Abstract
A diagnosis of an autism spectrum condition (autism) provides limited information regarding an individual’s level of functioning, information key in determining support and funding needs. Using the framework introduced by Arksey and O’Malley, this scoping review aimed to identify measures of functioning suitable for school-aged children on the autism spectrum and evaluate their overall utility, including content validity against the International Classification of Functioning, Disability and Health (ICF) and the ICF Core Sets for Autism. The overall utility of the 13 included tools was determined using the Outcome Measures Rating Form (OMRF), with the Adaptive Behavior Assessment System (ABAS-3) receiving the highest overall utility rating. Content validity of the tools in relation to the ICF and ICF Core Sets for Autism varied, with few assessment tools including any items linking to Environmental Factors of the ICF. The ABAS-3 had the greatest total number of codes linking to the Comprehensive ICF Core Set for Autism while the Vineland Adaptive Behavior Scales (Vineland-3) had the greatest number of unique codes linking to both the Comprehensive ICF Core Set for Autism and the Brief ICF Core Set for Autism (6–16 years). Measuring functioning of school-aged children on the spectrum can be challenging, however, it is important to accurately capture their abilities to ensure equitable and individualised access to funding and supports.
1. Introduction
Autism spectrum conditions (hereinafter autism, aligning with the preferred language of the autistic community [1]) encompass a range of persistent neurodevelopmental outcomes, primarily characterised by altered social communication and social interaction behaviours, along with the presence of restricted or repetitive behaviours or interests [2,3]. According to these diagnostic criteria outlined in both the latest version of the Diagnostic and Statistical Manual of Mental Disorders [3] and the International Classification of Diseases [2], these traits must also have a considerable impact on an individual’s ability to function in educational, family, occupational, personal, social and/or other important domains and contexts [2,3]. Restrictions within these contexts can result in reduced social outcomes for children on the autism spectrum when compared to their peers [4]. Globally, the rate of autism diagnoses is increasing, with an estimated rate of at least 1 in 100 children diagnosed with autism [5,6], with the highest prevalence of autism seen among school-aged children [6,7].
During the school years, children spend a significant amount of time with their peers and are heavily influenced by their interactions with others. For young people on the spectrum, establishing and maintaining peer support networks may be hindered by their social and communication challenges [4], limiting their ability to develop the skills required to successfully navigate important developmental stages. In addition, school-aged children are driven to acquire complex competencies and develop independence across various areas of functioning, integrating their sense of self [8]. Given that impaired functioning is associated with an autism diagnosis, it is important to ensure that children on the spectrum are provided with sufficient supports to maximise their potential during their development.
In 2013, the Australian Government launched the National Disability Insurance Scheme (NDIS) following an inquiry into the previous disability support system, identifying the need for systemic change to improve outcomes for people with disabilities, including autism [9]. Delivered by the National Disability Insurance Agency (NDIA), the NDIS aspires to increase independence and promote social and economic engagement of individuals with significant and permanent disability by funding reasonable and necessary supports and services [10]. A substantial portion (65%) of children aged between seven and 14 who are currently accessing the NDIS are diagnosed with autism [11]. However, diagnosis alone provides limited information regarding an individual’s functioning and support needs which can vary significantly between individuals [12]. Therefore, the Australian guideline on autism assessment and diagnosis recommends that individuals on the spectrum receive a comprehensive needs assessment, including an assessment of functioning, to determine the level of support they require to participate effectively in their daily lives [13]. This approach aligns with other international guidelines that recommend assessment of functioning, including strengths, skills, impairments and needs, occurs across multiple contexts such as at home and at school [14,15,16].
