Environmental Factors in the Rehabilitation Framework: Role of the One Health Approach to Improve the Complex Management of Disability
Abstract
:1. Introduction
2. Research Methodology
3. Environmental Diseases
4. Functional Impairment and Environment
4.1. Does the Environment Affect the Risk of Disability?
4.2. Environment and Healthy Aging, Frailty and Disability
4.3. Sanitary Costs, Opportunities, and Barriers to Independence
5. One Health Approach
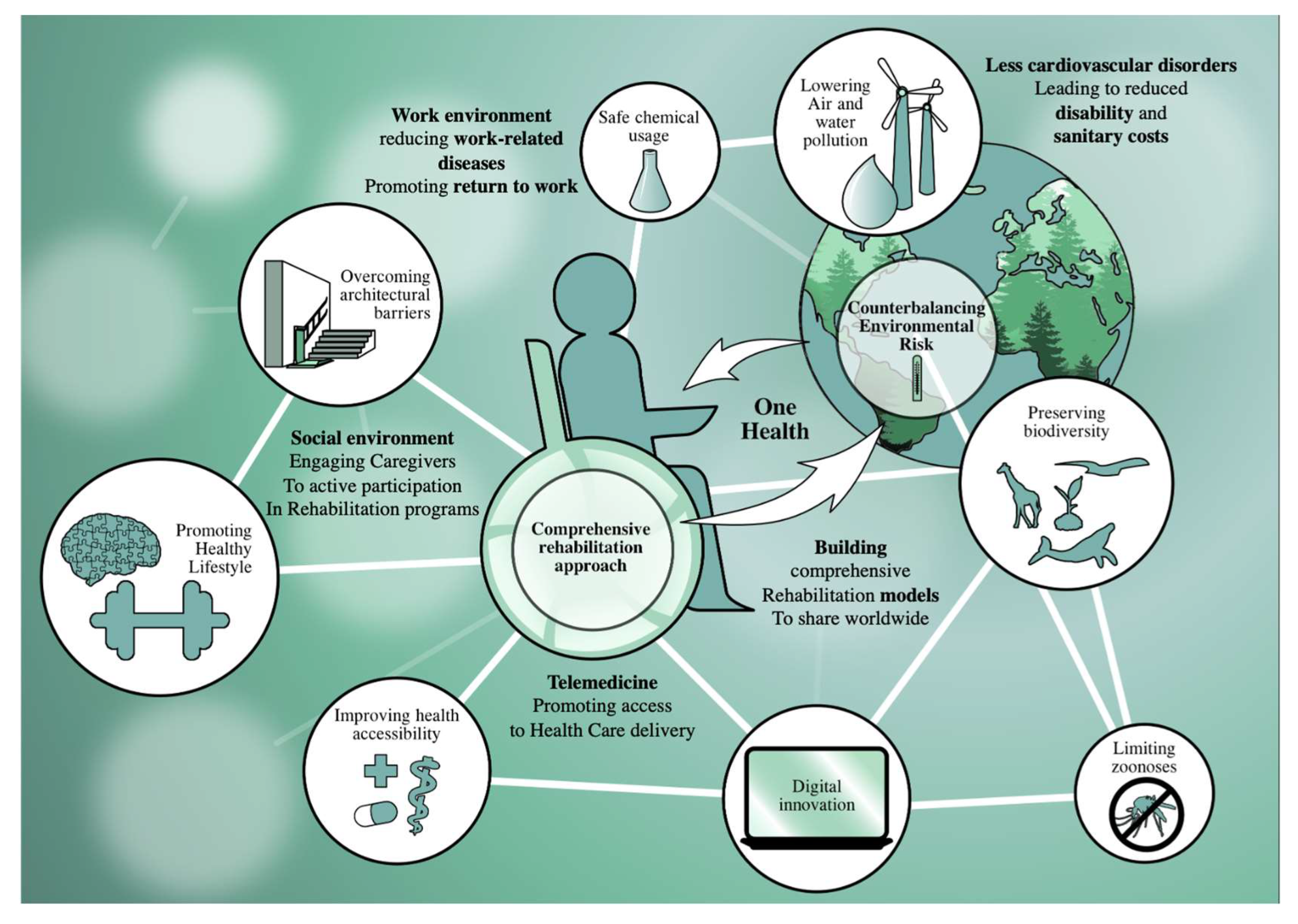
6. One Health Approach and Disability
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Prüss-Ustün, A.; Wolf, J.; Corvalán, C.; Bos, R.; Neira, M. Preventing Disease through Healthy Environments: A Global Assessment of the Burden of Disease from Environmental Risks; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Frank, D.M. What is the environment in environmental health research? Perspectives from the ethics of science. Stud. Hist. Philos. Sci. 2021, 88, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Okoro, C.A.; Hollis, N.D.; Cyrus, A.C.; Griffin-Blake, S. Prevalence of disabilities and health care access by disability status and type among adults—United States, 2016. Morb. Mortal. Wkly. Rep. 2018, 67, 882–887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC. One Health. Available online: https://www.cdc.gov/onehealth/index.html (accessed on 24 August 2022).
