Oral Contraceptive Use and Assessment of Breast Cancer Risk among Premenopausal Women via Molecular Characteristics: Systematic Review with Meta-Analysis
Abstract
1. Introduction
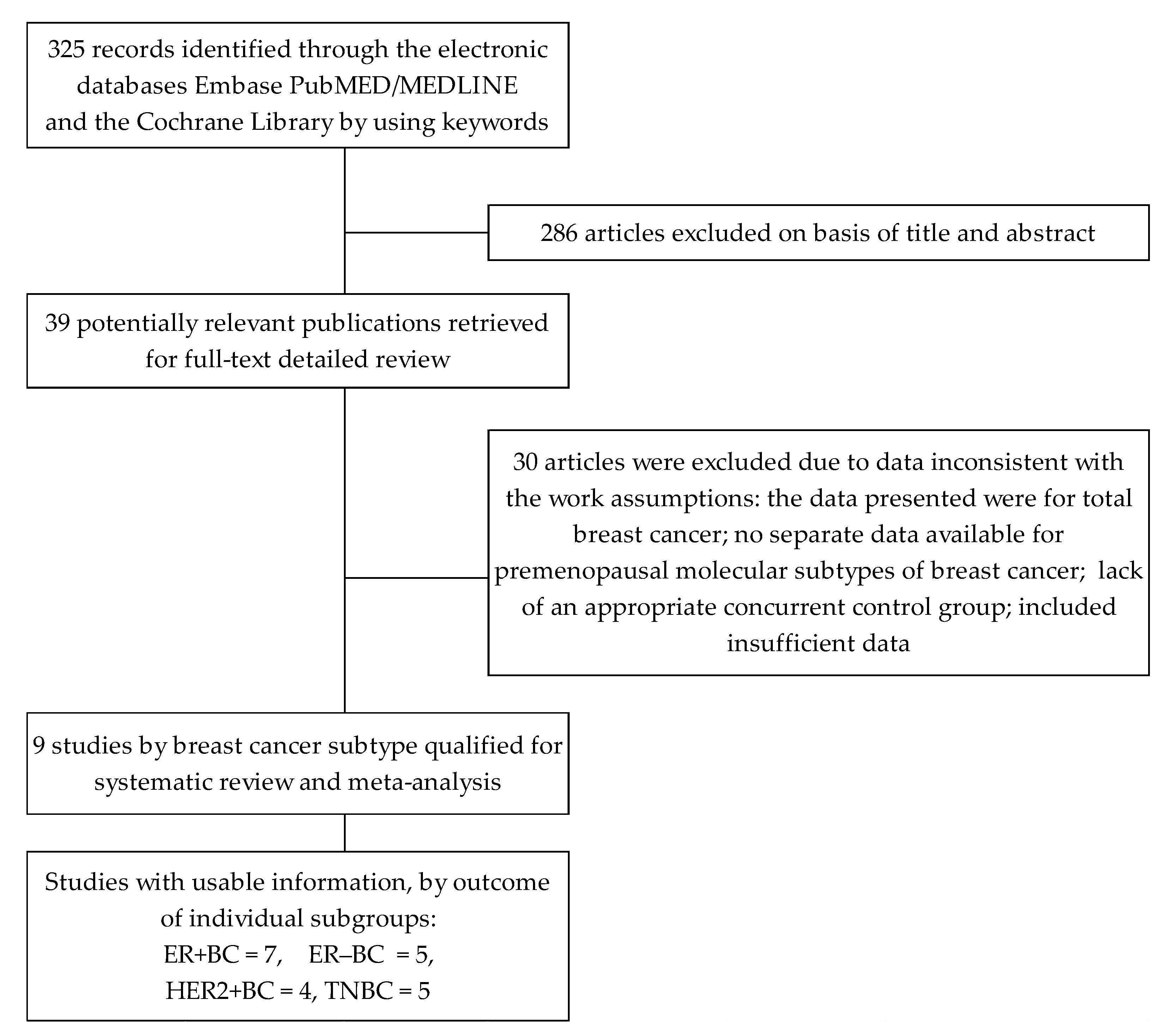
2. Methods
2.1. Search Strategy and Selection Criteria
2.2. Data Extraction
2.3. Assessment of Study Quality
2.4. Statistical Analysis
3. Results
3.1. Effects of Oral Contraceptive Use on ER-Positive Subtype
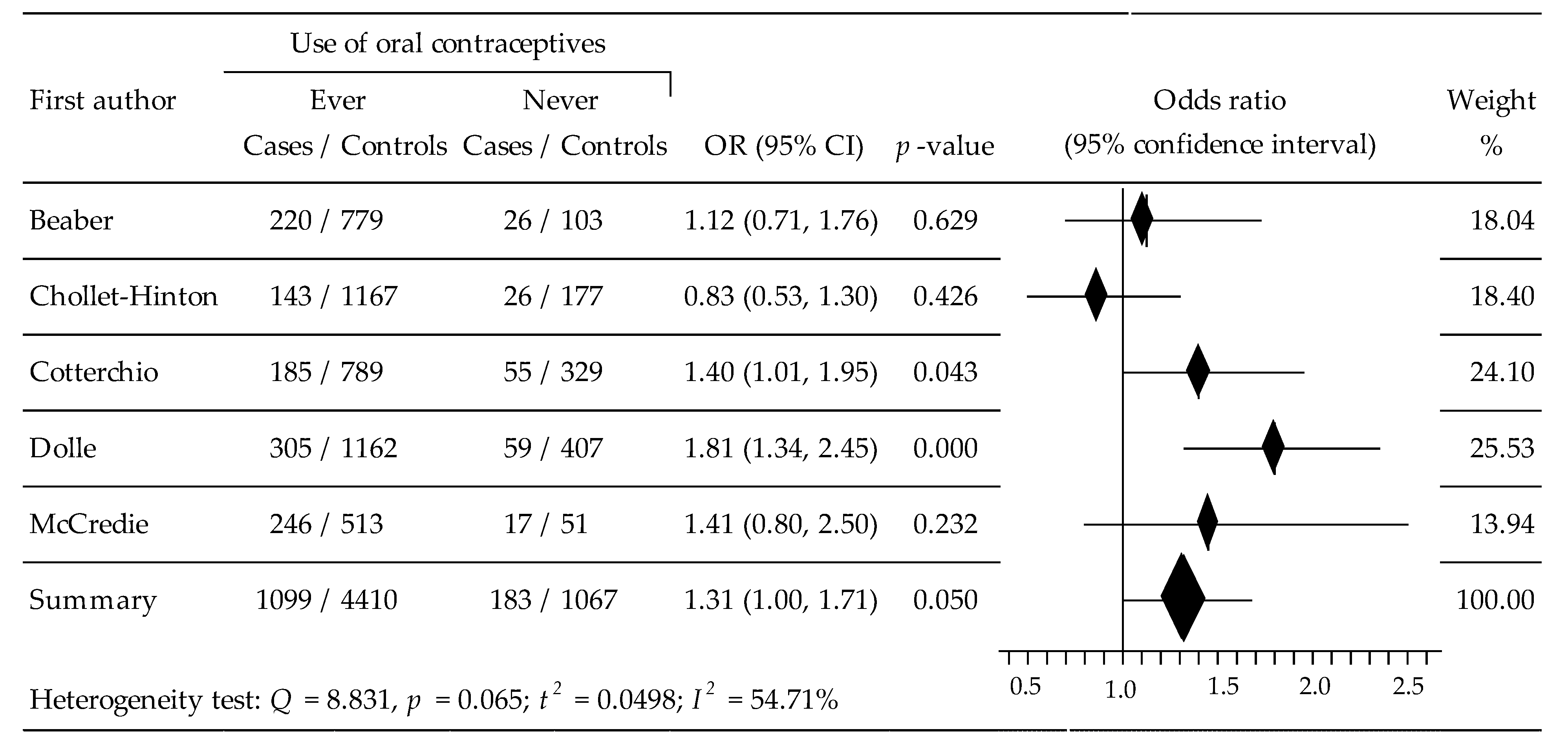
3.2. Effects of Oral Contraceptive Use on ER-Negative Subtype
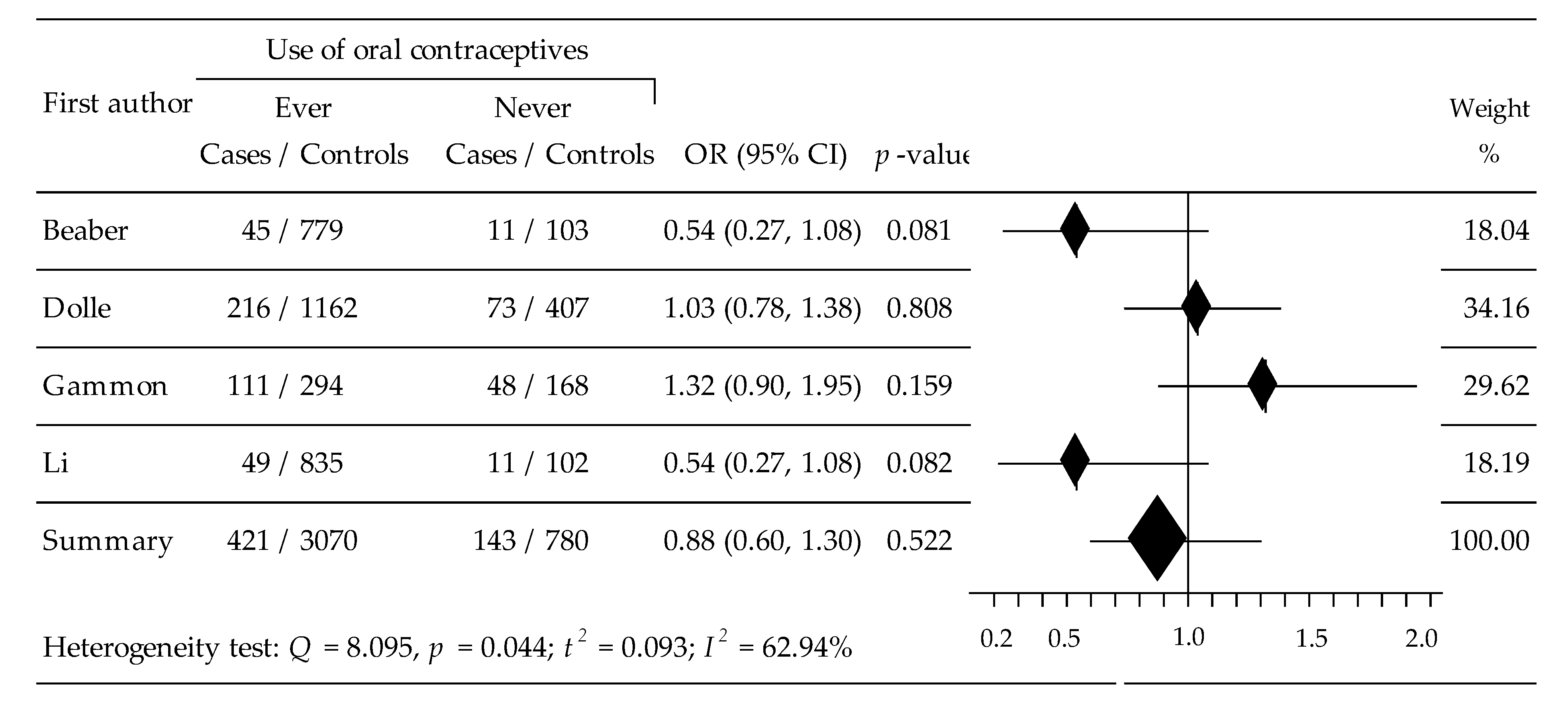
3.3. Effects of Oral Contraceptive Use on HER2-Positive Subtype
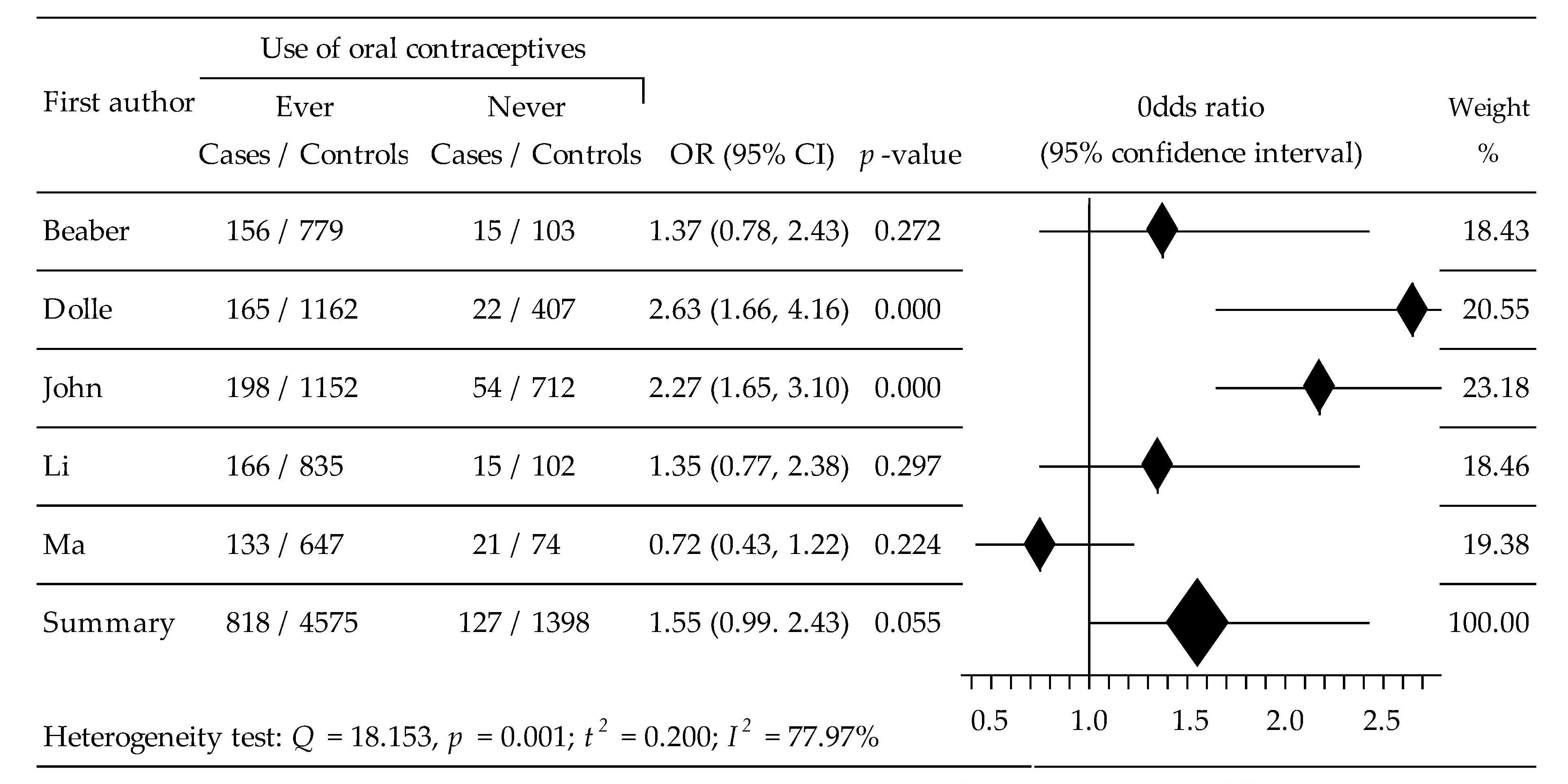
3.4. Effects of Oral Contraceptive Use on Triplet Negative Subtype
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Łukasiewicz, S.; Czeczelewski, M.; Forma, A.; Baj, J.; Sitarz, R.; Stanisławek, A. Breast Cancer—Epidemiology, Risk Factors, Classification, Prognostic Markers, and Current Treatment Strategies—An Updated Review. Cancers 2021, 13, 4287. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R. Global, regional, national burden of breast cancer in 185 countries: Evidence from GLOBOCAN 2018. Breast Cancer Res. Treat. 2021, 187, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Lynch, H.; Synder, C.; Wang, S.M. Considerations for comprehensive assessment of genetic predisposition in familial breast cancer. Breast J. 2015, 21, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Ginsburg, O.; Yip, C.H.; Brooks, A.; Cabanes, A.; Caleffi, M.; Dunstan Yataco, J.A.; Gyawali, B.; McCormack, V.; McLaughlin de Anderson, M.; Mehrotra, R.; et al. Breast cancer early detection: A phased approach to implementation. Cancer 2020, 126 (Suppl. S10), 2379–2393. [Google Scholar] [CrossRef] [PubMed]
- Latif, S.; Perveen, S.; Najib, S. Epidemiology of Carcinoma Breast in Young Adolescence Women. Cureus 2022, 14, e23683. [Google Scholar] [CrossRef]
