Effects of Mindfulness-Based Interventions in Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
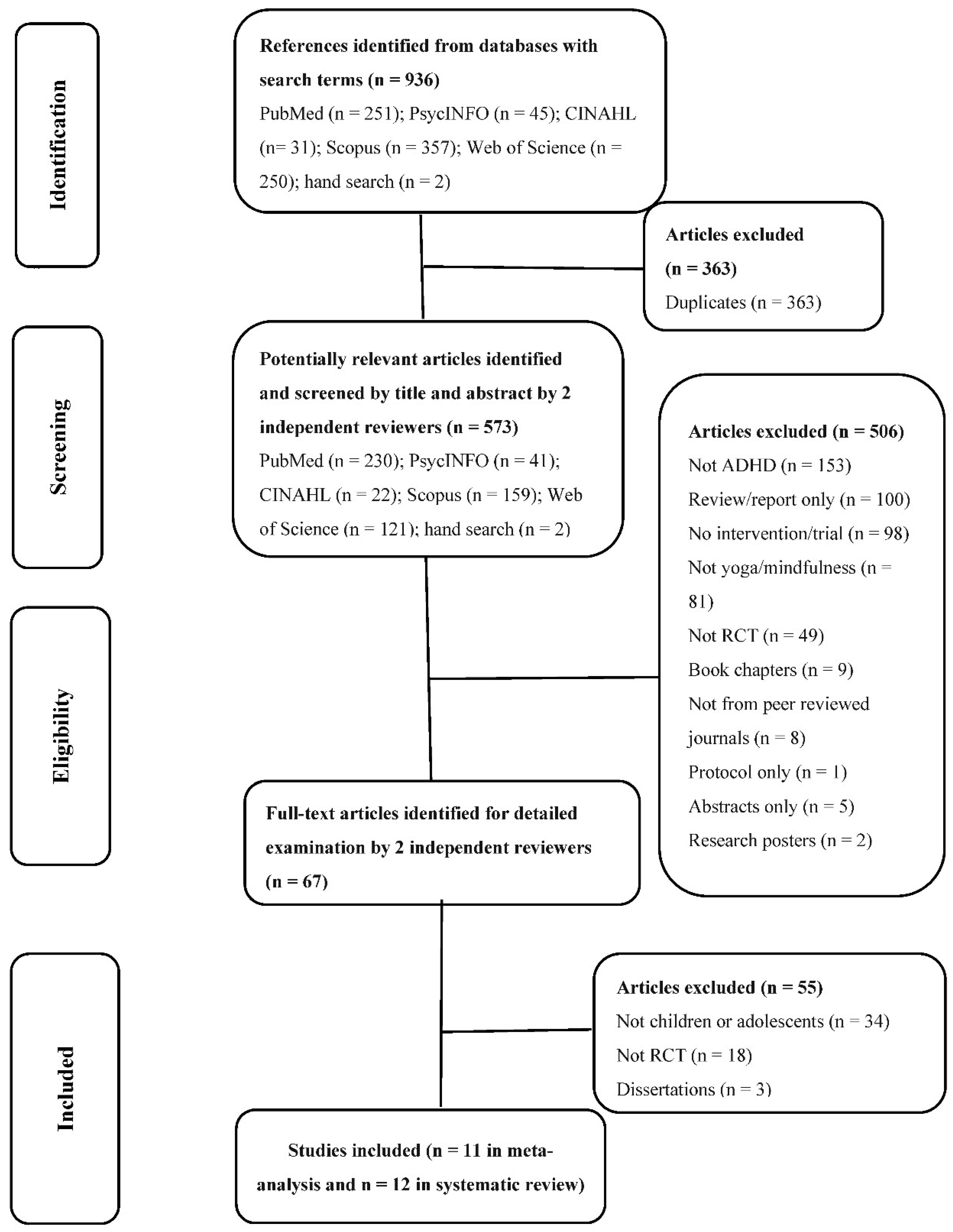
2. Method
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Methodological Quality Assessment
2.4. Data Extraction
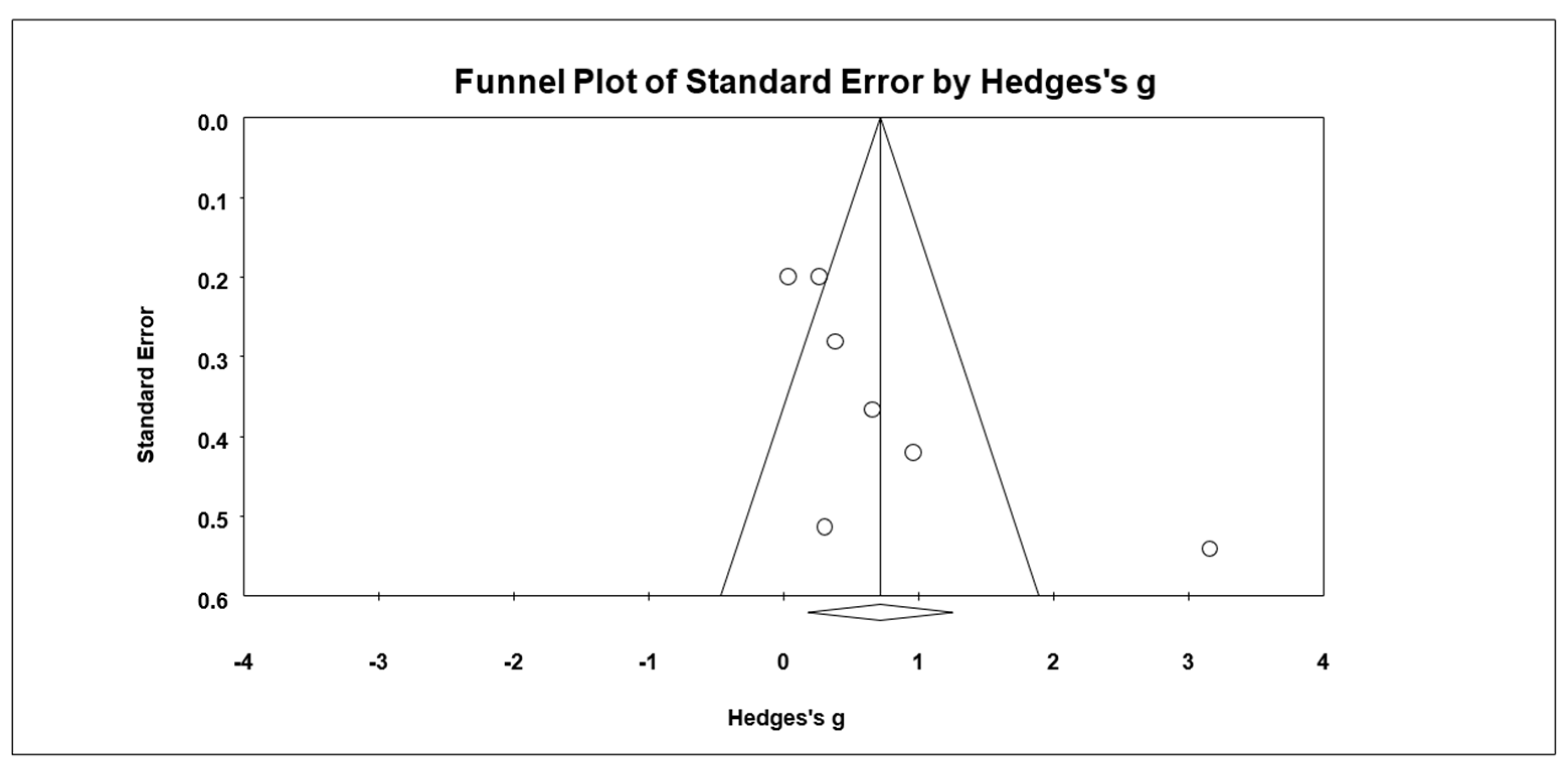
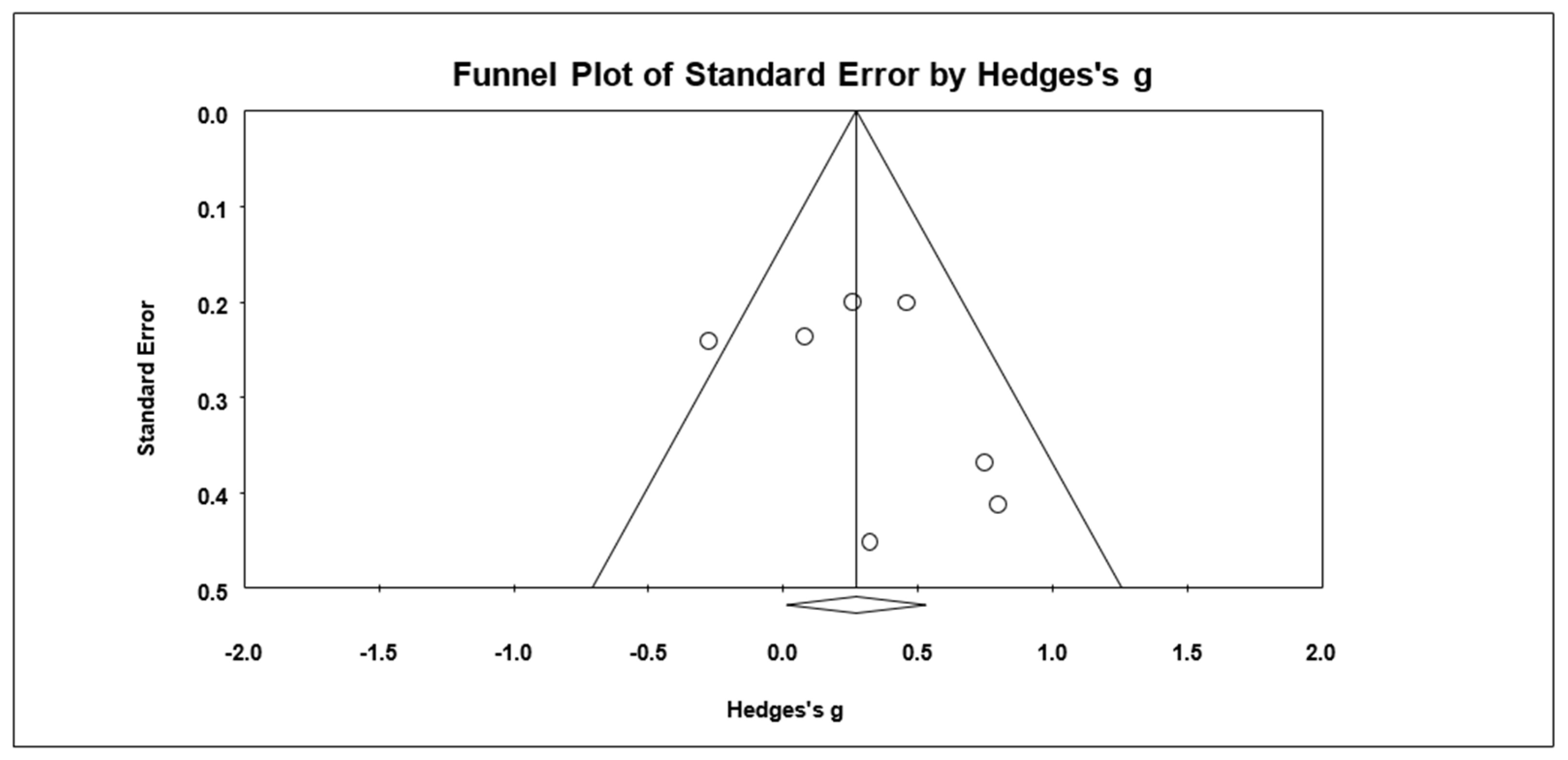
2.5. Statistical Analysis
2.6. Test of Heterogeneity and Analysis of Moderator
3. Results
3.1. Descriptions of Studies
3.2. Participants
3.3. Intervention
3.4. Control Group
3.5. Outcome Measures
3.6. Quality Assessment
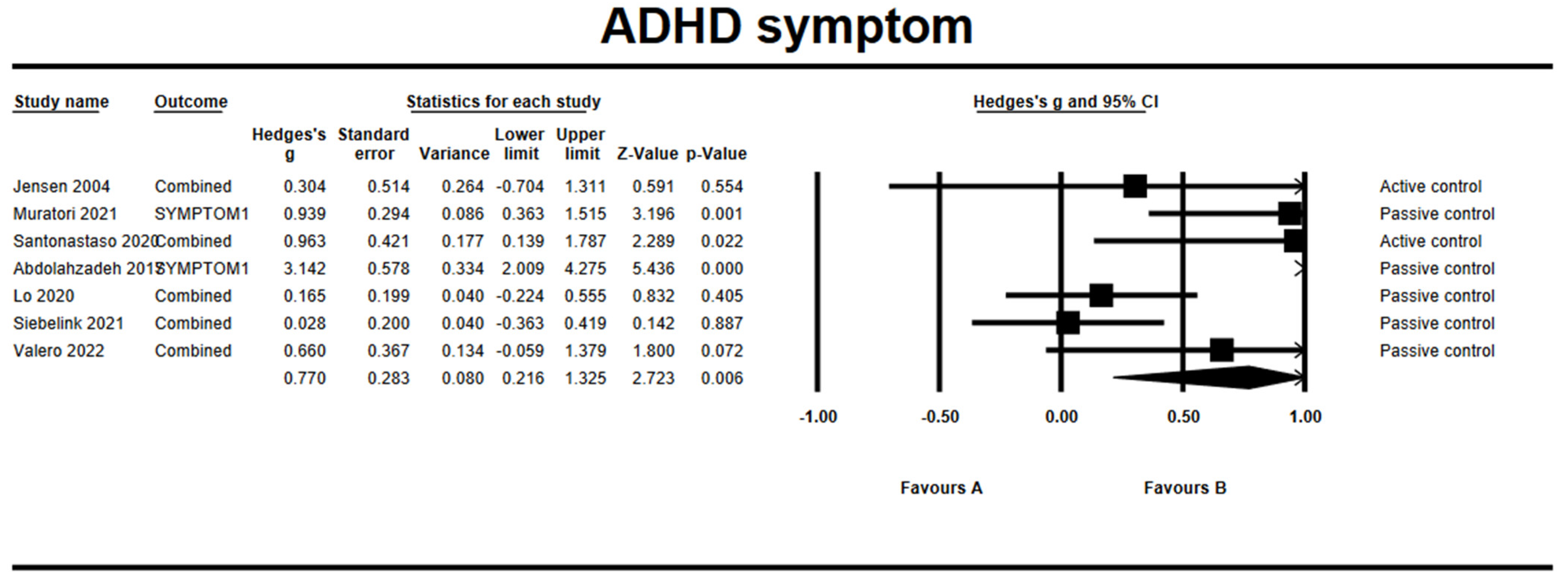
3.7. Effects on ADHD Symptoms
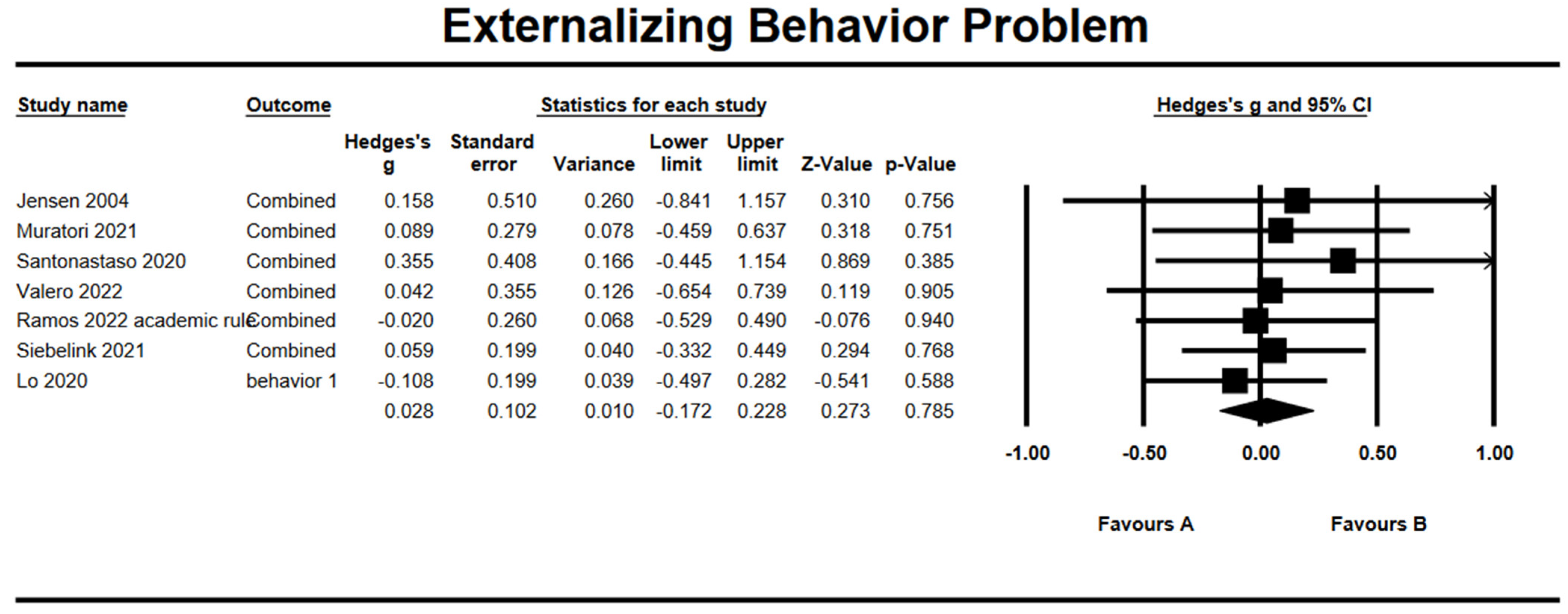
3.8. Effects on Externalizing Behavioral Problem
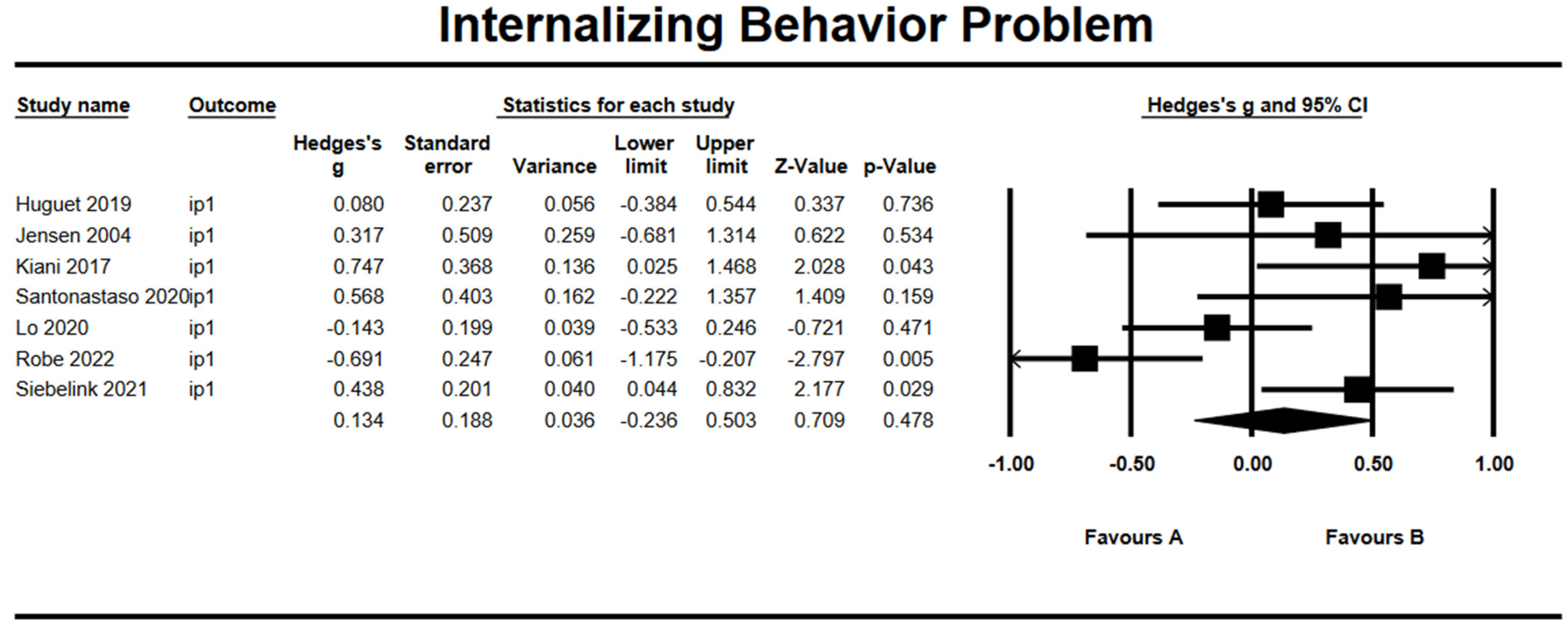
3.9. Effects on Internalizing Behavioral Problem
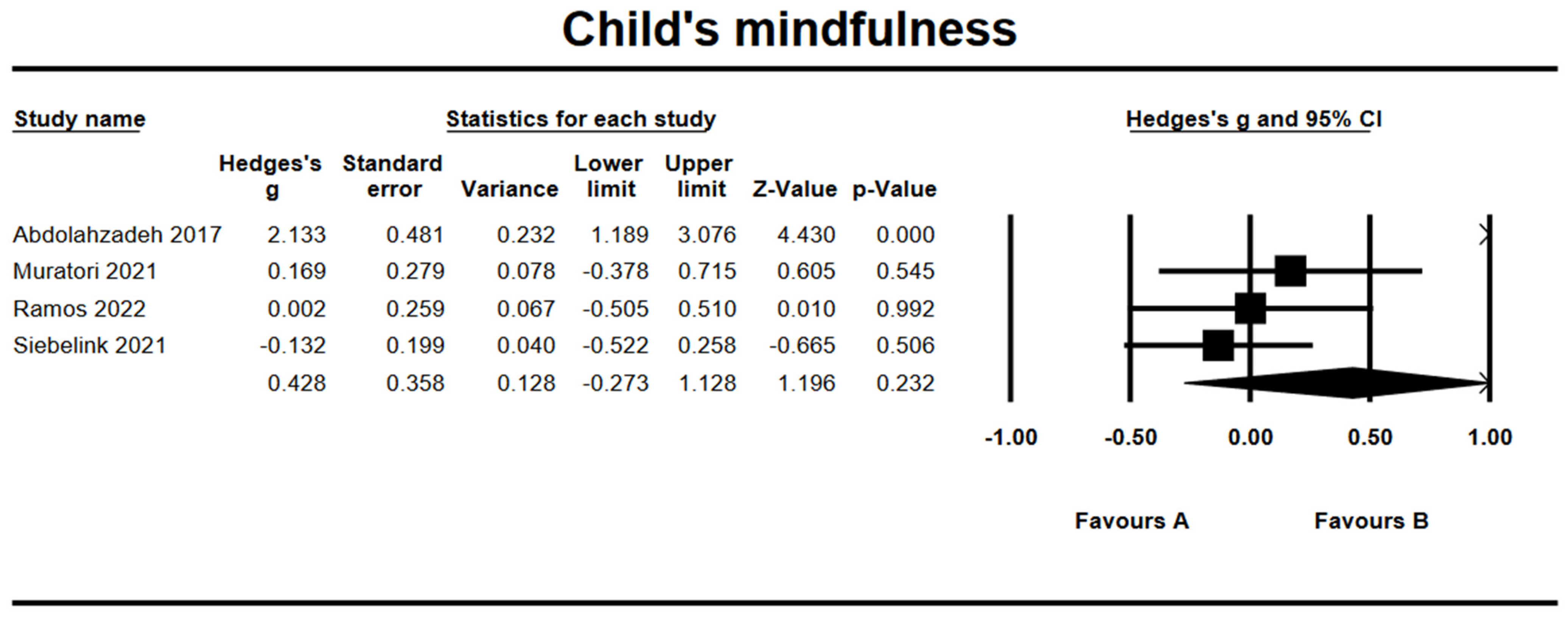
3.10. Effects on Child’s Mindfulness
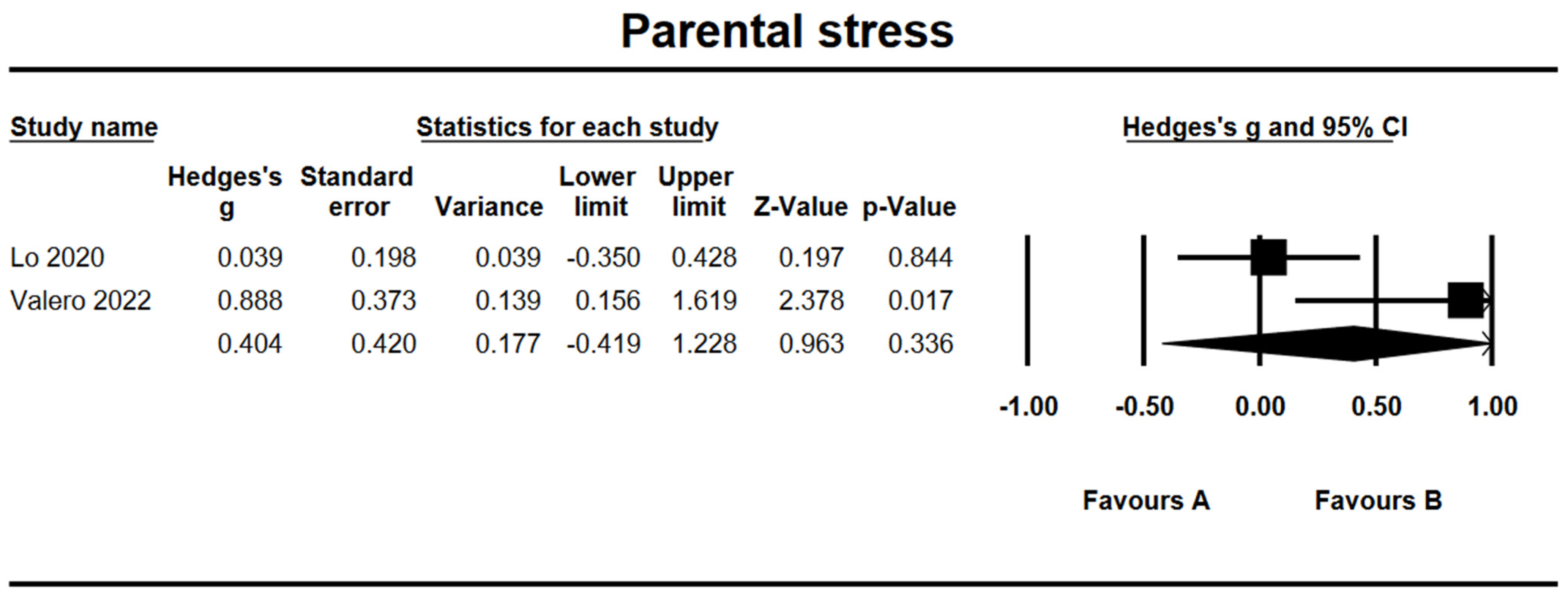
3.11. Effects on Parental Stress
3.12. Subgroup Analysis
3.13. Meta-Regression Analyses
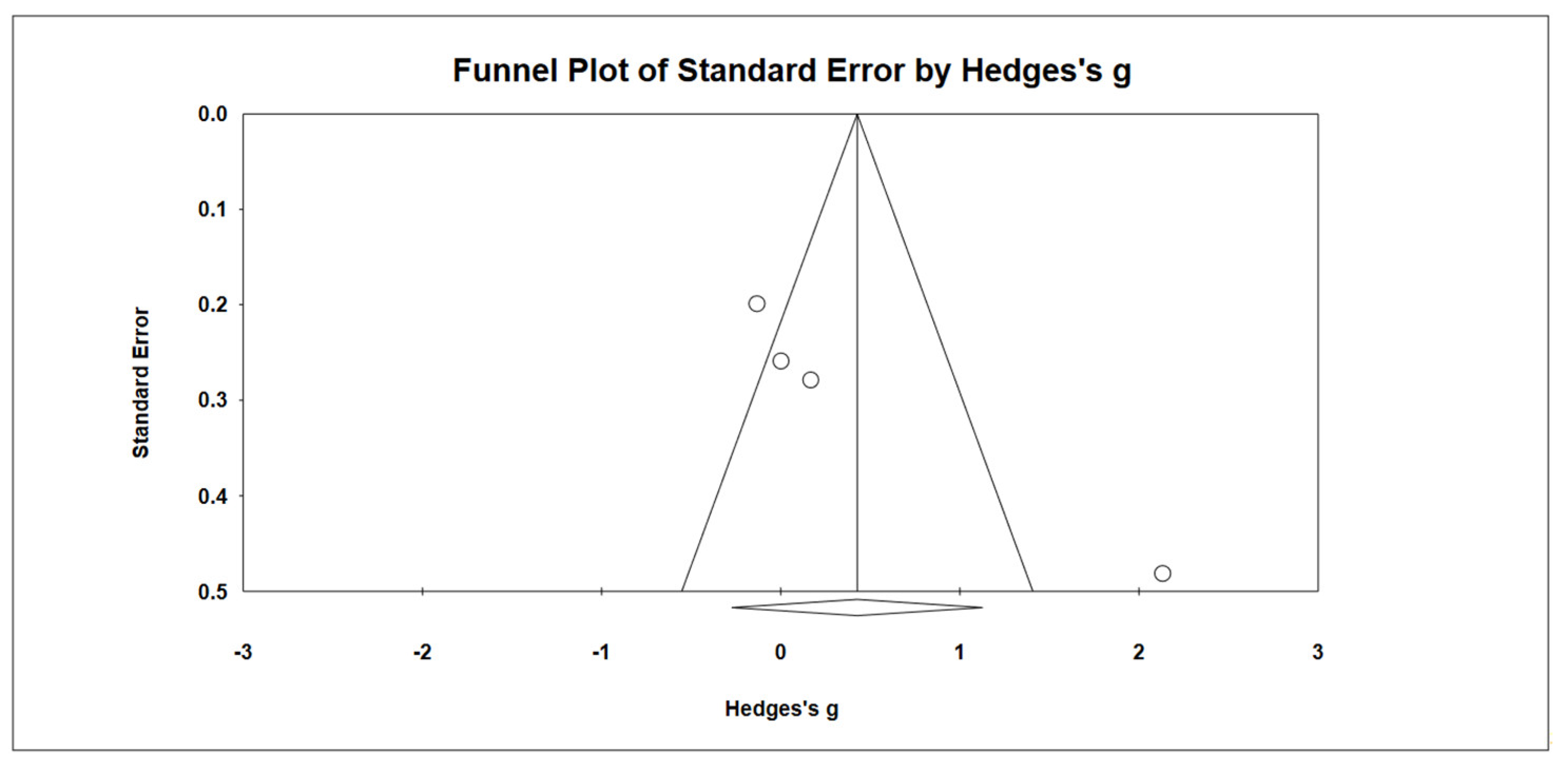
3.14. Sensitivity Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Polanczyk, G.; de Lima, M.S.; Horta, B.L.; Biederman, J.; Rohde, L.A. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am. J. Psychiatry 2007, 164, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.; Sanders, S.; Doust, J.; Beller, E.; Glasziou, P. Prevalence of Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-analysis. Pediatrics 2015, 135, e994–e1001. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Dupaul, G.J.; Morgan, P.L.; Farkas, G.; Hillemeier, M.M.; Maczuga, S. Eight-Year Latent Class Trajectories of Academic and Social Functioning in Children with Attention-Deficit/Hyperactivity Disorder. J. Abnorm. Child Psychol. 2018, 46, 979–992. [Google Scholar] [CrossRef] [PubMed]