- Frier, A.; Barnett, F.; Devine, S.; Barker, R. Understanding disability and the ‘social determinants of health’: How does disability affect peoples’ social determinants of health? Disabil. Rehabil. 2018, 40, 538–547. [Google Scholar] [CrossRef]
- Physical, E.; Alliance, R.M.B. White book on physical and rehabilitation medicine (PRM) in Europe. Chapter 1. Definitions and concepts of PRM. Eur. J. Phys. Rehabil. Med. 2018, 54, 156–165. [Google Scholar]
- Clarke, P.; George, L.K. The role of the built environment in the disablement process. Am. J. Public Health 2005, 95, 1933–1939. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [Green Version]
- Cooke, A.; Smith, D.; Booth, A. Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qual. Health Res. 2012, 22, 1435–1443. [Google Scholar] [CrossRef]
- WHO. Compendium of WHO and Other UN Guidance on Health and Environment; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Rappaport, S.M. Discovering environmental causes of disease. J. Epidemiol. Community Health 2012, 66, 99–102. [Google Scholar] [CrossRef]
- Rojas-Rueda, D.; Morales-Zamora, E.; Alsufyani, W.A.; Herbst, C.H.; AlBalawi, S.M.; Alsukait, R.; Alomran, M. Environmental risk factors and health: An umbrella review of meta-analyses. Int. J. Environ. Res. Public Health 2021, 18, 704. [Google Scholar] [CrossRef]
- Milstein, B.; Homer, J.; Briss, P.; Burton, D.; Pechacek, T. Why behavioral and environmental interventions are needed to improve health at lower cost. Health Aff. 2011, 30, 823–832. [Google Scholar] [CrossRef] [PubMed]
- Walker, B., Jr. Pediatric environmental health. J. Natl. Med. Assoc. 2005, 97, 262–269. [Google Scholar] [PubMed]
- Mena, C.; Ormazabal, Y.; Fuentes, E.; Palomo, I. Impacts of physical environment perception on the frailty condition in older people. Geospat. Health 2020, 15. [Google Scholar] [CrossRef] [PubMed]
- Stokols, D. Establishing and maintaining healthy environments: Toward a social ecology of health promotion. Am. Psychol. 1992, 47, 6–22. [Google Scholar] [CrossRef]
- WHO. Environmental Health. Available online: https://www.who.int/health-topics/environmental-health (accessed on 25 August 2022).
