Individual Differences in the Association of Lifestyle with Cardiometabolic Risk in Middle-Aged Koreans Based on Traditional Korean Medicine
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Variables
2.2.1. Lifestyle Factors
2.2.2. Sociodemographic Variables
2.2.3. Anthropometric and Biochemical Variables
2.3. Definition of Cardiometabolic Risk Factors
2.4. Sasang Constitution Type
2.5. Statistical Analysis
3. Results
3.1. The Participants’ General Characteristics
3.2. Association between Each Lifestyle and CM Risk by SC Type
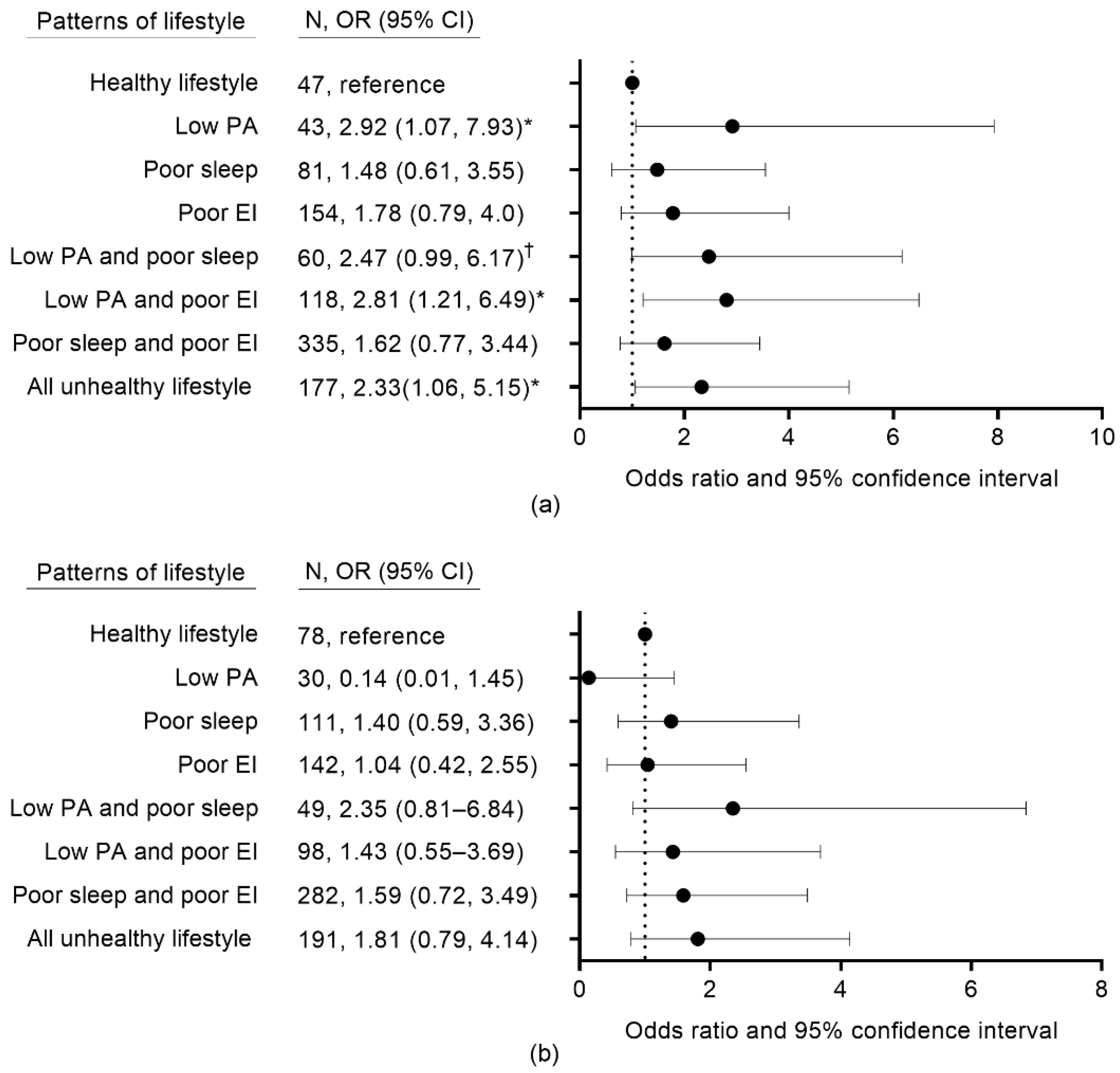
3.3. Association between Lifestyle Patterns and CM Risk
3.4. Associations between Each Lifestyle and Individual CM Risk Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eckel, R.H.; Kahn, R.; Robertson, R.M.; Rizza, R.A. Preventing cardiovascular disease and diabetes: A call to action from the American Diabetes Association and the American Heart Association. Circulation 2006, 113, 2943–2946. [Google Scholar] [CrossRef] [PubMed]
- Leiter, L.A.; Fitchett, D.H.; Gilbert, R.E.; Gupta, M.; Mancini, G.J.; McFarlane, P.A.; Ross, R.; Teoh, H.; Verma, S.; Anand, S. Cardiometabolic risk in Canada: A detailed analysis and position paper by the cardiometabolic risk working group. Can. J. Cardiol. 2011, 27, e1–e33. [Google Scholar] [CrossRef] [PubMed]
- Maddaloni, E.; D’Onofrio, L.; Alessandri, F.; Mignogna, C.; Leto, G.; Pascarella, G.; Mezzaroma, I.; Lichtner, M.; Pozzilli, P.; Agrò, F.E. Cardiometabolic multimorbidity is associated with a worse Covid-19 prognosis than individual cardiometabolic risk factors: A multicentre retrospective study (CoViDiab II). Cardiovasc. Diabetol. 2020, 19, 164. [Google Scholar] [CrossRef] [PubMed]
- Miranda, J.J.; Carrillo-Larco, R.M.; Ferreccio, C.; Hambleton, I.R.; Lotufo, P.A.; Nieto-MartSínez, R.; Zhou, B.; Bentham, J.; Bixby, H.; Hajifathalian, K. Trends in cardiometabolic risk factors in the Americas between 1980 and 2014: A pooled analysis of population-based surveys. Lancet Glob. Health 2020, 8, e123–e133. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Fried, T.R.; Boyd, C.M. Designing health care for the most common chronic condition—multimorbidity. JAMA 2012, 307, 2493–2494. [Google Scholar] [CrossRef]
- Hozawa, A. Attributable fractions of risk factors for cardiovascular diseases. J. Epidemiol. 2011, 21, 81–86. [Google Scholar] [CrossRef]
- Hulsegge, G.; Looman, M.; Smit, H.A.; Daviglus, M.L.; van der Schouw, Y.T.; Verschuren, W.M. Lifestyle changes in young adulthood and middle age and risk of cardiovascular disease and all-cause mortality: The Doetinchem Cohort Study. J. Am. Heart Assoc. 2016, 5, e002432. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.P.; Grandner, M.A.; Brown, D.; Conroy, M.B.; Jean-Louis, G.; Coons, M.; Bhatt, D.L. Sleep duration and quality: Impact on lifestyle behaviors and cardiometabolic health: A scientific statement from the American Heart Association. Circulation 2016, 134, e367–e386. [Google Scholar] [CrossRef]
