Abstract
The increased aging of populations and rises in immigration have prompted the design of new methodologies and instruments for fostering the invisible care of geriatric patients among health science students in accordance with the 2030 Agenda and the SDGs. A total of 656 psychology, nursing and dentistry students participated in this study, which had a pretest–posttest design and was implemented over the course of three academic years. The intervention groups received training using an active learning methodology based on a case study involving a geriatric patient; specifically, a Maghrebi woman. The control groups were not exposed to the case study. The CCI-U questionnaire was designed ad hoc to evaluate the acquisition of invisible competences for caring for geriatric patients in accordance with their age, sex, emotional situation and ethnic origin. The questionnaire had a reliability of α = 0.63 to 0.72 and its factor solution was found to have a good fit. Students in the intervention groups scored higher than those in the control groups, with the difference being statistically significant for ethnic origin in all three undergraduate courses and all three academic years. The proper application of this active learning methodology fosters the invisible care of geriatric patients among students in accordance with the 2030 Agenda.
1. Introduction
1.1. Aging and Multiculturalism
According to a report published by EUROSTAT [1], there are 3,459,090 immigrants aged 65 years or over currently living in Europe. The latest data indicate that 412,198 of them reside in Spain [2]. This is approximately 4% of the entire Spanish population aged 65 years and older (9.5 million).
The number of inhabitants in Spain (47.4 million) is expected to increase by 1 million over the coming 15 years [3]. Forecasts for 2035 predict that the +65 population will increase from 20% to 26.5% of the entire population. These figures warn of a gradual aging of the Spanish population, and it should also be borne in mind that the almost 1.3 million immigrants on the Spanish census who are currently aged between 45 and 64 years will be gradually joining this older demographic segment in the next decades [2].
It has been calculated that, in March 2020, at the start of the COVID-19 pandemic, 390,000 native Spaniards and immigrants were living in nursing homes in Spain. Furthermore, the number of people with dementia in Spain has risen, from 113,874 in 2011 to 443,976 in 2020 [4]. According to data published by the Alzheimer Europe Foundation, Spain is expected to have 1 million cases of dementia by 2025 and 1.7 million by 2050, representing 4% of the population forecast for that country by the middle of the century [5]. In 2011, 1.27% of the native population in Spain aged 65 years or older was diagnosed with Alzheimer’s disease. In the same age group, 0.43% of the immigrant population in Spain was diagnosed with Alzheimer’s. In 2019, 0.08% of the population in Spain < 65 years, 1.97% of those aged 65–79 years and 11.16% of those aged 80 years or over had diagnosed Alzheimer’s [4]. These indices indicate that the increased aging of the native and immigrant population could be linked to a higher number of cases of dementia. It should also be remembered that the 2030 Agenda for Sustainable Development contemplates an integrated agenda for everyone, with special emphasis on avoiding the exclusion and vulnerability of older adults [6].
1.2. Sustainable Development Goals (SDGs) and Invisible Care for Older Adults
Back in 2015, the United Nations proposed 17 different Sustainable Development Goals (SDGs) with the aim of enhancing economic, social and environmental sustainable development. These goals include ensuring healthy lives, promoting well-being for all at all ages and achieving gender equality and empowering all women and girls. In addition, the SDGs aim to ensure high-quality education, paying special attention to cultural diversity and gender equality [7]. To demarcate our intervention and objectives in a wider framework, the SDGs can be used to find solutions to the present issues with an interrelated and integrative approach.
However, new care demands oriented towards integrated care require us to think about multidisciplinary care [8,9] and to promote its presence in university health science degrees, expanding this training to also include other health professionals [10,11], such as physicians, psychologists and physiotherapists, among others.
The concept of care, which has a long tradition in nursing, began to be redefined at the beginning of the second decade of the current century (2010–2015). Ten years earlier, Colliere [12] had initiated this process of reflection by adopting a psychosocial approach to care, defining the most important type of care as that which is invisible and not recorded, referring to knowledge about the care recipient and their environment. Ausserhofer et al. [13] identified care related to patient comfort, communication with patients, the updating and development of care plans and the education of patients and their families as the types of care that European nurses most often do not provide due to unfavourable working conditions or low nurse/patient ratios. This results in the worsening of the quality of care provided, which in turn is reflected in a decrease in patient satisfaction, a drop in indicators [14] and even an increase in the mortality rate [15,16].
Various authors have studied the devaluation and invisibility of comprehensive care in nursing [17], and others [18] have identified specific care interventions, attitudes and behaviours that tend to go unnoticed or to which less value is attached in comparison with visible and quantifiable tasks, such as nursing techniques and tasks delegated by physicians. These authors define this type of care as ”invisible care”, since it involves interventions that are not recorded, transmitted to colleagues or valued institutionally, despite requiring much time and having a positive impact on the well-being, autonomy and safety of patients and their families.
In this same study [18], the authors identified the following as variables of invisible care: the education of patients and their families regarding the new situation and self-care, emotional support, comfort, pain reduction through non-pharmacological treatments and collaboration with health professionals to offer patient-centred care. In addition to being important to well-being and recovery, these types of care are also necessary elements within comprehensive care. However, they rarely enjoy the same degree of recognition as more technical and specialist types of care.
Invisible care is often more closely linked to people’s humanist and emotional dimensions, something which does not appear to be a coincidence and which supports the idea that the type of care that is more closely related to emotional aspects is less highly valued and relegated to second place in favour of the more technical aspects of caring for a patient. In this sense, Allen [19] explores the invisibility of organisational work in nursing, which has increased as a result of certain tasks being delegated to nursing staff by physicians but which should not be confused with invisible care during patient interactions.
In sum, the starting point for the present study was an acknowledgement of the importance of providing high-quality education (SDG 7) that fosters invisible care competences for personal interactions with patients oriented towards SDG 3 (ethical and humanist care of geriatric patients), SDG 5 (gender equality) and SDG 10 (reducing inequality stemming from age and/or cultural origin).