- Gao, P.; Shen, X.; Zhang, X.; Jiang, C.; Zhang, S.; Zhou, X.; Schüssler-Fiorenza Rose, S.M.; Snyder, M. Precision environmental health monitoring by longitudinal exposome and multi-omics profiling. Genome Res. 2022, 32, 1199–1214. [Google Scholar] [CrossRef]
- García-Esquinas, E.; Rodríguez-Artalejo, F. Environmental pollutants, limitations in physical functioning, and frailty in older adults. Curr. Environ. Health Rep. 2017, 4, 12–20. [Google Scholar] [CrossRef]
- Pérez-Hernández, B.; Lopez-García, E.; Graciani, A.; Ayuso-Mateos, J.L.; Rodríguez-Artalejo, F.; García-Esquinas, E. Housing conditions and risk of physical function limitations: A prospective study of community-dwelling older adults. J. Public Health 2018, 40, e252–e259. [Google Scholar] [CrossRef] [Green Version]
- Tough, H.; Siegrist, J.; Fekete, C. Social relationships, mental health and wellbeing in physical disability: A systematic review. BMC Public Health 2017, 17, 414. [Google Scholar] [CrossRef] [Green Version]
- Choi, J.; Yang, K.; Chu, S.H.; Youm, Y.; Kim, H.C.; Park, Y.R.; Son, Y.J. Social activities and health-related quality of life in rural older adults in South Korea: A 4-year longitudinal analysis. Int. J. Environ. Res. Public Health 2020, 17, 5553. [Google Scholar] [CrossRef]
- Fuller, R.; Landrigan, P.J.; Balakrishnan, K.; Bathan, G.; Bose-O’Reilly, S.; Brauer, M.; Caravanos, J.; Chiles, T.; Cohen, A.; Corra, L.; et al. Pollution and health: A progress update. Lancet Planet. Health 2022, 6, e535–e547. [Google Scholar] [CrossRef]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and health impacts of air pollution: A review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Rider, C.F.; Carlsten, C. Air pollution and DNA methylation: Effects of exposure in humans. Clin. Epigenetics 2019, 11, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, Y.; Lu, H.; Man, Q.; Liu, Z.; Wang, L.; Wang, Y.; Suo, C.; Zhang, T.; Jin, L.; Dong, Q.; et al. Stroke burden and mortality attributable to ambient fine particulate matter pollution in 195 countries and territories and trend analysis from 1990 to 2017. Environ. Res. 2020, 184, 109327. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, A.; Ralli, M.; Gilardi, A.; Salvi, R. Occupational noise: Auditory and non-auditory consequences. Int. J. Environ. Res. Public Health 2020, 17, 8963. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Marotta, N.; Ferrillo, M.; Agostini, F.; Sconza, C.; Lippi, L.; Respizzi, S.; Giudice, A.; Invernizzi, M.; Ammendolia, A. Oxygen-Ozone Therapy for Reducing Pro-Inflammatory Cytokines Serum Levels in Musculoskeletal and Temporomandibular Disorders: A Comprehensive Review. Int. J. Mol. Sci. 2022, 23, 2528. [Google Scholar] [CrossRef]
- Blanc, P.D.; Eisner, M.D.; Trupin, L.; Yelin, E.H.; Katz, P.P.; Balmes, J.R. The association between occupational factors and adverse health outcomes in chronic obstructive pulmonary disease. Occup. Environ. Med. 2004, 61, 661–667. [Google Scholar] [CrossRef] [Green Version]
- Torén, K.; Zock, J.P.; Kogevinas, M.; Plana, E.; Sunyer, J.; Radon, K.; Jarvis, D.; Kromhout, H.; d’Errico, A.; Payo, F.; et al. An international prospective general population-based study of respiratory work disability. Thorax 2009, 64, 339–344. [Google Scholar] [CrossRef] [Green Version]
- Bruno, R.M.; Di Pilla, M.; Ancona, C.; Sørensen, M.; Gesi, M.; Taddei, S.; Munzel, T.; Virdis, A. Environmental factors and hypertension. Curr. Pharm. Des. 2017, 23, 3239–3246. [Google Scholar] [CrossRef]
