Test of the Rehabilitation Goal Screening (ReGoS) Tool to Support Decision Making and Goal Setting in Physical and Rehabilitation Medicine Practice
Abstract
1. Introduction
- Lack of time to talk about the details of the patient’s life situation, personal expectations and priorities as well as contextual factors;
- Lack of unbiased information from the patient (who will be easily influenced by the doctor’s convictions, at least in the first few consultations and before confidence can grow);
- The fact that sum-scores as outcomes of assessment tools are not useful for goal setting;
- The fact that besides the patient’s health condition, function-related goals must be taken into account, especially with regard to activities, participation and the modification of contextual factors;
- The difficulty in reducing multiple expectations to a “leading” goal that can be used for follow-up goal attainment.
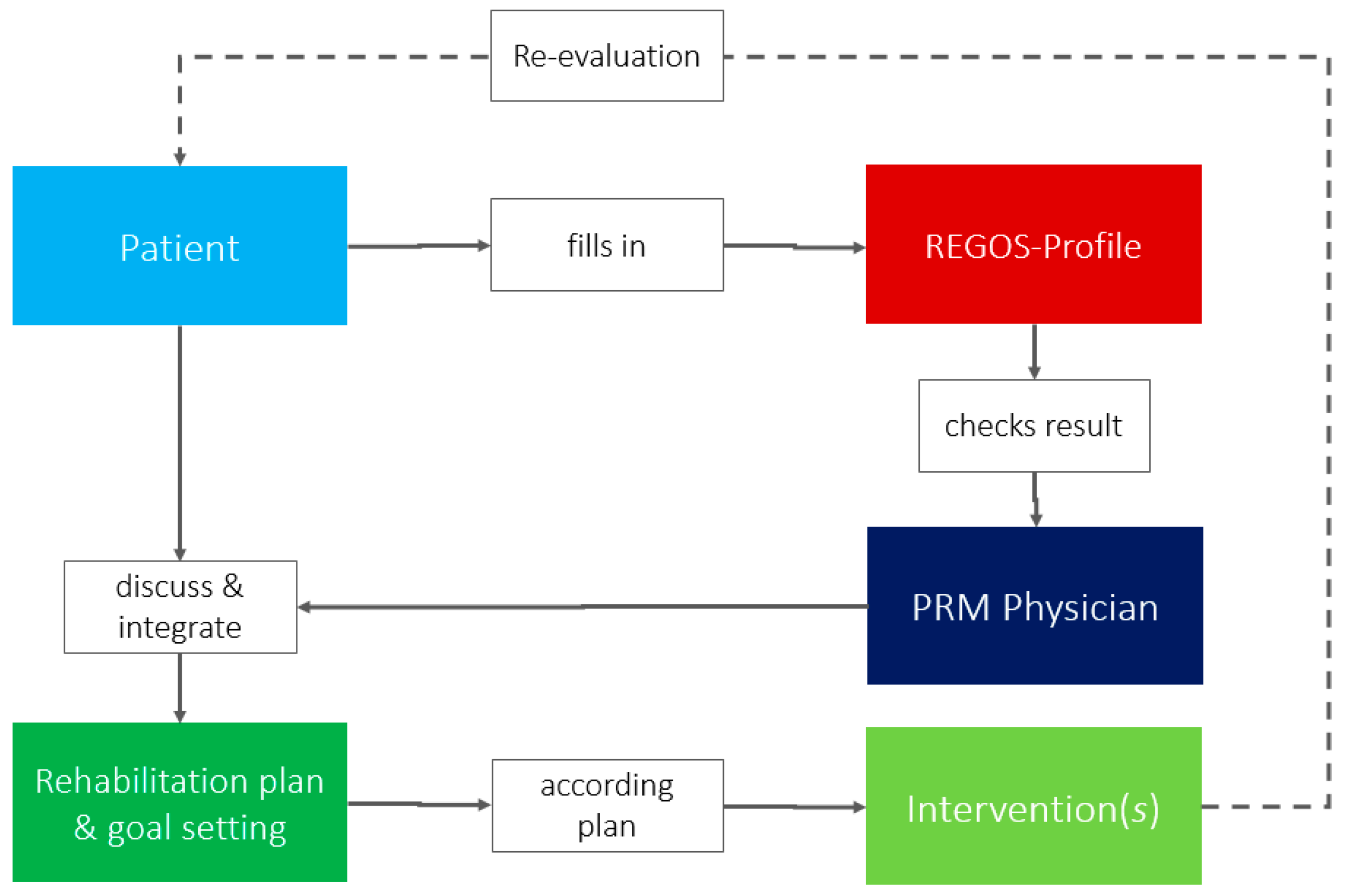
- Obtain the patients’ own and unbiased perspective before discussion with the MD;
- Support the negotiation process between patient and MD with regard to goal setting;
- Support a patient-centered interview and facilitate shared decision making;
- Support efficient time management in outpatient rehabilitation practices.