Functioning, as it relates to health, is defined by the World Health Organization (WHO) [17] as “an umbrella term for body functions, body structures, activities and participation. It denotes the positive aspects of the interaction between an individual (with a health condition) and that individual’s contextual factors (environmental and personal factors)” (p. 8). The WHO’s framework for measuring health and disability, known as the International Classification of Functioning, Disability and Health (ICF), is a biopsychosocial model that can be used to organise information relating to functioning and disability [17]. Although useful for classifying information across the categories of Body Functions, Activities and Participation, and Environmental Factors, the comprehensiveness of the framework limits it’s utility in clinical settings [18]. However, recent publications suggest that the ICF can be used as a framework to guide the diagnostic and assessment process, in capturing the holistic nature of functioning and accounting for variability across contexts [13,19].
Despite recognising the importance of assessing functioning associated with autism, there is to date no universally accepted measure designed to assess the unique functional strengths and challenges of children on the spectrum [20]. At an individual level, understanding functioning is essential to planning and providing supports. The school years are a critical period of development, during which children are expected to comply with the demands and expectations of the classroom environment as well as in variable social contexts [21]. A benefit of the ICF is that it takes into account the unique environmental factors impacting a child’s functioning [17]. As highlighted by Bronfenbrenner’s bioecological theory, children develop and function across multiple contexts or ‘systems’, ranging from their immediate environments (microsystems) through to the broader contexts of society and culture (macrosystems) [21]. Understanding the functional impacts of autism across contexts is key in ensuring children have adequate opportunities to challenge themselves and develop their own identities. More broadly, understanding the functioning of individuals on the spectrum is important in developing and managing models of service delivery, allocating funding, and measuring support needs at a population level.
Previous research investigating the psychometric properties of measures has focused on younger children, up to the age of six [22], likely due to the emphasis on early assessment and intervention in autism. Other reviews of measures applicable for school-aged children on the spectrum focus on screening [23,24] and diagnostic measures [25]. However, given the shift towards assessing functioning alongside or within the diagnostic assessment process, there is a need to understand the utility of measures of functioning across age groups.
The Outcome Measures Rating Form (OMRF) [26] is a tool for evaluating the overall utility of outcome measures. The OMRF documents the focus of the measure, clinical utility, scale construction, standardisation, reliability, and validity. The overall utility of a measure is determined according to ease of availability, quality of psychometric properties, and level of clinical utility [26]. Clinical utility has been further conceptualised as consisting of four main components: (1) appropriate, including effectiveness and relevance; (2) accessible, including resource implications and procurement; (3) practicable, including functionality, suitability, and training or knowledge required; and (4) acceptable, from the perspective of clinicians, clients and society [27]. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) is an initiative aiming to improve the selection of health measurement instruments by facilitating evaluation of their content and measurement properties [28]. The COSMIN refers to three main quality domains: (1) reliability; (2) validity; and (3) responsiveness.
Content validity refers to how accurately the content of an instrument reflects the construct it intends to measure [29]. Validity is often measured indirectly using methods such as Rasch, factor analysis, or Item Response Theory; however, these methods alone may be limited in determining an instrument’s true validity [30]. Derived from the extensive ICF framework and developed using a rigorous, multi-phase research process with international data collection, the ICF Core Sets for Autism have established content validity and are well placed in providing a reference point in determining the content validity of existing measures evaluating the functioning in this population [31,32].
This review aimed to evaluate the overall utility of existing assessment of functioning measures suitable for assessing school-aged children on the spectrum. Research objectives included: identifying appropriate tools, investigating the components of overall utility using the OMRF [26] and determining their content validity against the ICF Core Sets for Autism [20]. This review provides a unique contribution to the current body of literature investigating measures of functioning in autism, summarising their overall utility, as well as providing new evidence highlighting their content validity for school-aged children on the spectrum. This review is expected to provide both an overview of the measures currently available to assess functioning in this age group, and guide clinicians when evaluating the suitability of existing measures for use with school-aged children, ranging between six and 16 years, on the spectrum.