- Miranda, L.C.; Parente, M.; Silva, C.; Clemente-Coelho, P.; Santos, H.; Cortes, S.; Medeiros, D.; Ribeiro, J.S.; Barcelos, F.; Sousa, M.; et al. Perceived pain and weather changes in rheumatic patients. Acta Reumatol. Port. 2007, 32, 351–361. [Google Scholar]
- Carlsen, H.K.; Oudin, A.; Steingrimsson, S.; Oudin Åström, D. Ambient temperature and associations with daily visits to a psychiatric emergency unit in Sweden. Int. J. Environ. Res. Public Health 2019, 16, 286. [Google Scholar] [CrossRef] [Green Version]
- Cheng, J.; Xu, Z.; Bambrick, H.; Su, H.; Tong, S.; Hu, W. The mortality burden of hourly temperature variability in five capital cities, Australia: Time-series and meta-regression analysis. Environ. Int. 2017, 109, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Boyce, M.R.; Katz, R.; Standley, C.J. Risk factors for infectious diseases in urban environments of sub-Saharan Africa: A systematic review and critical appraisal of evidence. Trop. Med. Infect. Dis. 2019, 4, 123. [Google Scholar] [CrossRef]
- Carpio, D.; Barreiro-de Acosta, M.; Echarri, A.; Pereira, S.; Castro, J.; Ferreiro, R.; Lorenzo, A. Influence of urban/rural and coastal/inland environment on the prevalence, phenotype, and clinical course of inflammatory bowel disease patients from northwest of Spain: A cross-sectional study. Eur. J. Gastroenterol. Hepatol. 2015, 27, 1030–1037. [Google Scholar] [CrossRef] [PubMed]
- Siddharthan, T.; Grigsby, M.; Morgan, B.; Kalyesubula, R.; Wise, R.A.; Kirenga, B.; Checkley, W. Prevalence of chronic respiratory disease in urban and rural Uganda. Bull. World Health Organ. 2019, 97, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Paciência, I.; Moreira, A. Human health: Is it who you are or where you live? Lancet Planet. Health 2017, 1, e263–e264. [Google Scholar] [CrossRef]
- Persson, Å.; Pyko, A.; Lind, T.; Bellander, T.; Östenson, C.G.; Pershagen, G.; Eriksson, C.; Lõhmus, M. Urban residential greenness and adiposity: A cohort study in Stockholm County. Environ. Int. 2018, 121, 832–841. [Google Scholar] [CrossRef]
- Vallée, J.; Cadot, E.; Roustit, C.; Parizot, I.; Chauvin, P. The role of daily mobility in mental health inequalities: The interactive influence of activity space and neighbourhood of residence on depression. Soc. Sci. Med. 2011, 73, 1133–1144. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Wang, Y.; Feng, L.; Hou, C.; Gu, Q. Effects of air pollution and green spaces on impaired lung function in children: A case-control study. Environ. Sci. Pollut. Res. Int. 2022, 29, 11907–11919. [Google Scholar] [CrossRef]
- Dinsa, G.D.; Goryakin, Y.; Fumagalli, E.; Suhrcke, M. Obesity and socioeconomic status in developing countries: A systematic review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2012, 13, 1067–1079. [Google Scholar] [CrossRef] [Green Version]
- Feng, X.; Wilson, A. Neighbourhood socioeconomic inequality and gender differences in body mass index: The role of unhealthy behaviours. Prev. Med. 2017, 101, 171–177. [Google Scholar] [CrossRef]
- Karriker-Jaffe, K.J.; Chartier, K.G.; Bares, C.B.; Kendler, K.S.; Greenfield, T.K. Intersection of familial risk and environmental social control on high-risk drinking and alcohol dependence in a US national sample of adults. Addict. Behav. 2021, 113, 106668. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C.A.; Hahn, R.A.; Elder, R.; Brewer, R.; Chattopadhyay, S.; Fielding, J.; Naimi, T.S.; Toomey, T.; Lawrence, B.; Middleton, J.C.; et al. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am. J. Prev. Med. 2009, 37, 556–569. [Google Scholar] [CrossRef] [PubMed]