2. Materials and Methods
- The tool should provide information on the most relevant aspects of functioning.
- The information gathered should reflect the patient’s individual rehabilitation goals.
- The tool should use plain language so that the patient is able to fill in the questionnaire without any external support.
- The patient should be given the opportunity to think about and formulate his or her individual goals.
- The result of the questionnaire should be transferable to a profile that can be interpreted by the doctor at a glance.
- The results of the screening must be available immediately as a basis for goal setting negotiation.
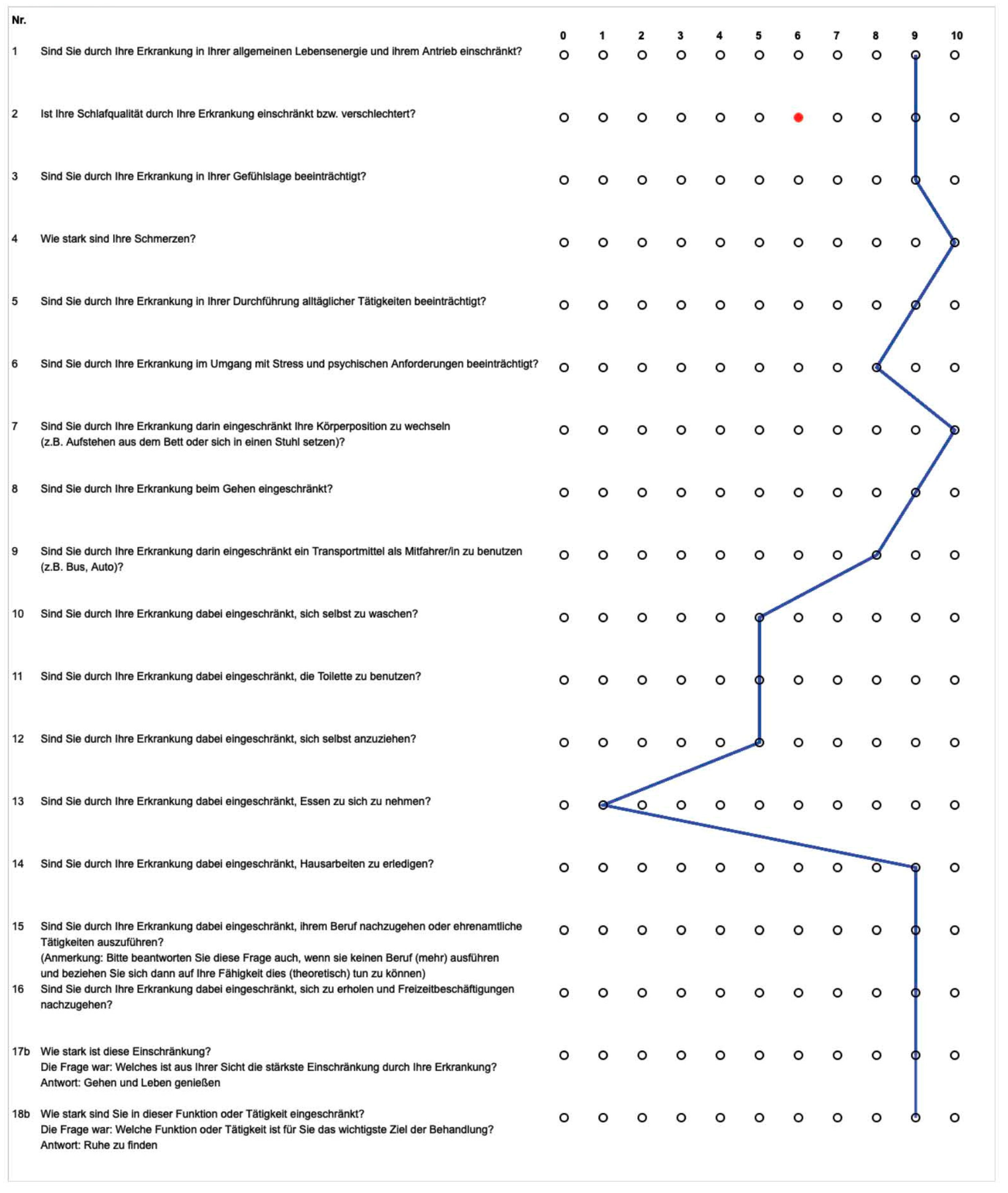
- Selection of not more than 20 items by two experienced PRM physicians according to the criteria, using only one item that can represent a group of categories (e.g., out of washing, dressing and taking care of body parts);
- Translate the selected categories into questions written in plain language;
- Use a Likert scale to enable a differentiated graphical profile;
- Include a question on the patient’s own top-priority rehabilitation goals and ask them to rate these goals on another Likert scale.
2.1. Case Study as Practical Example
2.2. Participants and Setting
2.2.1. Subjective Work Ability
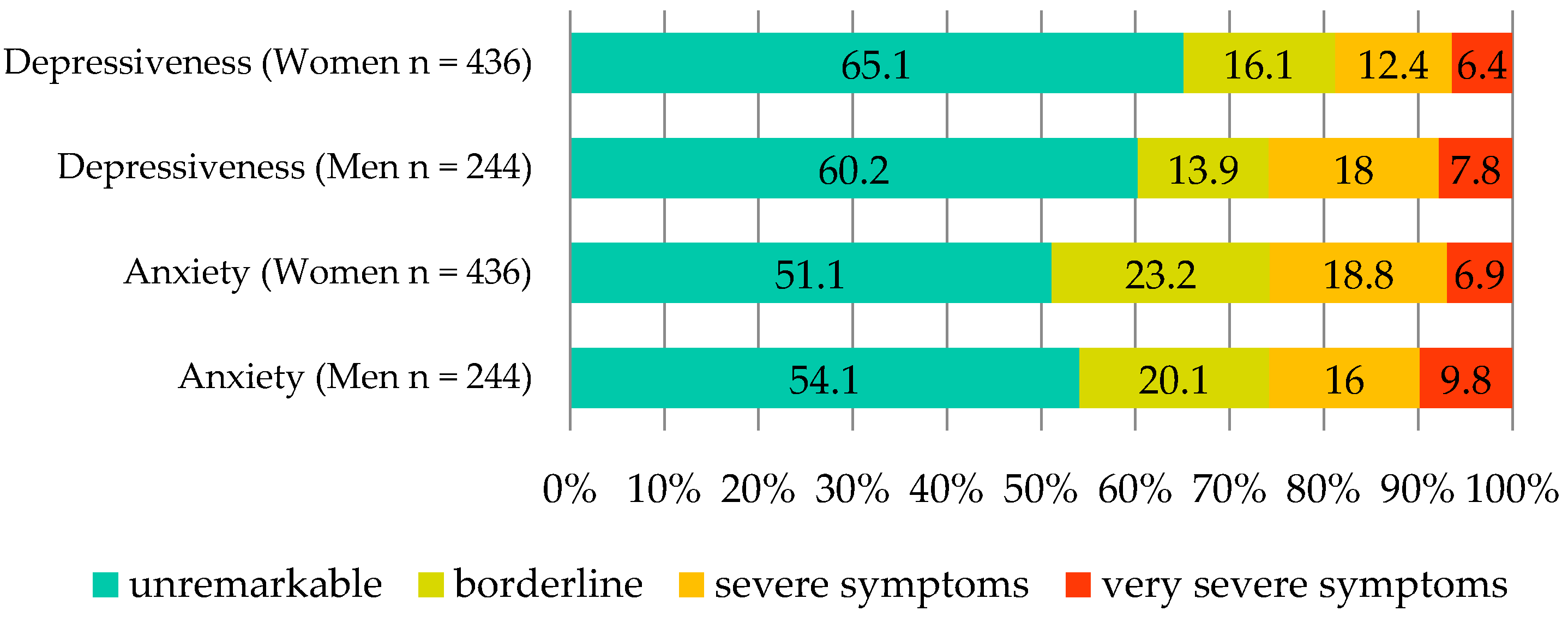
2.2.2. Mental Condition
- -
- <7 = unremarkable;
- -
- 8–10 = borderline;
- -
- 11–14 = severe symptomatology;
- -
- 15–21 = very severe symptomatology.
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic Data
3.2. Anxiety and Depressiveness (HADS)
3.3. Work Ability (WAI)
3.4. Main Diagnoses (ICD)
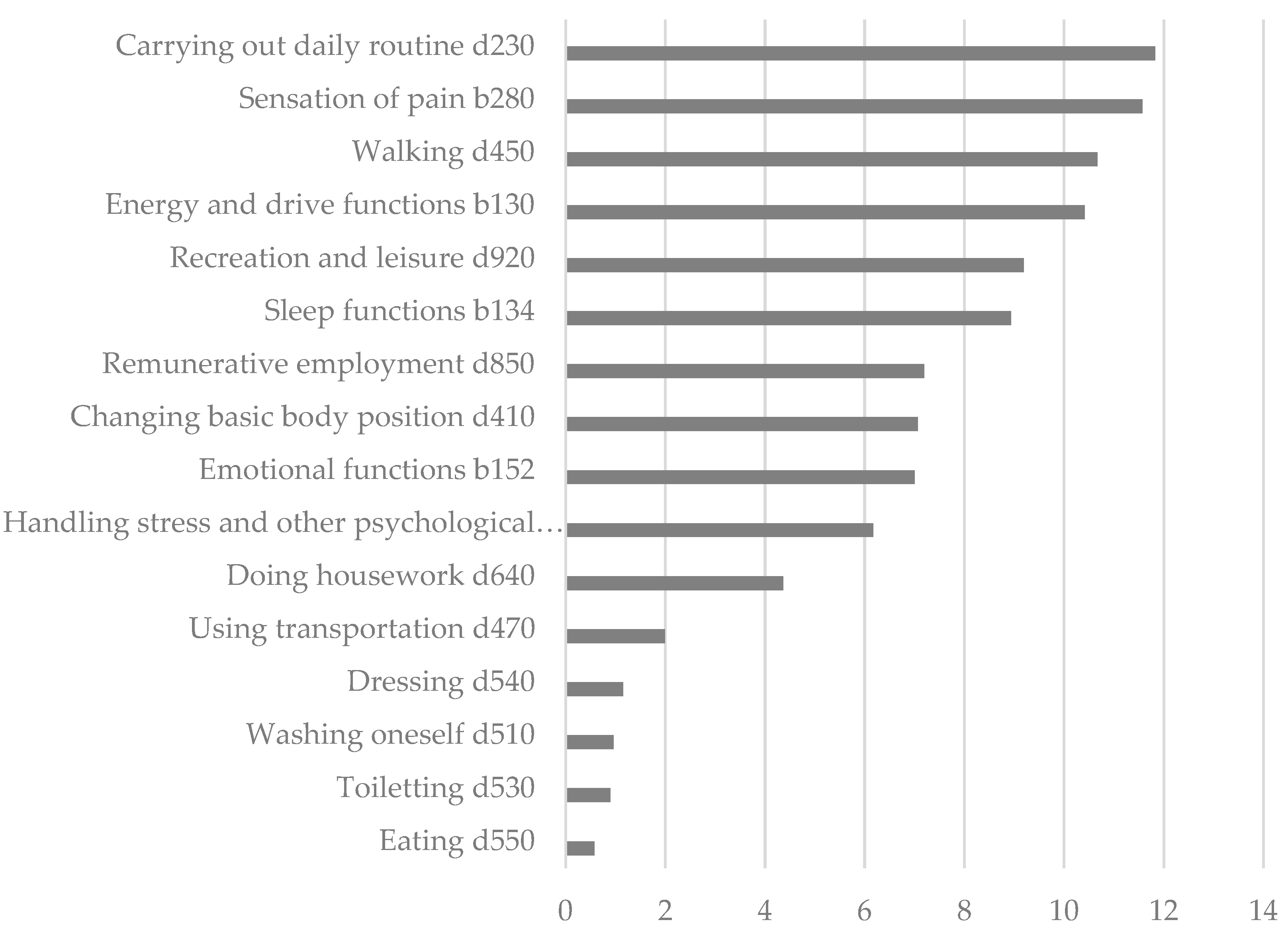
3.5. Detailed Functioning Profile and Free Texts of the Study Cohort