1.3. Active Learning Methodologies for Invisible Care and Its Evaluation
Invisible care is not always addressed in a sufficiently detailed manner in university training programmes. This type of care requires prior thought and reflection and forms the basis of future interactions with geriatric patients. In the last three years (2020–2022), our university has developed/carried out a total of 11 teaching innovation projects linked to Agenda 2030 and health science (four in nursing, one in medicine, five in psychology and one in pharmacy). However, our project is the only one developed at an interdisciplinary level in health science at this university.
The importance of active learning methodologies for health science studies lies in the way these methodologies link professional knowledge acquisition, research, interdisciplinary learning, clinical reasoning and patient-specific interventions [20].
The active learning methodology has the potential to link the three main domains of knowledge required by healthcare professionals: (1) clinical reasoning, assessment and profession-specific interventions; (2) fundamental sciences that underpin basic professional knowledge and its relationship to research; and (3) knowledge resulting from collaborative research between many professional groups. This knowledge is especially oriented to the acquisition of professional competencies and professional accreditation in the university environment [20].
Using an active learning methodology based on a case study of a female geriatric patient, we aim to foster individual and collective reflection among students in order to encourage the development of non-prejudiced, stereotype-free attitudes towards geriatric parents (see Figure 1) [21] and to promote interactions based on patients’ individual characteristics and needs, particularly in relation to their age [22,23], sex [23], emotional situation [18] and cultural origin [24,25], thereby enabling the practice of invisible care.
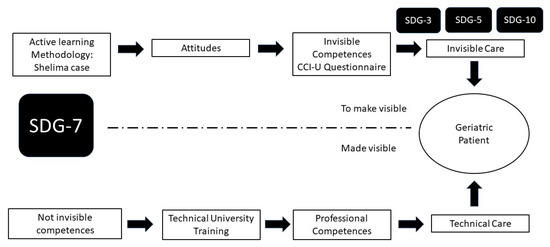
Figure 1.
Invisible care vs. technical care.
The implementation of the active learning methodology promotes reflection and a change in attitudes (see Figure 1) oriented to the invisible care of the geriatric patient. The change in attitudes must emerge prior to the progressive acquisition over time of the competencies and their fit with SDGs 3, 5 and 7.
In addition to technical training that results in the acquisition of professional competences, there is also space for fostering invisible care competences in a balanced manner oriented towards SDGs 3, 5 and 10. These competences are located within the framework of the professional–patient relationship and may emerge in a type of care that is more humanised, respectful and sensitive to constantly changing situations. In this sense, Darbyshire and McKenna [26] ask whether basic nursing care—we would add invisible care as well—has become a ”ghost in the machine”, since its absence is justified within syllabuses by the fact that it is considered to be implicit and dispersed into existing curricula; hence, the need to render invisible care visible. It is here that the use of active learning methodologies is justified. In our study, we used a case study method involving a patient (Shelima) and her clinical treatment. Using the problem-based learning through inquiry method (IBL) [27], our aim was to encourage students in the intervention groups to engage in reflective action and critical thinking [28] in order to become aware of this type of care and render it visible. By applying this innovative teaching process, we hoped to help students avoid the passive model of knowledge acquisition. The idea was that this new knowledge would emerge from new shared and innovative teaching experiences that would contribute to better academic performance by highlighting the usefulness of the subject for students’ future professional activities [29].
Finally, it is important to point out that this methodology involves a recalibration of the teaching scaffolding and the help provided to students through the IBL process. The aid required depends on academic level (first, second or third year), with more intense help and guidance being necessary at the start of the activity. As students move through their degree, however, the scaffolding provided should gradually decrease in order to bestow on them a greater degree of autonomy [30].
These circumstances justify the aim of the present study, which was to design and apply a new active learning methodology for the acquisition of invisible competences in accordance with the SDGs and to evaluate it pre- and posttest using a new instrument designed ad hoc (CCI-U). This strategy enabled us to measure the progress made by students in the acquisition of invisible competences beyond mere academic performance within the framework of the 2030 Agenda.
2. Materials and Methods
2.1. Participants
The participants were 656 students (85.2% women) from the faculties of nursing, psychology and dentistry (see Table 1). A total of 99.2% of the students were Spanish, 0.1% were from Morocco, 0.2% were from East Europe and 0.5% from South America. The percentage of immigrant students in the intervention groups was 0.15%. All were undergraduates over the course of three academic years (2019 to 2022) and enrolled in the following subjects: Psychology, Basic Nursing Methodologies and Quality and Safety in Nursing Care. A sample of 34 students of human histology (dentistry) were added in the last year of the study (2021–2022) in order to further analyse the effect of the intervention program on other health science students. This increase was undertaken after the major restrictions resulting from the COVID-19 pandemic were lifted.

Table 1.
Sociodemographic data.
A total of 576 students (87.8%) participated in the pre- and posttest phases; the remaining 80 (12.2%) failed to complete the posttest phase and were included in the sample only to ensure the sample size necessary for the factor analyses.
2.2. Instruments
Short Sociodemographic Questionnaire: data were collected regarding participants’ sex, academic level and degree course.
Invisible Care for Health Science Studies Questionnaire (Cuestionario de cuidado invisibles en ciencias de la salud (CCI-U)): This questionnaire was designed ad hoc and comprises 17 items (see Appendix A). It measures the acquisition of competences for invisible care in accordance with the patient’s age (factor 1: four items), sex (factor 2: four items), emotional situation (factor 3: three items) and ethnic-cultural origin (factor 4: six items). Of the 17 items, 13 (76%) are phrased as reverse items to avoid response bias. Items are rated on a six-point Likert-type scale (1—completely disagree, 2—mainly disagree, 3—partly disagree, 4—partly agree, 5—mainly agree and 6—completely agree). This six-point scale prevents centrality bias in the responses given.
2.3. Procedure
Five experts collaborated in the design of the CCI-U questionnaire, assessing and selecting the items proposed for the new instrument. Three of them were researchers and university professors specialized in geriatric nursing (invisible care), and another was a professor and researcher in neurosciences specialized in dementia and Alzheimer’s. The fifth expert was a professor and researcher specialized in attitudes and stereotypes towards the elderly and cross-cultural studies.