- Swanson, J.M.; Arnold, L.E.; Molina, B.S.; Sibley, M.H.; Hechtman, L.T.; Hinshaw, S.P.; Abikoff, H.B.; Stehli, A.; Owens, E.B.; Mitchell, J.T.; et al. Young adult outcomes in the follow-up of the multimodal treatment study of attention-deficit/hyperactivity disorder: Symptom persistence, source discrepancy, and height suppression. J. Child Psychol. Psychiatry 2017, 58, 663–678. [Google Scholar] [CrossRef] [PubMed]
- Deault, L.C. A Systematic Review of Parenting in Relation to the Development of Comorbidities and Functional Impairments in Children with Attention-Deficit/Hyperactivity Disorder (ADHD). Child Psychiatry Hum. Dev. 2010, 41, 168–192. [Google Scholar] [CrossRef] [PubMed]
- Craig, F.; Operto, F.F.; De Giacomo, A.; Margari, L.; Frolli, A.; Conson, M.; Ivagnes, S.; Monaco, M.; Margari, F. Parenting stress among parents of children with Neurodevelopmental Disorders. Psychiatry Res. 2016, 242, 121–129. [Google Scholar] [CrossRef]
- Lee, P.-C.; Lin, K.-C.; Robson, D.; Yang, H.-J.; Chen, V.C.-H.; Niew, W.-I. Parent–child interaction of mothers with depression and their children with ADHD. Res. Dev. Disabil. 2013, 34, 656–668. [Google Scholar] [CrossRef]
- Modesto-Lowe, V.; Chaplin, M.; Godsay, V.; Soovajian, V. Parenting Teens with Attention-Deficit/Hyperactivity Disorder: Challenges and Opportunities. Clin. Pediatr. 2014, 53, 943–948. [Google Scholar] [CrossRef]
- Bhide, S.; Sciberras, E.; Anderson, V.; Hazell, P.; Nicholson, J.M. Association Between Parenting Style and Socio-Emotional and Academic Functioning in Children with and Without ADHD: A Community-Based Study. J. Atten. Disord. 2016, 23, 463–474. [Google Scholar] [CrossRef]
- Langberg, J.M.; Becker, S. Does Long-Term Medication Use Improve the Academic Outcomes of Youth with Attention-Deficit/Hyperactivity Disorder? Clin. Child Fam. Psychol. Rev. 2012, 15, 215–233. [Google Scholar] [CrossRef]
- Graham, J.; Coghill, D. Adverse Effects of Pharmacotherapies for Attention-Deficit Hyperactivity Disorder: Epidemiology, Prevention and Management. CNS Drugs 2008, 22, 213–237. [Google Scholar] [CrossRef]
