Association between Sleep and Suicidal Ideation in Chinese Undergraduate Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Measure
2.2.1. Suicidal Ideation and Emotional Health
2.2.2. Sleep
2.2.3. Demographic Characteristics
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Characteristics of Sleep and Emotional Symptoms with or without SI
3.3. Correlational Analysis
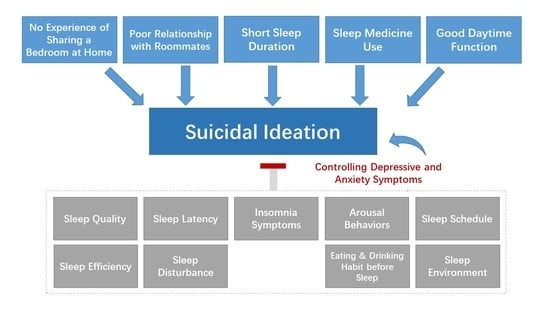
3.4. Hierarchical Linear Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Suicide Worldwide in 2019. Available online: https://www.who.int/publications/i/item/9789240026643 (accessed on 1 October 2022).
- Turecki, G.; Brent, D.A. Suicide and suicidal behaviour. Lancet 2016, 387, 1227–1239. [Google Scholar] [CrossRef]
- Batterham, P.J.; Werner-Seidler, A.; Calear, A.L.; McCallum, S.; Gulliver, A. Specific aspects of sleep disturbance associated with suicidal thoughts and attempts. J. Affect. Disord. 2021, 282, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Kearns, J.C.; Coppersmith, D.D.L.; Santee, A.C.; Insel, C.; Pigeon, W.R.; Glenn, C.R. Sleep problems and suicide risk in youth: A systematic review, developmental framework, and implications for hospital treatment. Gen. Hosp. Psychiatry 2022, 63, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Pigeon, W.R.; Pinquart, M.; Conner, K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J. Clin. Psychiatry 2012, 73, e1160–e1167. [Google Scholar] [CrossRef]
- Nadorff, M.R.; Nazem, S.; Fiske, A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep 2011, 34, 93–98. [Google Scholar] [CrossRef]
- Nadorff, M.R.; Sarra Nazem, A.F. Insomnia symptoms, nightmares and suicide risk: Duration of sleep disturbance matters. Suicide Life-Threat. Behav. 2013, 43, 139–149. [Google Scholar] [CrossRef]
- Dolsen, M.R.; Prather, A.A.; Lamers, F.; Penninx, B.W.J.H. Suicidal ideation and suicide attempts: Associations with sleep duration, insomnia, and inflammation. Psychol. Med. 2021, 51, 2094–2103. [Google Scholar] [CrossRef]
- Saulnier, K.G.; Singh, R.; Lenker, K.P.; Calhoun, S.L.; He, F.; Liao, D.; Vgontzas, A.N.; Bixler, E.O.; Fernandez-Mendoza, J. Association of insomnia phenotypes based on polysomnography-measured sleep duration with suicidal ideation and attempts. Sleep Health 2022, 8, 391–397. [Google Scholar] [CrossRef]
- Dinis, J.; Bragança, M. Quality of sleep and depression in college students: A systematic review. Sleep Sci. 2018, 11, 290–301. [Google Scholar] [CrossRef]
- Kaplan, S.G.; Ali, S.K.; Simpson, B.; Britt, V.; McCall, W.V. Associations between sleep disturbance and suicidal ideation in adolescents admitted to an inpatient psychiatric unit. Int. J. Adolesc. Med. Health 2014, 26, 411–416. [Google Scholar] [CrossRef]