During this initial process, the Content Validity Index (CVI) indicator was used. Members of the research team proposed a total of 100 items for measuring invisible care in accordance with a patient’s age, sex, emotional situation and ethnic origin. The proposal of these 100 items was based on a review of the literature and pre-existing scales, placing the health science student and the geriatric immigrant patient at the centre of the questionnaire and making sure to represent the four main areas of invisible care: the gender, age, emotional state and ethnicity of the geriatric patient. The items were not extracted from other validated tools and were based on the most common experiences that occur in geriatric centres with immigrant patients and on the experience of the professionals who work in these centres with immigrant elderly people.
The Content Validity Index (CVI) was calculated based on the experts’ scores for all items, using a four-point Likert-type scale (1 = not relevant, 2 = needs serious revision, 3 = relevant but needs minor revision, 4 = quite relevant). The CVI values were greater than 0.79 for 32 items, with scores of between 3 and 4 on the Likert-type scale, thus indicating good content validity [31].
To establish an English-language version of the CCI-U scale, the items were translated by an expert translator with extensive experience in the academic field in general and in psychology in particular [32]. The final English version (see Appendix A) was then translated back into Spanish [33] by three other university faculty members working independently from those responsible for the initial adaptation proposed. Finally, a definitive consensus model (Kappa = 0.89, p < 0.03) was agreed on for the final version of the CCI-U scale. The consensus model (Kappa = 0.93, p < 0.01) was then agreed on for the Spanish version of the CCI-U. Finally, the CCI-U questionnaire was administered to a small sample of 15 participants using a “face validity procedure” to test for possible mistakes and general understanding. The final version presented no problems.
The G*Power program (see 3.1.9.6, Franz Paul: Kiel, Germany) was used to calculate the minimum sample size required in light of the study design and the use of Student’s t-tests (n = 2 groups, control vs. intervention), with a medium effect size (0.50 to 0.79), a confidence level set to 95% and power = 0.8. The results indicated that the minimum sample size required per academic year was 128 [34].
2.4. The Intervention Program
The students in the intervention group participated in the active learning methodology in class time, during practical sessions held from weeks 4 to 11 of the 15 week term (see Figure 2). The methodology was applied over the course of seven face-to-face sessions in the classroom, each lasting 2 h. All the material included in the active learning methodology was uploaded to the e-gela platform (Moodle). The working reports drafted by the intervention groups for the case study (patient Shelima) were submitted to the faculty in paper format.
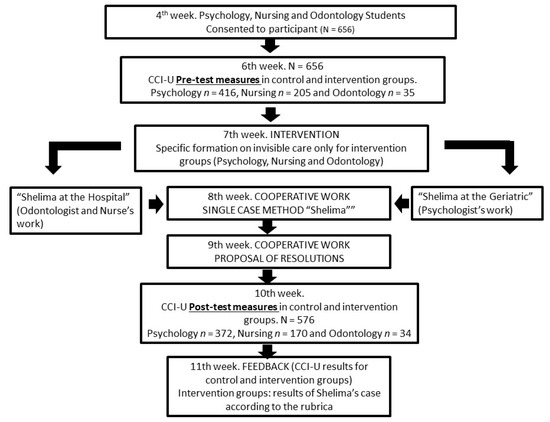
Figure 2.
Flowchart of the active learning methodology on invisible care.
To evaluate the efficacy of the active learning methodology intervention programme, the CCI-U questionnaire was activated on the e-gela (Moodle) platform during the pretest (week 6) and posttest (week 10) phases. Both the control and intervention groups had access to the questionnaire. Following the pretest measures, the intervention group attended a training seminar on invisible care (week 7). As a complementary training activity, outside of face-to-face class time, students of the intervention group were provided with access to a video link on the e-gela platform (Moodle) where they could watch two documentaries, one about the French psychiatry revolution led by Philippe Pinel (1745–1826) and one about the current functioning of short-stay centres for patients with mental disorders. After watching the videos, these students were asked to respond to a ten-question quiz (Socrative Pro) about the most important contents linked to the historical evolution of care.
Throughout weeks 7, 8 and 9 (see Figure 2), students from the intervention group worked on the case study involving the geriatric patient Shelima from the Maghreb. The storyboard of the case encompassed four principal scenarios in a hospital context and one in a nursing home context. The first scene described a conflictive situation in a work therapy session, where Shelima was rejected by the other patients due to being a woman and from the Maghreb. The second scenario featured a conflict between Shelima and the canteen staff over the midday meal menu offered during Ramadan, as well as over some of the patient’s cultural beliefs that prompted her to reject both the menu and her mediation. The third scenario was set during afternoon visiting hours, when Shelima was visited by a friend who lied to her about a series of family events, since she believed that, due to her age, she should not be informed of certain occurrences. Finally, the fourth scenario placed Shelima in a delicate emotional situation when she learned that her daughter did not want to visit her or have anything to do with her. In all the scenarios of this IBL, students from the intervention group were asked to articulate solutions using invisible care and outline them in a case method report.
At the end of the session held in week 9, all the solutions proposed by each intervention group were shared during a cooperative debate.
During week 11, after the posttest evaluation (CCI-U), individual student (control and intervention) results were published (using an anonymous four-digit identifier) and each working group (intervention) was provided with feedback on the case method report submitted.
Unlike the intervention group, the control group was not exposed to Shelima’s case study (IBL) during weeks 7, 8, 9 and 10. In this time, the control group received teaching in another subject. The two groups received the same teaching and subjects without an active learning methodology during the rest of the weeks.
2.5. Data Analyses
All data were processed using the SPSS program (see 22.0, IBM: Armonk, NY, USA). Student’s t test was used to determine whether or not significant differences existed between the control and intervention groups in terms of their pretest and posttest scores. The Wilcoxon U test was performed to determine the degree of individual improvement among students following the application of the active learning methodology. The AMOS program (see 22.0, IBM: Chicago, IL, USA) was used for the confirmatory factor analysis.
2.6. Ethical Considerations
The study was approved by the ethics committee of the University of the Basque Country (CEISH num. M10_2021_278) prior to data collection. All participants received and signed an informed consent document. All the information collected was registered anonymously. Refusal to participate in the study had no impact on students’ academic grades.