2. Materials and Methods
2.1. Study Design
Scoping reviews can be used to explore a topic and synthesise the findings of existing research, identifying gaps in the current literature [33]. This review adopted the scoping review framework introduced by Arksey and O’Malley [33] and later refined by Levac et al. [34] and Daudt et al. [35]. The Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) is a checklist that was developed based on these existing frameworks to provide further clarity in reporting requirements of scoping reviews [36]. The scoping review framework and PRISMA-ScR were initially utilised to identify existing measures of functioning for school-aged children on the spectrum, then to evaluate their overall utility based on relevant research articles. This review undertook the following steps: (1) identifying the research question; (2) identifying relevant measures and studies; (3) selecting studies; (4) charting the data (including a methodological assessment of quality); and (5) collating, summarising, and reporting the results [33,34,35,36].
2.2. Identifying Relevant Tools and Studies
Scoping search strategies typically involve searching multiple sources, including both published and grey literature, to obtain a broad overview of relevant existing literature [34]. Since functioning is a broad concept that can be broken down into individual (e.g., body functions, body structures, activities) and contextual components (e.g., personal and environmental factors), the literature search was conducted in two phases: (1) search for relevant measures of functioning; and (2) search for studies evaluating the utility of those measures.
2.2.1. Phase One
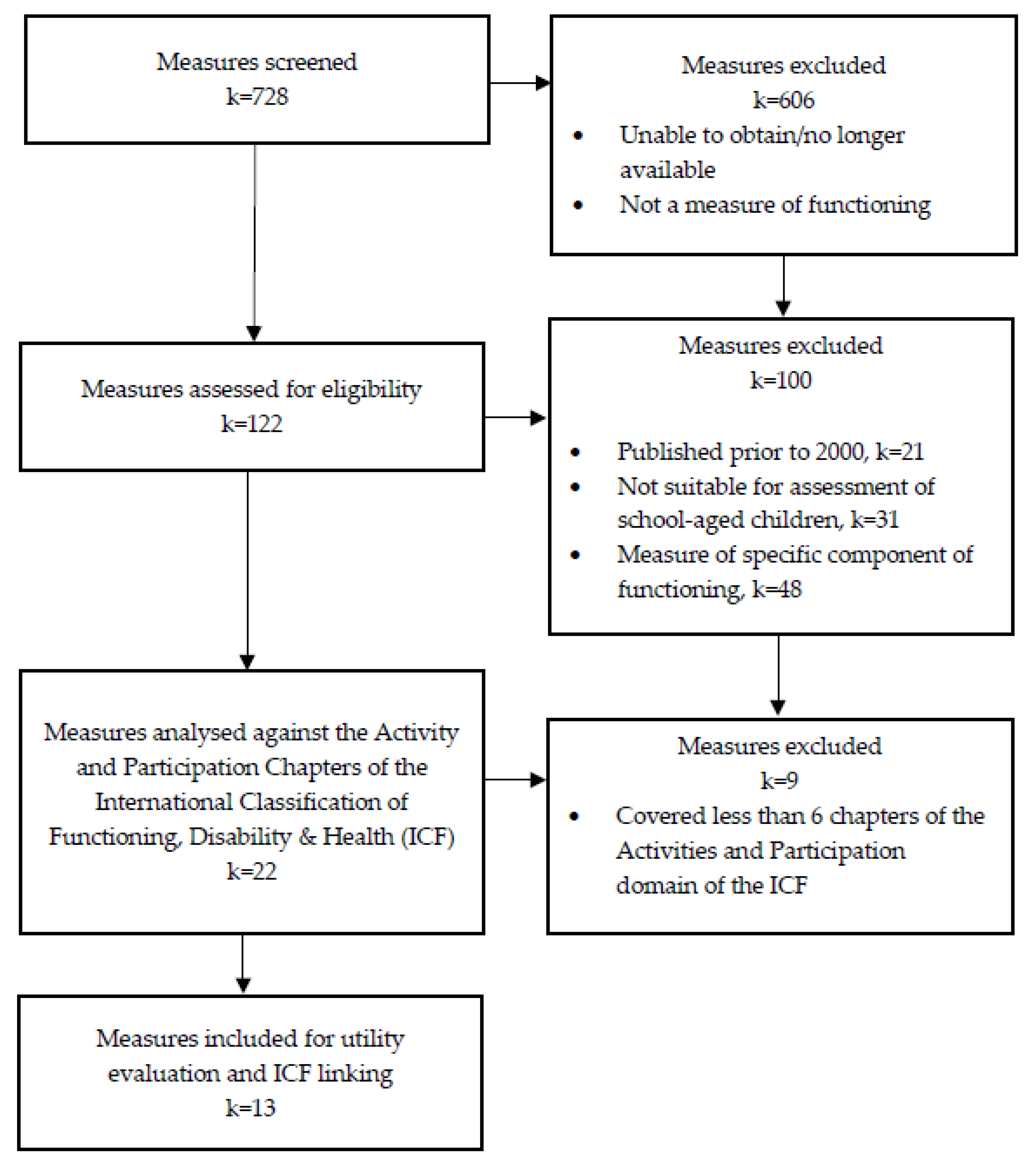
Measures were initially identified via internet searches, including Google, websites of major publishers (e.g., Pearson and Acer), reference books, catalogues of measures, and consultation with clinicians involved in assessing the functioning of individuals with neurodevelopmental conditions (Figure 1). Measures were eligible for inclusion in the review if they were: (1) available in English; (2) reflected at least six of the nine chapters included in the Activities and Participation domain of the ICF, to ensure inclusion of measures broadly assessing functioning; (3) were appropriate for use with individuals aged between six and 16 years, including measures that assessed either all or part of that range; and, (4) were published between January 2000 and June 2022. This timeframe was selected to ensure only the most recent versions of measures were included, aligning with current evidence-based practices. Measures were excluded if they: (1) only measured functioning in a specific population outside of neurodevelopmental conditions; (2) primarily measured impairment associated with a specific health condition (i.e., diagnostic tools); (3) had been superseded by a more recent version; or, 4) were no longer available online and/or in print. A shortlist of relevant measures was determined by two reviewers, guided by these criteria.
Figure 1.
Phase One, study identification and screening process.
2.2.2. Phase Two
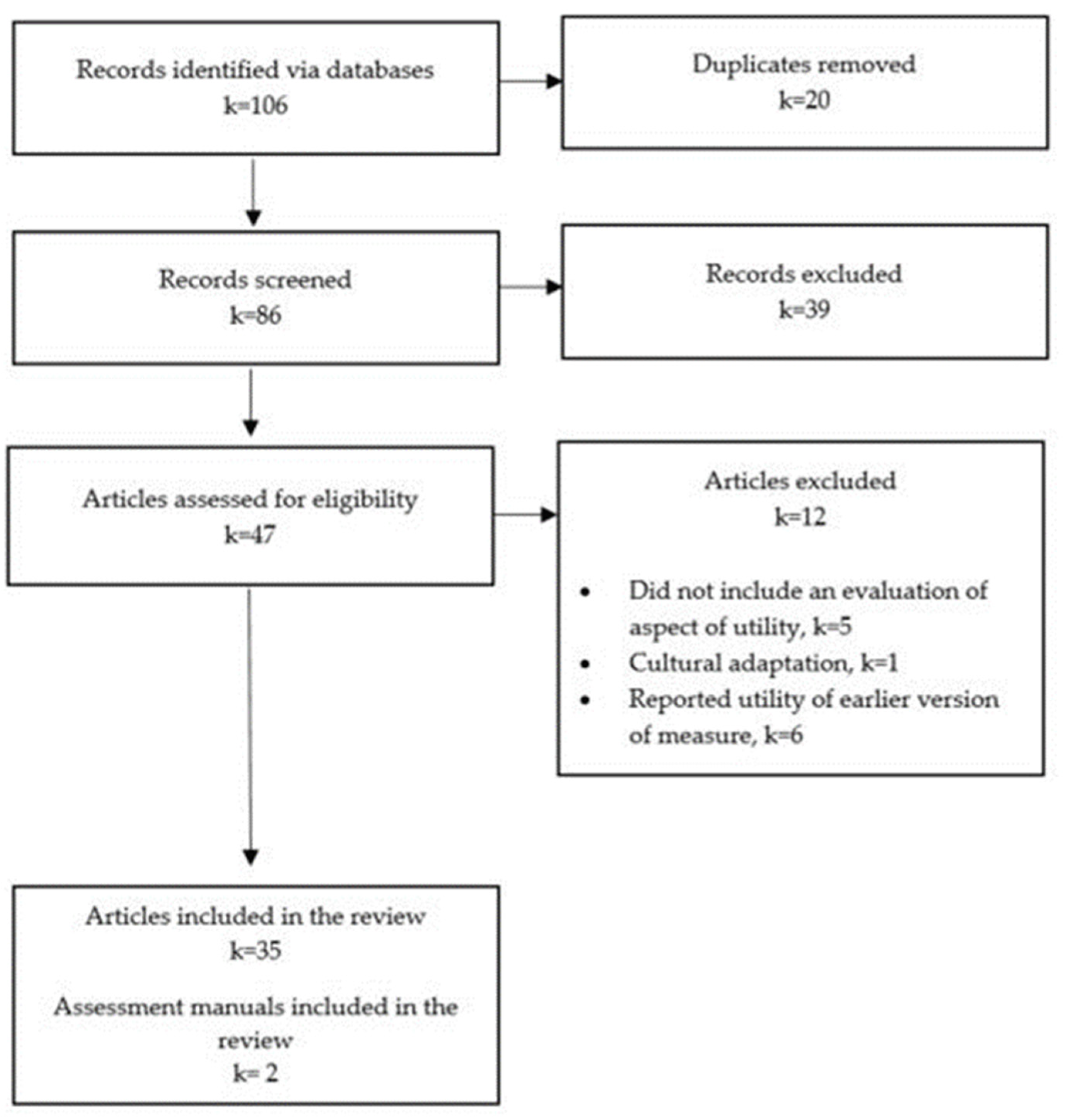