- Derogatis, L.A.; Cleary, P. Method: The practical confirmation of the dimensional structure of the SCL-90: A study in construct validation. J. Clin. Psychol. 1977, 33, 981–989. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, X. Chinese college students’ SCL-90 scores and their relations to the college performance. Asian J. Psychiatr. 2013, 6, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Liu, X.C.; Tang, M.Q. Reliability and validity of the Pittsburgh Sleep Quality Index (Chinese version). Chin. J. Psychiatry 1996, 29, 103–107. [Google Scholar]
- Geng, F.; Fan, F.; Mo, L.; Simandl, I.; Liu, X. Sleep problems among adolescent survivors following the 2008 Wenchuan Earthquake in China: A Cohort Study. J. Clin. Psychiatry 2013, 74, 67–74. [Google Scholar] [CrossRef]
- Yang, C.M.; Lin, S.C.; Hsu, S.C.; Cheng, C.P. Maladaptive sleep hygiene practices in good sleepers and patients with insomnia. J. Health Psychol. 2010, 15, 147–155. [Google Scholar] [CrossRef]
- Morin, C.M.; Press, T.G. Insomnia: Psychological Assessment and Management; Guilford Press: New York, NY, USA, 1993. [Google Scholar]
- Bastien, Â.H.; Vallie, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Higuchi, S.; Motohashi, Y.; Liu, Y.; Maeda, A. Effects of playing a computer game using a bright display on presleep physiological variables, sleep latency, slow wave sleep and REM sleep. J. Sleep Res. 2005, 14, 267–273. [Google Scholar] [CrossRef]
- Lapierre, S.; Boyer, R.; Desjardins, S.; Dubé, M.; Lorrain, D.; Préville, M.; Brassard, J. Daily hassles, physical illness, and sleep problems in older adults with wishes to die. Int. Psychogeriatr. 2012, 24, 243–252. [Google Scholar] [CrossRef]
- Wu, R.; Zhu, H.; Wang, Z.J.; Jiang, C.L. A large sample survey of suicide risk among university students in China. BMC Psychiatry 2021, 21, 474. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.K.; Li, Q.F.; Han, D.C.; Cheng, W.; Song, N.; Hu, M.; Xiao, S.Y. The association between sleep and suicidality in the presence and absence of depressive symptoms: A cross-sectional study in rural China. Med. 2022, 101, e29725. [Google Scholar] [CrossRef] [PubMed]
- Lüdtke, T.; Pfuhl, G.; Moritz, S.; Rüegg, N.L.; Berger, T.; Westermann, S. Sleep problems and worrying precede psychotic symptoms during an online intervention for psychosis. Br. J. Clin. Psychol. 2021, 60, 48–67. [Google Scholar] [CrossRef] [PubMed]
- Mulyadi, M.; Tonapa, S.I.; Luneto, S.; Lin, W.-T.; Lee, B.-O. Prevalence of mental health problems and sleep disturbances in nursing students during the COVID-19 pandemic: A systematic review and meta-analysis. Nurse Educ. Pract. 2021, 57, 103228. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.T.; Perlis, M.L.; Haythornthwaite, J.A. Suicidal ideation in outpatients with chronic musculoskeletal pain: An exploratory study of the role of sleep onset insomnia and pain intensity. Clin. J. Pain 2004, 20, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Bernert, R.A.; Nadorff, M.R. Sleep disturbances and suicide risk. Sleep Med. Clin. 2015, 10, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Simmons, Z.; Burlingame, G.; Korbanka, J.; Eastman, K.; Thomas, D.; Christensen, J.; Jenson, M.; Nadorff, M.R.; Kay, D.B. Insomnia symptom severity is associated with increased suicidality and death by suicide in a sample of patients with psychiatric disorders. Sleep 2021, 44, zsab032. [Google Scholar] [CrossRef]