3. Results
3.1. Factor Analysis and Reliability
An exploratory factor analysis (EFA) of the CCI-U theoretical construct was conducted with a sample of 335 students using the principal components method with varimax rotation. A total of 15 items with loadings of less than 0.30 were removed from the initial version. The Kaiser–Meyer–Olkin (KMO) index, which was used as a measure of sampling adequacy, was 0.87. Bartlett’s test was statistically significant [χ2 (210) = 1725.83, p < 0.001], enabling the inclusion of the factors selected in the factor analysis. Factor loadings were between 0.38 and 0.76. The four-dimensional solution with a total of 17 items (see Table 2) explained 47.27% of the variance of the CCI-U.

Table 2.
CCI-U questionnaire. Exploratory factor analysis, descriptive statistics and reliabilities (n = 335).
Next, a confirmatory factor analysis (CFA) was carried out with a different subsample (n = 321) to test the goodness of fit of the CCI-U with a four-factor structure (17 items). The kurtosis and asymmetry indicators were all less than 3, thereby indicating univariate normal distribution.
The goodness of fit of the CCI-U questionnaire was assessed using the following indicators: (a) the ratio between chi squared and degrees of freedom (χ2/df); (b) the comparative fit index (CFI); (c) the incremental fit index (IFI); and (d) the root mean square of approximation (RMSEA).
Hu and Bentler [35] consider CFI and IFI values of above 0.90 to be acceptable, and according to Marsh et al. [36], values of between 0.05 and 0.10 are acceptable for the RMSEA. For the theoretical learning subscale, the following CFA values were obtained (n = 321): χ2 (113) = 275.24, p < 0.001; χ2/df = 2.436; CFI = 0.91; IFI = 0.90; RMSEA = 0.06. All items had saturations of over 0.30 (see Figure 3).
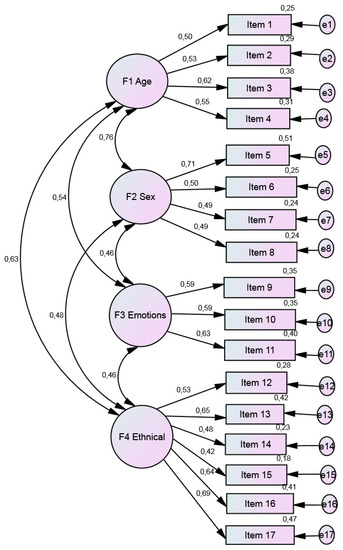
Figure 3.
Confirmatory factor analysis of the CCI-U.
The analysis of the CCI-U revealed reliability coefficients of between α = 0.62 and 0.72 for the different factors. Four factors were found to have acceptable reliability values [37].
3.2. Intervention Effects on Outcome Variables
The control and intervention groups from the psychology, nursing and dentistry undergraduate courses were compared statistically to verify sample normality in terms of previous invisible care. The K-S test revealed a normal distribution (p > 0.05) in all three samples. The skewness values for all groups (Sk = −1.75 to 0.74) were less than 3 and kurtosis values (k = −0.89 to 4.01) were less than 8, confirming good symmetry and normality [38] prior to the intervention programme in each academic year. The results of the student analysis test (see Table 3) revealed, with a reliability level of 95% (p > 0.05), homogeneity between the control and intervention groups prior to the intervention programme.

Table 3.
CCI-U questionnaire. Pretest scores for psychology, nursing and dentistry students in the control and intervention groups, classified by academic year.
The results returned by the Student’s t-test in the posttest phase after the implementation of the methodology to foster invisible care in accordance with patients’ ethnic and cultural origin (see Table 4) revealed a statistically significant group-level effect in psychology and dentistry, whereas in nursing no effect of the intervention on the subject was observed at a higher level (third year).

Table 4.
CCI-U questionnaire. Posttest scores for psychology, nursing and dentistry students in the control and intervention groups, classified by academic year.
In relation to the evolution of the improvement achieved by the active learning methodology across the three academic years analysed, students in the intervention group on the psychology course obtained the best results in all four factors (F1 to F4), as measured in terms of invisible competences during the last academic year (2021–2022). The effect size for care in accordance with the patient’s ethnic origin was medium–large (Dz = 0.36 to 0.84) in this last academic year.
Among the students in the intervention group undertaking the nursing degree, a significant group improvement was observed during the last academic year (2021–2022) in the Basic Nursing Methodologies subject; in this case, in three of the four factors (F2 to F4) with a small effect size (Dz = 0.32 to 0.39). The other subject, Quality and Safety in Nursing Care, could not be analysed over time since it was only taught during the last academic year. Nevertheless, in this subject, significant group-level differences were observed only in F3 (emotional situation), although with a very large effect size (Dz = 1.12). As mentioned in the description of the participants, the results obtained by the first-year dental students could only be analysed in the last year of this project.
Significant group-level differences were observed only in F4 (ethnic origin) and had a small effect size (Dz = 0.36).
In order to explore individual differences in the psychology, nursing and dentistry degree intervention groups, we conducted a Wilcoxon test (see Table 5). Significant differences (p < 0.03) were found among psychology students for the invisible care in accordance with the patient’s ethnic origin factor (F3) over the three academic years studied. Statistically significant individual improvements (p < 0.05) were also observed for the invisible care in accordance with the patient’s sex factor (F2) in the three psychology intervention subgroups during the final academic year (2021–2022).

Table 5.
CCI-U questionnaire. Analysis of the level of individual improvement among psychology, nursing and dentistry students in the control and intervention groups, classified by academic year.
Among the students undertaking the nursing degree, no statistically significant individual improvements were observed in the Basic Nursing Methodologies subject during the 2020–2021 academic year. The greatest statistically significant improvement (p < 0.05) was found during the last academic year (2021–2022) in all factors except F3 (care in accordance with emotional situation); in contrast, among those taking the Quality and Safety in Nursing Care subject, the greatest statistically significant individual improvement (p < 0.05) was found in factors F3 (emotional situation) and F4 (ethnic origin).
Among those studying dentistry, greater statistically significant individual improvements (p < 0.03) were observed in all factors except F2 (patient’s sex).
