The Effect of a Combined Exercise Program on Postural Control and Fine Motor Skills in Parkinson’s Disease: Study Design
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.2.1. Preliminary Evaluations
2.2.2. Sample Size
2.2.3. PRE and POST Evaluations
- -
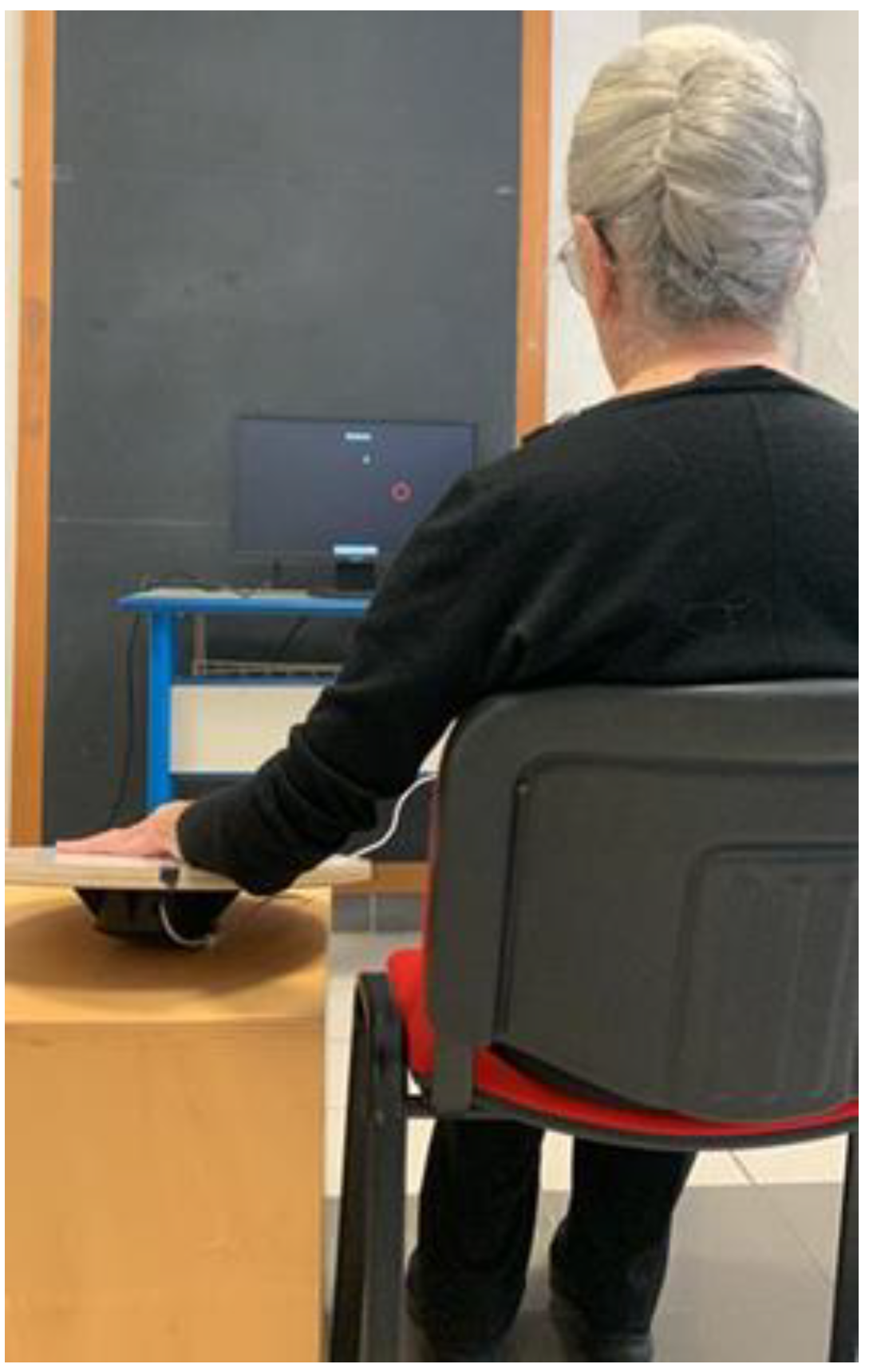
- Wobble Board
- -
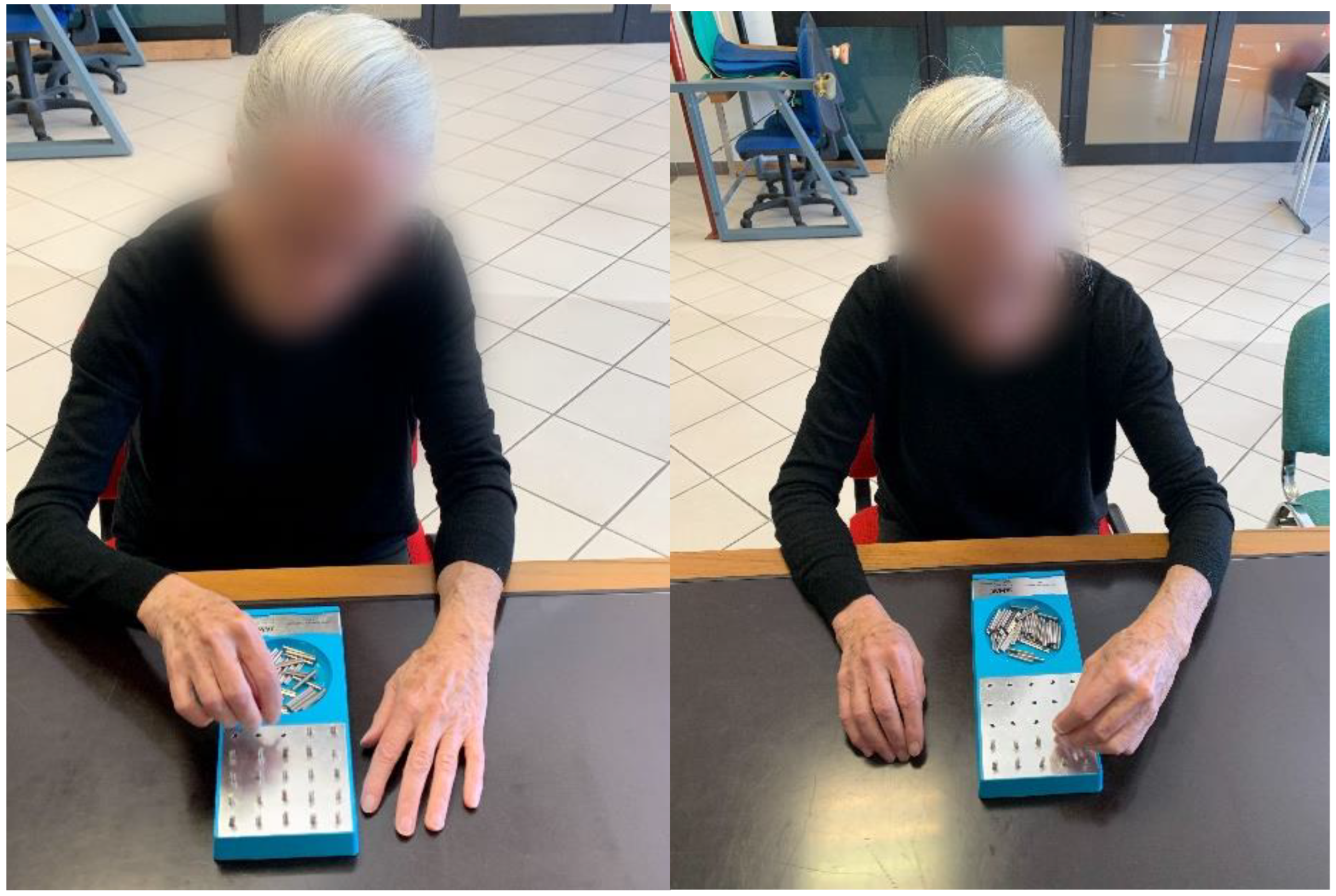
- Grooved Pegboard Test
2.2.4. Intervention
- -
- PD group
- Postural control exercises: bipodalic and monopodalic position (3 sets for 30-s (for limb)); stand up on the feet’ sole (10 repetitions, 3 sets); stand up on heels (10 repetitions, 3 sets); calf raises (10 repetitions, 3 sets); hip abduction (12 repetitions, 3 sets); get up and sit down from a chair (5 repetitions); walking with stop (5 min); walking with change of direction (5 min); walking on a stable surfaces (5 min); walking on an unstable surfaces (5 min); walking with a tennis ball in hands (5 min) and walking and crossing several obstacles (5 min).
- Fine motor skills exercises for lower limbs: in sitting position, lift legs forward by placing a tennis ball between the feet trying not to let it fall (10 repetitions, 3 sets); sitting position and barefoot, grab and drop a towel with toes (for limb) (10 repetitions, 3 sets); pass a tennis ball from foot to foot (20 steps); and in sitting position and barefoot, play a musical carpet (5 min) and toe raises with an elastic band (10 repetitions, 3 sets (for limb)).