- Lee, P.-C.; Niew, W.-I.; Yang, H.-J.; Chen, V.C.-H.; Lin, K.-C. A meta-analysis of behavioral parent training for children with attention deficit hyperactivity disorder. Res. Dev. Disabil. 2012, 33, 2040–2049. [Google Scholar] [CrossRef]
- McClintock, C.H.; Lau, E.; Miller, L. Phenotypic Dimensions of Spirituality: Implications for Mental Health in China, India, and the United States. Front. Psychol. 2016, 7, 1600. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Mindfulness-based interventions in context: Past, present, and future. Clin. Psychol. Sci. Pract. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Bishop, S.R.; Lau, M.; Shapiro, S.; Carlson, L.; Anderson, N.D.; Carmody, J.; Segal, Z.V.; Abbey, S.; Speca, M.; Velting, D.; et al. Mindfulness: A proposed operational definition. Clin. Psychol. Sci. Pract. 2004, 11, 230–241. [Google Scholar] [CrossRef]
- Schmalzl, L.; Crane-Godreau, M.A.; Payne, P. Movement-based embodied contemplative practices: Definitions and paradigms. Front. Hum. Neurosci. 2014, 8, 205. [Google Scholar] [CrossRef]
- Krisanaprakornkit, T.; Ngamjarus, C.; Witoonchart, C.; Piyavhatkul, N. Meditation therapies for attention-deficit/hyperactivity disorder (ADHD). Cochrane Database Syst. Rev. 2010, 2010, CD006507. [Google Scholar] [CrossRef]
- Bögels, S.M.; de Bruin, E.I.; van der Oord, S. Mindfulness-based interventions in child and adolescent psychopathology. In Cognitive Behaviour Therapy for Children and Families, 3rd ed.; Graham, P., Reynolds, S., Eds.; Cambridge University Press: Cambridge, UK, 2013; pp. 371–384. [Google Scholar]
- Smalley, S.L.; Loo, S.K.; Hale, T.S.; Shrestha, A.; McGough, J.; Flook, L.; Reise, S. Mindfulness and attention deficit hyperactivity disorder. J. Clin. Psychol. 2009, 65, 1087–1098. [Google Scholar] [CrossRef]
- Evans, S.; Ling, M.; Hill, B.; Rinehart, N.; Austin, D.; Sciberras, E. Systematic review of meditation-based interventions for children with ADHD. Eur. Child Adolesc. Psychiatry 2018, 27, 9–27. [Google Scholar] [CrossRef]