- Gabriel, C.A.; Domchek, S.M. Breast cancer in young women. Breast Cancer Res. 2010, 12, 212. [Google Scholar] [CrossRef] [PubMed]
- Borstelmann, N.A.; Gray, T.F.; Gelber, S.; Rosenberg, S.; Zheng, Y.; Meyer, M.; Ruddy, K.J.; Schapira, L.; Come, S.; Borges, V.; et al. Psychosocial issues and quality of life of parenting partners of young women with breast cancer. Support. Care Cancer 2022, 30, 4265–4274. [Google Scholar] [CrossRef]
- Avis, N.E.; Crawford, S.; Manuel, J. Psychosocial problems among younger women with breast cancer. Psychooncology 2004, 13, 295–308. [Google Scholar] [CrossRef]
- Howell, D.M.; Metcalfe, K.; Kong, S.; Stephen, J.; Olivotto, I.A.; Baxter, N.; Friedenreich, C.M.; Warner, E.; Akbari, M.R.; McBain, K.; et al. Risk factors for psychological morbidity and the protective role of coping self-efficacy in young women with breast cancer early in diagnosis: A national multicentre cohort study. Breast Cancer Res. Treat. 2022, 194, 91–102. [Google Scholar] [CrossRef]
- Li, X.; Zhou, J.; Xiao, M.; Zhao, L.; Zhao, Y.; Wang, S.; Gao, S.; Zhuang, Y.; Niu, Y.; Li, S.; et al. Uncovering the Subtype-Specific Molecular Characteristics of Breast Cancer by Multiomics Analysis of Prognosis-Associated Genes, Driver Genes, Signaling Pathways, and Immune Activity. Front. Cell Dev. Biol. 2021, 1, 689028. [Google Scholar] [CrossRef]
- Munzone, E.; Botteri, E.; Sandri, M.T.; Esposito, A.; Adamoli, L.; Zorzino, L.; Sciandivasci, A.; Cassatella, M.C.; Rotmensz, N.; Aurilio, G.; et al. Prognostic value of circulating tumor cells according to immunohistochemically defined molecular subtypes in advanced breast cancer. Clin. Breast Cancer 2012, 12, 340–346. [Google Scholar] [CrossRef]
