Effect of the Use of Home and Community Care Services on the Multidimensional Health of Older Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Variables and Their Measurement
2.3. Statistical Methods
3. Results
3.1. Sample Characteristics
3.2. Estimates of Propensity Scores Using a Logit Model
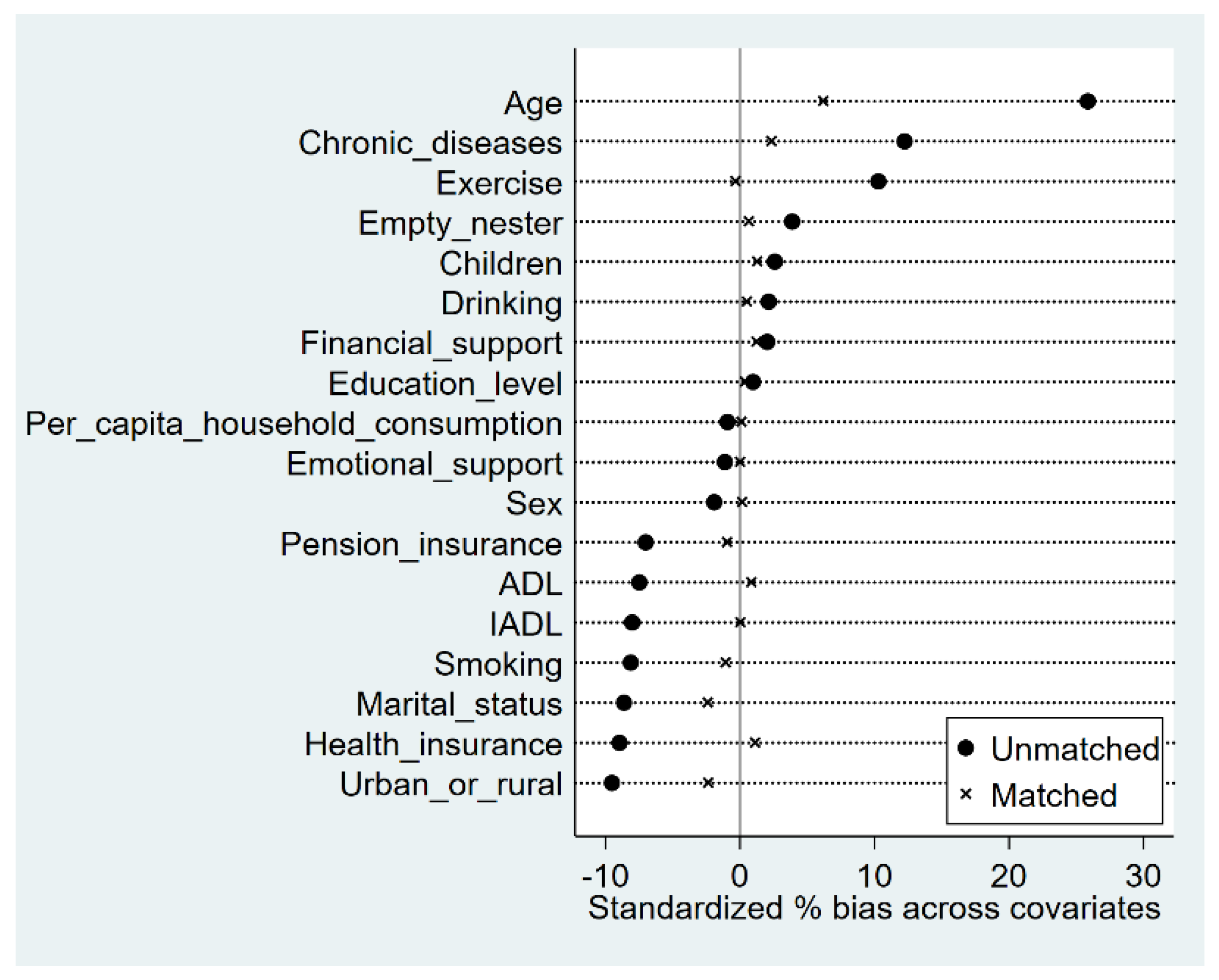
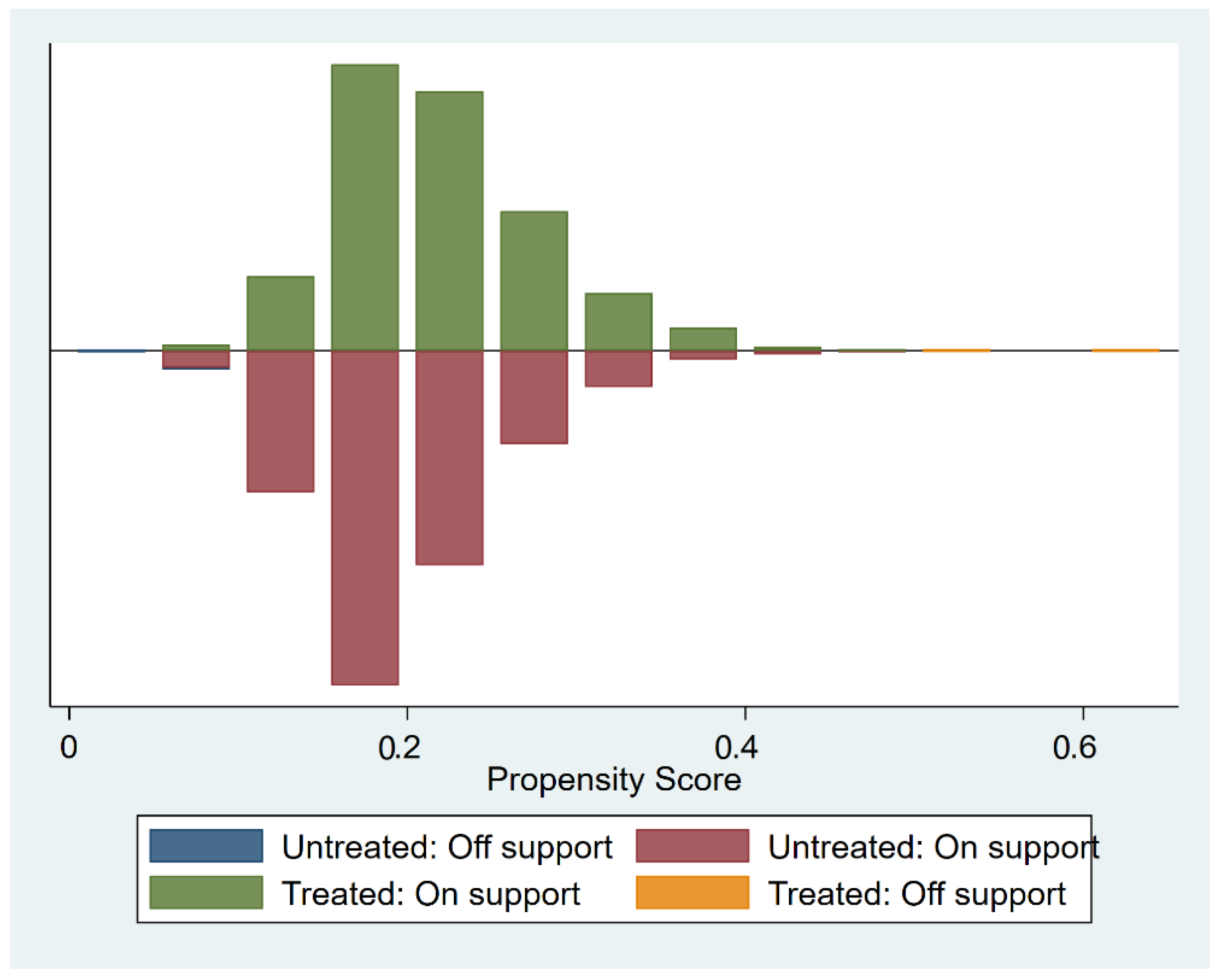
3.3. The Quality of Matching
3.4. The Effect of Using Home and Community Care on the Health of Older People
3.5. Heterogeneity Analysis
3.6. Robustness Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harrefors, C.; Sävenstedt, S.; Axelsson, K. Elderly People’s Perceptions of How They Want to Be Cared for: An Interview Study with Healthy Elderly Couples in Northern Sweden. Scand. J. Caring Sci. 2009, 23, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Ryan, A.A.; McCann, S.; McKenna, H. Impact of Community Care in Enabling Older People with Complex Needs to Remain at Home. Int. J. Older People Nurs. 2009, 4, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Joshua, L. Aging and Long Term Care Systems: A Review of Finance and Governance Arrangements in Europe, North America and Asia-Pacific; Social Protection & Labor Discussion Paper; World Bank Group: Washington, DC, USA, 2017. [Google Scholar]
- Lu, B.; Mi, H.; Zhu, Y.; Piggott, J. A Sustainable Long-Term Health Care System for Aging China: A Case Study of Regional Practice. Health Syst. Reform 2017, 3, 182–190. [Google Scholar] [CrossRef] [PubMed]
- The Leading Group of the State Council for the Seventh National Population Census Main Data of the Seventh National Population Census. Available online: http://www.stats.gov.cn/english/PressRelease/202105/t20210510_1817185.html (accessed on 9 October 2022).
- Feng, Z.; Glinskaya, E.; Chen, H.; Gong, S.; Qiu, Y.; Xu, J.; Yip, W. Long-Term Care System for Older Adults in China: Policy Landscape, Challenges, and Future Prospects. Lancet 2020, 396, 1362–1372. [Google Scholar] [CrossRef]
- World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 11 October 2022).
- Grossman, M. The Demand for Health: A Theoretical and Empirical Investigation; Columbia University Press: New York, NY, USA, 1972; ISBN 978-0-231-17900-3. [Google Scholar]
