Towards Co-Design in Delivering Assistive Technology Interventions: Reconsidering Roles for Consumers, Allied Health Practitioners, and the Support Workforce
Abstract
1. Introduction
1.1. Supercomplex Environments and Allied Health Professions
Assistive Technology—A Key Intervention for Many Allied Health Professions
1.2. The Australian Context
2. Method
2.1. Step 1: Recruit Expert Panel
2.2. Step 2: Identify Key Constructs
Existing Frameworks Relevant to Co-Design of AT Interventions
2.3. Step 3: Develop AT Collaboration Tool
2.4. Step 4: Pilot AT Collaboration Tool
2.5. Step 5: Review and Revise AT Collaboration Tool
3. Results
3.1. Data Sources
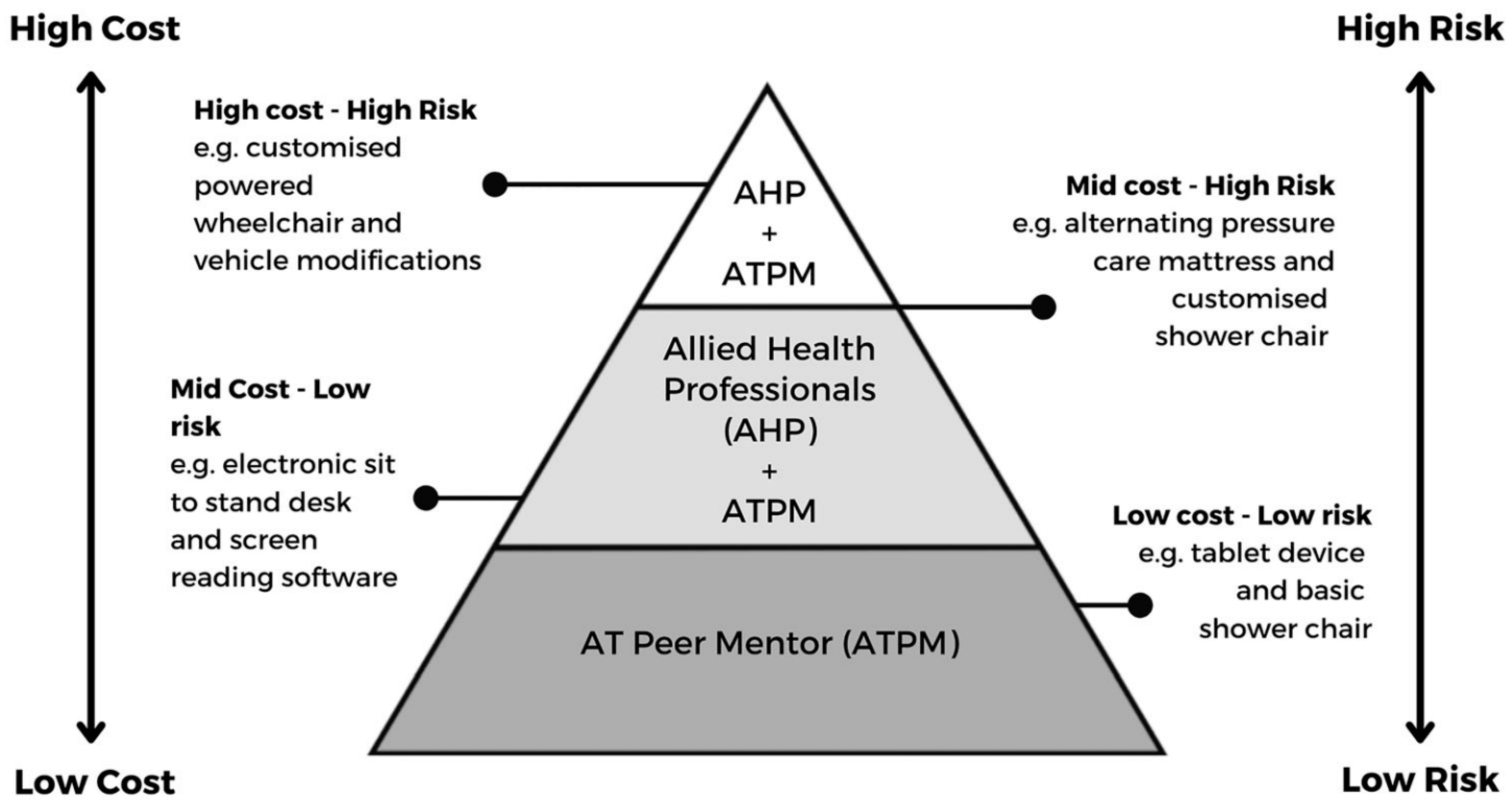
3.1.1. AT Stakeholders
- AT user and support network;
- disability support worker/peer supporter;
- allied health practitioner;
- team (multidisciplinary or interdisciplinary).