- Fine motor skills for upper limbs: paper folding (5 repetitions, 3 sets); play a musical carpet (3 min); create shapes with paper (5 min); finger painting (5 min); trace a drawing (3 min); make bracelets (5 min); count coins and put in a moneybox; close a bottle (10 repetitions, 3 sets); press stamp on paper (10 repetitions, 3 sets); make letters from plasticine (3 min); and press shaped blocks on plasticine (3 min).
- -
- CON group
- Stretching during seated position: straight arm forward rotation; straight arm backward rotation; straight arm up and down flapping; straight arm horizontal abduction and adduction; trunk rotation and hold. During standing position (with hands rest on chair back): hamstring stretch; calf stretch; upper trapezius stretch; straight leg forward kick; straight leg backward kick; straight leg hip adduction and abduction; and alternate knee raise (30-s, 2 cycles with 20 s rest in between) [35].
2.2.5. Work Environment and Safety of Procedures
2.2.6. Statistical Analysis
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Harman, D. The Aging Process. Proc. Natl. Acad. Sci. USA 1981, 78, 7124–7128. [Google Scholar] [CrossRef] [PubMed]
- de Rijk, M.C.; Tzourio, C.; Breteler, M.M.; Dartigues, J.F.; Amaducci, L.; Lopez-Pousa, S.; Manubens-Bertran, J.M.; Alperovitch, A.; Rocca, W.A. Prevalence of Parkinsonism and Parkinson’s Disease in Europe: The EUROPARKINSON Collaborative Study. European Community Concerted Action on the Epidemiology of Parkinson’s Disease. J. Neurol. Neurosurg. Psychiatry 1997, 62, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Ou, Z.; Pan, J.; Tang, S.; Duan, D.; Yu, D.; Nong, H.; Wang, Z. Global Trends in the Incidence, Prevalence, and Years Lived With Disability of Parkinson’s Disease in 204 Countries/Territories From 1990 to 2019. Front. Public Health 2021, 9, 10–15. [Google Scholar] [CrossRef]
- Obeso, J.A.; Rodriguez-Oroz, M.C.; Goetz, C.G.; Marin, C.; Kordower, J.H.; Rodriguez, M.; Hirsch, E.C.; Farrer, M.; Schapira, A.H.V.; Halliday, G. Missing Pieces in the Parkinson’s Disease Puzzle. Nat. Med. 2010, 16, 653–661. [Google Scholar] [CrossRef]
- Fukunaga, J.Y.; Quitschal, R.M.; Doná, F.; Ferraz, H.B.; Ganança, M.M.; Caovilla, H.H. Postural Control in Parkinson’s Disease. Braz. J. Otorhinolaryngol. 2014, 80, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.; Hong, C.T.; Chen, J.-H.; Chan, L.; Chi, W.-C.; Yen, C.-F.; Liao, H.-F.; Liou, T.-H.; Wu, D. Hand Fine Motor Skill Disability Correlates with Cognition in Patients with Moderate-to-Advanced Parkinson’s Disease. Brain Sci. 2020, 10, 337. [Google Scholar] [CrossRef] [PubMed]
- Muslimovic, D.; Post, B.; Speelman, J.D.; Schmand, B.; de Haan, R.J. Determinants of Disability and Quality of Life in Mild to Moderate Parkinson Disease. Neurology 2008, 70, 2241–2247. [Google Scholar] [CrossRef]
- Hertel, J.; Braham, R.A.; Hale, S.A.; Olmsted-Kramer, L.C. Simplifying the Star Excursion Balance Test: Analyses of Subjects With and Without Chronic Ankle Instability. J. Orthop. Sport. Phys. Ther. 2006, 36, 131–137. [Google Scholar] [CrossRef]
- Olmsted, L.C.; Carcia, C.R.; Hertel, J.; Shultz, S.J. Efficacy of the Star Excursion Balance Tests in Detecting Reach Deficits in Subjects With Chronic Ankle Instability. J. Athl. Train. 2002, 37, 501–506. [Google Scholar]
- Fusco, A.; Giancotti, G.F.; Fuchs, P.X.; Wagner, H.; Varalda, C.; Capranica, L.; Cortis, C. Dynamic Balance Evaluation: Reliability and Validity of a Computerized Wobble Board. J. Strength Cond. Res. 2020, 34, 1709–1715. [Google Scholar] [CrossRef]