- Lippi, L.; D’Abrosca, F.; Folli, A.; Dal Molin, A.; Moalli, S.; Maconi, A.; Ammendolia, A.; de Sire, A.; Invernizzi, M. Closing the gap between inpatient and outpatient settings: Integrating pulmonary rehabilitation and technological advances in the comprehensive management of frail patients. Int. J. Environ. Res. Public Health 2022, 19, 9150. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) approach to healthy ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Manzi, F.; Del Riccio, M.; Setola, N.; Naldi, E.; Milani, C.; Giorgetti, D.; Dellisanti, C.; Lorini, C. Impact of the built environment and the neighborhood in promoting the physical activity and the healthy aging in older people: An Umbrella review. Int. J. Environ. Res. Public Health 2020, 17, 6127. [Google Scholar] [CrossRef] [PubMed]
- Di Ciaula, A.; Portincasa, P. The environment as a determinant of successful aging or frailty. Mech. Ageing Dev. 2020, 188, 111244. [Google Scholar] [CrossRef] [PubMed]
- Bektas, A.; Schurman, S.H.; Sen, R.; Ferrucci, L. Aging, inflammation and the environment. Exp. Gerontol. 2018, 105, 10–18. [Google Scholar] [CrossRef]
- Yu, R.; Wang, D.; Leung, J.; Lau, K.; Kwok, T.; Woo, J. Is neighborhood green space associated with less frailty? Evidence from the Mr. and Ms. Os (Hong Kong) study. J. Am. Med. Dir. Assoc. 2018, 19, 528–534. [Google Scholar] [CrossRef]
- Lee, W.J.; Liu, C.Y.; Peng, L.N.; Lin, C.H.; Lin, H.P.; Chen, L.K. PM(2.5) air pollution contributes to the burden of frailty. Sci. Rep. 2020, 10, 14478. [Google Scholar] [CrossRef]
- Tsubota-Utsugi, M.; Yonekura, Y.; Tanno, K.; Nozue, M.; Shimoda, H.; Nishi, N.; Sakata, K.; Kobayashi, S. Association between health risks and frailty in relation to the degree of housing damage among elderly survivors of the great East Japan earthquake. BMC Geriatr. 2018, 18, 133. [Google Scholar] [CrossRef]
- Momosaki, R.; Wakabayashi, H.; Maeda, K.; Shamoto, H.; Nishioka, S.; Kojima, K.; Tani, Y.; Suzuki, N.; Hanazato, M.; Kondo, K. Association between food store availability and the incidence of functional disability among community-dwelling older adults: Results from the Japanese gerontological evaluation cohort study. Nutrients 2019, 11, 2369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.H.; Wu, C.D.; Lee, Y.L.; Lee, K.Y.; Lin, W.Y.; Yeh, J.I.; Chen, H.C.; Guo, Y.L. Air pollution enhance the progression of restrictive lung function impairment and diffusion capacity reduction: An elderly cohort study. Respir. Res. 2022, 23, 186. [Google Scholar] [CrossRef] [PubMed]
- Cassou, B.; Derriennic, F.; Iwatsubo, Y.; Amphoux, M. Physical diability after retirement and occupational risk factors during working life: A cross sectional epidemiological study in the Paris area. J. Epidemiol. Community Health 1992, 46, 506–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindemann, U.; Oksa, J.; Skelton, D.A.; Beyer, N.; Klenk, J.; Zscheile, J.; Becker, C. Effect of cold indoor environment on physical performance of older women living in the community. Age Ageing 2014, 43, 571–575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zanobetti, A.; Coull, B.A.; Kloog, I.; Sparrow, D.; Vokonas, P.S.; Gold, D.R.; Schwartz, J. Fine-scale spatial and temporal variation in temperature and arrhythmia episodes in the VA Normative Aging Study. J. Air Waste Manag. Assoc. 