- Gunn, H.E.; Troxel, W.M.; Hall, M.H.; Buysse, D.J. Interpersonal distress is associated with sleep and arousal in insomnia and good sleepers. J. Psychosom. Res. 2014, 76, 242–248. [Google Scholar] [CrossRef]
- Chu, C.; Nota, J.A.; Silverman, A.L.; Beard, C.; Björgvinsson, T. Pathways among sleep onset latency, relationship functioning, and negative affect differentiate patients with suicide attempt history from patients with suicidal ideation. Psychiatry Res. 2019, 273, 788–797. [Google Scholar] [CrossRef]
- Trockel, M.; Karlin, B.E.; Taylor, C.B.; Brown, G.K.; Manber, R. Effects of cognitive behavioral therapy for insomnia on suicidal ideation in veterans. Sleep 2015, 38, 259–265. [Google Scholar] [CrossRef]
- McCauley, E.; Berk, M.S.; Asarnow, J.R.; Adrian, M.; Cohen, J.; Korslund, K.; Avina, C.; Hughes, J.; Harned, M.; Gallop, R.; et al. Efficacy of dialectical behavior therapy for adolescents at high risk for suicide: A randomized clinical trial. JAMA Psychiatry 2018, 75, 777–785. [Google Scholar] [CrossRef]
- Mohamadi, J.; Ghazanfari, F.; Drikvand, F.M. Comparison of the effect of dialectical behavior therapy, mindfulness based cognitive therapy and positive psychotherapy on perceived stress and quality of life in patients with Irritable Bowel Syndrome: A pilot randomized controlled trial. Psychiatr. Q. 2019, 90, 565–578. [Google Scholar] [CrossRef] [PubMed]
- Wu, R.; Zhong, S.Y.; Wang, G.H.; Wu, M.Y.; Xu, J.F.; Zhu, H.; Liu, L.L.; Su, W.J.; Cao, Z.Y.; Jiang, C.L. The effect of brief mindfulness meditation on suicidal ideation, stress and sleep quality. Arch. Suicide Res. 2021. [Google Scholar] [CrossRef] [PubMed]
- Tremaine, R.B.; Dorrian, J.; Blunden, S. Subjective and objective sleep in children and adolescents: Measurement, age, and gender differences. Sleep Biol. Rhythm. 2010, 8, 229–238. [Google Scholar] [CrossRef]
- Nelson, T.D.; Lundahl, A.; Molfese, D.L.; Waford, R.N.; Roman, A.; Gozal, D.; Molfese, V.J.; Ferguson, M.C. Estimating child sleep from parent report of time in bed: Development and evaluation of adjustment approaches. J. Pediatr. Psychol. 2014, 39, 624–632. [Google Scholar] [CrossRef] [PubMed]
| Variables | n | % | Variables | n | % | ||
|---|---|---|---|---|---|---|---|
| Sex | Male | 411 | 17.28% | Shares a bedroom with sibling at home | No sibling or does not share | 1841 | 77.39% |
| Female | 1968 | 82.72% | Shares a bedroom | 538 | 22.61% | ||
| Grade | Freshman | 748 | 31.44% | Sleeping schedules consistent with roommates | Consistent | 218 | 9.16% |
| Sophomore | 734 | 30.85% | Inconsistent but does not affect sleep | 1499 | 63.01% | ||
| Junior | 543 | 22.82% | Inconsistent and does affect sleep | 662 | 27.83% | ||