- Ferguson, N.L.; Bell, J.; Heidel, R.; Lee, S.; Vanmeter, S.; Duncan, L.; Munsey, B.; Panella, T.; Orucevic, A. rognostic value of breast cancer subtypes, Ki-67 proliferation index, age, and pathologic tumor characteristics on breast cancer survival in Caucasian women. Breast J. 2013, 19, 22–30. [Google Scholar] [CrossRef]
- Colombo, P.-E.; Milanezi, F.; Weigelt, B.; Reis-Filho, J.S. Microarrays in the 2010s: The contribution of microarray-based gene expression profiling to breast cancer classification, prognostication and prediction. Breast Cancer Res. 2011, 13, 212. [Google Scholar] [CrossRef]
- Coleman, W.B.; Anders, C.K. Discerning clinical responses in breast cancer based on molecular signatures. Am. J. Pathol. 2017, 187, 2199–2207. [Google Scholar] [CrossRef] [PubMed]
- Rosato, V.; Bosetti, C.; Negri, E.; Talamini, R.; Dal Maso, L.; Malvezzi, M.; Falcini, F.; Montella, M.; La Vecchia, C. Reproductive and hormonal factors, family history, and breast cancer according to the hormonal receptor status. Eur. J. Cancer Prev. 2014, 23, 412–417. [Google Scholar] [CrossRef]
- Lambertini, M.; Santoro, L.; Del Mastro, L.; Nguyen, B.; Livraghi, L.; Ugolini, D.; Peccatori, F.A.; Azim, H.A., Jr. Reproductive behaviors and risk of developing breast cancer according to tumor subtype: A systematic review and meta-analysis of epidemiological studies. Cancer Treat. Rev. 2016, 49, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Hankinson, S.E. Endogenous steroid hormone concentrations and risk of breast cancer among premenopausal women. J. Natl. Cancer Inst. 2006, 98, 1406–1415. [Google Scholar]
- Barnard, M.E.; Boeke, C.E.; Tamimi, R.M. Established breast cancer risk factors and risk of intrinsic tumor subtypes. Biochim. Biophys. Acta 2015, 1856, 73–85. [Google Scholar] [CrossRef]
- Gonzalez, R.; Reingold, B.K.; Gao, X.; Gaidhu, M.P.; Tsushima, R.G.; Unniappan, S. Nesfatin-1 exerts a direct, glucose-dependent insulinotropic action on mouse islet beta- and MIN6 cells. J. Endocrinol. 2011, 208, R9–R16. [Google Scholar] [CrossRef]