- Foley, N.C.; Teasell, R.W.; Bhogal, S.K.; Speechley, M.R. Stroke Rehabilitation Evidence-Based Review: Methodology. Top. Stroke Rehabil. 2003, 10, 1–7. [Google Scholar] [CrossRef]
- Borenstein, M.; Rothstein, H. Comprehensive Meta-Analysis: A Computer Program for Research Synthesis; Biostat: Englewood Cliffs, NJ, USA, 1999. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.C.L.; Harvey, D.J.; Shields, R.; Shields, G.; Rashedi, R.N.; Tancredi, D.; Angkustsiri, K.; Hansen, R.L.; Schweitzer, J.B. Effects of Yoga on Attention, Impulsivity, and Hyperactivity in Preschool-Aged Children with Attention-Deficit Hyperactivity Disorder Symptoms. J. Dev. Behav. Pediatr. 2018, 39, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Abdolahzadeh, Z.; Mashhadi, A.; Tabibi, Z. Effectiveness of mindfulness-based therapy on the rate of symptoms and mindfulness in adolescents with attention-deficit hyperactivity disorder. Q. J. Fundam. Mental Health 2017, 19, 30–37. [Google Scholar]
- Kiani, B.; Hadianfard, H.; Mitchell, J.T. The impact of mindfulness meditation training on executive functions and emotion dysregulation in an Iranian sample of female adolescents with elevated attention-deficit/hyperactivity disorder symptoms. Aust. J. Psychol. 2017, 69, 273–282. [Google Scholar] [CrossRef]
- Huguet, A.; Eguren, J.I.; Miguel-Ruiz, D.; Vallés, X.V.; Alda, J.A. Deficient Emotional Self-Regulation in Children with Attention Deficit Hyperactivity Disorder: Mindfulness as a Useful Treatment Modality. J. Dev. Behav. Pediatr. 2019, 40, 425–431. [Google Scholar] [CrossRef]
- Valero, M.; Cebolla, A.; Colomer, C. Mindfulness Training for Children with ADHD and Their Parents: A Randomized Control Trial. J. Atten. Disord. 2022, 26, 755–766. [Google Scholar] [CrossRef]
- Muratori, P.; Conversano, C.; Levantini, V.; Masi, G.; Milone, A.; Villani, S.; Bögels, S.; Gemignani, A. Exploring the efficacy of a mindfulness program for boys with attention-deficit hyperactivity disorder and oppositional defiant disorder. J. Atten. Disord. 2021, 25, 1544–1553. [Google Scholar] [CrossRef]