3.6. Rehabilitation Goals
3.7. Internal Consistency of ReGoS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wade, D.T. Goal setting in rehabilitation: An overview of what, why and how. Clin. Rehabil. 2009, 23, 291–295. [Google Scholar] [CrossRef]
- Levack, W.M.M.; Weatherall, M.; Hay-Smith, E.J.C.; Dean, S.G.; McPherson, K.; Siegert, R.J. Goal setting and strategies to enhance goal pursuit for adults with acquired disability participating in rehabilitation. Cochrane Database Syst. Rev. 2015, 2015, CD009727. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2001.
- Liu, S.; Reinhardt, J.D.; Zhang, X.; Ehrmann, C.; Cai, W.; Prodinger, B.; Liu, S.; Li, J. System-wide clinical assessment of functioning based on the International Classification of Functioning, Disability and Health in China: Interrater reliability, convergent, known group, and predictive validity of the ICF Generic-6. Arch. Phys. Med. Rehabil. 2019, 100, 1450–1457.e1. [Google Scholar] [CrossRef]
- Senju, Y.; Mukaino, M.; Ozeki, M.; Watanabe, M.; Okochi, Y.; Mizutani, K.; Saito, E.; Sonoda, S. Interrater agreement between clinician ratings and patient self-assessments for body function categories of ICF Rehabilitation Set. Jpn. J. Compr. Rehabil.-Sci. 2020, 11, 9–16. [Google Scholar] [CrossRef]
- Linden, M.; Keller, L.; Noack, N.; Muschalla, B. Self-rating of capacity limitations in mental disorders: The “Mini-ICF-APP-S”. Behav. Med. Rehabil. Pract. 2018, 101, 14–22. [Google Scholar]
- Cieza, A.; Oberhauser, C.; Bickenbach, J.; Chatterji, S.; Stucki, G. Towards a minimal generic set of domains of functioning and health. BMC Public Health 2014, 14, 218. [Google Scholar] [CrossRef] [PubMed]