- Bardaweel, S.K.; Akour, A.A.; Al-Muhaissen, S.; AlSalamat, H.A.; Ammar, K. Oral contraceptive and breast cancer: Do benefits outweigh the risks? A case—Control study from Jordan. BMC Women Health 2019, 19, 72. [Google Scholar] [CrossRef]
- Kanadys, W.; Barańska, A.; Malm, M.; Błaszczuk, A.; Polz-Dacewicz, M.; Janiszewska, M.; Jędrych, M. Use of oral contraceptives as a potential risk factor for breast cancer: A systematic review and meta-analysis of case-control studies up to 2010. Int. J. Environ. Res. Public Health 2021, 18, 4638. [Google Scholar] [CrossRef]
- Barańska, A.; Błaszczuk, A.; Kanadys, W.; Malm, M.; Drop, K.; Polz-Dacewicz, M. Oral contraceptive use and breast cancer risk assessment: A systematic review and meta-analysis of case-control studies, 2009–2020. Cancers 2021, 13, 5654. [Google Scholar] [CrossRef]
- Mørch, L.S.; Skovlund, C.W.; Hannaford, P.C.; Iversen, L.; Fielding, S.; Lidegaard, Ø. Contemporary Hormonal Contraception and the Risk of Breast Cancer. N. Engl. J. Med. 2017, 77, 2228–2239. [Google Scholar] [CrossRef]
- Hunter, D.J.; Colditz, G.A.; Hankinson, S.E.; Malspeis, S.; Spiegelman, D.; Chen, W.; Stampfer, M.J.; Willett, W.C. Oral contraceptive use and breast cancer: A prospective study of young women. Cancer Epidemiol. Biomark. Prev. 2010, 19, 2496–2502. [Google Scholar] [CrossRef]
- Barańska, A.; Dolar-Szczasny, J.; Kanadys, W.; Kinik, W.; Ceglarska, D.; Religioni, U.; Rejdak, R. Oral contraceptive use and breast cancer risk according to molecular subtypes status: A systematic review and meta-analysis of case-control studies. Cancers 2022, 14, 574. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in metaanalyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Baker, W.L.; White, C.M.; Cappelleri, J.C.; Kluger, J.; Coleman, C.I. Health Outcomes, Policy, and Economics (HOPE) Collaborative Group. Understanding heterogeneity in meta-analysis: The role of meta-regression. Int. J. Clin. Pract. 2009, 63, 1426–1434. [Google Scholar] [CrossRef] [PubMed]