4. Discussion
The present study analysed the effects of an active learning methodology applied to health science students through an intervention and educational innovation programme located within the framework of the SDGs [7]. The psychology, nursing and dentistry students who participated in the intervention groups scored higher for the acquisition of invisible competences for the care of geriatric patients than their counterparts in the control groups. These findings enabled us to fulfil our aim of developing, applying and evaluating an active learning methodology for acquiring invisible competences in geriatric care.
The CCI-U questionnaire, which was designed ad hoc to evaluate the acquisition of invisible competences by students, was found to have a correct factor structure, as ratified by good fit values in the confirmatory factor analysis. This new instrument was also found to have reliability values similar to those reported for the Perception of Invisible Nursing Care—Hospitalisation (PINC-H) questionnaire [39]. However, unlike the PINC-H, which reflects the perceptions of young and adult oncological patients about invisible care [39], and the Care-Q Caring Assessment instrument [40], which measures the satisfaction of all type of patients regarding two specific elements of invisible care, such as the comfort and confidence provided by the health care professionals, our results confirmed the good functioning of the CCI-U in the evaluation of an intervention designed to foster the acquisition of invisible competences.
The two instruments mentioned above (PINC-H and Care-Q) are not designed to evaluate care based on the perceptions of health professionals, nor are they meant to be applied in university training. In this sense, the CCI-U also performs better than the CIBISA scale [41], which is applied with nursing students and measures three principal factors (well-being, clinical safety and autonomy) but does not address changes in attitude prior to the acquisition of competences in invisible care. From the perspective of teaching innovation, the CCI-U scale focuses on the invisible care of geriatric patients and does so in accordance with the 2030 Agenda, seeking to explore the “bridge” that exists between non-stereotypical attitudes and invisible care competences (see Figure 1). It also includes other health professions (psychology, medicine, dentistry, etc.) as well as nurses and fits in well with the application of active learning methodologies.
The results of the study reveal that the active learning methodology used promotes greater group-level awareness among intervention groups regarding the invisible care of geriatric patients, particularly in relation to factors F3 (emotional situation) and F4 (ethnic origin). Improvements in F1 (patient’s age) and F2 (patient’s sex) were also observed following the intervention, although they were not as statistically significant. In terms of proximal attitudes to ageism and sexism, the results of our study are not consistent with those reported by other studies carried out in relation to geriatric care [23,42,43]. With regard to the nursing students in the intervention groups, the absence of any improvement in factors F1 and F2 may be explained by the fact that care itself is traditionally implicit in their chosen profession [44]. It may also be explained by a greater social awareness and responsibility in relation to the age and sex of geriatric patients, as indeed demonstrated by the high pretest scores for the invisible competences linked to these two factors obtained by the control groups for all three health science degrees.
In the specific cases of the intervention groups from the Psychology and Basic Nursing Methodologies courses, we were able to compare scores across three different academic years, observing a gradual improvement at a group level in the implementation of the active learning methodology, which was particularly reflected in the results obtained for the 2021–2022 academic year. The poorest implementation for all four factors analysed during the three different academic years was in 2020–2021. This may be explained by the restrictions and reduced interactions imposed following the initial lockdown of the university population (including health science students) during the COVID-19 pandemic for the first months of face-to-face teaching [45]. The pandemic suspended synchronous and face-to-face teaching, which is particularly beneficial for the cooperative work required by IBL and knowledge sharing from critical thinking, especially for teaching students in the early grades [46].
In relation to factors F3 (emotional situation) and F4 (ethnic origin), the results may plausibly be explained by the fact that, unlike age and sex, these are not strictly biological factors. Moreover, age- and sex-based stereotypes and discrimination in geriatric care are more commonly known and are therefore more susceptible to social desirability bias among respondents. When we address the emotional situation (F3) of a geriatric patient, we often do so from the perspective of caring for people with dementia, and our results, which revealed an improvement in pretest scores, may be explained by the initial presence of attitudes that were not particularly empathetic [23], avoidant behaviours among caregivers in response to poor prognoses and the irreversible nature of the situation [47,48] and the lack of specialist training in geriatric care among health science students [49].
It should be highlighted that invisible care in accordance with the patient’s ethnic origin (F4) was the factor that responded best to the active learning methodology and the intervention programme with health science students. The low percentage of immigrant students in the intervention groups was not expected to affect the results.
This margin for improvement is consistent with that reported by other studies regarding the existence of racist prejudice towards patients [50,51,52,53,54]. Another possible explanation may be found in the emphasis placed on the Maghrebi origin of the geriatric patient Shelima in the four principal scenarios of the case study storyboard. Everything seems to indicate that age and sex intersect [23] with the ethnic factor, which emerged most noticeably in the scenarios portraying the conflict around the group’s acceptance of Shelima during a work therapy session, the conflict regarding diet during Ramadan, the patient’s poor social–family network and her inability to cope with emotions.
In relation to the individual analysis performed using the Wilcoxon U test, the individual improvement observed in the dentistry intervention groups was greater than the group improvement observed using Student’s t test. This improvement encompassed all factors except F2 (sex). A similar pattern of individual improvement was observed in the psychology intervention groups, particularly in the 2021–2022 academic year, in which the group improvement was negligible. These results may be explained by the fact that the Wilcoxon U test is a non-parametric test and is therefore more sensitive when groups contain fewer than 30 subjects and have non-normal distributions. It is important to highlight that, again, ethnic origin (F4) was the factor most sensitive to individual student improvement, similarly to the observation in relation to group improvement.
One could argue that ethnic origin (F4) may be considered a biological factor and that it should have been analysed from this perspective within our active learning methodology. However, consistently with the way in which the invisible care of a Maghrebi geriatric patient was approached in this study, the four scenarios of the storyboard focused more on the patient’s social–cultural characteristics (identity, tradition, religious beliefs and cultural practices) than on her biogenetic make-up linked to the concept of race. We therefore opted to view the variable “ethnic origin” in accordance with recent contributions to the field of health science [55,56].