- Prodinger, B.; Cieza, A.; Oberhauser, C.; Bickenbach, J.; Üstün, T.B.; Chatterji, S.; Chatterji, S.; Stucki, G. Toward the international classification of functioning, disability and health (ICF) rehabilitation set: A minimal generic set of domains for rehabilitation as a health strategy. Arch. Phys. Med. Rehabil. 2016, 97, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Ilmarinen, J. Work ability—A comprehensive concept for occupational health research and prevention. Scand. J. Work Environ. Health 2009, 35, 1–5. [Google Scholar] [CrossRef]
- Hermann-Lingen, C. Hospital Anxiety and Depression Scale—Deutsche Version; Hogrefe-Verlag: Göttingen, Germany, 2011. [Google Scholar]
- Hasselhorn, H.M.; Freude, F.G. Der Work Ability Index. Ein Leitfaden. Schriftenreihe der Bundesanstalt für Arbeitsschutz und Arbeitsmedizin: Sonderschrift; Wirtschaftsverlag: Wien, Austria, 2007; p. 87. [Google Scholar]
- INQA-WAI-Netzwerk. Available online: https://www.wainetzwerk.de/uploads/z-neue%20Uploads/WAI-Netzwerk/WAI%20Fragebogen/NEU_WAI-Langversion%20mit%20Auswertung%202021.pdf (accessed on 29 September 2022).
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Cieza, A.; Geyh, S.; Chatterji, S.; Kostanjsek, N.; Üstün, B.; Stucki, G. ICF linking rules: An update based on lessons learned. J. Rehabil. Med. 2005, 37, 212–218. [Google Scholar] [CrossRef]
- Stucki, G.; Cieza, A.; Melvin, J. The international classification of functioning, disability and health: A unifying model for the conceptual description of the rehabilitation strategy. J. Rehabil. Med. 2007, 39, 279–285. [Google Scholar] [CrossRef]
- Rauch, A.; Cieza, A.; Stucki, G. How to apply the International Classification of Functioning, Disability and Health (ICF) for rehabilitation management in clinical practice. Eur. J. Phys. Rehabil. Med. 2008, 44, 329–342. [Google Scholar]