- Fusco, A.; Giancotti, G.F.; Fuchs, P.X.; Wagner, H.; Varalda, C.; Cortis, C. Wobble Board Balance Assessment in Subjects with Chronic Ankle Instability. Gait Posture 2019, 68, 352–356. [Google Scholar] [CrossRef] [PubMed]
- De Maio, M.; Cortis, C.; Iannaccone, A.; da Silva, R.A.; Fusco, A. Association between Anthropometric Variables, Sex, and Visual Biofeedback in Dynamic Postural Control Assessed on a Computerized Wobble Board. Appl. Sci. 2021, 11, 8370. [Google Scholar] [CrossRef]
- Liu, H.; An, J.; Wang, J. Preliminary Study of the Olduvai Termination Recorded in the Red Loam in Southeast Shanxi Province, China. J. Geomagn. Geoelectr. 1993, 45, 331–338. [Google Scholar] [CrossRef]
- D’Hondt, E.; Deforche, B.; De Bourdeaudhuij, I.; Lenoir, M. Childhood Obesity Affects Fine Motor Skill Performance under Different Postural Constraints. Neurosci. Lett. 2008, 440, 72–75. [Google Scholar] [CrossRef] [PubMed]
- da Silva, E.S.M.; Santos, G.L.; Catai, A.M.; Borstad, A.; Furtado, N.P.D.; Aniceto, I.A.V.; Russo, T.L. Effect of Aerobic Exercise Prior to Modified Constraint-Induced Movement Therapy Outcomes in Individuals with Chronic Hemiparesis: A Study Protocol for a Randomized Clinical Trial. BMC Neurol. 2019, 19, 196. [Google Scholar] [CrossRef]
- Gershon, R.C.; Cella, D.; Fox, N.A.; Havlik, R.J.; Hendrie, H.C.; Wagster, M.V. Assessment of Neurological and Behavioural Function: The NIH Toolbox. Lancet Neurol. 2010, 9, 138–139. [Google Scholar] [CrossRef]
- Bezdicek, O.; Nikolai, T.; Hoskovcová, M.; Štochl, J.; Brožová, H.; Dušek, P.; Zárubová, K.; Jech, R.; Růžička, E. Grooved Pegboard Predicates More of Cognitive Than Motor Involvement in Parkinson’s Disease. Assessment 2014, 21, 723–730. [Google Scholar] [CrossRef]
- Amato, A.; Baldassano, S.; Vasto, S.; Schirò, G.; Davì, C.; Drid, P.; Dos Santos Mendes, F.A.; Caldarella, R.; D’Amelio, M.; Proia, P. Effects of a Resistance Training Protocol on Physical Performance, Body Composition, Bone Metabolism, and Systemic Homeostasis in Patients Diagnosed with Parkinson’s Disease: A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 13022. [Google Scholar] [CrossRef]
- Smania, N.; Corato, E.; Tinazzi, M.; Stanzani, C.; Fiaschi, A.; Girardi, P.; Gandolfi, M. Effect of Balance Training on Postural Instability in Patients With Idiopathic Parkinson’s Disease. Neurorehabilit. Neural Repair 2010, 24, 826–834. [Google Scholar] [CrossRef]
- Conradsson, D.; Löfgren, N.; Nero, H.; Hagströmer, M.; Ståhle, A.; Lökk, J.; Franzén, E. The Effects of Highly Challenging Balance Training in Elderly With Parkinson’s Disease. Neurorehabil. Neural Repair 2015, 29, 827–836. [Google Scholar] [CrossRef]
- Schlenstedt, C.; Paschen, S.; Kruse, A.; Raethjen, J.; Weisser, B.; Deuschl, G. Resistance versus Balance Training to Improve Postural Control in Parkinson’s Disease: A Randomized Rater Blinded Controlled Study. PLoS ONE 2015, 10, e0140584. [Google Scholar] [CrossRef] [PubMed]
- Vanbellingen, T.; Nyffeler, T.; Nigg, J.; Janssens, J.; Hoppe, J.; Nef, T.; Müri, R.M.; van Wegen, E.E.H.; Kwakkel, G.; Bohlhalter, S. Home Based Training for Dexterity in Parkinson’s Disease: A Randomized Controlled Trial. Park. Relat. Disord. 2017, 41, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Vorasoot, N.; Termsarasab, P.; Thadanipon, K.; Pulkes, T. Effects of Handwriting Exercise on Functional Outcome in Parkinson Disease: A Randomized Controlled Trial. J. Clin. Neurosci. 2020, 72, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Riebe, D.; Ehrman, J.; Liguori, G. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2021. [Google Scholar]