- Andersson, C.; Vasan, R.S. Epidemiology of cardiovascular disease in young individuals. Nat. Rev. Cardiol. 2018, 15, 230–240. [Google Scholar] [CrossRef]
- Tsai, M.C.; Lee, C.C.; Liu, S.C.; Tseng, P.J.; Chien, K.L. Combined healthy lifestyle factors are more beneficial in reducing cardiovascular disease in younger adults: A meta-analysis of prospective cohort studies. Sci. Rep. 2020, 10, 18165. [Google Scholar] [CrossRef]
- Freisling, H.; Viallon, V.; Lennon, H.; Bagnardi, V.; Ricci, C.; Butterworth, A.S.; Sweeting, M.; Muller, D.; Romieu, I.; Bazelle, P. Lifestyle factors and risk of multimorbidity of cancer and cardiometabolic diseases: A multinational cohort study. BMC Med. 2020, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Singh-Manoux, A.; Fayosse, A.; Sabia, S.; Tabak, A.; Shipley, M.; Dugravot, A.; Kivimäki, M. Clinical, socioeconomic, and behavioural factors at age 50 years and risk of cardiometabolic multimorbidity and mortality: A cohort study. PLoS Med. 2018, 15, e1002571. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Pham, D.D. Sasang constitutional medicine as a holistic tailored medicine. Evid. Based Complement. Altern. Med. 2009, 6, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Bae, N.Y.; Lee, E. Clinical practice guideline for Sasang constitutional medicine: Prevention and risk fators of sasangin disease. J. Sasang Constit. Med. 2015, 27, 82–109. [Google Scholar] [CrossRef][Green Version]
- Park, J.E.; Shin, C.; Lee, S. Effect of Lifestyle Factors on Hypertension by Constitution Type: A Large Community-Based Study. Evid. Based Complement. Altern. Med. 2019, 2019, 3231628. [Google Scholar] [CrossRef]
- Kim, T.Y.; You, S.E.; Ko, Y.S. Association between Sasang constitutional types with obesity factors and sleep quality. Integr. Med. Res. 2018, 7, 341–350. [Google Scholar] [CrossRef]
- Kim, J.; Jeong, K.; Lee, S.; Seo, B.N.; Baek, Y. Low nutritional status links to the prevalence of pre-metabolic syndrome and its cluster in metabolically high-risk Korean adults: A cross-sectional study. Medicine 2021, 100, e25905. [Google Scholar] [CrossRef]
- Kim, J.; Jeong, K.; Lee, S.; Baek, Y. Relationship between Low Vegetable Consumption, Increased High-Sensitive C-Reactive Protein Level, and Cardiometabolic Risk in Korean Adults with Tae-Eumin: A Cross-Sectional Study. Evid. Based Complement. Altern. Med. 2021, 100, e25905. [Google Scholar] [CrossRef]