- Hellström, Y.; Andersson, M.; Hallberg, I.R. Quality of Life among Older People in Sweden Receiving Help from Informal and/or Formal Helpers at Home or in Special Accommodation. Health Soc. Care Community 2004, 12, 504–516. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Karlsson, S.; Edberg, A.-K.; Jakobsson, U.; Hallberg, I.R. Care Satisfaction among Older People Receiving Public Care and Service at Home or in Special Accommodation. J. Clin. Nurs. 2013, 22, 318–330. [Google Scholar] [CrossRef] [PubMed]
- Imanishi, M.; Tomohisa, H.; Higaki, K. Quality of Life in Elderly People at the Start of Using In-Home Care. Springerplus 2015, 4, 381. [Google Scholar] [CrossRef][Green Version]
- Prot-Klinger, K.; Pawłowska, M. The Effectiveness of Community Care for People with Severe Mental Disorders. Arch. Psychiatry Psychother. 2009, 11, 43–50. [Google Scholar]
- Kadowaki, L.; Wister, A.V.; Chappell, N.L. Influence of Home Care on Life Satisfaction, Loneliness, and Perceived Life Stress. Can. J. Aging 2015, 34, 75–89. [Google Scholar] [CrossRef]
- Yue, Z.; Xiang, N.; Li, H.; Liu, E. The Evolution Trend of Availability of China’s Community-Based Care Services and Its Impact on the Cognitive Function of Elderly People: 2008-2018. Int. J. Equity Health 2021, 20, 203. [Google Scholar] [CrossRef]
- World Health Organization. Constitution of the World Health Organization; World Health Organization: Basic Documents; World Health Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Wang, Q.; Tian, W. Prevalence, Awareness, and Treatment of Depressive Symptoms among the Middle-Aged and Elderly in China from 2008 to 2015. Int. J. Health Plan. Manag. 2018, 33, 1060–1070. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Li, J.; Chen, M. The Association Between Cognitive Impairment and Subsequent Falls Among Older Adults: Evidence From the China Health and Retirement Longitudinal Study. Front. Public Health 2022, 10. [Google Scholar] [CrossRef] [PubMed]
- Larson, J.S. The Measurement of Social Well-Being. Soc. Indic. Res. 1993, 28, 285–296. [Google Scholar] [CrossRef]