- Gammon, M.D.; Hibshoosh, H.; Terry, M.B.; Bose, S.; Schoenberg, J.B.; Brinton, L.A.; Bernstein, J.L.; Thompson, W.D. Oral contraceptive use and other risk factors in relation to HER-2/neu overexpression in breast cancer among young women. Cancer Epidemiol. Biomark. Prev. 1999, 8, 413–419. [Google Scholar]
- McCredie, M.R.; Dite, G.; Southey, M.C.; Venter, D.J.; Giles, G.; Hopper, J.L. Risk factors for breast cancer in young women by oestrogen receptor and progesterone receptor status. Br. J. Cancer 2003, 89, 1661–1663. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cotterchio, M.; Kreiger, N.; Theis, B.; Sloan, M.; Bahl, S. Hormonal factors and the risk of breast cancer according to estrogen and progesterone-receptor subgroup. Cancer Epidemiol. Biomark. Prev. 2003, 12, 1053–1060. [Google Scholar]
- Dolle, J.M.; Daling, J.R.; White, E.; Brinton, L.A.; Doody, D.R.; Porter, P.L.; Malone, K.E. Risk factors for triple-negative breast cancer in women under the age of 45 years. Cancer Epidemiol. Biomark. Prev. 2009, 18, 1157–1166. [Google Scholar] [CrossRef]
- Ma, H.; Wang, Y.; Sullivan-Halley, J.; Weiss, L.; Marchbanks, P.A.; Spirtas, R.; Ursin, G.; Burkman, R.T.; Simon, M.S.; Malone, K.E.; et al. Use of four biomarkers to evaluate the risk of breast cancer subtypes in the women’s contraceptive and reproductive experiences study. Cancer Res. 2010, 70, 575–587. [Google Scholar] [CrossRef]
- Li, C.I.; Beaber, E.F.; Tang, M.T.C.; Porter, P.L.; Daling, J.R.; Malone, K.E. Reproductive factors and risk of estrogen receptor positive, triple-negative, and HER2-neu overexpressing breast cancer among women 20–44 years of age. Breast Cancer Res. Treat. 2013, 137, 579–587. [Google Scholar] [CrossRef]