- Gimigliano, F.; De Sire, A.; Gastaldo, M.; Maghini, I.; Paoletta, M.; Pasquini, A.; Boldrini, P.; Selb, M.; Prodinger, B. SIMFER Residents Section Group. Use of the International Classification of Functioning, Disability and Health Generic-30 Set for the characterization of outpatients: Italian Society of Physical and Rehabilitative Medicine Residents Section Project. Eur. J. Phys. Rehabil. Med. 2019, 55, 258–264. [Google Scholar] [CrossRef]
- Li, J.; Prodinger, B.; Reinhardt, J.; Stucki, G. Towards the system-wide implementation of the International Classification of Functioning, Disability and Health in routine practice: Lessons from a pilot study in China. J. Rehabil. Med. 2016, 48, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Gutenbrunner, C.; Lemoine, F.; Yelnik, A.; Joseph, P.-A.; de Korvin, G.; Neumann, V.; Delarque, A. The field of competence of the specialist in physical and rehabilitation medicine (PRM). Ann. Phys. Rehabil. Med. 2011, 54, 298–318. [Google Scholar] [CrossRef] [PubMed]
- Plass, D.; Vos, T.; Hornberg, C.; Scheidt-Nave, C.; Zeeb, H.; Krämer, A. Trends in disease burden in Germany: Results, implications and limitations of the Global Burden of Disease study. Dtsch. Ärzteblatt Int. 2014, 111, 629. [Google Scholar]
- Hinz, A.; Brähler, E. Normative values for the hospital anxiety and depression scale (HADS) in the general German population. J. Psychosom. Res. 2011, 71, 74–78. [Google Scholar] [CrossRef]
- Phongamwong, C.; Deema, H. The impact of multi-site musculoskeletal pain on work ability among health care providers. J. Occup. Med. Toxicol. 2015, 10, 1–5. [Google Scholar] [CrossRef][Green Version]