- Baek, Y.; Seo, B.N.; Jeong, K.; Yoo, H.; Lee, S. Lifestyle, genomic types and non-communicable diseases in Korea: A protocol for the Korean Medicine Daejeon Citizen Cohort study (KDCC). BMJ Open 2020, 10, e034499. [Google Scholar] [CrossRef]
- Armstrong, T.; Bull, F. Development of the world health organization global physical activity questionnaire (GPAQ). J. Public Health 2006, 14, 66–70. [Google Scholar] [CrossRef]
- Jeon, J.Y. Development of the Korean Version of Global Physical Activity Questionnaire and Assessment of Reliability and Validity; Korea Centers for Disease Control and Prevention: Osong, Korea, 2013; pp. 1–105. [Google Scholar]
- Ministry of Health and Welfare. Korea Health Statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2); Korea Centers for Disease Control and Prevention: Cheongwon, Korea, 2012. [Google Scholar]
- Yook, S.M.; Park, S.; Moon, H.K.; Kim, K.; Shim, J.E.; Hwang, J.Y. Development of Korean healthy eating index for adults using the Korea national health and nutrition examination survey data. J. Nutr. Health 2015, 48, 419–428. [Google Scholar] [CrossRef]
- Ezzati, M.; Lopez, A.D.; Rodgers, A.; Murray, C.J. Comparative quantification of health risks. In Global and Regional Burden of Disease Attributable to Selected Major Risk Factors; World Health Organization: Geneva, Switzerland, 2004; p. 968. [Google Scholar]
- National Cholesterol Education Program. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3421. [Google Scholar]
- Baek, Y.H.; Jang, E.S.; Park, K.H.; Yoo, J.H.; Jin, H.J. Lee, S.W. Development and validation of brief KS-15 (Korea Sasang Constitutional Diagnostic Questionnaire) based on body shape, temperament and symptoms. J. Sasang Constit. Med. 2015, 27, 211–221. [Google Scholar] [CrossRef]
- Kim, Y.; Jang, E. Test-retest reliability of Brief KS-15: Korean Sasang constitutional diagnostic questionnaire. J. Physiol. Pathol. Korean Med. 2016, 30, 177–183. [Google Scholar] [CrossRef]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef] [PubMed]
- Gesteiro, E.; Megía, A.; Guadalupe-Grau, A.; Fernandez-Veledo, S.; Vendrell, J.; González-Gross, M. Early identification of metabolic syndrome risk: A review of reviews and proposal for defining pre-metabolic syndrome status. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2557–2574. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.H.; Kang, D.R.; Jang, J.Y.; Shin, J.H.; Kim, J.Y.; Choi, S.; Cho, E.J.; Park, J.S.; Sohn, I.S.; Jo, S.H. Metabolic syndrome epidemic among Korean adults: Korean survey of Cardiometabolic Syndrome (2018). Atherosclerosis 2018, 277, 47–52. [Google Scholar] [CrossRef]
- Cho, Y.A.; Kim, J.; Cho, E.R.; Shin, A. Dietary patterns and the prevalence of metabolic syndrome in Korean women. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 893–900. [Google Scholar] [CrossRef]