Furthermore, the use of this methodology and its evaluation using the CCI-U questionnaire enabled us to identify specific areas of improvement in certain groups. This was the case, for example, with the Quality and Safety in Nursing Care subject and the invisible care of geriatric patients in accordance with their sex (F2). In this case, a sharp drop (<5 points) was observed in this invisible competence following the intervention and application of the active learning methodology in the 2021–2022 academic year. Since this was the nursing group with the most practical experience (third year of the degree course), it is possible that contents from another subject [57] or real experiences with immigrant women in hospital practicums [58] may have interfered with the methodology.
The aim of this study was not to compare IBL with traditional teaching but to improve the design and efficacy of IBL within the active learning methodology in order to achieve greater acquisition of competencies in the four areas of invisible care. After this experience, we will in the future directly apply the IBL method to all students without control groups. We understand that IBL promotes greater critical thinking [28] by giving greater visibility to invisible care in line with the SDGs. The present study has certain limitations. First, only 50% of the subjects were analysed across all three academic years, which precluded a longitudinal overview of the implementation of invisible care across all groups. Second, of the 12 groups analysed, only 3 had more than 30 participants and 4 had 20 or fewer. This lack of balance may have affected the results obtained in the Student’s t tests. Third, the groups analysed were studying subjects from different academic levels. This may have resulted in higher invisible care scores among students in later years.
Future research should strive to include native male geriatric patients in this type of active learning methodology in order to enable comparisons with their immigrant female counterparts. It is also important to verify the stability of the new CCI-U questionnaire in other countries and cultural contexts. Finally, a social desirability scale should also be included in order to control for this variable.
5. Conclusions
From the perspective of teaching innovation, the new CCI-U scale presented here focuses on the invisible care of geriatric patients in accordance with the precepts of the 2030 Agenda, exploring the “bridge” that exists between non-stereotypical attitudes and competences linked to invisible care. This active learning methodology is also suitable for use in other health professions (psychology, medicine, dentistry, etc.) as well as nursing and fits in well with the application of active learning methodologies in general.
The good functioning of the CCI-U and the active learning methodology applied has important implications in the field of health science since they can foster the invisible care of geriatric patients from university training onwards alongside its more technical counterpart, rendering this type of care visible. We are currently adapting the active learning methodology for invisible geriatric care to incorporate multidisciplinary care [8,9] and interdisciplinary teaching (IDT) [59], integrating students from nursing, psychology and dentistry degree courses into the intervention groups.
Author Contributions
Conceptualisation, A.O.-G. and A.I.-O.; methodology, M.S.D.M.; software, M.S.D.M.; validation, M.S.D.M., A.O.-G. and A.I.-O.; formal analysis, M.S.D.M.; investigation, M.S.D.M., A.O.-G. and A.I.-O.; resources, I.B.-E. and F.J.O.d.E.-D.; data curation, M.S.D.M. and A.G.-G.; writing—original draft preparation, M.S.D.M.; writing—review and editing, M.S.D.M. and A.G.-G.; visualisation, A.O.-G., A.I.-O. and F.J.O.d.E.-D.; supervision, M.S.D.M.; project administration, M.S.D.M. and F.J.O.d.E.-D.; funding acquisition, I.B.-E. All authors have read and agreed to the published version of the manuscript.
Funding
This research project was funded by the University of the Basque Country, Office of the Pro Vice-Chancellor for Educational Innovation, grant number IKDI3-21-04, and the APC was funded by the University of the Basque Country.
Institutional Review Board Statement
The study was approved by the ethics committee of the University of the Basque Country (CEISH M10_2021_278, date: 18 October 2021) for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, M.S.D.M.
Acknowledgments
We are immensely grateful to the health science students at the University of the Basque Country for their participation in this study. We also thank Diana Draper for translating the paper.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Response scale: (1) completely disagree, (2) mainly disagree, (3) partly disagree, (4) partly agree, (5) mainly agree and (6) completely agree.
(*) Reverse items.
- As older people age, it makes little sense to work on sensory stimulation. (*)
- When you work with older people, you realise how insignificant their sexuality is. (*)
- Since older people only have a limited time left to live, it is better to avoid talking to them about death and to focus instead on meaningless things. (*)
- Your professional relationship with older people improves if you treat them like children. (*)
- Given their greater life expectancy, it is reasonable for older women to expect a little more than older men when receiving treatment. (*)
- It is normal to treat older men and women differently, since they were brought up in that cultural model. (*)
- Mixing groups of older men and women in occupational activities (e.g., nursing homes, day centres or associations) brings nothing but problems. (*)
- A female <psychologist, nurse, dentist> will have more trouble establishing a good professional relationship with an older man than with an older woman. (*)
- It is best to keep a certain distance when dealing with older people suffering from depression or low mood. (*)
- Establishing an emotional connection with patients/residents is counterproductive. (*)
- You should avoid getting emotionally involved with older people who are terminally ill. (*)
- When dealing with older immigrants, you need to be more flexible and adapt the care you provide to their cultural idiosyncrasies.
- When treating older immigrants, it is important to learn how to identify the characteristics of different cultural groups.
- When assessing older immigrants, you need to be practical and not consider the possible influence of their religious beliefs on their current situation. (*)
- When dealing with older immigrants, it is more important to prescribe and ensure adhesion to treatments than to reason with them in accordance with their cultural origin. (*)
- When interviewing older immigrants, you should consider the possibility of their having a different concept of health/illness from the one we have.
- When assessing older immigrants, it is important to consider the possibility of communication problems arising between professional and patient.
References
- EUROSTAT-2020. Available online: https://ec.europa.eu/info/departments/eurostat-european-statistics_es (accessed on 1 June 2022).
- INE-2022. Available online: https://www.ine.es/dyngs/INEbase/es/categoria.htm?c=Estadistica_P&cid=1254735572981 (accessed on 1 June 2022).
- INE-2020. Available online: https://www.ine.es/dyngs/INEbase/es/categoria.htm?c=Estadistica_P&cid=1254735572981 (accessed on 1 June 2022).
- Ministerio de Sanidad-2019. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/docs/Plan_Integral_Alhzeimer_Octubre_2019.pdf (accessed on 1 June 2022).
