The Feasibility and Impact of Practising Online Forest Bathing to Improve Anxiety, Rumination, Social Connection and Long-COVID Symptoms: A Pilot Study
Abstract
1. Introduction
2. Aims
3. Materials and Methods
3.1. Design
3.2. Participants
3.3. Procedure
3.4. Outcome Measures
Feasibility
3.5. Survey
3.6. Intervention
4. Results
4.1. Feasibility
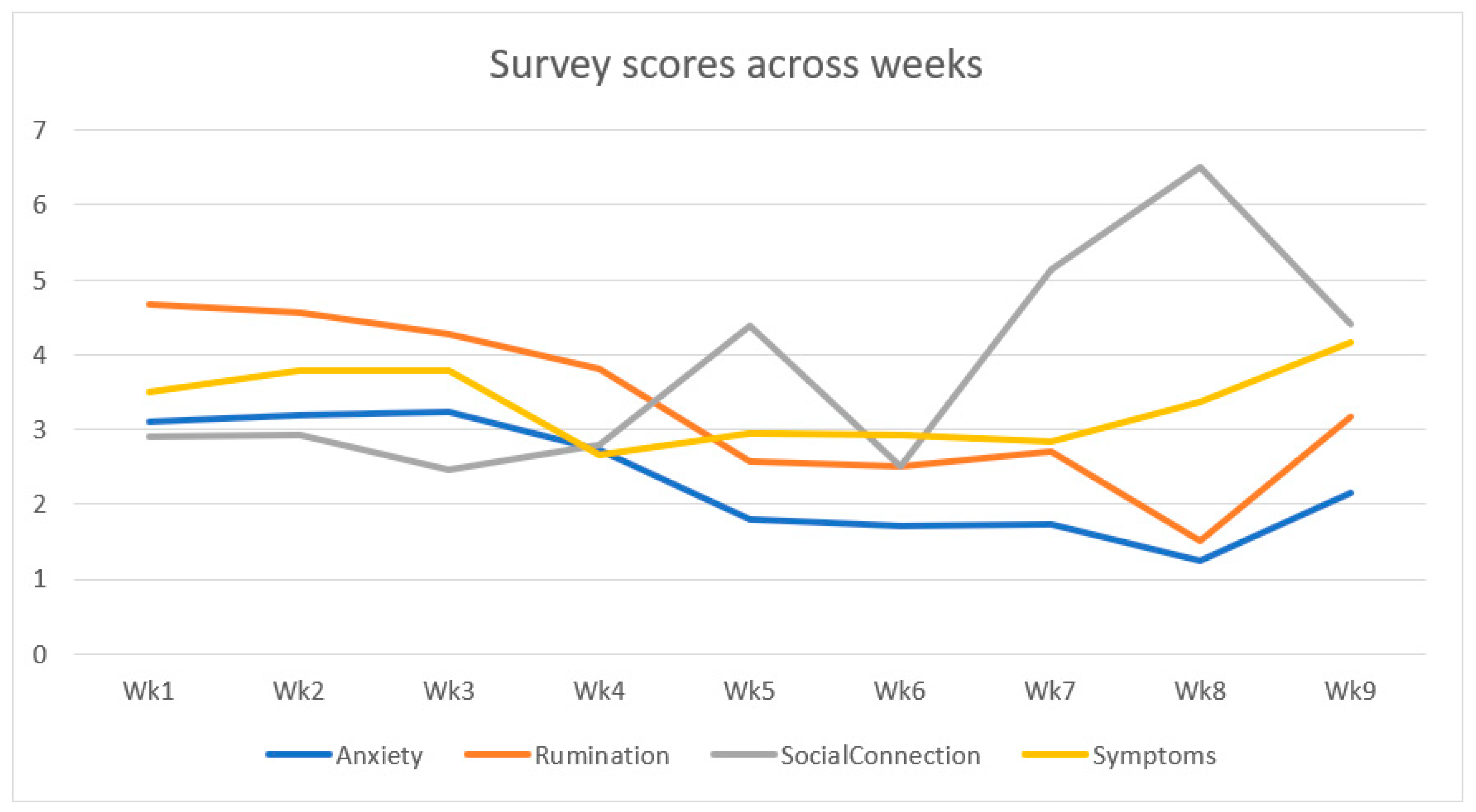
4.2. Impact
4.3. Qualitative Results
5. Discussion
Limitations and Future Directions
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Responding to Community Spread of COVID-19; Reference WHO/COVID-19/Community_Transmission/20201; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Deer, R.R.; A Rock, M.; Vasilevsky, N.; Carmody, L.; Rando, H.; Anzalone, A.J.; Basson, M.D.; Bennett, T.D.; Bergquist, T.; Boudreau, E.A.; et al. Characterizing Long COVID: Deep Phenotype of a Complex Condition. eBioMedicine 2021, 74, 103722. [Google Scholar] [CrossRef] [PubMed]
- Burton, C.; Dawes, H.; Goodwill, S.; Thelwell, M.; Dalton, C. Symptom variation, correlations, and relationship to physical activity in Long-COVID: Intensive longitudinal study. medRxiv 2022. [Google Scholar] [CrossRef]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef] [PubMed]
- Michelen, M.; Manoharan, L.; Elkheir, N.; Cheng, V.; Dagens, A.; Hastie, C.; O’Hara, M.; Suett, J.; Dahmash, D.; Bugaeva, P.; et al. Characterising long COVID: A living systematic review. BMJ Glob. Health 2021, 6, e005427. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.A.; O’Brien, K.K. Conceptualising long COVID as an episodic health condition. BMJ Glob. Health 2021, 6, e007004. [Google Scholar] [CrossRef] [PubMed]
- Faghy, M.A.; Maden-Wilkinson, T.; Arena, R.; Copeland, R.J.; Owen, R.; Hodgkins, H.; Willmott, A. COVID-19 patients require multi-disciplinary rehabilitation approaches to address persisting symptom profiles and restore pre-COVID quality of life. Expert Rev. Respir. Med. 2022, 16, 595–600. [Google Scholar] [CrossRef]
- Hanson, S.W.; Abbafati, C.; Aerts, J.G.; Al-Aly, Z.; Ashbaugh, C.; Ballouz, T.; Vos, T. A global systematic analysis of the occurrence, severity, and recovery pattern of long COVID in 2020 and 2021. medRxiv 2022. [Google Scholar] [CrossRef]
- Thompson, E.J.; Williams, D.M.; Walker, A.J.; Mitchell, R.E.; Niedzwiedz, C.L.; Yang, T.C.; Steves, C.J. Long COVID burden and risk factors in 10 UK longitudinal studies and electronic health records. Nat. Commun. 2022, 13, 3528. [Google Scholar] [CrossRef]
- Hawke, L.D.; Nguyen, A.T.P.; Ski, C.F.; Thompson, D.R.; Ma, C.; Castle, D. Interventions for mental health, cognition, and psychological wellbeing in long COVID: A systematic review of registered trials. Psychol. Med. 2022, 52, 2426–2440. [Google Scholar] [CrossRef]
- Chandan, J.S.; Brown, K.R.; Simms-Williams, N.; Bashir, N.Z.; Camaradou, J.; Heining, D.; Aiyegbusi, O.L. Non-pharmacological therapies for postviral syndromes, including Long COVID: A systematic review. medRxiv 2022. [Google Scholar] [CrossRef]
