar] [CrossRef]
- Brinkel, J.; Krämer, A.; Krumkamp, R.; May, J.; Fobil, J. Mobile phone-based mHealth approaches for public health surveillance in sub-Saharan Africa: A systematic review. Int. J. Environ. Res. Public Health 2014, 11, 11559–11582. [Google Scholar] [CrossRef]
- Trewin, B.; Scientific, T.C. Assessing the Risk of Establishment by the Dengue Vector, Aedes aegypti (L.) (Diptera: Culicidae), through rainwater tanks in Queensland: Back to the Assessing the Risk of Establishment by the Dengue Vector, Aedes aegypti (L.) Diptera: Culicid. Ph.D. Thesis, The University of Queensland, Brisbane, QLD, Australia, 2018. [Google Scholar]
- Trewin, B.J.; Darbro, J.M.; Jansen, C.C.; Schellhorn, N.A.; Zalucki, M.P.; Hurst, T.P.; Devine, G.J. The elimination of the dengue vector, Aedes aegypti, from Brisbane, Australia: The role of surveillance, larval habitat removal and policy. PLoS Negl. Trop. Dis. 2017, 11, e0005848. [Google Scholar] [CrossRef]
- Kraemer, M.U.G.; Sinka, M.E.; Duda, K.A.; Mylne, A.Q.N.; Shearer, F.M.; Barker, C.M.; Moore, C.G.; Carvalho, R.G.; Coelho, G.E.; Van Bortel, W.; et al. The global distribution of the arbovirus vectors Aedes aegypti and Ae. Albopictus. Elife 2015, 4, e08347. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Abubakr, M.; Sami, H.; Mahdi, I.; Mohamed, N.S.; Zinsstag, J. The First Molecular Detection of Aedes albopictus in Sudan Associates with Increased Outbreaks of Chikungunya and Dengue. Int. J. Mol. Sci. 2022, 23, 11802. [Google Scholar] [CrossRef]
- Martín, M.E.; Alonso, A.C.; Faraone, J.; Stein, M.; Estallo, E.L. Satellite observation to assess dengue risk due to Aedes aegypti and Aedes albopictus in a subtropical city of Argentina. Med. Vet. Entomol. 2022, 1–10. [Google Scholar] [CrossRef]
- Benitez, E.M.; Estallo, E.L.; Grech, M.G.; Frías-Céspedes, M.; Almirón, W.R.; Robert, M.A.; Luduena-Almeida, F.F. Understanding the role of temporal variation of environmental variables in predicting Aedes aegypti oviposition activity in a temperate region of Argentina. Acta Trop. 2021, 216, 105744. [Google Scholar] [CrossRef]
- Benitez, E.M.; Ludueña-Almeida, F.; Frías-Céspedes, M.; Almirón, W.R.; Estallo, E.L. Could land cover influence Aedes aegypti mosquito populations? Med. Vet. Entomol. 2020, 34, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Kajeguka, D.C.; Msonga, M.; Schiøler, K.L.; Meyrowitsch, D.W.; Syrianou, P.; Tenu, F.; Alifrangis, M.; Mosha, F.W.; Kavishe, R.A. Individual and environmental risk factors for dengue and chikungunya seropositivity in North-Eastern Tanzania. Infect. Dis. Health 2017, 22, 65–76. [Google Scholar] [CrossRef]
- Mardekian, S.K.; Roberts, A.L. Diagnostic Options and Challenges for Dengue and Chikungunya Viruses. BioMed Res. Int. 2015, 2015, 834371. [Google Scholar] [CrossRef]
- Ahmed, A.; Ali, Y.; Elmagboul, B.; Mohamed, O.; Elduma, A.; Bashab, H.; Mahamoud, A.; Khogali, H.; Elaagip, A.; Higazi, T. Dengue fever in the Darfur area, Western Sudan. Emerg. Infect. Dis. 2019, 25, 2125–2126. [Google Scholar] [CrossRef] [PubMed]
- Paupy, C.; Ollomo, B.; Kamgang, B.; Moutailler, S.; Rousset, D.; Demanou, M.; Hervé, J.P.; Leroy, E.; Simard, F. Comparative role of aedes albopictus and aedes aegypti in the emergence of dengue and chikungunya in central Africa. Vector-Borne Zoonotic Dis. 2010, 10, 259–266. [Google Scholar] [CrossRef]
- Puthanakit, T.; Anugulruengkitt, S.; Jantarabenjakul, W. Prevention of Emerging Infections in Children. Pediatr. Clin. N. Am. 2022, 69, 185–202. [Google Scholar] [CrossRef] [PubMed]