- Santonastaso, O.; Zaccari, V.; Crescentini, C.; Fabbro, F.; Capurso, V.; Vicari, S.; Menghini, D. Clinical Application of Mindfulness-Oriented Meditation: A Preliminary Study in Children with ADHD. Int. J. Environ. Res. Public Health 2020, 17, 6916. [Google Scholar] [CrossRef]
- Zaccari, V.; Santonastaso, O.; Mandolesi, L.; De Crescenzo, F.; Foti, F.; Crescentini, C.; Fabbro, F.; Vicari, S.; Curcio, G.; Menghini, D. Clinical application of mindfulness-oriented meditation in children with ADHD: A preliminary study on sleep and behavioral problems. Psychol. Health 2022, 37, 563–579. [Google Scholar] [CrossRef]
- Ramos, M.C.; Macphee, F.L.; Merrill, B.M.; Altszuler, A.R.; Raiker, J.S.; Gnagy, E.M.; Greiner, A.R.; Parent, J.; Coles, E.K.; Burger, L.; et al. Mindfulness as an Adjunct to Behavior Modification for Elementary-aged Children with ADHD. Res. Child Adolesc. Psychopathol. 2022, 50, 1573–1588. [Google Scholar] [CrossRef]
- Jensen, P.S.; Kenny, D.T. The effects of yoga on the attention and behavior of boys with Attention-Deficit/hyperactivity Disorder (ADHD). J. Atten. Disord. 2004, 7, 205–216. [Google Scholar] [CrossRef]
- Robe, A.; Dobrean, A. The effectiveness of a single session of mindfulness-based cognitive training on cardiac vagal control and core symptoms in children and adolescents with attention-deficit/hyperactivity disorder (ADHD): A preliminary randomized controlled trial. Eur. Child Adolesc. Psychiatry 2022, 1–10. [Google Scholar] [CrossRef]
- Lo, H.H.M.; Wong, S.W.L.; Wong, J.Y.H.; Yeung, J.W.K.; Snel, E.; Wong, S.Y.S. The Effects of Family-Based Mindfulness Intervention on ADHD Symptomology in Young Children and Their Parents: A Randomized Control Trial. J. Atten. Disord. 2020, 24, 667–680. [Google Scholar] [CrossRef]
- Siebelink, N.M.; Bögels, S.M.; Speckens, A.E.M.; Dammers, J.T.; Wolfers, T.; Buitelaar, J.K.; Greven, C.U. A randomised controlled trial (MindChamp) of a mindfulness-based intervention for children with ADHD and their parents. J. Child Psychol. Psychiatry 2022, 63, 165–177. [Google Scholar] [CrossRef]