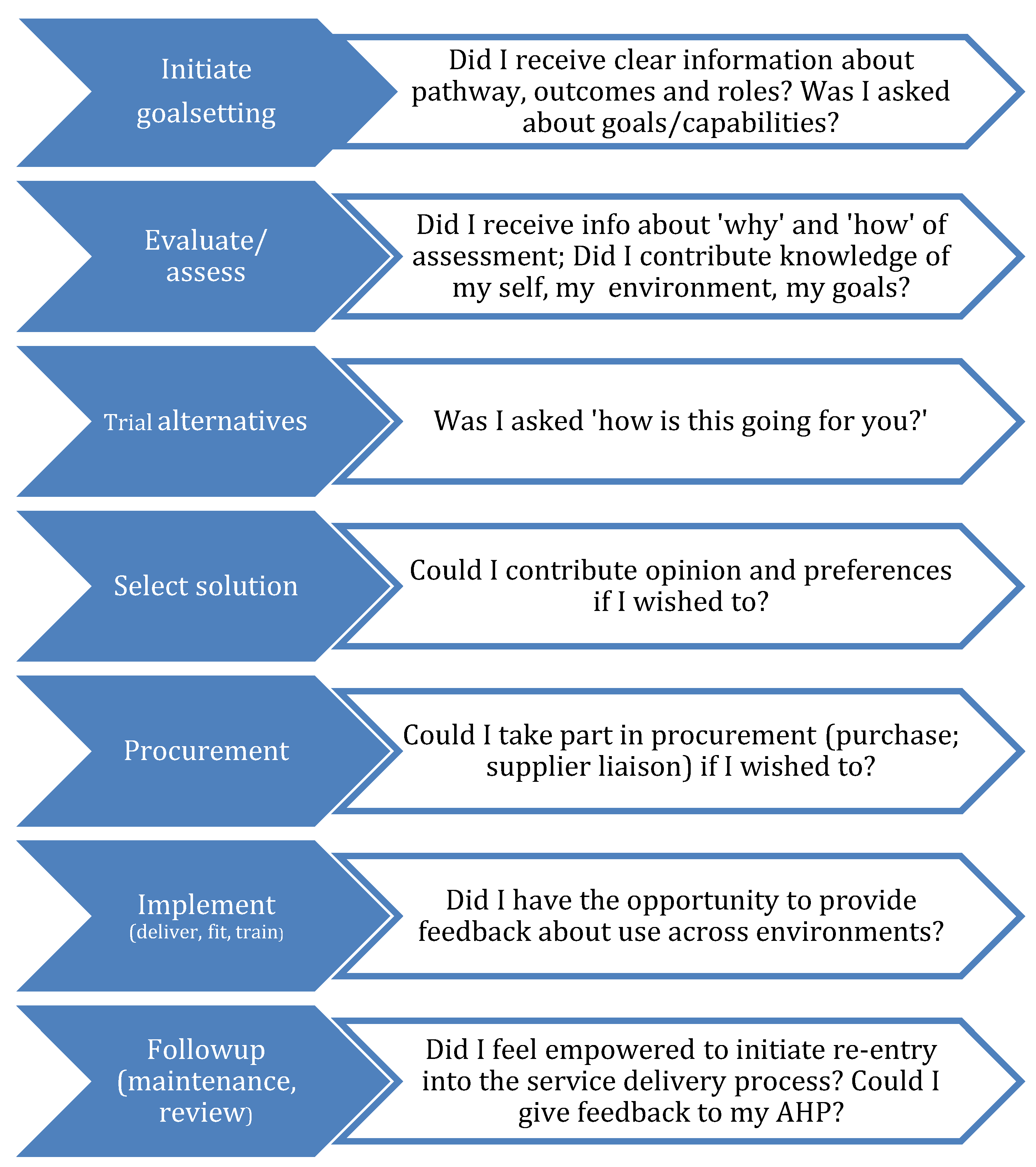
3.1.2. AT Service Delivery Steps
3.1.3. Competence
4. Discussion
5. Limitations and Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A. Assistive Products Level 1 Categories from AS/ISO:9999: 2018 and AHPs
| AS/ISO 9999 Classes of Assistive Products [21] | AHPs Scope * |
| 04 Assistive products for measuring, supporting, training or replacing body functions (examples: respiratory and circulatory support products; medication management systems; feeding pumps, accessories for parenteral (intravenous) feeding) |
|
| 05 Assistive products for education and for training in skills (examples: Assistive products for training alternative communication techniques and vocabulary to allow interpersonal communication; continence training products; memory training products) |
|
| 06 Assistive products attached to the body for supporting neuromusculoskeletal or movement related functions (orthoses) and replacing anatomical structures (prostheses) (examples: supportive footwear; upper limb splints, lower limb prosthesis) |
|
| 09 Assistive products for self-care activities and participation in self-care (examples: adapted clothing; shower stool; belts and harnesses; positioning supports; products for tracheostomy care; continence products) |
|
| 12 Assistive products for activities and participation relating to personal mobility and transportation (examples: walking aids; wheelchairs; vehicle adaptations; transfer supports; mobile hoists) |
|
| 15 Assistive products for domestic activities and participation in domestic life (examples: adapted cutting board; one-handed chopping equipment; wheeled laundry basket; long handled gardening equipment) |
|
| 18 Furnishings, fixtures and other assistive products for supporting activities in indoor and outdoor human-made environments (examples rise/recline lounge chair; adjustable bed; fold down grabrails; portable ramps) |
|
| 22 Assistive products for communication and information management (examples: assistive products for voice production; hearing loops; electronic communication devices; adapted computer mouse) |
|
| 24 Assistive products for controlling, carrying, moving and handling objects and devices (examples: environmental control units for operating devices from a distance; assistive products for extended reach; forearm support for computer use; robotic manipulator; non-slip products) |
|
| 27 Assistive products for controlling, adapting or measuring elements of physical environments (examples: air filters; products for reducing vibration; lighting management products; noise cancelling headphones) |
|
| 28 Assistive products for work activities and participation in employment (examples: workstations; lifting platforms; adapted tools; occupational health and safety products such as alarms and monitors) |
|
| 30 Assistive products for recreation and leisure (examples: adapted saddles; sports wheelchairs; one handed playing card holders) |
|
| * Focussing on AHPs Who Recommend Assistive Products. | |
Appendix B. Dietetics: Co-Design in Home Enteral Nutrition (HEN)
| Person/Circle of Support 1 | Disability Support Worker 2 | Nurse or Accredited Practising Dietitian (APD) | Accredited Practising Dietitian (APD) | Multidisciplinary Team |
| Deliver feed by pump, gravity or syringe | Deliver feed by pump, gravity or syringe | Care of enteral feeding tube and tube replacement depending on type of tube and skill level | Assessing and continued monitoring of nutritional requirements | |
| Basic trouble shooting | Basic trouble shooting | Monitor for complications related to the tube or feeding | Nutrition goals determined in collaboration with participant and evidence base eg nutrient reference values (NRV) | Assessment of ability to take oral diet and need for enteral nutrition |
| Basic care of enteral feeding tubes/devices and gastrostomy site | Basic care of enteral feeding tubes/devices and gastrostomy site | Training and support for patients, carer and/or disability support workers to ensure adequate skill level to provide tube care and feeding | Recommending formula, route of administration and regimen. | Insertion of enteral tube, tube changes (depending on type of tube) and management of complications |