- Beaber, E.F.; Malone, K.E.; Tang, M.-T.C.; Barlow, W.E.; Porter, P.L.; Daling, J.R.; Li, C. Oral contraceptives and breast cancer risk overall and by molecular subtype among young women. Cancer Epidemiol. Biomark. Prev. 2014, 23, 755–764. [Google Scholar] [CrossRef]
- Chollet-Hinton, L.; Olshan, A.F.; Nichols, H.B.; Anders, C.K.; Lund, J.L.; Allott, E.H.; Bethea, T.N.; Hong, C.C.; Cohen, S.M.; Khoury, T.; et al. Biology and etiology of young-onset breast cancers among premenopausal African American women: Results from the AMBER Consortium. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1722–1729. [Google Scholar] [CrossRef]
- John, E.M.; Hines, L.M.; Phipps, A.I.; Koo, J.; Longacre, T.A.; Ingles, S.A.; Baumgartner, K.B.; Slattery, M.L.; Wu, A.H. Reproductive history, breast-feeding and risk of triple negative breast cancer: The Breast Cancer Etiology in Minorities (BEM) study. Int. J. Cancer 2018, 142, 2273–2285. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhong, Y.; Zhang, H.; Yu, H.; Huang, Y.; Li, Z.; Chen, G.; Hua, X. Association between oral contraceptive use as a risk factor and triple-negative breast cancer: A systematic review and meta-analysis. Mol. Clin. Oncol. 2017, 7, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Kahlenborn, C.; Modugno, F.; Potter, D.M.; Severs, W.B. Oral contraceptive use as a risk factor for premenopausal breast cancer: A meta-analysis. Mayo Clin. Proc. 2006, 81, 1290–1302. [Google Scholar] [CrossRef] [PubMed]
- Bethea, T.N.; Rosenberg, L.; Hong, C.C.; Troester, M.A.; Lunetta, K.L.; Bandera, E.V.; Schedin, P.; Kolonel, L.N.; Olshan, A.F.; Ambrosone, C.B.; et al. A case–control analysis of oral contraceptive use and breast cancer subtypes in the African American Breast Cancer Epidemiology and Risk Consortium. Breast Cancer Res. 2015, 17, 22. [Google Scholar] [CrossRef] [PubMed]