- Vekety, B.; Logemann, H.N.A.; Takacs, Z.K. The effect of mindfulness-based interventions on inattentive and hyperactive–impulsive behavior in childhood: A meta-analysis. Int. J. Behav. Dev. 2021, 45, 133–145. [Google Scholar] [CrossRef]
- Lutz, A.; Slagter, H.; Rawlings, N.B.; Francis, A.D.; Greischar, L.L.; Davidson, R.; Lutz, A.; Slagter, H.; Rawlings, N.B.; Francis, A.D.; et al. Mental Training Enhances Attentional Stability: Neural and Behavioral Evidence. J. Neurosci. 2009, 29, 13418–13427. [Google Scholar] [CrossRef]
- Cairncross, M.; Miller, C.J. The Effectiveness of Mindfulness-Based Therapies for ADHD: A Meta-Analytic Review. J. Atten. Disord. 2020, 24, 627–643. [Google Scholar] [CrossRef]

| Experimental Group | Control Group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study (Year and Country of the Authors) | Age | ADHD Subtype (%) | Male (%) | N | Age, Mean (SD) or Range | Intervention | N | Age, Mean (SD) or Range, Years | Intervention | Follow- up | Outcome (ADHD Symptoms) | Informants | On ADHD Medication (%) |
| Abdolahzadeh et al. (2017, Iran) [28] | Adolescent | NR | 0 | 13 | Mean: 15.96 | MBI, 90 min/session, 8 sessions | 13 | Mean: 15.96 | Waitlist | No FU | SNAP-IV | Parent | NR |
| Cohen et al. (2018, USA) [27] | Children | NR | 65.22 | 10 | 4.33 (0.58) | Yoga 30 min/session, twice/week, 6 weeks | 11 | 3.83 (0.83) | Regular activities | 6 weeks, 3 months | ADHD RS-IV preschool version | Parent Teacher | 4.35 |
| Huguet et al. (2019, Spain) [30] | Child Parent | C: 64.29% I: 31.43% Hy: 4.29% | 72.86 | 34 | 8.79 (1.29) | MBI, 75 min/session, 8 sessions | 36 | 8.81 (1.65) | Standard care | No FU | CBCL | Parent | 0 |
| Jessen et al. (2004, Australia) [36] | Children | C: 78.58% I: 22.42% | NR | 11 | 10.63 (1.78) | Yoga, 60 min/session, 20 sessions | 8 | 9.35 (1.70) | Cooperative activities | No FU | CPRS, CTRS | Parent Teacher | 85.71 |