- Dumont, Y.; Chiroleu, F.; Domerg, C. On a temporal model for the Chikungunya disease: Modeling, theory and numerics. Math. Biosci. 2008, 213, 80–91. [Google Scholar] [CrossRef]
- Tancredi, A.; Papandrea, D.; Marconcini, M.; Carballar-Lejarazu, R.; Casas-Martinez, M.; Lo, E.; Chen, X.-G.; Malacrida, A.R.; Bonizzoni, M. Tracing temporal and geographic distribution of resistance to pyrethroids in the arboviral vector aedes albopictus. PLoS Negl. Trop. Dis. 2020, 14, e0008350. [Google Scholar] [CrossRef]
- Rezza, G.; Nicoletti, L.; Angelini, R.; Romi, R.; Finarelli, A.C.; Panning, M.; Cordioli, P.; Fortuna, C.; Boros, S.; Magurano, F.; et al. Infection with chikungunya virus in Italy: An outbreak in a temperate region. Lancet 2007, 370, 1840–1846. [Google Scholar] [CrossRef] [PubMed]
- Macal, C.M.; North, M.J. Agent-based modeling and simulation. In Proceedings of the Winter Simulation Conference, Austin, TX, USA, 13–16 December 2009; pp. 86–98. [Google Scholar]
- Macal, C.M.; North, M.J. Tutorial on Agent-Based Modeling and Simulation. In Proceedings of the 2005 Winter Simulation Conference, Orlando, FL, USA, 4 December 2005; pp. 1643–1649. [Google Scholar] [CrossRef]
- Macal, C.; North, M. Introductory tutorial: Agent-based modeling and simulation. In Proceedings of the Winter Simulation Conference, Savannah, GA, USA, 7–10 December 2014; pp. 6–20. [Google Scholar]
- Sabzian, H.; Shafia, M.A.; Maleki, A.; Hashemi, S.M.S.; Baghaei, A.; Gharib, H. Theories and practice of agent based modeling: Some practical implications for economic planners. arXiv 2019, arXiv:190108932. [Google Scholar]
- Kasaie, P.; Kelton, W.D. Guidelines for design and analysis in agent-based simulation studies. In Proceedings of the Winter Simulation Conference, Huntington Beach, CA, USA, 6–9 December 2015; pp. 183–193. [Google Scholar]
- Clarke, K.C. Cellular automata and agent-based models. In Handbook of Regional Science; Springer: Berlin/Heidelberg, Germany, 2014; pp. 1217–1233. [Google Scholar]
- Crooks, A.; Heppenstall, A.; Malleson, N. Agent-Based Modeling. Compr. Geogr. Inf. Syst. 2017, 3, 218–243. [Google Scholar]
- Eisinger, D.; Thulke, H.H. Spatial pattern formation facilitates eradication of infectious diseases. J. Appl. Ecol. 2008, 45, 415–423. [Google Scholar] [CrossRef]
- Railsback; Steven, F.; Grimm, V. An Agent-Based and Individual-Based Modelling: A Practical Introduction; Princeton University Press: Princeton, NJ, USA, 2017. [Google Scholar]
- Jacintho, L.F.O.; Batista, A.F.M.; Ruas, T.L.; Marietto, M.G.B.; Silva, F.A. An agent-based model for the spread of the Dengue fever: A swarm platform simulation approach. In Proceedings of the 2010 Spring Simulation Multiconference, Orlando, FL, USA, 11–15 April 2010; pp. 1–8. [Google Scholar]
- Stiner, S.; Chellamuthu, V. An Agent-Based Model of West Nile Virus: Predicting the Impact of Public Health Agents and Vaccinations on Horses. Curiosit. Interdiscip. J. Res. Innov. 2020, 1, 44–66. [Google Scholar] [CrossRef]
- Mniszewski, S.M.; Manore, C.A.; Bryan, C.; Del Valle, S.Y.; Roberts, D. Towards a hybrid agent-based model for mosquito borne disease. Simul. Ser. 2014, 46, 66–73. [Google Scholar]
- Alam, M.Z.; Niaz Arifin, S.M.; Al-Amin, H.M.; Alam, M.S.; Rahman, M.S. A spatial agent-based model of Anopheles vagus for malaria epidemiology: Examining the impact of vector control interventions. Malar. J. BioMed Cent. 2017, 16, 432. [Google Scholar] [CrossRef]
- Tennant, W.; McKinley, T.; Recker, M. Inferring the ecological drivers of arboviral outbreaks. bioRxiv 2019. [Google Scholar] [CrossRef]
- Paaijmans, K.P.; Imbahale, S.S.; Thomas, M.B.; Takken, W. Relevant microclimate for determining the development rate of malaria mosquitoes and possible implications of climate change. Malar. J. 2010, 9, 196. [Google Scholar] [CrossRef]