- Gaudet, M.M.; Press, M.F.; Haile, R.W.; Lynch, C.F.; Glaser, S.L.; Schildkraut, J.; Gammon, M.D.; Thompson, W.D.; Bernstein, J.L. Risk factors by molecular subtypes of breast cancer across a population-based study of women 56 years or younger. Breast Cancer Res. Treat. 2011, 130, 587–597. [Google Scholar] [CrossRef]

| Authors [Ref.] Publication Year | Country | Study Year | Age Range | Breast Cancer Subtype; N (n%) | NOS Score |
|---|---|---|---|---|---|
| Gammon [33] 1999 | USA | 1990–1992 | 20–40 | HER2+: 159 (69.8); CRL: 462 (63.6) | 4 |
| McCredie [34] 2003 | Australia | 1992–1999 | <40 | ER+: 357 (92.7); ER−: 261 (93.5); CRL: 564 (91.0) | 6 |
| Cotterchio [35] 2003 | Canada | 1995–1998 | <50 | ER+: 439 (67.0); ER−: 240 (77.1); CRL: 1118 (70.6) | 6 |
| Dolle [36] 2009 | USA | 1983–1992 | 21–45 | ER+: 532 (74.1); ER−: 364 (83.8); HER2+: 289 (74.7); TN: 187 (88.2); CRL: 1569 (74.1) | 8 |
| Ma [37] 2010 | USA | 1994–1998 | 35–44 | ER+: 197 (88.8%); TN: 154 (86.4%); CRL: 721 (89.7%) | 7 |
| Li [38] 2013 | USA | 2004–2010 | 20–44 | ER+: 767 (88.1); HER2+: 60 (81.7); TN: 181 (91.7); CRL: 937 (89.1) | 8 |
| Beaber [39] 2014 | USA | 2004–2010 | 20–44 | ER+: 730 (87.4), ER−: 246 (89.4); HER2+: 56 (80.4); TN: 171 (91.2); CRL: 882 (88.3) | 8 |
| Chollet-Hinton [40] 2017 | USA | 1996–2001 | <40 | ER+: 162 (81.5); ER−: 169 (86.6); CRL: 1347 (86.8) | 8 |
| John [41] 2018 | USA | 1995–2009 | <50 | TN: 252 (78.6); CRL: 2223 (67.8) | 7 |
| Molecular Subtypes of Breast Cancer | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ER-Positive | ER-Negative | HER2-Overexpressing | Triplet-Negative | |||||||||||||
| OR (95% CI) | p | I2 (%) | Ref. | OR (95% CI) | p | I2 (%) | Ref. | OR (95% CI) | p | I2 (%) | Ref. | OR (95% CI) | p | I2 (%) | Ref. | |
| Cases/Controls | Cases/Controls | Cases/Controls | Cases/Controls | |||||||||||||
| Use of contraceptive | 0.91 (0.81, 1.03) | 0.128 | 00.00 | [34,35,36,37,38,39,40] | 1.31 (1.00, 1.71) | 0.050 | 54.71 | [34,35,36,39,40] | 0.88 (0.60, 1.30) | 0.522 | 62.94 | [33,36,38,39] | 1.55 (0.99, 2.43) | 0.055 | 77.97 | [36,37,38,39,41] |