| Know when to call for additional help | Know when to call for additional help | Trouble shooting | ||
| Source information on accessing HEN products (selection of pump, delivery method) | Recommend balance between oral intake and enteral nutrition to meet nutrition requirements and agreed nutrition goals | |||
| Active participant in decisions around HEN management | Ongoing monitoring and evaluation against nutrition goals (this includes support to achieve goals), and monitoring for nutrition-related complications | Access to specialist services to address tube and feeding complications as required | ||
| Provision of information /prescription for accessing HEN products (feeds, pumps, giving sets, delivery method). Ensuring patient has a valid registration to order feeds and equipment. Liaising with patient, carer, disability support worker and nursing for any changes to feeding regimen | ||||
| Quality measures for each stakeholder: | ||||
| Up-to-date and ongoing AT training. Can clearly outline who to contact when assistance is needed. | Appropriate qualification. Up-to-date and ongoing training Operating within scope of practice. Regular monitoring/audit of complication rates. | Appropriate qualification. Up-to-date workplace training/credentialing/APD credentialing. Regular monitoring/audit of complication rates. | APD credential. Participant satisfaction. Ensure client is achieving their nutrition goal. Follows Regulatory body code of conduct. APD operating within person centred model. | All members appropriate qualification & trained. Follows Regulatory body code of conduct. Regular case conferences. Operating within scope of practice. |
| 1 (i.e., NDIS participant with training. Currently being trained by APD and nurse; 2 Appropriately qualified (Certificate IV or III) with nutrition modules (ideally with a unit on HEN care which is not currently available). Current practice is that an APD with HEN experience and/or nurse train patients/carers/support workers. | ||||
Appendix C. Speech Pathology: Co-Design with Communication Devices
| Person/Circle of Support | Disability Support Worker | AT Supplier/AT Mentor | Speech Pathologist | Multidisciplinary Team |
| Identify need and preferences based on previous experiences | Follow communication plan developed by participant and speech pathologist | Organise and monitor adequate trial of the device/s, including training and programming of device as required | Complete thorough communication assessment across environments | Provide training to participant/support network and speech pathologist to position and access device appropriately as needed |
| Set goals for communication such as what a device might be used for | Basic troubleshooting | Assist with funding application as required | Assessment and tertiary consultation with other AHPs needed such as occupational therapist or physiotherapist for positioning and device access if appropriate | Receive training in using the device with the participant from speech pathologist or participant/support network depending on preference and/or skill level of participant/support network |
| Provide vocabulary list or communication dictionary | ||||
| Learn about the device or system and how to show others how to use it | ||||
| Basic programming and troubleshooting, depending on skill level and desire | Know when to contact others for repairs or support | Advanced training and troubleshooting support | Analysis of short- and long-term communication needs and factors leading to likely change in needs, including multi-modal approach | Use device to make sure participant is able to participate effectively in all environments |
| Provide feedback about what is working and what isn’t | Experience of what has worked for a range of other AT users | Programming and troubleshooting depending on skill level | ||
| Quality measures for each stakeholder: | ||||