- de Carvalho Vidigal, F.; Ribeiro, A.Q.; Babio, N.; Salas-Salvadó, J.; Bressan, J. Prevalence of metabolic syndrome and pre-metabolic syndrome in health professionals: LATINMETS Brazil study. Diabetol. Metab. Syndr. 2015, 7, 1–9. [Google Scholar]
- Pham, D.D.; Leem, C.H. Body temperature regulation: Sasang typology-based perspective. Integr. Med. Res. 2015, 4, 189–194. [Google Scholar] [CrossRef]
- Shim, E.B.; Lee, S.W.; Kim, J.Y.; Leem, C.H.; Earm, Y.E. Taeeum-type people in Sasang constitutional medicine have a reduced mitochondrial metabolism. Integr. Med. Res. 2012, 1, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Cha, S.; Koo, I.; Park, B.L.; Jeong, S.; Choi, S.M.; Kim, K.S.; Shin, H.D.; Kim, J.Y. Genetic Effects of FTO and MC4R Polymorphisms on Body Mass in Constitutional Types. Evid. Based Complement Altern. Med. 2011, 2011, 106390. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.E.; Shin, S.; Lee, H.W.; Lim, J.; Lee, J.k.; Shin, A.; Kang, D. Association between sleep duration and metabolic syndrome: A cross-sectional study. BMC Public Health 2018, 18, 720. [Google Scholar] [CrossRef]
- Han, Y.R.; Lee, H.B.; Han, S.Y.; Kim, B.J.; Lee, S.J.; Chae, H. Systematic review of type-specific pathophysiological symptoms of Sasang typology. Integr. Med. Res. 2016, 5, 83–98. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.M.; Kim, B.J.; Shin, S.; Hwang, M. Changes in Body Water Caused by Sleep Deprivation in Taeeum and Soyang Types in Sasang Medicine: Prospective Intervention Study. Evid. Based Complement Altern. Med. 2017, 2017, 2105343. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, S.T.; Singh-Manoux, A.; Pentti, J.; Madsen, I.E.; Sabia, S.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Goldberg, M. Association of healthy lifestyle with years lived without major chronic diseases. JAMA Intern. Med. 2020, 180, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Yamaoka, K.; Tango, T. Effects of lifestyle modification on metabolic syndrome: A systematic review and meta-analysis. BMC Med. 2012, 10, 138. [Google Scholar] [CrossRef]
| Variable | CM Risk Group (n = 676) | Normal Group (n = 1320) | p-Value | |||
|---|---|---|---|---|---|---|
| TE | Non-TE | TE | Non-TE | |||
| (n = 522) | (n = 154) | (n = 493) | (n = 827) | |||
| Age (y) | 30–44 | 235 (45) | 42 (27.3) | 290 (58.8) | 429 (51.9) | <0.001 |
| 45–55 | 287 (55) | 112 (72.7) | 203 (41.2) | 398 (48.1) | ||
| Sex | Men | 243 (46.6) | 70 (45.5) | 131 (26.6) | 166 (20.1) | <0.001 |
| Women | 279 (53.5) | 84 (54.6) | 362 (73.4) | 661 (79.9) | ||
| Married status 1 | Unmarried | 60 (11.6) | 12 (7.8) | 89 (18.1) | 114 (13.8) | 0.003 |