2017, 67, 96–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dardiotis, E.; Siokas, V.; Moza, S.; Kosmidis, M.H.; Vogiatzi, C.; Aloizou, A.M.; Geronikola, N.; Ntanasi, E.; Zalonis, I.; Yannakoulia, M.; et al. Pesticide exposure and cognitive function: Results from the Hellenic Longitudinal Investigation of Aging and Diet (HELIAD). Environ. Res. 2019, 177, 108632. [Google Scholar] [CrossRef] [PubMed]
- Weuve, J.; D’Souza, J.; Beck, T.; Evans, D.A.; Kaufman, J.D.; Rajan, K.B.; de Leon, C.F.M.; Adar, S.D. Long-term community noise exposure in relation to dementia, cognition, and cognitive decline in older adults. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2021, 17, 525–533. [Google Scholar] [CrossRef]
- Gao, Q.; Zang, E.; Bi, J.; Dubrow, R.; Lowe, S.R.; Chen, H.; Zeng, Y.; Shi, L.; Chen, K. Long-term ozone exposure and cognitive impairment among Chinese older adults: A cohort study. Environ. Int. 2022, 160, 107072. [Google Scholar] [CrossRef]
- Lauriola, P.; Crabbe, H.; Behbod, B.; Yip, F.; Medina, S.; Semenza, J.C.; Vardoulakis, S.; Kass, D.; Zeka, A.; Khonelidze, I.; et al. Advancing global health through environmental and public health tracking. Int. J. Environ. Res. Public Health 2020, 17, 1976. [Google Scholar] [CrossRef] [Green Version]
- Lightwood, J.M.; Coxson, P.G.; Bibbins-Domingo, K.; Williams, L.W.; Goldman, L. Coronary heart disease attributable to passive smoking: CHD Policy Model. Am. J. Prev. Med. 2009, 36, 13–20. [Google Scholar] [CrossRef] [Green Version]
- Reitsma, M.B.; Kendrick, P.J.; Ababneh, E.; Abbafati, C.; Abbasi-Kangevari, M.; Abdoli, A.; Abedi, A.; Abhilash, E.S.; Abila, D.B.; Aboyans, V.; et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet 2021, 397, 2337–2360. [Google Scholar] [CrossRef]
- Gielen, A.C.; Green, L.W. The impact of policy, environmental, and educational interventions: A synthesis of the evidence from two public health success stories. Health Educ. Behav. 2015, 42, 20s–34s. [Google Scholar] [CrossRef] [PubMed]
- Virapongse, A.; Brooks, S.; Metcalf, E.C.; Zedalis, M.; Gosz, J.; Kliskey, A.; Alessa, L. A social-ecological systems approach for environmental management. J. Environ. Manag. 2016, 178, 83–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aslam, B.; Khurshid, M.; Arshad, M.I.; Muzammil, S.; Rasool, M.; Yasmeen, N.; Shah, T.; Chaudhry, T.H.; Rasool, M.H.; Shahid, A.; et al. Antibiotic resistance: One health one world outlook. Front. Cell. Infect. Microbiol. 2021, 11, 771510. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, J.R. Importance of a One Health approach in advancing global health security and the Sustainable Development Goals. Rev. Sci. Tech. 2019, 38, 145–154. [Google Scholar] [CrossRef]
- Sterckx, A.; Van den Broeck, K.; Remmen, R.; Dekeirel, K.; Hermans, H.; Hesters, C.; Daeseleire, T.; Broes, V.; Barton, J.; Gladwell, V.; et al. Operationalization of one health burnout prevention and recovery: Participatory action research-design of nature-based health promotion interventions for employees. Front. Public Health 2021, 9, 720761. [Google Scholar] [CrossRef]
- Capps, B.; Lederman, Z. One Health and paradigms of public biobanking. J. Med. Ethics 2015, 41, 258–262. [Google Scholar] [CrossRef]