| Provides feedback to therapist about satisfaction with device AT assists goal achievement Remains informed of options and use in manner decided on by participant Contacts speech pathologist/team members when assistance needed | Received training Regular updates to training Proactively seeks review, maintenance and adjustments Participates in informed discussions with all other stakeholders Uses AT as intended and appropriate Documents progress as appropriate Knows who to contact when assistance needed | Appropriate qualification Received training Regular updates to training Manufacturing standards and warranty requirements met and maintained AT quality checks prior to provision | Certified practising speech pathologist status Regular supervision Uses outcome measures to ensure person has met goals Follows Regulatory body code of conduct Operating within scope of practice | Appropriate qualification Received training Regular updates to training Manufacturing Follows Regulatory body code of conduct Regular case conferences Operating within scope of practice |
Appendix D. Prosthetics and Orthotics: Co-Design with a Custom Prosthesis
| Person/Circle of Support | Allied Health Assistant | Prosthetist | Technician/Manufacturer | Multidisciplinary (MD) Team |
| Set goals and share knowledge of environments of use | Assessment using relevant valid and reliable outcome measures as directed by the prosthetist and/or MD team to inform baseline assessment and progress toward goal achievement | Assessment of ability to use prosthesis in line with goals Determine goals in collaboration with participant based on outcome measure and assessment findings | Manufactures prosthesis as directed by Prosthetist according to applicable standards and instructions | Physiotherapist and/or Occupational Therapist provide education and training in use of AT, particularly within specific environments as well as care of whole self when using |
| Maintain AT | Provides person with and receives from others ongoing education and training in use as directed by prosthetist and/or MD team | Discuss advantages and disadvantages of all prosthesis options in line with evidence base | Sources required parts to be included in prosthesis | Assessment, discussion and provision as required of complementary AT |
| Use AT safely and within warranty requirements | Shared decision making regarding type of prosthesis to be used | Nursing/Podiatrist-wound management as required | ||
| Troubleshoot fit and use challenges independently and seek assistance as appropriate | Assists person to access financial support for AT and related services as required | |||
| Trial where possible and report subjective and objective feedback Research available options to enable informed discussion and choice regarding prosthetic parts | Ensure optimal fit, function and safety of prosthesis in an ongoing manner Provide education re use, care and maintenance requirements of AT in collaboration with MD Team, Allied Health Assistant and persons support network | Medical-access to specialist services and/or medications to enable use as required e.g. pain medication, mental health assistance, investigative measures | ||
| Informed of and able to share information related to payment options & preferences | ||||
| Quality measures for each stakeholder: | ||||
| Received training Regular updates to training Proactively remains informed of options and use Proactively seeks review, maintenance and adjustments Participates in informed discussions with all other stakeholders as preferred Uses AT as intended and appropriate AT assists goal achievement | Appropriate qualification Regular updates to training Operates within scope of practice Operates within person centred model | Appropriate qualification Operates within scope of practice Participates in continued learning, provides and receives supervision Remains aware of all AT options Integrates current evidence to practice Operates within person centred model Seeks feedback from all stakeholders Uses outcome measures to ensure person has met goals | Appropriate training and supervision Manufacturing standards and warranty requirements met and maintained AT quality checks prior to provision | Appropriate qualification Participates in continued learning, remains aware of all AT options, integrates current evidence to practice Operates within person centred model Operates within scope of practice Uses outcome measures to ensure person has met goals |