- Liu, H.; Byles, J.E.; Xu, X.; Zhang, M.; Wu, X.; Hall, J.J. Evaluation of Successful Aging among Older People in China: Results from China Health and Retirement Longitudinal Study. Geriatr. Gerontol. Int. 2017, 17, 1183–1190. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Li, Y.-X.; Hu, Y.; Wu, C. Association of Frailty with Recovery from Disability among Community-Dwelling Chinese Older Adults: China Health and Retirement Longitudinal Study. BMC Geriatr. 2020, 20. [Google Scholar] [CrossRef]
- ROSENBAUM, P.R.; RUBIN, D.B. The Central Role of the Propensity Score in Observational Studies for Causal Effects. Biometrika 1983, 70, 41–55. [Google Scholar] [CrossRef]
- Creavin, S.T.; Wisniewski, S.; Noel-Storr, A.H.; Trevelyan, C.M.; Hampton, T.; Rayment, D.; Thom, V.M.; Nash, K.J.E.; Elhamoui, H.; Milligan, R.; et al. Mini-Mental State Examination (MMSE) for the Detection of Dementia in Clinically Unevaluated People Aged 65 and over in Community and Primary Care Populations. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Yi, Y.M.; Park, Y.-H.; Cho, B.; Lim, K.-C.; Jang, S.-N.; Chang, S.J.; Ko, H.; Noh, E.-Y.; Ryu, S.I. Development of a Community-Based Integrated Service Model of Health and Social Care for Older Adults Living Alone. Int. J. Environ. Res. Public Health 2021, 18, 825. [Google Scholar] [CrossRef]
- Zhou, W.; Jiang, B.; Yu, L.; Dai, W. Measuring Demand and Supply of Community Care Services for Older People Healthy Ageing in Rural Zhejiang Province. BMC Geriatr. 2022, 22, 286. [Google Scholar] [CrossRef]
- Gu, L.; Cheng, Y.; Phillips, D.R.; Rosenberg, M. Understanding the Wellbeing of the Oldest-Old in China: A Study of Socio-Economic and Geographical Variations Based on CLHLS Data. Int. J. Environ. Res. Public Health 2019, 16, 601. [Google Scholar] [CrossRef]
- Ailing, G.; Zhanlian, F. Building an Efficient and Sustainable Aged Care System in China; China Financial and Economic Publishing House: Beijing, China, 2018. [Google Scholar]
- Zhu, H. Unmet Needs in Long-Term Care and Their Associated Factors among the Oldest Old in China. BMC Geriatr. 2015, 15, 46. [Google Scholar] [CrossRef] [PubMed]
- Loveys, K.; Prina, M.; Axford, C.; Domènec, Ò.R.; Weng, W.; Broadbent, E.; Pujari, S.; Jang, H.; Han, Z.A.; Thiyagarajan, J.A. Artificial Intelligence for Older People Receiving Long-Term Care: A Systematic Review of Acceptability and Effectiveness Studies. Lancet Healthy Longev. 2022, 3, e286–e297. [Google Scholar] [CrossRef]
| Variable | Measurement | Mean or % | |