- Yang, W.; Hamilton, J.L.; Kopil, C.; Beck, J.C.; Tanner, C.M.; Albin, R.L.; Ray Dorsey, E.; Dahodwala, N.; Cintina, I.; Hogan, P.; et al. Current and Projected Future Economic Burden of Parkinson’s Disease in the U.S. Npj Park. Dis. 2020, 6, 15. [Google Scholar] [CrossRef]
- Cheon, S.-M.; Chae, B.-K.; Sung, H.-R.; Lee, G.C.; Kim, J.W. The Efficacy of Exercise Programs for Parkinson’s Disease: Tai Chi versus Combined Exercise. J. Clin. Neurol. 2013, 9, 237. [Google Scholar] [CrossRef]
- De Maio, M.; Bratta, C.; Iannaccone, A.; Castellani, L.; Foster, C.; Cortis, C.; Fusco, A. Home-Based Physical Activity as a Healthy Aging Booster before and during COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2022, 19, 4317. [Google Scholar] [CrossRef]
- Duncan, M.J.; Rosenkranz, R.R.; Vandelanotte, C.; Caperchione, C.M.; Rebar, A.L.; Maeder, A.J.; Tague, R.; Savage, T.N.; van Itallie, A.; Mummery, W.K.; et al. What Is the Impact of Obtaining Medical Clearance to Participate in a Randomised Controlled Trial Examining a Physical Activity Intervention on the Socio-Demographic and Risk Factor Profiles of Included Participants? Trials 2016, 17, 580. [Google Scholar] [CrossRef]
- Mahieux, F.; Michelet, D.; Manifacier, M.-J.; Boller, F.; Fermanian, J.; Guillard, A. Mini-Mental Parkinson: First Validation Study of a New Bedside Test Constructed for Parkinson’s Disease. Behav. Neurol. 1995, 8, 15–22. [Google Scholar] [CrossRef]
- Hoenh, M.; Yahr, M. Parkinsonism: Onset, Progression and Mortality. Neurology 1967, 17, 427–442. [Google Scholar]
- WHO. Physical Status: The Use and Interpretation of Anthropometry: Report of a World Health Organization (WHO) Expert Committee; World Health Organization: Geneva, Switzerland, 1995; Volume 854, pp. 1–452. [Google Scholar]
- Fusco, A.; Fuchs, P.X.; De Maio, M.; Wagner, H.; Cortis, C. A Novel Approach to Measuring Wobble Board Performance in Individuals with Chronic Ankle Instability. Heliyon 2020, 6, e04937. [Google Scholar] [CrossRef]
- Petrigna, L.; Pajaujiene, S.; Iacona, G.M.; Thomas, E.; Paoli, A.; Bianco, A.; Palma, A. The Execution of the Grooved Pegboard Test in a Dual-Task Situation: A Pilot Study. Heliyon 2020, 6, e04678. [Google Scholar] [CrossRef] [PubMed]
- Alexandre de Assis, I.S.; Luvizutto, G.J.; Bruno, A.C.M.; Sande de Souza, L.A.P. The Proprioceptive Neuromuscular Facilitation Concept in Parkinson Disease: A Systematic Review and Meta-Analysis. J. Chiropr. Med. 2020, 19, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Kwok, J.Y.Y.; Kwan, J.C.Y.; Auyeung, M.; Mok, V.C.T.; Lau, C.K.Y.; Choi, K.C.; Chan, H.Y.L. Effects of Mindfulness Yoga vs Stretching and Resistance Training Exercises on Anxiety and Depression for People With Parkinson Disease. JAMA Neurol. 2019, 76, 755. [Google Scholar] [CrossRef] [PubMed]
- Romero, D.H.; Stelmach, G.E. Changes in Postural Control with Aging and Parkinson’s Disease. IEEE Eng. Med. Biol. Mag. 2003, 22, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Bjorklund, G.; Stejskal, V.; Urbina, M.A.; Dadar, M.; Chirumbolo, S.; Mutter, J. Metals and Parkinson’s Disease: Mechanisms and Biochemical Processes. Curr. Med. Chem. 2018, 25, 2198–2214. [Google Scholar] [CrossRef] [PubMed]
- Dahdal, P.; Meyer, A.; Chaturvedi, M.; Nowak, K.; Roesch, A.D.; Fuhr, P.; Gschwandtner, U. Fine Motor Function Skills in Patients with Parkinson Disease with and without Mild Cognitive Impairment. Dement. Geriatr. Cogn. Disord. 2016, 42, 127–134. [Google Scholar] [CrossRef]