Appendix E. Occupational Therapy and Co-Design in Vehicle Modifications
| Person/Circle of Support | AT Supplier/Vehicle Modification Agent | Occupational Therapist |
| Goal identification and knowledge of environments of use | Goalsetting and establish outcomes | |
| Knowledge of transfer capacity | Assess participant [physical capacity; future needs; balance; reach range; endurance; cognition] | |
| Understanding of physical and organisational capacity | Assess environments of use [parking and driving clearances and distances; path of travel; transfer and handling implications of trailers, hoists and ramps] | |
| Source information on vehicle modification options | Knowledge regarding product options and vehicle ‘fit’ with range of products | |
| Envision the link between all these factors, when looking at available options on the market | ||
| Determine when to consult experts to determine the solution which will fit person, task and environment | Experience of what has worked for a range of other AT users | Task analysis [physical and cognitive demands of transfers to carseat; ambulating to ramp/trailer; handling of hardware] |
| Quality measures for each stakeholder: | ||
| Develop own experience-based knowledge of needs and potential solutions Learn how to utilise evidence based resources such as National Equipment Database Skilled in appraising products as a consumer ie familiar with pro and con evaluation; utilise consumer and fair trading resources. | No formal training/credentialing exists Maintains currency with market and modification technology | No formal training/credentialing exists May complete driver-related certificate course which partially covers competencies Participate in community of practice for vehicle modifications Engages in appropriate mentoring/supervision relationships to maintain currency of skill |
References
- Fortune, T.; Ryan, S.; Adamson, L. Transition to practice in supercomplex environments: Are occupational therapy graduates adequately prepared? Aust. Occup. Ther. J. 2013, 60, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Bickenbach, J.; Bigby, C.; Salvador-Carulla, L.; Heller, T.; Leonardi, M.; LeRoy, B.; Mendez, J.; Putnam, M.; Spindel, A. The Toronto Declaration on Bridging Knowledge, Policy and Practice in Aging and Disability; FICCDAT: Toronto, ON, Canada, 2012. [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organisation. International Classification of Health Interventions; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Prodinger, B.; Cieza, A.; Oberhauser, C.; Bickenbach, J.; Üstün, T.B.; Chatterji, S.; Stucki, G. Toward the International Classification of Functioning, Disability and Health (ICF) Rehabilitation Set: A Minimal Generic Set of Domains for Rehabilitation as a Health Strategy. Arch. Phys. Med. Rehabil. 2016, 97, 875–884. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Rehabilitation 2030: A Call for Action; World Health Organisation: Geneva, Switzerland, 2017. [Google Scholar]
- Academy of Medical Sciences. Stratified, Personalised or P4 Medicine: A New Direction for Placing the Patient at the Centre of Healthcare and Health Education; Academy of Medical Sciences, The University of Southampton, Science Europe and the Medical Research Council: Southampton, UK, 2015. [Google Scholar]
- Sackett, D.L.; Straus, S.E.; Richardson, W.S.; Rosenberg, W.; Haynes, R.B. Evidence-Based Medicine: How to Practice and Teach EBM; Churchill Livingston: London, UK, 2000; Volume 2. [Google Scholar]
- Hill, S. (Ed.) The Knowledgeable Patient: Communication and Participation in Health (A Cochrane Handbook); Wiley-Blackwell: Hoboken, NJ, USA, 2011. [Google Scholar] [CrossRef]
- National Health & Medical Research Council. Consumer Involvement. Available online: https://www.nhmrc.gov.au/guidelinesforguidelines/plan/consumer-involvement (accessed on 1 January 2022).