| Married | 458 (88.4) | 141 (92.2) | 404 (82) | 711 (86.2) | ||
| Education 1 | Under high school | 201 (38.9) | 57 (37.3) | 160 (32.6) | 293 (35.6) | 0.213 |
| College and higher | 316 (61.1) | 96 (62.8) | 331 (67.4) | 531 (64.4) | ||
| Smoking status | Never | 356 (68.2) | 107 (69.5) | 409 (83) | 716 (86.6) | <0.001 |
| Former | 71 (13.6) | 17 (11) | 38 (7.7) | 37 (4.5) | ||
| Current | 95 (18.2) | 30 (19.5) | 46 (9.3) | 74 (9) | ||
| Alcohol consumption | Nondrinker | 184 (35.3) | 58 (37.7) | 191 (38.7) | 357 (43.2) | 0.001 |
| Responsible | 260 (49.8) | 71 (46.1) | 258 (52.3) | 395 (47.8) | ||
| Hazardous | 78 (14.9) | 25 (16.2) | 44 (8.9) | 75 (9.1) | ||
| Disease history (yes) | Hypertension | 84 (16.1) | 21 (13.6) | 12 (2.4) | 22 (2.7) | <0.001 |
| Diabetes | 28 (5.4) | 6 (3.9) | 4 (0.8) | 7 (0.9) | <0.001 | |
| Dyslipidemia | 81 (15.5) | 16 (10.4) | 25 (5.1) | 49 (5.9) | <0.001 | |
| BMI (kg/m2) | 28.2 ± 3.1 a | 23.3 ± 1.7 c | 25.3 ± 2.3 b | 21.5 ± 2 d | <0.001 | |
| CM risk factor | WC (cm) | 92.5 ± 7.9 a | 82.0 ± 6.3 c | 83.9 ± 6.4 b | 76 ± 6.3 d | <0.001 |
| SBP (mmHg) | 126.5 ± 15.6 a | 126.4 ± 17 a | 113.8 ± 12.2 b | 111 ± 12.5 c | <0.001 | |
| DBP (mmHg) | 81.1 ± 12.7 a | 80 ± 11.8 a | 71.1 ± 9.9 b | 68.9 ± 9.9 c | <0.001 | |
| TG (mg/dL) | 198.3 ± 158.8 a | 227.1 ± 238.9 a | 97.8 ± 43.9 b | 93.3 ± 53.8 c | <0.001 | |
| HDL-C (mg/dL) | 47.6 ± 10.3 a | 48.3 ± 12.2 a | 58.9 ± 11.8 b | 63.1 ± 13.4 c | <0.001 | |
| FPG (mg/dL) | 90.7 ± 22.7 a | 92.7 ± 28 a | 81.4 ± 7.3 b | 80.1 ± 8.4 b | <0.001 | |
| TE Group | Non-TE Group | |||||
|---|---|---|---|---|---|---|
| No. CM Risk (No/Yes) | Model 1 | Model 2 | No. CM Risk (No/Yes) | Model 1 | Model 2 | |
| Physical activity | ||||||
| High | 150/150 | reference | 249/45 | reference | ||
| Moderate | 165/152 | 0.98 (0.71–1.36) | 1.02 (0.69–1.51) | 268/51 | 1.36 (0.85–2.17) | 1.31 (0.80–2.15) |
| Low | 178/220 | 1.27 (0.93–1.74) | 1.63 (1.13–2.38) * | 310/58 | 1.42 (0.9–2.24) | 1.34 (0.83–2.16) |
| Sleep duration | ||||||
| 7 h | 174/188 | reference | 302/46 | reference | ||
| ≤6 h | 224/258 | 1.06 (0.8–1.41) | 0.92 (0.66–1.29) | 380/76 | 1.4 (0.91–2.14) | 1.53 (0.98–2.39) † |
| ≥8 h | 95/76 | 0.81 (0.56–1.19) | 0.88 (0.56–1.39) | 145/32 | 1.84 (1.08–3.14) * | 1.87 (1.07–3.29) * |
| Eating index | ||||||
| High | 125/106 | reference | 227/41 | reference | ||
| Moderate | 242/277 | 1.41 (1.02–1.95) * | 1.11 (0.76–1.62) | 413/88 | 1.31 (0.85–2.02) | 1.31 (0.83–2.05) |
| Low | 126/139 | 1.26 (0.86–1.84) | 1.05 (0.67–1.65) | 187/25 | 1.06 (0.59–1.89) | 1.04 (0.56–1.91) |
| High WC | High BP | High TG | Low HDL-C | High FPG | ||
|---|---|---|---|---|---|---|
| TE group | Physical activity (ref. = high) | |||||