|---|---|---|---|
| Outcome variables | Change in physical health | 1 = Maintenance or improvement, 0 = Deterioration | 0.474 |
| Depression | 0~30 | 8.596 | |
| Cognitive function | 0~30 | 21.176 | |
| Active participation in life | 1 = Yes, 0 = No | 0.125 | |
| Life satisfaction | 1~5 | 3.280 | |
| Explanatory variable | The use of home and community care | 1 = Yes, 0 = No | 0.202 |
| Covariates | Age | Continuous variable | 68.807 |
| Sex | 1 = Male, 0 = Female | 0.492 | |
| Urban/rural areas | 1 = Rural, 0 = Urban | 0.758 | |
| Marital status | 1 = Married, 0 = Not married | 0.791 | |
| Education level | 1 = Illiterate | 29.78% | |
| 2 = Primary school | 45.01% | ||
| 3 = Junior school | 15.70% | ||
| 4 = High school | 8.09% | ||
| 5 = Bachelor or above | 1.42% | ||
| Being an empty nester | 1 = Yes, 0 = No | 0.480 | |
| Pension insurance | 1 = Pension for public servants and public institution employees | 20.28% | |
| 2 = Basic pension for enterprise employees | 66.44% | ||
| 3 = Pension for land-expropriated farmers, commercial pension insurance | 2.55% | ||
| 4 = No pension insurance | 10.73% | ||
| Health insurance | 1 = Urban employee medical insurance or urban and rural resident health insurance | 94.53% | |
| 2 = Other health insurance | 2.47% | ||
| 3 = No health insurance | 3.00% | ||
| The number of chronic diseases | 0 = 0 | 52.50% | |
| 1 = 1 | 28.67% | ||
| 2 = 2 and above | 18.83% | ||
| ADL | 0~18 | 0.697 | |
| IADL | 0~18 | 1.592 | |
| Smoking | 1 = Yes, 0 = No | 0.289 | |
| Drinking | 1 = Yes, 0 = No | 0.349 | |
| Exercise | 1 = Yes, 0 = No | 0.885 | |
| SES | 1 = lowest 25%, 2 = lower25%, 3 = higher 25%, 4 = highest 25% | 25% | |
| The number of children | Continuous variable | 2.997 | |
| Financial support from children | Continuous variable | 5 244.528 | |
| Emotional support from children | 1 = Living with their children or contacting them almost every day | 59.62% | |
| 2 = Contact children two or three times a week | 29.02% | ||
| 3 = Contact children every half month or one month | 9.56% | ||
| 4 = Other | 1.80% |
| Variables | Coef. | S.E. | p-Value | [95% CI] | |
|---|---|---|---|---|---|
| Age | 0.049 *** | 0.005 | <0.001 | 0.040 | 0.058 |
| Sex | −0.067 | 0.073 | 0.358 | −0.211 | 0.076 |
| Urban/rural areas | −0.076 | 0.071 | 0.287 | −0.215 | 0.064 |