- Reiner, R.C.; Perkins, T.A.; Barker, C.M.; Niu, T.; Chaves, L.F.; Ellis, A.M.; George, D.B.; Le Menach, A.; Pulliam, J.R.C.; Bisanzio, D.; et al. A systematic review of mathematical models of mosquito-borne pathogen transmission: 1970–2010. J. R. Soc. Interface 2013, 10, 20120921. [Google Scholar] [CrossRef]
- Ingabire, E.M.; Kimura, M. Effect Analysis of Climate Change on the Reproduction of Mosquitoes and Infection Rate Sensitivity for SI/SIR Epidemical Model in the Case of Malaria Disease. Int. J. Pharma Med. Biol. Sci. 2020, 9, 47–51. [Google Scholar] [CrossRef]
- Kapwata, T.; Wright, C.Y.; du Preez, D.J.; Kunene, Z.; Mathee, A.; Ikeda, T.; Landman, W.; Maharaj, R.; Sweijd, N.; Minakawa, N.; et al. Exploring rural hospital admissions for diarrhoeal disease, malaria, pneumonia, and asthma in relation to temperature, rainfall and air pollution using wavelet transform analysis. Sci. Total Environ. 2021, 791, 148307. [Google Scholar] [CrossRef] [PubMed]
- Tourre, Y.M.; Vignolles, C.; Viel, C.; Mounier, F. Climate impact on malaria in northern Burkina Faso. Geospat. Health 2017, 12, 351–359. [Google Scholar] [CrossRef]
- Mukhtar, A.Y.A.; Munyakazi, J.B.; Ouifki, R. Assessing the role of climate factors on malaria transmission dynamics in South Sudan. Math. Biosci. 2019, 310, 13–23. [Google Scholar] [CrossRef]
- Rumisha, S.F.; Smith, T.; Abdulla, S.; Masanja, H.; Vounatsou, P. Modelling heterogeneity in malaria transmission using large sparse spatio-temporal entomological data. Glob. Health Act. 2014, 7, 22682. [Google Scholar] [CrossRef]
- Colón-González, F.J.; Tompkins, A.M.; Biondi, R.; Bizimana, J.P.; Namanya, D.B. Assessing the effects of air temperature and rainfall on malaria incidence: An epidemiological study across Rwanda and Uganda. Geospat. Health 2016, 11, 379. [Google Scholar] [CrossRef] [PubMed]
- Wearing, H.J.; Robert, M.A.; Christofferson, R.C. Dengue and chikungunya: Modelling the expansion of mosquito-borne viruses into naïve populations. Parasitology 2016, 143, 860–873. [Google Scholar] [CrossRef]
- Deza-Cruz, I. Epidemiology of Dengue, Chikungunya and Zika in a Naïve Population in St. Kitts, West Indies. Ph.D. Thesis, School of Natural and Environment Sciences, Newcastle University, Newcastle, DE, USA, Ross University of School of Veterinary Medicine, St. Kitts, West Indies, 2018. [Google Scholar]
- Dommar, C.J.; Lowe, R.; Robinson, M.; Rodó, X. An agent-based model driven by tropical rainfall to understand the spatio-temporal heterogeneity of a chikungunya outbreak. Acta Trop. 2014, 129, 61–73. [Google Scholar] [CrossRef] [PubMed]
- Center DHD. Annual Meeting Report. In Proceedings of the SWARMFEST 2016: 20th Annual Meeting on Agent Based Modeling & Simulation, Burlington, VT, USA, 31 July–3 August 2016. [Google Scholar]
- Anders, K.L. The Epidemiology of Dengue in Southern Vietnam: Distribution of Disease and Determinants of Risk in an Endemic Setting. Ph.D. Thesis, Monash University, Victoria, Australia, 2015. [Google Scholar]
- Borges, F.; Gutierrez-milla, A.; Suppi, R.; Luque, E.; de Brito Arduino, M. An Agent-Based Model for Assessment of Aedes Aegypri Pupal Productivity. In Proceedings of the 2015 Winter Simulation Conference, Huntington Beach, CA, USA, 6–9 December 2015; pp. 159–170. [Google Scholar]
- Maneerat, S.; Daudé, E. A spatial agent-based simulation model of the dengue vector Aedes aegypti to explore its population dynamics in urban areas. Ecol. Model. 2016, 333, 66–78. [Google Scholar] [CrossRef]