- Australian Commission on Safety and Quality in Health Care. Safety and Quality Improvement Guide Standard 2: Partnering with Consumers; ACSQHC: Sydney, Australia, 2012. [Google Scholar]
- Carr, S. Enabling risk and ensuring safety: Self-directed support and personal budgets. J. Adult Prot. 2011, 13, 122–136. [Google Scholar] [CrossRef]
- Laragy, C.; David, C.; Moran, N. A framework for providing information in individualised funding programmes. Qual. Soc. Work. 2015, 15, 190–208. [Google Scholar] [CrossRef]
- Dean, E.E.; Dunn, W.; Tomchek, S. Role of Occupational Therapy in Promoting Self-Determination Through Consumer-Directed Supports. Occup. Ther. Health Care 2015, 29, 86–95. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. WHO Global Strategy on People-Centred and Integrated Health Services: Interim Report. 2015. Available online: https://apps.who.int/iris/handle/10665/155002 (accessed on 1 January 2022).
- Rist, P.; Freas, D.; Maislin, G.; Stineman, M. Recovery from Disablement: What functional abilities do rehabilitation professionals value the most? Arch. Phys. Med. Rehabil. 2008, 89, 1600–1606. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shakespeare, T.; Iezzoni, L.I.; Groce, N.E. Disability and the training of health professionals. Lancet 2009, 374, 1815–1816. [Google Scholar] [CrossRef]
- Fleming, P.; McGilloway, S.; Hernon, M.; Furlong, M.; O’Doherty, S.; Keogh, F.; Stainton, T. Individualised funding interventions to improve health and social care outcomes for people with a disability: A mixed-methods systematic review. Campbell Syst. Rev. 2019, 3, e1008. [Google Scholar]
- Moskos, M.; Isherwood, L. Individualised funding and its implications for the skills and competencies required by disability support workers in Australia. Labour Ind. A J. Soc. Econ. Relat. Work. 2019, 29, 34–51. [Google Scholar] [CrossRef]
- Meltzer, A.; Davy, L. Opportunities to enhance relational wellbeing through the National Disability Insurance Scheme: Implications from research on relationships and a content analysis of NDIS documentation. Aust. J. Public Adm. 2019, 78, 250–264. [Google Scholar] [CrossRef]
- AS/ISO. ISO 9999 Assistive Products for Persons with Disability—Classification and Terminology; ISO: Geneva, Switzerland, 2018. [Google Scholar]
- de Witte, L.; Steel, E.; Gupta, S.; Ramos, V.D.; Roentgen, U. Assistive technology provision: Towards an international framework for assuring availability and accessibility of affordable high-quality assistive technology. Disabil. Rehabil. Assist. Technol. 2018, 13, 467–472. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. World Report on Disability; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Toro, M.L.; Eke, C.; Pearlman, J. The impact of the World Health Organization 8-steps in wheelchair service provision in wheelchair users in a less resourced setting: A cohort study in Indonesia. BMC Health Serv. Res. 2016, 16, 26. [Google Scholar] [CrossRef] [PubMed]
- Dowd, J.; MacLachlan, M.; Khasnabis, C.; Geiser, P. Towards a Core Set of Clinical Skills for Health-Related Community Based Rehabilitation in Low and Middle Income Countries. Disabil. CBR Incl. Dev. 2015, 26, 39. [Google Scholar] [CrossRef]
- Commonwealth of Australia. National Disability Insurance Scheme Act 2013; Commonwealth of Australia: Canberra, Australia, 2013. [Google Scholar]
- Australian Government. Aged Care (Living Longer Living Better) Act 2013; Federal Register of Legislation: Canberra, Australia, 2013. [Google Scholar]
- Steel, E.J. The Duplicity of Choice and Empowerment: Disability Rights Diluted in Australia’s Policies on Assistive Technology. Societies 2019, 9, 39. [Google Scholar] [CrossRef]
- NDIA. Operational Guideline Assistive Technology (Equipment, Technology and Devices); NDIA: Canberra, Australia, 2022. [Google Scholar]
- Foley, K.; Attrill, S.; McAllister, S.; Brebner, C. Impact of transition to an individualised funding model on allied health support of participation opportunities. Disabil. Rehabil. 2020, 43, 3021–3030. [Google Scholar] [CrossRef]
- DSS. NDIS Quality and Safeguarding Framework; Department of Social Services: Canberra, Australia, 2016. [Google Scholar]
- NDIS Quality and Safeguards Commission. NDIS Practice Standards: Skills Descriptors; NDIS: Geelong, Australia, 2021. [Google Scholar]
- World Health Organisation. Policy Brief: Access to Assistive Technology; GATE, Ed.; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/phi/implementation/assistive_technology/phi_gate/en/ (accessed on 1 January 2022).