Targeted literature searches were conducted to identify articles reporting on aspects of overall utility, further defined in Table 1, of each measure identified in Phase One. The electronic databases ProQuest, Embase, CINAHL, and Scopus were used to search the literature for relevant articles published in English since 2000 (Figure 2). Search terms were grouped in relation to aspects of overall utility and the title of the measures, and searched for in the title or abstract of relevant resources. Combinations of search terms were truncated, exploded and adjusted with the assistance of a faculty librarian to meet the requirements of individual databases. Measure-specific search terms are included in Appendix A. Where applicable, the manuals of relevant measures were retrieved.

Table 1.
The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) definitions of domains and psychometric properties [28] (Note. Adapted from: “COSMIN methodology for systematic reviews of Patient-Reported Outcome Measures (PROMs)” by Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C., 2012, Amsterdam Public Health Research Institute: BT Amsterdam, p. 11–12 (https://cosmin.nl/wp-content/uploads/COSMIN-syst-review-for-PROMs-manual_version-1_feb-2018.pdf)).

Figure 2.
Phase Two, measures of functioning identification and screening process.
2.3. Selecting Studies
An iterative approach was utilised to ensure transparency and rigour of the scoping review process [34]. The inclusion and exclusion criteria were refined throughout the study selection process as familiarity with the research topic increased [33]. Studies were included if they reported on one or more aspects of overall utility of an included measure, and were peer-reviewed and available in full text. Studies were excluded if they only reported on the utility of an existing measure’s cultural adaptation.