| Moderate | 0.98 (0.64–1.5) | 1.17 (0.8–1.7) | 1.0 (0.69–1.44) | 0.85 (0.59–1.24) | 1.93 (1.06–3.51) * | |
| Low | 1.7 (1.13–2.56) * | 1.24 (0.87–1.78) | 1.39 (0.99–1.96) | 1.11 (0.78–1.58) | 2.04 (1.14–3.63) * | |
| Sleep duration (ref. = 7 h) | ||||||
| ≤6 h | 1.12 (0.78–1.61) | 0.86 (0.62–1.18) | 0.99 (0.73–1.36) | 0.75 (0.55–1.04) | 1.51 (0.91–2.52) | |
| ≥8 h | 1.17 (0.73–1.9) | 0.54 (0.34–0.86) | 1.02 (0.67–1.57) | 0.7 (0.45–1.09) | 1.81 (0.92–3.53) | |
| Eating index (ref. = high) | ||||||
| Moderate | 0.87 (0.58–1.3) | 1.21 (0.83–1.77) | 0.97 (0.67–1.39) | 0.97 (0.68–1.39) | 1.29 (0.73–2.27) | |
| Low | 0.85 (0.52–1.38) | 0.86 (0.55–1.35) | 1.2 (0.79–1.83) | 0.96 (0.62–1.49) | 0.74 (0.36–1.51) | |
| Non-TE group | Physical activity (ref. = high) | |||||
| Moderate | 1.1 (0.48–2.51) | 0.92 (0.6–1.44) | 1.4 (0.87–2.25) | 1.76 (1.09–2.83) * | 0.98 (0.4–2.41) | |
| Low | 1.64 (0.75–3.58) | 0.8 (0.52–1.23) | 1.53 (0.97–2.41) | 1.42 (0.88–2.29) | 1.16 (0.51–2.66) | |
| Sleep duration (ref. = 7 h) | ||||||
| ≤6 h | 2.14 (1.01–4.5) * | 1.04 (0.7–1.53) | 1.29 (0.85–1.95) | 1.45 (0.94–2.21) | 1.13 (0.5–2.55) | |
| ≥8 h | 1.45 (0.56–3.74) | 0.73 (0.42–1.25) | 1.36 (0.79–2.33) | 1.84 (1.09–3.1) * | 1.9 (0.74–4.84) | |
| Eating index (ref. = high) | ||||||
| Moderate | 1.47 (0.7–3.1) | 1.36 (0.88–2.09) | 1.85 (1.18–2.89) * | 1.15 (0.76–1.74) | 0.77 (0.35–1.72) | |
| Low | 0.9 (0.32–2.48) | 1.1 (0.62–1.92) | 1.43 (0.8–2.57) | 0.87 (0.49–1.54) | 1.0 (0.35–2.82) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baek, Y.; Park, K.; Jung, K.; Lee, S. Individual Differences in the Association of Lifestyle with Cardiometabolic Risk in Middle-Aged Koreans Based on Traditional Korean Medicine. Int. J. Environ. Res. Public Health 2022, 19, 14963. https://doi.org/10.3390/ijerph192214963
Baek Y, Park K, Jung K, Lee S. Individual Differences in the Association of Lifestyle with Cardiometabolic Risk in Middle-Aged Koreans Based on Traditional Korean Medicine. International Journal of Environmental Research and Public Health. 2022; 19(22):14963. https://doi.org/10.3390/ijerph192214963
Chicago/Turabian StyleBaek, Younghwa, Kihyun Park, Kyoungsik Jung, and Siwoo Lee. 2022. "Individual Differences in the Association of Lifestyle with Cardiometabolic Risk in Middle-Aged Koreans Based on Traditional Korean Medicine" International Journal of Environmental Research and Public Health 19, no. 22: 14963. https://doi.org/10.3390/ijerph192214963
APA StyleBaek, Y., Park, K., Jung, K., & Lee, S. (2022). Individual Differences in the Association of Lifestyle with Cardiometabolic Risk in Middle-Aged Koreans Based on Traditional Korean Medicine. International Journal of Environmental Research and Public Health, 19(22), 14963. https://doi.org/10.3390/ijerph192214963