| Marital status | −0.063 | 0.066 | 0.338 | −0.193 | 0.066 |
| Education level | −0.007 | 0.032 | 0.829 | −0.071 | 0.057 |
| Being an empty nester | 0.104 | 0.058 | 0.071 | −0.009 | 0.218 |
| The number of chronic diseases | 0.172 *** | 0.033 | <0.001 | 0.107 | 0.236 |
| ADL | −0.030 | 0.021 | 0.144 | −0.070 | 0.010 |
| IADL | −0.032 ** | 0.011 | 0.005 | −0.054 | −0.009 |
| Smoking | −0.120 | 0.068 | 0.077 | −0.252 | 0.013 |
| Drinking | 0.064 | 0.064 | 0.319 | −0.062 | 0.189 |
| Exercise | 0.343 *** | 0.091 | <0.001 | 0.164 | 0.523 |
| SES | −0.029 | 0.025 | 0.240 | −0.078 | 0.020 |
| The number of children | −0.055 ** | 0.020 | 0.007 | −0.095 | −0.015 |
| Financial support from children | 1.24 × 10−6 | 2.19 × 10−6 | 0.571 | −3.05 × 10−6 | 5.53 × 10−6 |
| Emotional support from children | −0.045 | 0.039 | 0.256 | −0.121 | 0.032 |
| Pension insurance | −0.047 | 0.036 | 0.191 | −0.117 | 0.023 |
| Health insurance | −0.333 *** | 0.082 | <0.001 | −0.494 | −0.172 |
| Constant | −4.267 *** | 0.382 | <0.001 | −5.017 | −3.518 |
| Variables | Mean | Standardized Differences (%) | t-Test | |||
|---|---|---|---|---|---|---|
| Treatment Group | Control Group | t Value | p > T | |||
| Age | Before matching | 70.149 | 68.467 | 10.11 | 0.00 | |
| After matching | 70.110 | 69.708 | 76.1 | 1.90 | 0.06 | |
| Sex | Before matching | 0.484 | 0.494 | −0.76 | 0.45 | |
| After matching | 0.485 | 0.484 | 92.4 | 0.05 | 0.96 | |
| Urban/rural areas | Before matching | 0.725 | 0.766 | −3.82 | 0.00 | |
| After matching | 0.724 | 0.735 | 75.0 | −0.73 | 0.47 | |
| Marital status | Before matching | 0.762 | 0.798 | −3.47 | 0.00 | |
| After matching | 0.764 | 0.774 | 72.0 | −0.74 | 0.46 | |
| Education level | Before matching | 2.071 | 2.062 | 0.38 | 0.71 | |
| After matching | 2.071 | 2.068 | 61.8 | 0.12 | 0.91 | |
| Being an empty nester | Before matching | 0.495 | 0.476 | 1.53 | 0.13 | |
| After matching | 0.495 | 0.492 | 83.3 | 0.20 | 0.84 | |
| The number of chronic diseases | Before matching | 0.739 | 0.644 | 4.87 | 0.00 | |
| After matching | 0.739 | 0.721 | 81.0 | 0.72 | 0.47 | |
| ADL | Before matching | 0.597 | 0.723 | −2.83 | 0.01 | |
| After matching | 0.598 | 0.584 | 88.9 | 0.29 | 0.77 | |
| IADL | Before matching | 1.397 | 1.641 | −3.07 | 0.00 | |