2.4. Charting the Data
Data were extracted from the selected articles by two separate reviewers in line with the Arksey and O’Malley [33] framework. A data extraction table was developed and used to ensure a uniform data extraction process. Data from each of the articles were extracted in relation to the purpose of the study, study population, participant age, and methodological quality. Two reviewers independently evaluated the quality of the articles included in the review using the QualSyst checklists for assessing the quality of studies [37]. The QualSyst tool includes a 14-item checklist for evaluating quantitative studies and a 10-item checklist for evaluating qualitative studies. Each study was allocated a score represented as a percentage of 100 and a corresponding label indicating the study’s quality. As outlined by Kmet, Cook and Lee [37] in the user manual, a score of more than 80% indicates a strong study, 70–80% indicates good quality, 50–69% is adequate, and less than 50% indicates the study was of poor quality. Any inconsistencies in scores between the reviewers were resolved via discussion until total agreement was reached.
Two reviewers independently completed the OMRF [26] for each measure, taking into consideration the results of the targeted literature searches and the information included in the measures’ manuals, to evaluate their overall utility. Following this, any discrepancies between the two reviewers were discussed until consensus was reached. Using the OMRF [26], overall utility is assigned a descriptive rating, ranging from poor to excellent. An overall poor rating indicates poor clinical utility, the measure is not easily available, and has poor reliability and validity. An overall adequate rating indicates adequate to excellent clinical utility, the measure is easily available and has adequate to excellent reliability and validity. An overall excellent rating indicates adequate to excellent clinical utility, measure is easily available and has excellent reliability and validity.
In order to further determine the content validity of the included measures, specifically for autistic populations, meaningful concepts of each question or item included in the measure were independently linked by two reviewers to the ICF following the methodological rules outlined by Cieza et al. [38]. Using this methodology, items were first linked to the comprehensive ICF coding framework and later to specific ICF Core Sets for Autism, including the Comprehensive ICF Core Set and the Brief ICF Core Set for Autism (6–16 years) [20]. This process involved identifying the meaningful concepts in each item and linking these, as well as any examples, to the ICF. Meaningful concepts that were able to be linked to the ICF are referred to from this point forward as ‘codes’. Meaningful concepts that were determined ‘non-definable’ or ‘not covered’ in the ICF are not reported here. Consensus meetings were arranged to discuss any differences in the linking until total agreement was reached. Where the reviewers were unable to agree completely on a particular code for a meaningful concept, a third external reviewer experienced in ICF linking was consulted.
2.5. Collating, Summarising and Reporting the Results
PRISMA flow diagrams were developed and used to demonstrate the search process for Phases One and Two of this study. Key data extracted from the included articles were summarised and tabulated, including assessment tool characteristics, ICF Activities and Participation chapters covered, QualSyst ratings, and individual aspects of, as well as overall, utility. Descriptive statistics explaining the included measures’ coverage of both the comprehensive ICF Core Set for Autism and the Brief ICF Core Set for Autism (6–16 years) are also presented. A narrative synthesis of the available data was also conducted to summarise and highlight the key findings of the review.
3. Results
3.1. Identifying and Selecting Relevant Measures and Studies
Phase One identified 119 potential measures thorough searches of multiple sources. After applying the eligibility criteria listed above, 13 of these measures were deemed eligible for inclusion in the review. Targeted literature searches conducted in Phase Two returned a total of 106 abstracts. Once duplicates had been removed, 86 abstracts remained to be screened, and a total of 47 full-text articles were assessed for eligibility. The overall utility of the 13 eligible measures were assessed using a total of 35 original research articles, and two assessment manuals. The majority of articles investigating the utility of the measures were published by the authors of the measures themselves and no articles meeting the eligibility criteria were identified for either the Adaptive Behavior Assessment System (ABAS-3) or the Vineland Adaptive Behavior Scales (Vineland-3).