- Rashid, M.; Heiden, M.; Nilsson, A.; Kristofferzon, M. Do work ability and life satisfaction matter for return to work? Predictive ability of the work ability index and life satisfaction questionnaire among women with long-term musculoskeletal pain. BMC Public Health 2021, 21, 1–9. [Google Scholar] [CrossRef]
- de Vries, H.J.; Reneman, M.F.; Groothoff, J.W.; Geertzen, J.H.B.; Brouwer, S. Self-reported work ability and work performance in workers with chronic nonspecific musculoskeletal pain. J. Occup. Rehabil. 2013, 23, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Leijten, F.R.M.; van den Heuvel, S.G.; Ybema, J.F.; van der Beek, A.J.; Robroek, S.J.W.; Burdorf, A. The influence of chronic health problems on work ability and productivity at work: A longitudinal study among older employees. Scand. J. Work Environ. Health 2014, 40, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Hinton, P.R. Statistics Explained; Routledge: London, UK, 2014. [Google Scholar]

| Sociodemographic Sample Characteristics | N = 1.008 |
|---|---|
| Age in years, M (SD) | 53.9 (16.2) |
| Gender, n (%) | |
| Female | 665 (66.0) |
| Male | 343 (34.0) |
| Employed, n (%) | |
| Yes | 487 (48.3) |
| No | 521 (51.7) |
| Patient’s ID | Function or Activity with the Greatest Limitation | Severity | Most Important Treatment Goal (Function or Activity) | Severity |
|---|---|---|---|---|
| ID xxxxxx8310 | “walking and standing” | 8 | “To be able to walk properly again. I have the feeling that I am not moving forward properly.” | 8 |
| ID xxxxxx0420 | “Lack of strength in the hands. Fine motor skills severely limited.” | 5 | “Avoid further ulnar deviation” | 5 |