| After matching | 1.399 | 1.398 | 99.8 | 0.01 | 1.00 | |
| Smoking | Before matching | 0.260 | 0.296 | −3.17 | 0.00 | |
| After matching | 0.260 | 0.265 | 86.7 | −0.34 | 0.73 | |
| Drinking | Before matching | 0.357 | 0.347 | 0.84 | 0.40 | |
| After matching | 0.357 | 0.354 | 76.5 | 0.16 | 0.88 | |
| Exercise | Before matching | 0.910 | 0.878 | 3.91 | 0.00 | |
| After matching | 0.910 | 0.911 | 96.6 | −0.12 | 0.91 | |
| SES | Before matching | 2.489 | 2.499 | −0.37 | 0.71 | |
| After matching | 2.491 | 2.490 | 89.5 | 0.03 | 0.98 | |
| The number of children | Before matching | 3.028 | 2.990 | 1.03 | 0.30 | |
| After matching | 3.031 | 3.012 | 51.1 | 0.40 | 0.69 | |
| Financial support from children | Before matching | 5426.800 | 5198.400 | 0.79 | 0.43 | |
| After matching | 5433.600 | 5296.300 | 39.9 | 0.39 | 0.70 | |
| Emotional support from children | Before matching | 1.529 | 1.537 | −0.44 | 0.66 | |
| After matching | 1.528 | 1.528 | 99.9 | 0.00 | 1.00 | |
| Pension insurance | Before matching | 1.992 | 2.049 | −2.78 | 0.01 | |
| After matching | 1.992 | 2.000 | 86.2 | −0.30 | 0.76 | |
| Health insurance | Before matching | 1.060 | 1.091 | −3.33 | 0.00 | |
| After matching | 1.060 | 1.056 | 87.6 | 0.40 | 0.69 | |
| Health Indicators | Matching Methods | ATT | S.E. | t-Value | p-Value |
|---|---|---|---|---|---|
| Change in physical health | K-nearest neighbor matching | 0.029 ** | 0.013 | 2.26 | 0.016 |
| Nuclear matching | 0.035 ** | 0.014 | 2.50 | 0.044 | |
| Radius matching | 0.030 ** | 0.013 | 2.36 | 0.012 | |
| Depression | K-nearest neighbor matching | −0.479 *** | 0.165 | −2.90 | 0.001 |
| Nuclear matching | −0.539 ** | 0.184 | −2.93 | 0.017 | |
| Radius matching | −0.457 *** | 0.166 | −2.75 | 0.002 | |
| Cognitive function | K-nearest neighbor matching | 0.694 *** | 0.126 | 5.49 | <0.001 |
| Nuclear matching | 0.723 *** | 0.140 | 5.16 | <0.001 | |
| Radius matching | 0.717 *** | 0.127 | 5.64 | <0.001 | |
| Active participation in life | K-nearest neighbor matching | 0.040 *** | 0.009 | 4.46 | <0.001 |
| Nuclear matching | 0.041 *** | 0.010 | 4.11 | 0.001 | |
| Radius matching | 0.041 *** | 0.009 | 4.50 | <0.001 | |
| Life satisfaction | K-nearest neighbor matching | 0.088 *** | 0.020 | 4.51 | <0.001 |