3.2. Measures of Functioning
An overview of the measures of functioning eligible for inclusion in this review, including a key for the abbreviations used in this section, is presented in Table 2.

Table 2.
Characteristics of included measures of functioning.
Four of the measures (ABAS-3, AusTOMs-OT, LIFE-H and Vineland-3) have a broad age range and can be used to assess functioning of individuals across the lifespan. The COPM is suitable for anyone aged over eight years. The remainder of the measures were intended to assess child and youth populations under the age of 21 (CAPE/PAC, PEM-CY, PEDI-CAT and PEDI-CAT ASD, PEGS, and SCOPE), and one measure can be used for individuals aged between 4 and 6 years (CPQ). Measures were predominantly developed in Canada (COPM, CAPE/PAC, LIFE-H, PEM-CY, and PEGS) and the USA (ABAS-3, PEDI-CAT, PEDI-CAT ASD, SCOPE and Vineland-3).
Six of the measures were designed to be administered as self- or proxy-report questionnaires (ABAS-3, CPQ, LIFE-H, PEM-CY, PEGS, and ROPP). Similarly, the PEDI-CAT and PEDI-CAT ASD are administered as proxy-report computer adaptive tests. Three of the measures were intended to be completed by a health professional either as an interview (COPM) or by rating an individual’s functioning following interaction with them (AusTOMs-OT and SCOPE). The CAPE-PAC and Vineland-3 have a variety of administration options, meaning they can be completed as an interview or proxy-report questionnaire.
The number of ICF Activity and Participation chapters covered by each included measure ranged between six and nine, with an average of eight chapters being covered. All measures included at least one question relating to the chapters of Domestic Life and Major Life Areas. The ICF chapters with the lowest representation across the measures of functioning were General Tasks and Demands and Communication, with only nine of the 13 measures including a question linking to these chapters. The following measures included at least one question linking to each of the nine chapters of the Activities and Participation domain of the ICF: ABAS-3, LIFE-H, PEDI-CAT, PEDI-CAT ASD, and Vineland-3.
3.3. Methodological Quality
The methodological quality of the studies reporting on the psychometric properties of the measures included in the review are presented in Table 3. The quality of the studies, scored by two independent reviewers using the QualSyst checklists developed by Kmet, Cook and Lee [37] ranged between adequate (60%) and strong (100%).

Table 3.
Descriptions and QualSyst ratings of studies evaluating the psychometric properties of included measures of functioning.
3.4. Psychometric Properties
An overview of the psychometric properties available for each measure and an assessment of their overall utility is presented in Table 4. Overall utility ratings ranged from poor to excellent, with the ABAS-3 receiving the highest overall rating and the CAPE-PAC receiving the lowest overall rating on the OMRF. Information regarding at least one type of reliability and validity was available for all measures. Responsiveness was the least reported property, with this information only available for five of the 13 assessments.

Table 4.
Characteristics of included assessment of functioning tools.
General content validity of the measures ranged from adequate to excellent, however, none of the measures included in this review were developed with the specific intention of assessing functioning of individuals on the spectrum. The ‘Activities and Participation’ domain of the ICF was most commonly assessed by the measures, with all measures including codes linking to a chapter of this domain, ranging between 21% and 100% of total codes. Three assessments tools (CAPE-PAC, COPM and CPQ) solely assessed functioning classified as Activities and Participation. Coverage of the Body Function domain ranged between 0% and 79% of total codes, with the AusTOMs-OT having the greatest number of codes linking to chapters of this domain. Environmental Factors were assessed less frequently, ranging between 0% and 42% of total codes. Only four measures included codes linking to Environmental Factors (ABAS-3, PEM-CY, ROPP and SCOPE). More information regarding the distribution of codes across the domains and chapters of the ICF is included in Table 5.

Table 5.
Distribution of codes linked to the International Classification of Functioning, Disability and Health [17] components and chapters.