- Worboys, M.; Timmermann, C.; Toon, E. Before translational medicine: Laboratory-clinic relations. Hist. Philos. Life Sci. 2021, 43, 48. [Google Scholar] [CrossRef]
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef]
- Leland, N.E.; Lepore, M.; Wong, C.; Chang, S.H.; Freeman, L.; Crum, K.; Gillies, H.; Nash, P. Delivering high quality hip fracture rehabilitation: The perspective of occupational and physical therapy practitioners. Disabil. Rehabil. 2018, 40, 646–654. [Google Scholar] [CrossRef]
- Bernhardt, J.; Urimubenshi, G.; Gandhi, D.B.C.; Eng, J.J. Stroke rehabilitation in low-income and middle-income countries: A call to action. Lancet 2020, 396, 1452–1462. [Google Scholar] [CrossRef]
- Wallander, J.L.; Varni, J.W.; Babani, L.; DeHaan, C.B.; Wilcox, K.T.; Banis, H.T. The social environment and the adaptation of mothers of physically handicapped children. J. Pediatr. Psychol. 1989, 14, 371–387. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Invernizzi, M.; Baricich, A.; Lippi, L.; Ammendolia, A.; Grassi, F.A.; Leigheb, M. Optimization of transdisciplinary management of elderly with femur proximal extremity fracture: A patient-tailored plan from orthopaedics to rehabilitation. World J. Orthop. 2021, 12, 456–466. [Google Scholar] [CrossRef] [PubMed]
- Göktalay, T.; Tuncal, A.N.; Sarı, S.; Köroğlu, G.; Havlucu, Y.; Yorgancıoğlu, A. Knowledge level of the primary healthcare providers on chronic obstructive pulmonary disease and pulmonary rehabilitation. Pulm. Med. 2015, 2015, 538246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogner, J.; Hade, E.M.; Peng, J.; Beaulieu, C.L.; Horn, S.D.; Corrigan, J.D.; Hammond, F.M.; Dijkers, M.P.; Montgomery, E.; Gilchrist, K.; et al. Family involvement in traumatic brain injury inpatient rehabilitation: A propensity score analysis of effects on outcomes during the first year after discharge. Arch. Phys. Med. Rehabil. 2019, 100, 1801–1809. [Google Scholar] [CrossRef] [PubMed]
- Doraiswamy, S.; Abraham, A.; Mamtani, R.; Cheema, S. Use of telehealth during the COVID-19 pandemic: Scoping review. J. Med. Internet Res. 2020, 22, e24087. [Google Scholar] [CrossRef] [PubMed]
- Grundstein, M.J.; Fisher, C.; Titmuss, M.; Cioppa-Mosca, J. The role of virtual physical therapy in a post-pandemic world: Pearls, pitfalls, challenges, and adaptations. Phys. Ther. 2021, 101, pzab145. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Marotta, N.; Agostini, F.; Drago Ferrante, V.; Demeco, A.; Ferrillo, M.; Inzitari, M.T.; Pellegrino, R.; Russo, I.; Ozyemisci Taskiran, O.; et al. A telerehabilitation approach to chronic facial paralysis in the COVID-19 pandemic scenario: What role for electromyography assessment? J. Pers. Med. 2022, 12, 497. [Google Scholar] [CrossRef]
- Paolucci, T.; de Sire, A.; Ferrillo, M.; di Fabio, D.; Molluso, A.; Patruno, A.; Pesce, M.; Lai, C.; Ciacchella, C.; Saggino, A.; et al. Telerehabilitation proposal of mind-body technique for physical and psychological outcomes in patients with fibromyalgia. Front. Physiol. 2022, 13, 917956. [Google Scholar] [CrossRef]
- Vornholt, K.; Villotti, P.; Muschalla, B.; Bauer, J.; Colella, A.; Zijlstra, F.; Van Ruitenbeek, G.; Uitdewilligen, S.; Corbière, M. Disability and employment–overview and highlights. Eur. J. Work Organ. Psychol. 2018, 27, 40–55. [Google Scholar] [CrossRef]
- WHO. Rehabilitation 2030 Initiative. Available online: https://www.who.int/initiatives/rehabilitation-2030 (accessed on 2 September 2022).