- Prabawa, I.M.Y.; Silakarma, D.; Manuaba, I.B.A.P. Physical Rehabilitation Therapy for Long COVID-19 Patient with Respiratory Sequelae: A Systematic Review. Open Access Maced. J. Med. Sci. 2022, 10, 468–474. [Google Scholar] [CrossRef]
- del Corral, T.; Garrido, R.F.; Plaza-Manzano, G.; Fernández-De-Las-Peñas, C.; Navarro-Santana, M.; López-De-Uralde-Villanueva, I. Home-based respiratory muscle training on quality of life and exercise tolerance in long-term post-COVID-19: Randomized controlled trial. Ann. Phys. Rehabil. Med. 2022, 101709, in press. [Google Scholar] [CrossRef] [PubMed]
- Estebanez-Pérez, M.-J.; Pastora-Bernal, J.-M.; Martín-Valero, R. The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients with Long COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 9566. [Google Scholar] [CrossRef] [PubMed]
- Robbins, T.; Gonevski, M.; Clark, C.; Baitule, S.; Sharma, K.; Magar, A.; Randeva, H.S. Hyperbaric oxygen therapy for the treatment of long COVID: Early evaluation of a highly promising intervention. Clin. Med. 2021, 21, e629. [Google Scholar] [CrossRef]
- Hawkins, J.; Hires, C.; Keenan, L.; Dunne, E. Aromatherapy blend of thyme, orange, clove bud, and frankincense boosts energy levels in post-COVID-19 female patients: A randomized, double-blinded, placebo controlled clinical trial. Complement. Ther. Med. 2022, 67, 102823. [Google Scholar] [CrossRef]
- Fowler-Davis, S.; Platts, K.; Thelwell, M.; Woodward, A.; Harrop, D. A mixed-methods systematic review of post-viral fatigue interventions: Are there lessons for long Covid? PLoS ONE 2021, 16, e0259533. [Google Scholar] [CrossRef]
- Jimenez, M.; DeVille, N.; Elliott, E.; Schiff, J.; Wilt, G.; Hart, J.; James, P. Associations between Nature Exposure and Health: A Review of the Evidence. Int. J. Environ. Res. Public Health. 2021, 18, 4790. [Google Scholar] [CrossRef]
- Yao, W.; Zhang, X.; Gong, Q. The effect of exposure to the natural environment on stress reduction: A meta-analysis. Urban For. Urban Green. 2021, 57, 126932. [Google Scholar] [CrossRef]
- Desrochers, J.E.; Bell, A.L.; Nisbet, E.K.; Zelenski, J.M. Does Spending Time in Nature Help Students Cope with the COVID-19 Pandemic? Sustainability 2022, 14, 2401. [Google Scholar] [CrossRef]
- Wen, Y.; Yan, Q.; Pan, Y.; Gu, X.; Liu, Y. Medical empirical research on forest bathing (Shinrin-yoku): A systematic review. Environ. Health Prev. Med. 2019, 24, 1–21. [Google Scholar] [CrossRef]
- Antonelli, M.; Barbieri, G.; Donelli, D. Effects of forest bathing (shinrin-yoku) on levels of cortisol as a stress biomarker: A systematic review and meta-analysis. Int. J. Biometeorol. 2019, 63, 1117–1134. [Google Scholar] [CrossRef] [PubMed]
- Kotera, Y.; Richardson, M.; Sheffield, D. Effects of Shinrin-Yoku (Forest Bathing) and Nature Therapy on Mental Health: A Systematic Review and Meta-analysis. Int. J. Ment. Health Addict. 2020, 20, 337–361. [Google Scholar] [CrossRef]
- McEwan, K.; Giles, D.; Clarke, F.J.; Kotera, Y.; Evans, G.; Terebenina, O.; Minou, L.; Teeling, C.; Wood, W. A pragmatic controlled trial of Forest Bathing compared with Compassionate Mind Training in a UK population: Impacts on self-reported wellbeing and heart rate variability. Sustainability 2021, 13, 1380. [Google Scholar] [CrossRef]