- Wiratman, W.; Kobayashi, S.; Chang, F.-Y.; Asano, K.; Ugawa, Y. Assessment of Cognitive and Motor Skills in Parkinson’s Disease by a Robotic Object Hitting Game. Front. Neurol. 2019, 10, 19. [Google Scholar] [CrossRef]
- Biundo, R.; Weis, L.; Antonini, A. Cognitive Decline in Parkinson’s Disease: The Complex Picture. Npj Park. Dis. 2016, 2, 16018. [Google Scholar] [CrossRef]
- Kalyani, H.H.; Sullivan, K.A.; Moyle, G.M.; Brauer, S.G.; Jeffrey, E.R.; Kerr, G.K. Dance Improves Symptoms, Functional Mobility and Fine Manual Dexterity in People with Parkinson Disease: A Quasi-Experimental Controlled Efficacy Study. Eur. J. Phys. Rehabil. Med. 2020, 56, 563–574. [Google Scholar] [CrossRef]
- Kalyani, H.H.N.; Sullivan, K.A.; Moyle, G.; Brauer, S.; Jeffrey, E.R.; Kerr, G.K. Impacts of Dance on Cognition, Psychological Symptoms and Quality of Life in Parkinson’s Disease. NeuroRehabilitation 2019, 45, 273–283. [Google Scholar] [CrossRef]
- Duncan, R.P.; Earhart, G.M. Are the Effects of Community-Based Dance on Parkinson Disease Severity, Balance, and Functional Mobility Reduced with Time? A 2-Year Prospective Pilot Study. J. Altern. Complement. Med. 2014, 20, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Ni, X.; Liu, S.; Lu, F.; Shi, X.; Guo, X. Efficacy and Safety of Tai Chi for Parkinson’s Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2014, 9, e99377. [Google Scholar] [CrossRef] [PubMed]
- Cugusi, L.; Manca, A.; Bergamin, M.; Di Blasio, A.; Monticone, M.; Deriu, F.; Mercuro, G. Aquatic Exercise Improves Motor Impairments in People with Parkinson’s Disease, with Similar or Greater Benefits than Land-Based Exercise: A Systematic Review. J. Physiother. 2019, 65, 65–74. [Google Scholar] [CrossRef]
- Shen, X.; Mak, M. Repetitive Step Training with Preparatory Signals Improves Stability Limits in Patients with Parkinsonâ€TMs Disease. J. Rehabil. Med. 2012, 44, 944–949. [Google Scholar] [CrossRef] [PubMed]
- Lena, F.; Iezzi, E.; Etoom, M.; Santilli, M.; Centonze, D.; Foti, C.; Grillea, G.; Modugno, N. Effects of Postural Exercises in Patients with Parkinson’s Disease and Pisa Syndrome: A Pilot Study. NeuroRehabilitation 2017, 41, 423–428. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Maio, M.; Castellani, L.; Cugusi, L.; Cortis, C.; Fusco, A. The Effect of a Combined Exercise Program on Postural Control and Fine Motor Skills in Parkinson’s Disease: Study Design. Int. J. Environ. Res. Public Health 2022, 19, 15216. https://doi.org/10.3390/ijerph192215216
De Maio M, Castellani L, Cugusi L, Cortis C, Fusco A. The Effect of a Combined Exercise Program on Postural Control and Fine Motor Skills in Parkinson’s Disease: Study Design. International Journal of Environmental Research and Public Health. 2022; 19(22):15216. https://doi.org/10.3390/ijerph192215216
Chicago/Turabian StyleDe Maio, Marianna, Loriana Castellani, Lucia Cugusi, Cristina Cortis, and Andrea Fusco. 2022. "The Effect of a Combined Exercise Program on Postural Control and Fine Motor Skills in Parkinson’s Disease: Study Design" International Journal of Environmental Research and Public Health 19, no. 22: 15216. https://doi.org/10.3390/ijerph192215216
APA StyleDe Maio, M., Castellani, L., Cugusi, L., Cortis, C., & Fusco, A. (2022). The Effect of a Combined Exercise Program on Postural Control and Fine Motor Skills in Parkinson’s Disease: Study Design. International Journal of Environmental Research and Public Health, 19(22), 15216. https://doi.org/10.3390/ijerph192215216