| S | PI | D | E | R |
|---|---|---|---|---|
| Sample | Phenomenon of Interest | Design | Evaluation | Research Type |
| Human subjects | Environment | Any | Disability | Qualitative |
| “Environmental risk factors” “Environment” “Environmental Medicine” | “Disability” “Function” “Impairment” “Rehabilitation” |
| Environmental Factors | Effects on Human Health and Disability |
|---|---|
| Environmental pollution | Environmental pollution represents one of the most studied environmental factors leading to environmental diseases, with approximately 9 million premature deaths every year and might be related to environmental pollution [24]. In this scenario, fine particulate matter < 2.5 µm (particulate matter—PM2.5) air pollution is one of the most important environmental risk factors leading to cardiovascular disorders commonly correlated with significant functional impairment, disability, high sanitary and assistance costs and even mortality [25,26,27]. |
| Noise pollution | Chronic noise pollution plays an important role in the disability development process, with significant implications in the work setting. Beyond the widely documented effects of reduction in hearing sensitivity [28], noise pollution might be related also to stress, cardiovascular disease and cognitive impairment risk [28]. |
| Occupational risks | Limitation of exposure to occupational risk factors and effective protection strategies have a crucial role in reducing the incidence of occupational diseases with relevant implications in terms of disability. More in detail, work-related musculoskeletal disorders are highly prevalent conditions related to work overuse affecting muscles, nerves, tendons, joints, cartilage, and spinal discs [29]. In this scenario, the functional limitation and pain symptoms might be effectively targeted by a comprehensive rehabilitation plan, which might include environmental and ergonomic modifications. On the other hand, vapors, gas, dust, or fumes might promote the development of pathological respiratory conditions (emphysema, chronic bronchitis, chronic obstructive pulmonary disease, silicosis, mesothelioma, lung cancer) leading to an increased incidence of functional impairment, reduced physical performance and higher need of assistance [30,31]. |
| Climatic change | Climate changes might influence the onset of several health issues, including cardiovascular disorders [32], musculoskeletal painful conditions [33], psychiatric health status [34] and even death [35]. |
| Urban, suburban or rural setting and green areas | In recent years, it has been observed that non-communicable diseases (NCDs), including diabetes, obesity, and heart disease, are strongly associated with urbanization [36], and urban or rural setting plays a key role in the prevalence of these environmental diseases. In this context, recent research suggested that rural and urban organization of the areas might affect not only the prevalence of environmental diseases but also their clinical course [37,38]. In addition, it has been reported a close link between exposure to residential green spaces and improved health outcomes in urban populations [39,40,41,42]. |
| Socioeconomic condition | Socioeconomic condition significantly affects human health leading to disparities in accessibility to healthy behaviors and healthcare service. In particular, socioeconomic conditions appear to be related primarily to body composition, obesity and power physical activity levels [43]. According to the study by Feng et al. [44], the mean BMI was higher in the poorest socioeconomic condition, with increased inactivity time and poor physical activity levels. An interesting analysis of social control by Karriker-Jaffe et al. [45] reported that a family history of alcoholism might exacerbate a high-risk drinking trend. To decrease the high-risk of drinking and alcohol issues, policymakers should consider the differential advantages of limiting alcohol access for persons from high-risk households [46]. In addition, healthcare service deliveries are recently implemented with digital innovation solutions to boost the management of functional impairment. Telemedicine and telerehabilitation solutions are growing solutions that have been proposed to overcome barriers to healthcare accessibility [47]. However, it has been reported that social disparities might reduce accessibility to technological interventions for patients with socioeconomic disadvantages. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lippi, L.; de Sire, A.; Folli, A.; Turco, A.; Moalli, S.; Ammendolia, A.; Maconi, A.; Invernizzi, M. Environmental Factors in the Rehabilitation Framework: Role of the One Health Approach to Improve the Complex Management of Disability. Int. J. Environ. Res. Public Health 2022, 19, 15186. https://doi.org/10.3390/ijerph192215186
Lippi L, de Sire A, Folli A, Turco A, Moalli S, Ammendolia A, Maconi A, Invernizzi M. Environmental Factors in the Rehabilitation Framework: Role of the One Health Approach to Improve the Complex Management of Disability. International Journal of Environmental Research and Public Health. 2022; 19(22):15186. https://doi.org/10.3390/ijerph192215186
Chicago/Turabian StyleLippi, Lorenzo, Alessandro de Sire, Arianna Folli, Alessio Turco, Stefano Moalli, Antonio Ammendolia, Antonio Maconi, and Marco Invernizzi. 2022. "Environmental Factors in the Rehabilitation Framework: Role of the One Health Approach to Improve the Complex Management of Disability" International Journal of Environmental Research and Public Health 19, no. 22: 15186. https://doi.org/10.3390/ijerph192215186
APA StyleLippi, L., de Sire, A., Folli, A., Turco, A., Moalli, S., Ammendolia, A., Maconi, A., & Invernizzi, M. (2022). Environmental Factors in the Rehabilitation Framework: Role of the One Health Approach to Improve the Complex Management of Disability. International Journal of Environmental Research and Public Health, 19(22), 15186. https://doi.org/10.3390/ijerph192215186