| Senior | 354 | 14.88% | Relationship with roommates | Good | 2141 | 90.00% | |
| School | National key university | 871 | 36.61% | General | 193 | 8.11% | |
| Municipal key university | 1157 | 48.63% | Poor | 45 | 1.89% | ||
| General university | 351 | 14.75% | Seek treatment for sleep problems | No | 2296 | 96.51% | |
| Electronic equipment use in bedtime | 0 min | 147 | 6.18% | Receive psychological counseling | 35 | 1.47% | |
| <10 min | 198 | 8.32% | Get medical attention | 33 | 1.39% | ||
| 11–30 min | 745 | 31.32% | Both | 15 | 0.63% | ||
| >30 min | 1289 | 54.18% | Total | 2379 | 100% |
| All Participants (N = 2379) | Participants with SI (n = 327) | Participants without SI (n = 2052) | |||||
|---|---|---|---|---|---|---|---|
| Variables | Median (IQR) | n (%) (above or below the Thresholds) | Median (IQR) | n (%) (above or below the Thresholds) | Median (IQR) | n (%) (above or below the Thresholds) | p of Mann-Whitney U Test |
| Bedtime (hh:mm) | 23:30 (21:30–01:30) | 1499 (63.1%) | 24:00 (21:30–01:30) | 231 (70.6%) | 23:30 (21:30–01:30) | 1268 (61.8%) | <0.01 |
| Sleep latency (hh:mm) | 00:15 (00–01:00) | 738 (31%) | 00:20 (0–01:00) | 143 (43.7%) | 00:15 (0–01:00) | 595 (29%) | <0.01 |
| Sleep duration (h) | 7 (5–9) | 1099 (46.1%) | 7 (4.5–8.5) | 162 (49.5%) | 7 (5–9) | 697 (34%) | <0.01 |
| Sleep efficiency (%) | 92.31 (1.5–5.5) | 554 (23.3%) | 88.89 (0.64–1.15) | 95 (29.1%) | 92.86 (0.69–1.14) | 459 (22.4%) | <0.01 |
| PSQI_Quality | 0 (0–0) | 0 (0–2.5) | 0 (0–0) | <0.01 | |||
| PSQI_Latency | 1 (0–2.5) | 1 (0–5) | 1 (0–2.5) | <0.01 | |||
| PSQI_Duration | 1 (0–2.5) | 1 (1–1) | 1 (0–2.5) | <0.01 | |||
| PSQI_Efficiency | 0 (0–0) | 0 (0–2.5) | 0 (0–0) | <0.01 | |||
| PSQI_Disturbance | 1 (0–2.5) | 1 (0–2.5) | 1 (0–2.5) | <0.01 | |||
| PSQI_Medicine | 0 (0–0) | 0 (0–0) | 0 (0–0) | <0.01 | |||
| PSQI_Daytime function | 1 (0–5) | 1 (0–3.5) | 1 (0–5) | <0.01 | |||
| PSQI_Total | 3 (0–9.5) | 230 (9.7%) | 5 (0–10.5) | 78 (23.9%) | 3 (0–9.5) | 152 (7.4%) | <0.01 |
| SHPS_Arousal behaviors | 24 (6.5–42.5) | 27 (11–43) | 24 (8–40) | <0.01 | |||
| SHPS_Schedule | 21 (6–38) | 26 (10–42) | 21 (5–37) | <0.01 | |||
| SHPS_Eating & drinking | 11 (1.5–21.5) | 13 (1–25) | 11 (1.5–21.5) | <0.01 | |||
| SHPS_Environment | 17 (0–37) | 21 (0–43.5) | 16 (0–37) | <0.01 | |||
| SHPS_Total | 75 (29.5–121.5) | 87 (40–136) | 74 (30–118) | <0.01 | |||
| ISI_Total | 5 (0–17) | 702 (29.5%) | 8 (0–22.5) | 177 (54.1%) | 4 (0–17) | 525 (25.6%) | <0.01 |
| SCL-90_Depression | 1.38 (0–3.19) | 547 (23.0%) | 2.46 (0.31–4.62) | 241 (73.7%) | 1.27 (0.15–2.62) | 306 (14.9%) | <0.01 |
| SCL-90_Anxiety | 1.20 (0–2.75) | 508 (17.1%) | 2.10 (0.1–4.1) | 288 (88.3%) | 1.20 (0.25–2.25) | 220 (10.7%) | <0.01 |
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | PSQI_Quality | ||||||||||||||||
| 2 | PSQI_Latency | 0.36 ** | |||||||||||||||
| 3 | PSQI_Duration | 0.17 ** | 0.08 ** | ||||||||||||||