- Desmond, D.; Layton, N.; Bentley, J.; Boot, F.H.; Borg, J.; Dhungana, B.M.; Gallagher, P.; Gitlow, L.; Gowran, R.J.; Groce, N.; et al. Assistive technology and people: A position paper from the first global research, innovation and education on assistive technology (GREAT) summit. Disabil. Rehabil. Assist. Technol. 2018, 13, 437–444. [Google Scholar] [CrossRef]
- Smith, E.M.; Gowran, R.J.; Mannan, H.; Donnelly, B.; Alvarez, L.; Bell, D.; Contepomi, S.; Ennion, L.; Hoogerwerf, E.-J.; Howe, T.; et al. Enabling appropriate personnel skill-mix for progressive realization of equitable access to assistive technology. Disabil. Rehabil. Assist. Technol. 2018, 13, 445–453. [Google Scholar] [CrossRef]
- CAHE Review Team. Literature Review: Supporting the Transition of Allied Health Professionals to Remote and Rural Practice; Centre for Allied Health Evidence: Canberra, Australia, 2007. [Google Scholar]
- Watterson, D.; Walter, K.; O’Brien, L.; Terrill, D.; Philip, K.; Swan, I.; Somerville, L. Trans-disciplinary advanced allied health practitioners for acute hospital inpatients: A feasibility study. Int. J. Qual. Health Care 2019, 31, 103–109. [Google Scholar] [CrossRef]
- De Jonge, D.; Layton, N.; Vickery, F. Keynote Address A fresh analysis of the AT system in Australia: Listening to and understanding the perspectives of stakeholders in order to meet AT users expectations. In Proceedings of the NSW ILC Conference, Independent Living Centre Parramatta, Sydney, Australia, 25 November 2009. [Google Scholar]
- De Jonge, D.; Layton, N.; Vicary, F.; Steel, E. Motivations and incentives: Exploring assistive technology service delivery from the perspectives of multiple stakeholders. In Proceedings of the RESNA 2015: New Frontiers in Assistive Technology, Denver, CO, USA, 19 August 2015. [Google Scholar]
- De Jonge, D.; Hoyle, M.; Layton, N.; Verdonck, M. The Occupational Therapist: Enabling Activities and Participation Using Assistive Technology. In Assistive Technology Assessment Handbook; Scherer, F., Ed.; CRC Press: Boca Raton, FL, USA, 2017; pp. 211–234. [Google Scholar]
- Australian Skills Quality Authority. Certificate IV in Allied Health Assistance. Available online: https://www.training.com.au/ (accessed on 1 January 2022).