| ID xxxxxx5220 | “Many trips to the toilet during activities and mental problems. Infection of the urinary tract.” | 3 | “Control of bladder function during urges.” | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gutenbrunner, C.; Korallus, C.; Egen, C.; Schiller, J.; Sturm, C.; Teixido, L.; Eckhardt, I.; Boekel, A. Test of the Rehabilitation Goal Screening (ReGoS) Tool to Support Decision Making and Goal Setting in Physical and Rehabilitation Medicine Practice. Int. J. Environ. Res. Public Health 2022, 19, 15562. https://doi.org/10.3390/ijerph192315562
Gutenbrunner C, Korallus C, Egen C, Schiller J, Sturm C, Teixido L, Eckhardt I, Boekel A. Test of the Rehabilitation Goal Screening (ReGoS) Tool to Support Decision Making and Goal Setting in Physical and Rehabilitation Medicine Practice. International Journal of Environmental Research and Public Health. 2022; 19(23):15562. https://doi.org/10.3390/ijerph192315562
Chicago/Turabian StyleGutenbrunner, Christoph, Christoph Korallus, Christoph Egen, Joerg Schiller, Christian Sturm, Lidia Teixido, Isabelle Eckhardt, and Andrea Boekel. 2022. "Test of the Rehabilitation Goal Screening (ReGoS) Tool to Support Decision Making and Goal Setting in Physical and Rehabilitation Medicine Practice" International Journal of Environmental Research and Public Health 19, no. 23: 15562. https://doi.org/10.3390/ijerph192315562
APA StyleGutenbrunner, C., Korallus, C., Egen, C., Schiller, J., Sturm, C., Teixido, L., Eckhardt, I., & Boekel, A. (2022). Test of the Rehabilitation Goal Screening (ReGoS) Tool to Support Decision Making and Goal Setting in Physical and Rehabilitation Medicine Practice. International Journal of Environmental Research and Public Health, 19(23), 15562. https://doi.org/10.3390/ijerph192315562