- Ideno, Y.; Hayashi, K.; Abe, Y.; Ueda, K.; Iso, H.; Noda, M.; Lee, J.-S.; Suzuki, S. Blood pressure-lowering effect of Shinrin-yoku (Forest bathing): A systematic review and meta-analysis. BMC Complement. Altern. Med. 2017, 17, 409. [Google Scholar] [CrossRef]
- Li, Q.; Morimoto, K.; Nakadai, A.; Inagaki, H.; Katsumata, M.; Shimizu, T.; Hirata, Y.; Hirata, K.; Suzuki, H.; Miyazaki, Y.; et al. Forest Bathing Enhances Human Natural Killer Activity and Expression of Anti-Cancer Proteins. Int. J. Immunopathol. Pharmacol. 2007, 20, 3–8. [Google Scholar] [CrossRef]
- Kobayashi, H.; Song, C.; Ikei, H.; Park, B.-J.; Lee, J.; Kagawa, T.; Miyazaki, Y. Forest Walking Affects Autonomic Nervous Activity: A Population-Based Study. Front. Public Health 2018, 6, 278. [Google Scholar] [CrossRef]
- Olson, E.R.T.; Hansen, M.M.; Vermeesch, A. Mindfulness and Shinrin-Yoku: Potential for Physiological and Psychological Interventions during Uncertain Times. Int. J. Environ. Res. Public Health 2020, 17, 9340. [Google Scholar] [CrossRef]
- Muro, A.; Feliu-Soler, A.; Canals, J.; Parrado, E.; Sanz, A. Psychological benefits of Forest Bathing during the COVID-19 pandemic: A pilot study in a Mediterranean forest close to urban areas. J. For. Res. 2021, 27, 71–75. [Google Scholar] [CrossRef]
- Rajoo, K.S.; Karam, D.S.; Abdu, A.; Rosli, Z.; Gerusu, G.J. Addressing psychosocial issues caused by the COVID-19 lockdown: Can urban greeneries help? Urban For. Urban Green. 2021, 65, 127340. [Google Scholar] [CrossRef]
- Hubbard, G.; Daas, C.; Johnston, M.; Murchie, P.; Thompson, C.; Dixon, D. Are Rurality, Area Deprivation, Access to Outside Space, and Green Space Associated with Mental Health during the COVID-19 Pandemic? A Cross Sectional Study (CHARIS-E). Int. J. Environ. Res. Public Health 2021, 18, 3869. [Google Scholar] [CrossRef]
- De Kort, Y.A.W.; Meijnders, A.L.; Sponselee, A.A.G.; IJsselsteijn, W.A. What’s wrong with virtual trees? Restoring from stress in a mediated environment. J. Environ. Psychol. 2006, 26, 309–320. [Google Scholar] [CrossRef]
- Browning, M.H.E.M.; Mimnaugh, K.J.; van Riper, C.J.; Laurent, H.K.; LaValle, S.M. Can Simulated Nature Support Mental Health? Comparing Short, Single-Doses of 360-Degree Nature Videos in Virtual Reality With the Outdoors. Front. Psychol. 2020, 10, 2667. [Google Scholar] [CrossRef] [PubMed]
- Annerstedt, M.; Jönsson, P.; Wallergård, M.; Johansson, G.; Karlson, B.; Grahn, P.; Hansen, Å.M.; Währborg, P. Inducing physiological stress recovery with sounds of nature in a virtual reality forest—Results from a pilot study. Physiol. Behav. 2013, 118, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, M.; Nogaki, H.; Shimizu, Y.; Stone, T.E.; Kobayashi, T. Individual reactions to viewing preferred video representations of the natural environment: A comparison of mental and physical reactions. Jpn. J. Nurs. Sci. 2016, 14, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Kjellgren, A.; Buhrkall, H. A comparison of the restorative effect of a natural environment with that of a simulated natural environment. J. Environ. Psychol. 2010, 30, 464–472. [Google Scholar] [CrossRef]