| Nuclear matching | 0.078 *** | 0.022 | 3.60 | 0.001 | |
| Radius matching | 0.089 *** | 0.020 | 4.51 | <0.001 |
| Change in Physical Health | Depression | Cognitive Function | Active Participation in Life | Life Satisfaction | |
|---|---|---|---|---|---|
| Urban older adults (n = 2349) | 0.012 | −0.344 | 0.487 *** | 0.076 *** | 0.111 *** |
| Rural older adults (n = 7343) | 0.033 ** | −0.474 ** | 0.662 *** | 0.025 ** | 0.079 *** |
| People aged 60 to 79 years (n = 8896) | 0.029 ** | −0.632 *** | 0.728 *** | 0.042 *** | 0.092 *** |
| People aged ≥ 80 years (n = 796) | 0.030 | −0.784 | 0.514 | 0.034 | 0.033 |
| Non-disabled older adults (n = 7350) | 0.032 ** | −0.494 *** | 0.704 *** | 0.047 *** | 0.055 ** |
| Disabled older adults (n = 2342) | 0.030 | −0.566 | 0.700 *** | 0.023 | 0.209 *** |
| SES-high (n = 4846) | 0.020 | −0.345 | 0.696 *** | 0.060 *** | 0.071 ** |
| SES-low (n = 4846) | 0.029 *** | −0.479 *** | 0.694 *** | 0.040 *** | 0.088 *** |
| ATT | S.E. | t-Value | p-Value | |
|---|---|---|---|---|
| Self-reported health | 0.039 ** | 0.026 | 1.50 | 0.044 |
| Depression | 0.022 ** | 0.012 | 1.86 | 0.048 |
| Cognitive function | 0.042 *** | 0.011 | 3.57 | <0.001 |
| Social activities | 0.142 *** | 0.022 | 6.59 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Q.; Fan, K.; Li, P. Effect of the Use of Home and Community Care Services on the Multidimensional Health of Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 15402. https://doi.org/10.3390/ijerph192215402
Wang Q, Fan K, Li P. Effect of the Use of Home and Community Care Services on the Multidimensional Health of Older Adults. International Journal of Environmental Research and Public Health. 2022; 19(22):15402. https://doi.org/10.3390/ijerph192215402
Chicago/Turabian StyleWang, Qun, Kunyi Fan, and Peng Li. 2022. "Effect of the Use of Home and Community Care Services on the Multidimensional Health of Older Adults" International Journal of Environmental Research and Public Health 19, no. 22: 15402. https://doi.org/10.3390/ijerph192215402
APA StyleWang, Q., Fan, K., & Li, P. (2022). Effect of the Use of Home and Community Care Services on the Multidimensional Health of Older Adults. International Journal of Environmental Research and Public Health, 19(22), 15402. https://doi.org/10.3390/ijerph192215402