| Kiani et al. (2017, Iran) [29] | Adolescent | NR | 0 | 15 | 13.17 (.35) | Mindfulness mediation therapy (12 h/8 weeks) | 15 | 13.42 (.73) | Waitlist | None | NR | ||
| Muratori et al. (2021, Italy) [32] | Children Parent | NR | 100 | 25 | 8.75 (0.71) | MBI (90 min/session, 8 sessions) | 25 | 9.05 (1.05) | Waitlist | No FU | CBCL, SDQ | Parent | NR |
| Ramos et al. (2022, USA) [35] | Children | C: 75.9% I: 22.4% Hy: 1.7% | 93.2 | 29 | 9.2 (1.4) | MBI + BT 20 min/session, 3–4 sessions/week, 6-week summer camp | 29 | 9.2 (1.4) | BT | No FU | 63 | ||
| Robe-Dobrean et al. (2022, Romania) [37] | Children | NR | 62.9 | 35 | 11.66 (2.68) | MBI, 1 session | 35 | 10.40 (2.77) | A listening task | 4-week FU | ADHD-RS | Parent | 10 |
| Santonastaso et al. (2020, Italy) [33] Zaccari et al. (2022, Italy) [34] | Children | C: 85.71% I: 8.57% Hy: 5.71% | 74.29 | 15 | 8.9 (1.3) | Mindful-oriented meditation, 3 times/week, 8 weeks | 10 | 9 (1.2) | Emotional education program, 3 times/week, 8 weeks | 2-month FU | CPRS-R:L CBCL | Parent | NR |
| Lo et al. (2020, HongKong) [38] | Child Parent | NR | 83 | 50 | 6.24 (.87) | FBMI (Parent 9 h/6 weeks) (Child 8 h) | 50 | 5.92 (.70) | Waitlist | None | SWAN | Observer | NR |
| Siebelink et al. (2021, Netherlands) [39] | Child Parent | NR | 69.9 | 55 | 11.0 (1.8) | FMBI (12 h/8 weeks) | 48 | 11.4 (1.8) | Treatment as usual | 2-month FU | CPRS, SWAN | Observer | 81 |
| Valero et al. (2022, Spain) [31] | Child Parent | C: 56.7 I: 30 Hy: 13.33 | 76.7 | 15 | 10.33 (1.83) | FMBI (Parent 12 h/8 weeks) (Child 8 h/8 weeks) | 15 | 11.6 (1.29) | Waitlist | 6 mo | Conners—3rd Edition | Observer | 56.67 |
| Study | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Abdolahzadeh et al. (2017) [28] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Cohen et al. (2018) [27] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Huguet et al. (2019) [30] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Jensen et al. (2004) [36] | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Kiani