| ever/never | 3184/7144 | 1282/5477 | 564/3850 | 945/5973 | ||||||||||||
| Duration of contraceptive use | 0.89 (0.77, 1.04) | 0.141 | 00.00 | [35,36,37,38] | Inaccessible | 1.00 (0.67, 1.51) | 0.991 | 58.57 | [33,36,38] | 1.59 (0.76, 3.32) | 0.218 | 82.14 | [36,37,38] | |||
| ≥5 y/<5 y | 1539/3111 | 376/2291 | 464/2644 | |||||||||||||
| Time last use prior to diagnosis | 0.89 (0.64, 1.24) | 0.493 | 52.91 | [36,37,39] | Inaccessible | 0.90 (0.64, 1.26) | 0.537 | 19.30 | [33,36,39] | 1.47 (0.66, 3.25) | 0.340 | 81.18 | [36,37,39] | |||
| <5 y/≥5 y | 869/2096 | 349/1743 | 368/2196 | |||||||||||||
| Age at first Ocs use | Inaccessible | Inaccessible | Inaccessible | Inaccessible | ||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barańska, A. Oral Contraceptive Use and Assessment of Breast Cancer Risk among Premenopausal Women via Molecular Characteristics: Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 15363. https://doi.org/10.3390/ijerph192215363
Barańska A. Oral Contraceptive Use and Assessment of Breast Cancer Risk among Premenopausal Women via Molecular Characteristics: Systematic Review with Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(22):15363. https://doi.org/10.3390/ijerph192215363
Chicago/Turabian StyleBarańska, Agnieszka. 2022. "Oral Contraceptive Use and Assessment of Breast Cancer Risk among Premenopausal Women via Molecular Characteristics: Systematic Review with Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 22: 15363. https://doi.org/10.3390/ijerph192215363
APA StyleBarańska, A. (2022). Oral Contraceptive Use and Assessment of Breast Cancer Risk among Premenopausal Women via Molecular Characteristics: Systematic Review with Meta-Analysis. International Journal of Environmental Research and Public Health, 19(22), 15363. https://doi.org/10.3390/ijerph192215363