- Mulyani, H.; Djatna, T.; Sitanggang, I.S. Agent Based Modeling on Dynamic Spreading Dengue Fever Epidemic. TELKOMNIKA Telecommun. Comput. Electron. Control 2017, 15, 1380–1388. [Google Scholar] [CrossRef]
- Deng, C.; Tao, H.; Ye, Z. Agent-based modeling to simulate the dengue spread. In Proceedings of the Geoinformatics 2008 and Joint Conference on GIS and Built Environment: Geo-Simulation and Virtual GIS Environments, 28–29 June 2008; Volume 7143, p. 71431O. [Google Scholar]
- Rodríguez RRC. Enhancing Dengue Fever Modeling Through a Multi-Scale Analysis Framework—A Case Study in the Central Valley of Costa Rica. Ph.D. Thesis, Texas State University-San Marcos, San Marcos, TX, USA, 2013. [Google Scholar]
- Manore, C.A.; Hickmann, K.S.; Hyman, J.M.; Foppa, I.M.; Davis, J.K.; Wesson, D.M.; Mores, C.N. A network-patch methodology for adapting agent-based models for directly transmitted disease to mosquito-borne disease. J. Biol. Dyn. 2015, 9, 52–72. [Google Scholar] [CrossRef]
- Goindin, D.; Delannay, C.; Ramdini, C.; Gustave, J.; Fouque, F. Parity and longevity of aedes aegypti according to temperatures in controlled conditions and consequences on dengue transmission risks. PLoS ONE 2015, 10, e0135489. [Google Scholar] [CrossRef] [PubMed]
- Cronjé, B.J. A Framework to Support the Decision-Making Process for Modelling of Communicable Diseases. Master’s Thesis, Stellenbosch University, Western Cape, South Africa, 2019. Available online: http://scholar.sun.ac.za/handle/10019.1/105815 (accessed on 8 April 2022).
- Lambrechts, L.; Paaijmans, K.P.; Fansiri, T.; Carrington, L.B.; Kramer, L.D.; Thomas, M.B.; Scott, T.W. Impact of daily temperature fluctuations on dengue virus transmission by Aedes aegypti. Proc. Natl. Acad. Sci. USA 2011, 108, 7460–7465. [Google Scholar] [CrossRef]
- Lai, S.; Huang, Z.; Zhou, H.; Anders, K.L.; Perkins, T.A.; Yin, W.; Li, Y.; Mu, D.; Chen, Q.; Zhang, Z.; et al. The changing epidemiology of dengue in China, 1990-2014: A descriptive analysis of 25 years of nationwide surveillance data. BMC Med. 2015, 13, 100. [Google Scholar] [CrossRef] [PubMed]
- Whitehorn, J.; Yacoub, S.; Anders, K.L.; Macareo, L.R.; Cassetti, M.C.; Nguyen Van, V.C.; Shi, P.-Y.; Wills, B.; Simmons, C.P. Dengue Therapeutics, Chemoprophylaxis, and Allied Tools: State of the Art and Future Directions. PLoS Negl. Trop. Dis. 2014, 8, e3025. [Google Scholar] [CrossRef] [PubMed]
- Alto, B.W.; Juliano, S.A. Precipitation and temperature effects on populations of Aedes albopictus (Diptera: Culicidae): Implications for range expansion. J. Med. Entomol. 2001, 38, 646–656. [Google Scholar] [CrossRef]
- Liu, Y.; Li, Y.; Li, S.; Motesharrei, S. Spatial and Temporal Patterns of Global NDVI Trends: Correlations with Climate and Human Factors. Remote Sens. 2015, 7, 13233–13250. [Google Scholar] [CrossRef]
- Estallo, E.L.; Ludueña-Almeida, F.F.; Visintin, A.M.; Scavuzzo, C.M.; Lamfri, M.A.; Introini, M.V.; Zaidenberg, M.; Almirón, W.R. Effectiveness of normalized difference water index in modelling Aedes aegypti house index. Int. J. Remote Sens. 2012, 33, 4254–4265. [Google Scholar] [CrossRef]
- Mweya, C.N.; Kimera, S.I.; Stanley, G.; Misinzo, G.; Mboera, L.E.G. Climate change influences potential distribution of infected Aedes aegypti co-occurrence with dengue epidemics risk areas in Tanzania. PLoS ONE 2016, 11, e0162649. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.; Karki, S.; Smith, R.L.; Brown, W.M.; Ruiz, M.O.H. The spread of mosquito-borne viruses in modern times: A spatio-temporal analysis of dengue and chikungunya. Spat. Spatiotemporal Epidemiol. 2018, 26, 113–125. [Google Scholar] [CrossRef]