- Alzheimer Europe, Dementia in Europe Yearbook 2019. Available online: https://www.alzheimer-europe.org/content/download/195515/1457520/file/FINAL%2005707%20Alzheimer%20Europe%20yearbook%202019.pdf (accessed on 1 June 2022).
- UN-2015. Available online: https://www.un.org/sustainabledevelopment/ (accessed on 1 June 2022).
- Agenda-2030. Available online: https://unstats.un.org/sdgs/metadata/?Text=&Goal=4&Target=4.7 (accessed on 1 June 2022).
- Reeves, S.; Perrier, L.; Goldman, J.; Freeth, D.; Zwarenstein, M. Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database Syst. Rev. 2013, 3, 1–43. [Google Scholar] [CrossRef] [PubMed]
- Lattuca, L.R.; Knight, D.; Bergom, I. Developing a Measure of Interdisciplinary Competence. Int. J. Eng. Educ. 2013, 29, 729–739. [Google Scholar] [CrossRef]
- Davies, M.; Devlin, M. Chapter I, Interdisciplinary higher education. In Interdisciplinary Higher Education: Perspectives and Practicalities; Davies, M., Devlin, M., Tight, M., Eds.; Emerald Group Publishing Limited: Bingley, UK, 2010; Volume 5, pp. 3–28. [Google Scholar]
- MacDonnell, C.P.; Rege, S.V.; Misto, K.; Dollase, R.; George, P. An introductory interprofessional exercise for healthcare students. Am. J. Pharm. Educ. 2012, 76, 154. [Google Scholar] [CrossRef] [PubMed]
- Colliere, M.F. Encontrar el sentido original de los cuidados enfermeros. Rev. ROL Enfermería 1999, 22, 27–31. [Google Scholar]
- Ausserhofer, D.; Zander, B.; Busse, R.; Schubert, M.; De Geest, S.; Rafferty, A.M.; Schwendimann, R. Prevalence patterns and predictors of nursing care left undone in European hospitals: Results from the multicountry cross-sectional RN4CAST study. BMJ Qual. Saf. 2014, 23, 126–135. [Google Scholar] [CrossRef]
- Aikien, L.H.; Sermeus, W.; Van den Heede, K.; Sloane, D.M.; Busse, R.; Mckee, M.; Kutney-Lee, A. Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012, 344, e1717. [Google Scholar] [CrossRef]
- Aikien, L.H.; Sloane, D.M.; Bruyneel, L.; Van den Heede, K.; Griffiths, P.; Busse, R.; Sermeus, W. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 2014, 383, 1824–1830. [Google Scholar] [CrossRef]
- Ball, J.E.; Bruyneel, L.; Aiken, L.H.; Sermeus, W.; Sloane, D.M.; Rafferty, A.M. Post-operative mortality, missed care and nurse staffing in nine countries: A cross-sectional study. Int. J. Nurs. Stud. 2018, 78, 10–15. [Google Scholar] [CrossRef]
- Feo, R.; Kitson, A. Promoting patient-centred fundamental care in acute healthcare systems. Int. J. Nurs. Stud. 2016, 57, 1–11. [Google Scholar] [CrossRef]
- Huercanos-Esparza, I. El cuidado invisible, una dimensión de la población enfermera. Bibl. Las Casas 2010, 6, 1–52. [Google Scholar]
- Allen, D. The Invisible Work of Nurses: Hospitals, Organisations and Healthcare; Routledge: London, UK, 2015. [Google Scholar]
- Wozniak, H.; Mahony, M.J.; Everingham, F.; Poulos, A.; Reid, B. Inquiry Based Learning in the Health Sciences: Countering the limitations of “Problem Based” Learning. Focus Health Prof. Educ. A Multi-Discip. J. 2005, 7, 18–30. [Google Scholar]
- Dellai, M.; Mortari, L.; Meretoja, R. Self-assessment of nursing competences—Validation of the Finnish NCS instrument with Italian nurses. Scand. J. Caring Sci. 2009, 23, 783. [Google Scholar] [CrossRef] [PubMed]
- Canzan, F.; Heilemann, M.V.; Salani, L.; Mortari, L.; Ambrosi, E. Visible and invisible caring in nursing from the perspectives of patients and nurses in the gerontological context. Scand. J. Caring Sci. 2014, 28, 732–740. [Google Scholar] [CrossRef] [PubMed]
- Chrisler, J.; Palatino, B. Ageism can be hazardous to women’s health: Ageism, sexism, and stereotypes of older women in the healthcare system. J. Soc. Issues 2016, 72, 86–104. [Google Scholar] [CrossRef]
- Chang, L.; Chen, S.C.; Hung, S.L. Embracing diversity and transcultural society through community health practicum among college nursing students. Nurse Educ. Pract. 2018, 31, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xiao, L.D.; Yasheng, A. Nursing students’ cultural competence in caring for older people in a multicultural and developing region. Nurse Educ. Today 2018, 70, 47–53. [Google Scholar] [CrossRef]
- Darbyshire, P.; McKenna, L. Nursing’s crisis of care: What part does nursing education own? Nurse Educ. Today 2013, 33, 305. [Google Scholar] [CrossRef]
- Aditomo, A.; Goodyear, P.; Bliuc, A.; Ellis, R. Inquiry-based learning in higher education: Principal forms, educational objectives, and disciplinary variations. Stud. High. Educ. 2013, 38, 1239–1258. [Google Scholar] [CrossRef]
- Ellis, R.; Goodyear, P. Students’ experiences of e-learning in higher education. In The Ecology of Sustainable Innovation; Routledge: London, UK, 2010. [Google Scholar]
- Lavonen, J.; Lakksonen, S. Context of teaching and learning school science in Finland. Reflections on PISA 2006 results. J. Res. Sci. Teach. 2009, 46, 922–944. [Google Scholar] [CrossRef]
- Pastor-Duran, X.; Lozano-Rubí, R.; Gros-Salvat, B. El Aprendizaje Basado en la Indagación y el Codiseño. Experiencia Aplicada en el Grado de Ingeniería Biomédica; Ediciones Octaedro Sl: Barcelona, Spain, 2017. [Google Scholar]
- Polit, D.F.; Beck, C.T.; Owen, S.W. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health 2007, 30, 459–467. [Google Scholar] [CrossRef]