- Markwell, N.; Gladwin, T.E. Shinrin-yoku (forest bathing) reduces stress and increases people’s positive affect and well-being in comparison with its digital counterpart. Ecopsychology 2020, 12, 247–256. [Google Scholar] [CrossRef]
- Zabini, F.; Albanese, L.; Becheri, F.R.; Gavazzi, G.; Giganti, F.; Giovanelli, F.; Viggiano, M.P. Comparative study of the restorative effects of forest and urban videos during COVID-19 lockdown: Intrinsic and benchmark values. Int. J. Environ. Res. Public Health 2020, 17, 8011. [Google Scholar] [CrossRef] [PubMed]
- van Houwelingen-Snippe, J.; van Rompay, T.J.; Ben Allouch, S. Feeling connected after experiencing digital nature: A survey study. Int. J. Environ. Res. Public Health 2020, 17, 6879. [Google Scholar] [CrossRef]
- Soga, M.; Evans, M.J.; Tsuchiya, K.; Fukano, Y. A room with a green view: The importance of nearby nature for mental health during the COVID-19 pandemic. Ecol. Appl. 2020, 31, e2248. [Google Scholar] [CrossRef]
- Dzhambov, A.M.; Lercher, P.; Browning, M.H.E.M.; Stoyanov, D.; Petrova, N.; Novakov, S.; Dimitrova, D.D. Does greenery experienced indoors and outdoors provide an escape and support mental health during the COVID-19 quarantine? Environ. Res. 2021, 196, 110420. [Google Scholar] [CrossRef]
- Roviello, V.; Roviello, G.N. Less COVID-19 deaths in southern and insular Italy explained by forest bathing, Mediterranean environment, and antiviral plant volatile organic compounds. Environ. Chem. Lett. 2022, 20, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Roviello, V.; Gilhen-Baker, M.; Vicidomini, C.; Roviello, G.N. Forest-bathing and physical activity as weapons against COVID-19: A review. Environ. Chem. Lett. 2022, 20, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Morimoto, K.; Kobayashi, M.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Shimizu, T.; Li, Y.J.; Wakayama, Y.; et al. A forest bathing trip increases human natural killer activity and expression of anti-cancer proteins in female subjects. J. Biol. Regul. Homeost Agents 2008, 22, 45–55. [Google Scholar] [PubMed]
- Tsao, T.-M.; Tsai, M.-J.; Hwang, J.-S.; Cheng, W.-F.; Wu, C.-F.; Chou, C.-C.; Su, T.-C. Health effects of a forest environment on natural killer cells in humans: An observational pilot study. Oncotarget 2018, 9, 16501–16511. [Google Scholar] [CrossRef]
- White, M.P.; Yeo, N.L.; Vassiljev, P.; Lundstedt, R.; Wallergård, M.; Albin, M.; Lõhmus, M. A prescription for “nature”—The potential of using virtual nature in therapeutics. Neuropsychiatr. Dis. Treat. 2018, 14, 3001–3013. [Google Scholar] [CrossRef] [PubMed]
- Shacham, S. A shortened version of the Profile of Mood States. J. Personal. Assess. 1983, 47, 305–306. [Google Scholar] [CrossRef] [PubMed]
- Moberly, N.J.; Watkins, E.R. Ruminative self-focus and negative affect: An experience sampling study. J. Abnorm. Psychol. 2008. 117, 314. [CrossRef]