| 4 | PSQI_Efficiency | 0.15 ** | 0.30 ** | 0.25 ** | |||||||||||||
| 5 | PSQI_Disturbance | 0.22 ** | 0.27 ** | 0.03 | 0.09 ** | ||||||||||||
| 6 | PSQI_Medicine | 0.14 ** | 0.15 ** | −0.003 | 0.04 | 0.09 ** | |||||||||||
| 7 | PSQI_Daytime function | 0.30 ** | 0.20 ** | 0.20 ** | 0.09 ** | 0.24 ** | 0.06 ** | ||||||||||
| 8 | PSQI_Total | 0.55 ** | 0.64 ** | 0.49 ** | 0.48 ** | 0.52 ** | 0.19 ** | 0.66 ** | |||||||||
| 9 | SHPS_Arousal behaviors | 0.18 ** | 0.20 ** | 0.10 ** | 0.11 ** | 0.14 ** | 0.06 ** | 0.37 ** | 0.34 ** | ||||||||
| 10 | SHPS_Schedule | 0.33 ** | 0.43 ** | 0.16 ** | 0.15 ** | 0.33 ** | 0.13 ** | 0.36 ** | 0.52 ** | 0.41 ** | |||||||
| 11 | SHPS_Eating & drinking | 0.10 ** | 0.11 ** | 0.11 ** | 0.05 ** | 0.11 ** | 0.07 ** | 0.26 ** | 0.24 ** | 0.40 ** | 0.42 ** | ||||||
| 12 | SHPS_Environment | 0.25 ** | 0.26 ** | 0.06 ** | 0.07 ** | 0.24 ** | 0.07 ** | 0.32 ** | 0.36 ** | 0.34 ** | 0.50 ** | 0.39 ** | |||||
| 13 | SHPS_Total | 0.31 ** | 0.35 ** | 0.15 ** | 0.14 ** | 0.28 ** | 0.11 ** | 0.44 ** | 0.51 ** | 0.71 ** | 0.79 ** | 0.64 ** | 0.78 ** | ||||
| 14 | ISI_Total | 0.52 ** | 0.45 ** | 0.23 ** | 0.19 ** | 0.34 ** | 0.15 ** | 0.46 ** | 0.63 ** | 0.34 ** | 0.59 ** | 0.28 ** | 0.47 ** | 0.57 ** | |||
| 15 | SCL-90_Depression | 0.33 ** | 0.23 ** | 0.19 ** | 0.08 ** | 0.27 ** | 0.12 ** | 0.46 ** | 0.47 ** | 0.36 ** | 0.47 ** | 0.30 ** | 0.42 ** | 0.53 ** | 0.52 ** | ||
| 16 | SCL-90_Anxiety | 0.27 ** | 0.21 ** | 0.15 ** | 0.06 ** | 0.27 ** | 0.10 ** | 0.38 ** | 0.40 ** | 0.29 ** | 0.47 ** | 0.26 ** | 0.41 ** | 0.49 ** | 0.49 ** | 0.81 ** | |
| 17 | SCL-90_SI | 0.21 ** | 0.13 ** | 0.14 ** | 0.07 ** | 0.12 ** | 0.12 ** | 0.18 ** | 0.23 ** | 0.17 ** | 0.24 ** | 0.16 ** | 0.21 ** | 0.27 ** | 0.25 ** | 0.47 ** | 0.41 ** |
| Variables | B | SE | β | t | p | R2 | Adjusted R2 | R2 Change | F | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Step 1 | 0.04 | 0.04 | 0.04 | 21.34 | <0.01 | |||||
| Age | −0.02 | 0.01 | −0.04 | −1.76 | 0.08 | |||||
| Sex | 0.07 | 0.03 | 0.04 | 2.03 | 0.04 | |||||
| Shares a bedroom at home | −0.04 | 0.03 | −0.03 | −1.40 | 0.16 | |||||
| Sleeping schedules consistent with roommates | 0.07 | 0.02 | 0.06 | 2.92 | <0.01 | |||||
| Relationship with roommates | 0.30 | 0.03 | 0.18 | 8.71 | <0.01 | |||||
| Step 2 | 0.14 | 0.14 | 0.10 | 23.32 | <0.01 | |||||
| Age | −0.02 | 0.01 | −0.04 | −2.02 | 0.04 | |||||
| Sex | 0.03 | 0.03 | 0.02 | 1.07 | 0.29 | |||||
| Shares a bedroom at home | −0.05 | 0.03 | −0.03 | −1.74 | 0.08 | |||||
| Sleeping schedules consistent with roommates | −0.02 | 0.02 | −0.02 | −1.07 | 0.28 | |||||
| Relationship with roommates | 0.19 | 0.03 | 0.12 | 5.82 | <0.01 | |||||
| PSQI_Quality | 0.07 | 0.03 | 0.05 | 2.21 | 0.03 | |||||
| PSQI_Latency | −0.02 | 0.02 | −0.03 | −1.15 | 0.25 | |||||
| PSQI_Duration | 0.07 | 0.02 | 0.07 | 3.22 | <0.01 | |||||
| PSQI_Efficiency | 0.01 | 0.02 | 0.01 | 0.34 | 0.74 | |||||