- Hambleton, R.K. Issues, designs and technical guidelines for adapting tests into multiple languages and cultures. In Adapting Educational and Psychological Tests for Cross-Cultural Assessment; Hambleton, R.K., Merenda, P.F., Spielberg, S.D., Eds.; Lawrence Erlbaum Associates, Inc.: Hillsdale, NJ, USA, 2005; pp. 3–38. [Google Scholar]
- Balluerka, N.; Gorostiaga, A.; Alonso-Arbiol, I.; Haranburu, M. Test adaptation to other cultures. Psicothema 2007, 19, 124–133. [Google Scholar] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Marsh, H.W.; Wen, Z.; Hau, K.T. Structural equation models of latent interactions: Evaluation of alternative estimation strategies and indicator construction. Psychol. Methods 2004, 9, 275–300. [Google Scholar] [CrossRef] [PubMed]
- Nunnally, J.C.; Bernstein, I.H. The Assessment of Reliability. Psychom. Theory 1994, 3, 248–292. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modelling; The Gilford Press: New York, NY, USA, 2005. [Google Scholar]
- Huercanos-Esparza, I.; Anton-Solanas, I.; Orkaizagirre-Gomara, A.; Ramon-Arbues, E.; German-Bes, C. Measuring invisible nursing interventions: Development and validation of Perception of Invisible nursing Care-Hospitalisation questionnaire (PINC-H) in cancer patients. Eur. J. Oncol. Nurs. 2021, 50, 101888. [Google Scholar] [CrossRef] [PubMed]
- Larson, P.; Ferketich, S. Patients’ satisfaction with nurses’ caring during hospitalization. West. J. Nurs. Res. 1993, 15, 690–707. [Google Scholar] [CrossRef]
- Urcola-Pardo, F.; Ruiz de Viñaspre, R.; Orkaizagirre-Gomara, A.; Jiménez-Navascués, L.; Anguas-Gracia, A.; Germán-Bes, C. La escala CIBISA: Herramienta para la autoevaluación del aprendizaje práctico de estudiantes de enfermería. Index Enfermería 2017, 26, 226–230. [Google Scholar]
- North, M.S.; Fiske, S.T. An inconvenienced youth? Ageism and its potential intergenerational roots. Psychol. Bull. 2012, 138, 982–997. [Google Scholar] [CrossRef]
- Travis, C.B.; Howerton, D.M.; Szymanski, D.M. Risk, uncertainty, and gender stereotypes in healthcare decision. Women Ter. 2012, 35, 207–220. [Google Scholar] [CrossRef]
- Bristow, N.K. American Pandemic: The Lost Worlds of the 1918 Influenza Epidemic; Oxford University Press: New York, NY, USA, 2012. [Google Scholar]
- Iver, P.; Aziz, K.; Ojcius, D.M. Impact of COVID-19 on dental education in the United States. J. Dent. Educ. 2020, 84, 718–722. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, P.; Wolf, M. The Impact of COVID-19 on the undergraduate medical curriculum. Med. Educ. Online 2020, 25, 1764740. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.; Greenberg, J.; Pyszczynski, T. The Worm at the Core: On the Role of Death in Life; Random House: New York, NY, USA, 2015. [Google Scholar]
- Vina, J.; Lloret, A. Why women have more Alzheimer’s disease that men: Gender and mitochondrial toxicity of amyloid-beta peptide. J. Alzheimer’s Dis. 2010, 20, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Deschodt, M.; Diercks de Casterlé, B.; Milisen, K. Gerontological care in nursing education programs. J. Adv. Nurs. 2010, 66, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Rhee, T.G.; Marottoli, R.A.; Van Ness, P.H.; Levy, B.R. Impact of perceived racism on Healthcare Access among older minority adults. Am. J. Prev. Med. 2019, 56, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Sabin, J.A.; Rivara, F.P.; Greenwald, A.G.; Rivara, F.P. Physician implicit and explicit attitudes about race by MD race, ethnicity, and gender. J. Health Care Poor Underserved 2009, 20, 896–913. [Google Scholar] [CrossRef]
- Sabin, J.A.; Rivara, F.P.; Greenwald, A.G. Physician implicit attitudes and stereotypes about race and quality of medical care. Med. Care 2008, 46, 678–685. [Google Scholar] [CrossRef]
- Shelley, I. White-means, racial patterns in disabled elderly persons’ use of medical services. J. Gerontol. Ser. B 2000, 55, 76–89. [Google Scholar] [CrossRef]
- Ulusoy, N.; Schablon, A. Discrimination in Patient Geriatric Care: A Qualitative study on the experiences of employees with a Turkish migration background. Int. J. Environ. Res. Public Health 2020, 17, 2205. [Google Scholar] [CrossRef]
- Afshari, R.; Bhopal, R. Changing pattern of use of ethnicity and race in scientific literature. Int. J. Epidemiol. 2002, 31, 1074–1076. [Google Scholar] [CrossRef][Green Version]
- Vanegas, L.J.; Villalón, C.M.; Valenzuela, Y.C. Consideraciones acerca del uso de la variable etnia/raza en la investigación epidemiológica para la Salud Pública: A propósito de investigaciones en inequidades. Rev. Med. Chile 2008, 136, 637–644. [Google Scholar] [CrossRef][Green Version]
- Robinson, S.; Brigs, R.; O’Neill, D. Cognitive aging, geriatric textbooks, and unintentional ageism. J. Am. Geriatr. Soc. 2012, 60, 2183–2185. [Google Scholar] [CrossRef] [PubMed]
- Gullette, M.M. Age Wise: Fighting the New Ageism in America; University of Chicago Press: Chicago, IL, USA, 2004. [Google Scholar]
- Liu, H.Y.; Hsu, D.Y.; Han, H.M.; Wang, I.T.; Chen, N.H.; Han, C.Y.; Wu, S.M.; Chen, H.F.; Huang, D.H. Effectiveness of interdisciplinary teaching on creativity: A quasi-experimental study. Int. J. Environ. Res. Public Health 2022, 19, 5875. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).