- Aron, A.; Aron, E.N.; Smollan, D. Inclusion of other in the self scale and the structure of interpersonal closeness. J. Personal. Soc. Psychol. 1992, 63, 596. [Google Scholar] [CrossRef]
- Sampogna, G.; Di Vincenzo, M.; Giallonardo, V.; Perris, F.; Volpicelli, A.; Del Vecchio, V.; Fiorillo, A. The Psychiatric Consequences of Long-COVID: A Scoping Review. J. Pers. Med. 2022, 12, 1767. [Google Scholar] [CrossRef]
- Cohen, J. Set correlation and contingency tables. Appl. Psychol. Meas. 1988, 12, 425–434. [Google Scholar] [CrossRef]

| Waitlist Control | Post-Intervention | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t | d | |
| Anxiety (POMs) *** | 3.37 | 0.95 | 1.73 | 0.62 | 8.03 | 1.61 |
| Rumination *** | 4.79 | 1.41 | 2.50 | 1.10 | 5.84 | 1.19 |
| Social Connection *** | 2.68 | 1.11 | 4.76 | 1.51 | −6.10 | −1.22 |
| Long-COVID Symptoms ** | 3.99 | 1.16 | 3.11 | 1.15 | 3.65 | 0.73 |
| Major Themes | Minor Themes |
|---|---|
| Feelings of joy and appreciation -frequently expressed with terms like ‘enjoyed’ and ‘loved’ (15) | Barriers to participation–technical problems, other responsibilities, limited time (4) |
| Appreciation of being able to take time out for self (9) | Physical benefits of participation (2) |
| Feelings of calm, peace, and comfort away from pain and rumination about symptoms (6) | Disappointed that sessions ended–appreciated the contact with other people (2) |
| Having a good connection to nature (5) | Outdoor green spaces preferred (2) |
| Having a connection to other people (5) | |
| Better resourced after participation–new skills learnt (5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McEwan, K.; Collett, H.; Nairn, J.; Bird, J.; Faghy, M.A.; Pfeifer, E.; Jackson, J.E.; Cook, C.; Bond, A. The Feasibility and Impact of Practising Online Forest Bathing to Improve Anxiety, Rumination, Social Connection and Long-COVID Symptoms: A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 14905. https://doi.org/10.3390/ijerph192214905
McEwan K, Collett H, Nairn J, Bird J, Faghy MA, Pfeifer E, Jackson JE, Cook C, Bond A. The Feasibility and Impact of Practising Online Forest Bathing to Improve Anxiety, Rumination, Social Connection and Long-COVID Symptoms: A Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(22):14905. https://doi.org/10.3390/ijerph192214905
Chicago/Turabian StyleMcEwan, Kirsten, Harriet Collett, Jean Nairn, Jamie Bird, Mark A. Faghy, Eric Pfeifer, Jessica E. Jackson, Caroline Cook, and Amanda Bond. 2022. "The Feasibility and Impact of Practising Online Forest Bathing to Improve Anxiety, Rumination, Social Connection and Long-COVID Symptoms: A Pilot Study" International Journal of Environmental Research and Public Health 19, no. 22: 14905. https://doi.org/10.3390/ijerph192214905
APA StyleMcEwan, K., Collett, H., Nairn, J., Bird, J., Faghy, M. A., Pfeifer, E., Jackson, J. E., Cook, C., & Bond, A. (2022). The Feasibility and Impact of Practising Online Forest Bathing to Improve Anxiety, Rumination, Social Connection and Long-COVID Symptoms: A Pilot Study. International Journal of Environmental Research and Public Health, 19(22), 14905. https://doi.org/10.3390/ijerph192214905