- World Health Organisation. Community Based Rehabilitation Guidelines; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Winchcombe, M.; Ballinger, C. A Competence Framework for Trusted Assessors; Assist UK, in Partnership with: The College of Occupational Therapists; The Chartered Society of Physiotherapy; The Disabled Living Foundation; The Royal National Institute of the Blind; The Royal National Institute for Deaf People: Manchester, UK, 2005. [Google Scholar]
- Long, S.; Banes, D.; O’Donnell, J.; Richardson, P. Introducing an AT Passport: A Key to Managing Transitions across the Lifespan Studies. Stud. Health Technol. Inform. 2017, 242, 76–77. [Google Scholar]
- Summers, M.; Walker, L. Options Paper for a National Accreditation System for Assistive Technology Prescribers and Suppliers; ATSA: Parramatta, Australia, 2013. [Google Scholar]
- Layton, N.; Walker, L. Assistive Technology Capability Framework. In Proceedings of the GREAT Summit, Geneva, Switzerland, 3–4 August 2017. [Google Scholar]
- National Disability Insurance Agency. Assistive Technology Strategy; NDIA: Canberra, Australia, 2013. [Google Scholar]
- Australian Healthcare Associates. Review of Assistive Technology Programs in Australia: Final Report and Supplementary Technical Report for the Australian Government Department of Health; Department of Health: Canberra, Australia, 2020. [Google Scholar]
- Independent Living Assessment. Assistive Technology Essentials: Part 1 An Introduction to Low Risk Assistive Technology for Commonwealth Home Support Programme Service Providers; Independent Living Assessment: Perth, Australia, 2021. [Google Scholar]
- Layton, N.; Harper, K.; Martinez, K.; Berrick, N.; Naseri, C. Co-creating an assistive technology peer-support community: Learnings from AT Chat. Disabil. Rehabil. Assist. Technol. 2021, 1–7. [Google Scholar] [CrossRef]
- Davies, S. Embracing reflective practice. Educ. Prim. Care 2012, 23, 9–12. [Google Scholar] [CrossRef] [PubMed]

| Profession | Clinical Experience | Practice Setting | Role | Years |
|---|---|---|---|---|
| Occupational Therapist | Health Disability Ageing | Public/Private/Non-profit Practitioner association/regulator Academic research centre Tertiary education/vocational education Australia/International | Clinical Managerial Policy Research Support roles | 35 |
| Prosthetist/ Orthotist | Health Disability Ageing | Public/Private Australia/International Practitioner association/regulator | Clinical Managerial Policy Research AT user/Consumer | 21 |
| Speech Pathologist | Health Disability Ageing | Public/Private/Non-profit Practitioner association/regulator Australia/International | Clinical Managerial Policy Research Support roles AT user/Consumer | 19 |
| Dietitian | Health | Public Academic research centre Tertiary education/vocational education Australia/International | Clinical Managerial Policy Research Education | 23 |
| AT Stakeholder Roles | ||||
|---|---|---|---|---|
| AT User and Support Network | Disability Support Worker/Peer Supporter | Allied Health Practitioner | Team | |
| AT Service Delivery Step | ||||
|
|
|
|
|
| Quality measures for each stakeholder | ||||
| e.g., formal/informal advocacy training; other training | e.g., appropriate workplace credential | e.g., recognised academic training; evidence-based practice, continuing practitioner development, practicing within personal and practitioner scope | e.g., clinical practice, outcome measures guideline adherence | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Layton, N.; O’Connor, J.; Fitzpatrick, A.; Carey, S. Towards Co-Design in Delivering Assistive Technology Interventions: Reconsidering Roles for Consumers, Allied Health Practitioners, and the Support Workforce. Int. J. Environ. Res. Public Health 2022, 19, 14408. https://doi.org/10.3390/ijerph192114408
Layton N, O’Connor J, Fitzpatrick A, Carey S. Towards Co-Design in Delivering Assistive Technology Interventions: Reconsidering Roles for Consumers, Allied Health Practitioners, and the Support Workforce. International Journal of Environmental Research and Public Health. 2022; 19(21):14408. https://doi.org/10.3390/ijerph192114408
Chicago/Turabian StyleLayton, Natasha, Jackie O’Connor, Amy Fitzpatrick, and Sharon Carey. 2022. "Towards Co-Design in Delivering Assistive Technology Interventions: Reconsidering Roles for Consumers, Allied Health Practitioners, and the Support Workforce" International Journal of Environmental Research and Public Health 19, no. 21: 14408. https://doi.org/10.3390/ijerph192114408
APA StyleLayton, N., O’Connor, J., Fitzpatrick, A., & Carey, S. (2022). Towards Co-Design in Delivering Assistive Technology Interventions: Reconsidering Roles for Consumers, Allied Health Practitioners, and the Support Workforce. International Journal of Environmental Research and Public Health, 19(21), 14408. https://doi.org/10.3390/ijerph192114408