et al. (2017) [29] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Lo et al. (2020) [38] | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Muratori et al. (2021) [32] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Ramos et al. (2022) [35] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Robe-Dobrean et al. (2022) [37] | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Santonastaso et al. (2020) [33] Zaccari et al. (2022) [34] | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Siebelink et al. (2021) [39] | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Valero et al. (2022) [31] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Time | ADHD Symptoms | Externalizing Problem | Internalizing Problem | Mindfulness | Parenting Stress | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| k | Hedge’s g | k | Hedge’s g | k | Hedge’s g | k | Hedge’s g | k | Hedge’s g | |
| Post-treatment | 7 | 0.77 | 7 | 0.03 | 7 | 0.13 | 4 | 0.43 | 2 | 0.40 |
| Follow-up | 2 | 0.34 | 2 | 0.18 | 2 | −0.27 | 1 | −0.17 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-C.; Chen, C.-R.; Lin, K.-C. Effects of Mindfulness-Based Interventions in Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2022, 19, 15198. https://doi.org/10.3390/ijerph192215198
Lee Y-C, Chen C-R, Lin K-C. Effects of Mindfulness-Based Interventions in Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health. 2022; 19(22):15198. https://doi.org/10.3390/ijerph192215198
Chicago/Turabian StyleLee, Yi-Chen, Chyi-Rong Chen, and Keh-Chung Lin. 2022. "Effects of Mindfulness-Based Interventions in Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" International Journal of Environmental Research and Public Health 19, no. 22: 15198. https://doi.org/10.3390/ijerph192215198
APA StyleLee, Y.-C., Chen, C.-R., & Lin, K.-C. (2022). Effects of Mindfulness-Based Interventions in Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health, 19(22), 15198. https://doi.org/10.3390/ijerph192215198