- Metelmann, S.; Liu, X.; Lu, L.; Caminade, C.; Liu, K.; Cao, L.; Medlock, J.M.; Baylis, M.; Morse, A.P.; Liu, Q. Assessing the suitability for aedes albopictus and dengue transmission risk in china with a delay differential equation model. PLoS Negl. Trop. Dis. 2021, 15, e0009153. [Google Scholar] [CrossRef]
- Weyl, J.; Glake, D.; Clemen, T. Agent-based traffic simulation at city scale with MARS. In Proceedings of the Agent-Directed Simulation Symposium, Baltimore, MD, USA, 15–18 April 2018; pp. 1–9. [Google Scholar]
- Glake, D.; Panse, F.; Ritter, N.; Clemen, T.; Lenfers, U.A. Data Management in Multi-Agent Simulation Systems from Challenges to First Solutions. In Proceedings of the Datenbanksysteme für Business, Technol und Web {(BTW)}, 19 Fachtagung des GI-Fachbereichs Datenbanken und Informationssysteme, Bonn, Germany, 13–17 September 2021; pp. 11–20. [Google Scholar]
- Hüning, C.; Jason, W.; Clemen, T. MARS—A next-gen multi-agent simulation framework. In Proceedings of the Simulation Umwelt-und Geowissenschaften, Work Osnabrück; Wittmann, J., Maretis, D., Eds.; Shaker: Aachen, Germany, 2014; pp. 1–14. [Google Scholar]
- Beier, J.C.; Keating, J.; Githure, J.I.; MacDonald, M.B.; Impoinvil, D.E.; Novak, R.J. Integrated vector management for malaria control. Malar. J. 2008, 7, S4. [Google Scholar] [CrossRef]
- WHO. Toolkit for Integrated Vector Management in Sub-Saharan Africa (A); World Health Organization: Geneva, Switzerland, 2016.
- Rafikov, M.; Rafikova, E.; Yang, H.M. Optimization of the Aedes aegypti control strategies for integrated vector management. J. Appl. Math. 2015, 2015, 918194. [Google Scholar] [CrossRef]
- Li, R.; Xu, L.; Bjørnstad, O.N.; Liu, K.; Song, T.; Chen, A.; Xu, B.; Liu, Q.; Stenseth, N.C. Climate-driven variation in mosquito density predicts the spatiotemporal dynamics of dengue. Proc. Natl. Acad. Sci. USA 2019, 116, 3624–3629. [Google Scholar] [CrossRef] [PubMed]
- Castro, L.A.; Fox, S.J.; Chen, X.; Liu, K.; Bellan, S.E.; Dimitrov, N.B.; Galvani, A.P.; Meyers, L.A. Assessing real-time Zika risk in the United States. BMC Infect Dis. 2017, 17, 284. [Google Scholar] [CrossRef] [PubMed]
- Trewin, B.; Parry, H.; Zalucki, M.; Westcott, D.; Shellhorn, N. The Challenges of Developing Spatially Explicit Network Models for the Management of Disease Vectors in Ecological Systems. In Proceedings of the International Conference on Formal Methods in Macro-Biology, Nouméa, New Caledonia, 22–24 September 2014; pp. 159–161. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pascoe, L.; Clemen, T.; Bradshaw, K.; Nyambo, D. Review of Importance of Weather and Environmental Variables in Agent-Based Arbovirus Models. Int. J. Environ. Res. Public Health 2022, 19, 15578. https://doi.org/10.3390/ijerph192315578
Pascoe L, Clemen T, Bradshaw K, Nyambo D. Review of Importance of Weather and Environmental Variables in Agent-Based Arbovirus Models. International Journal of Environmental Research and Public Health. 2022; 19(23):15578. https://doi.org/10.3390/ijerph192315578
Chicago/Turabian StylePascoe, Luba, Thomas Clemen, Karen Bradshaw, and Devotha Nyambo. 2022. "Review of Importance of Weather and Environmental Variables in Agent-Based Arbovirus Models" International Journal of Environmental Research and Public Health 19, no. 23: 15578. https://doi.org/10.3390/ijerph192315578
APA StylePascoe, L., Clemen, T., Bradshaw, K., & Nyambo, D. (2022). Review of Importance of Weather and Environmental Variables in Agent-Based Arbovirus Models. International Journal of Environmental Research and Public Health, 19(23), 15578. https://doi.org/10.3390/ijerph192315578