| PSQI_Disturbance | −0.01 | 0.03 | −0.01 | −0.26 | 0.79 | |||||
| PSQI_Medicine | 0.33 | 0.05 | 0.12 | 6.18 | <0.01 | |||||
| PSQI_Daytime | 0.02 | 0.02 | 0.02 | 0.91 | 0.37 | |||||
| SHPS_Arousal behaviors | 0.00 | 0.00 | 0.01 | 0.65 | 0.52 | |||||
| SHPS_Schedule | 0.01 | 0.00 | 0.09 | 3.08 | <0.01 | |||||
| SHPS_Eating & drinking | 0.01 | 0.00 | 0.05 | 2.12 | 0.03 | |||||
| SHPS_Environment | 0.00 | 0.00 | 0.05 | 1.96 | 0.05 | |||||
| ISI_Total | 0.02 | 0.00 | 0.12 | 3.87 | <0.01 | |||||
| Step 3 | 0.38 | 0.38 | 0.24 | 76.26 | <0.01 | |||||
| Age | −0.01 | 0.01 | −0.01 | −0.68 | 0.50 | |||||
| Sex | 0.01 | 0.03 | 0.01 | 0.51 | 0.61 | |||||
| Shares a bedroom at home | −0.05 | 0.02 | −0.03 | −2.07 | 0.04 | |||||
| Sleeping schedules consistent with roommates | 0.00 | 0.02 | 0.00 | 0.05 | 0.96 | |||||
| Relationship with roommates | 0.08 | 0.03 | 0.05 | 2.79 | 0.01 | |||||
| PSQI_Quality | 0.02 | 0.03 | 0.01 | 0.58 | 0.56 | |||||
| PSQI_Latency | 0.01 | 0.02 | 0.01 | 0.60 | 0.55 | |||||
| PSQI_Duration | 0.04 | 0.02 | 0.04 | 1.99 | 0.05 | |||||
| PSQI_Efficiency | 0.02 | 0.02 | 0.02 | 0.87 | 0.38 | |||||
| PSQI_Disturbance | −0.03 | 0.02 | -0.02 | -1.38 | 0.17 | |||||
| PSQI_ Medicine use | 0.19 | 0.05 | 0.07 | 4.23 | <0.01 | |||||
| PSQI_ Daytime | −0.07 | 0.02 | −0.09 | −4.51 | <0.01 | |||||
| SHPS_Arousal behaviors | 0.00 | 0.00 | −0.03 | −1.55 | 0.12 | |||||
| SHPS_Schedule | 0.00 | 0.00 | −0.01 | −0.39 | 0.69 | |||||
| SHPS_Eating and drinking | 0.00 | 0.00 | 0.02 | 1.28 | 0.20 | |||||
| SHPS_Environment | 0.00 | 0.00 | 0.00 | −0.09 | 0.93 | |||||
| ISI_Total | 0.00 | 0.00 | −0.01 | −0.49 | 0.63 | |||||
| SCL-90_Depression | 0.61 | 0.03 | 0.65 | 20.37 | <0.01 | |||||
| SCL-90_Anxiety | −0.04 | 0.03 | −0.04 | −1.24 | 0.22 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, R.; Wang, C.-Y.; Wang, F.; Wang, Y.-J.; Zhu, H.; Wang, G.-H.; Jiang, C.-L. Association between Sleep and Suicidal Ideation in Chinese Undergraduate Students. Int. J. Environ. Res. Public Health 2022, 19, 15433. https://doi.org/10.3390/ijerph192315433
Wu R, Wang C-Y, Wang F, Wang Y-J, Zhu H, Wang G-H, Jiang C-L. Association between Sleep and Suicidal Ideation in Chinese Undergraduate Students. International Journal of Environmental Research and Public Health. 2022; 19(23):15433. https://doi.org/10.3390/ijerph192315433
Chicago/Turabian StyleWu, Ran, Chun-Ying Wang, Feng Wang, Yu-Jing Wang, Hong Zhu, Guang-Hai Wang, and Chun-Lei Jiang. 2022. "Association between Sleep and Suicidal Ideation in Chinese Undergraduate Students" International Journal of Environmental Research and Public Health 19, no. 23: 15433. https://doi.org/10.3390/ijerph192315433
APA StyleWu, R., Wang, C.-Y., Wang, F., Wang, Y.-J., Zhu, H., Wang, G.-H., & Jiang, C.-L. (2022). Association between Sleep and Suicidal Ideation in Chinese Undergraduate Students. International Journal of Environmental Research and Public Health, 19(23), 15433. https://doi.org/10.3390/ijerph192315433