Coverage of the comprehensive ICF Core Set for Autism ranged between 49% and 95%, with the ABAS-3 having the greatest total number of codes linking to this core set. Coverage of the Brief ICF Core Set for Autism (6–16 years) ranged between 35% and 73%, with the CAPE-PAC having the greatest total number of linked codes. However, all of these codes were linked to the Activities and Participation domain of the ICF. The percentages of total codes linking to the ICF Core Sets for Autism, both the Comprehensive and Brief (6–16 years), are presented in Table 6 for all included measures.

Table 6.
Percentage of total codes linking to the International Classification of Functioning, Disability and Health Core Sets [20] for Autism covered by measures of functioning.
The percentages of unique codes linking to the comprehensive ICF Core Set for Autism and the Brief ICF Core Set (6–16 years) were also determined and are presented in Table 7. Overall, coverage of the Comprehensive ICF Core Set for Autism ranged between 11% and 61%, with the Vineland-3 having the greatest percentage of unique codes linking to this core set. Coverage of items relevant to the Brief ICF Core Set for Autism (6–16 years) was less, ranging between 5% and 58%, with the Vineland-3 again having the highest percentage of unique codes linking to this core set.

Table 7.
Percentage of unique codes linking to the International Classification of Functioning, Disability and Health Core Sets [20] for Autism covered by measures of functioning.
4. Discussion
This scoping review aimed to identify existing measures of functioning suitable for use with school-aged children on the spectrum and evaluate the quality of their psychometric properties, specifically content validity. The results of this review identify the limitations of current measures of functioning, highlighting the variability in content validity of these measures for school-aged children on the spectrum, and providing further evidence that, at present, a suite of measures is required to effectively assess functioning of school-aged children on the spectrum. Existing measures focus almost exclusively on functioning in relation to activity participation without exploring the impact of body functions or environmental factors on an individual’s ability to function. This review also emphasised other inconsistencies across existing measures of functioning, both in their overall utility, and their methods of administration.
In addition to the presence of key features such as repetitive and inflexible behaviour patterns and difficulties during social interactions, a diagnosis of autism requires that these features significantly impact an individual’s ability to function across a range of contexts, including at home, work and/or school [84]. Although impaired functioning is inherent to a diagnosis of autism, the methods of obtaining and interpreting this information remains unclear. The findings of this review indicate that there is no single measure that adequately covers all areas of functioning in which a school-aged child on the spectrum may experience difficulties, with environmental factors being particularly underrepresented in the assessment tools reviewed. These results are supported by the information outlined in current guidelines for assessing and diagnosing autism, highlighting the importance of obtaining information from multiple sources to build an accurate and comprehensive picture of how well a person is able to function in their everyday life, which includes multiple environmental contexts [13,16,85].
Developed following a rigorous process endorsed by the WHO, the ICF Core Sets provide an appropriate framework for organising information relating to functioning, and are also considered a suitable basis for development of tools to comprehensively measure functioning in particular populations [18]. The ICF Core Sets for other conditions, including hearing loss [86], spinal cord injuries [87] and cancer [88], have been operationalised through the development of outcome measures designed to assess functioning or intervention efficacy [86,87,88]. In their original form, the ICF Core Sets provide a standard for evaluating functioning in particular health conditions. However, the development of measures based on the ICF Core Sets can improve their clinical utility and promote the progression of more holistic, biopsychosocial approaches to measuring functioning.
Overall utility of measures of functioning included in this review varied significantly, ranging from poor to excellent according to the OMRF standards. The ABAS-3 received the highest overall OMRF rating, however, when evaluating the content validity of the ABAS-3 against the ICF Core Sets for Autism, it covered less than half of the items considered most relevant for individuals on the spectrum. Despite receiving a lower overall OMRF rating, the Vineland-3 covered a higher percentage of the items included in the ICF Core Sets for Autism. This suggests that although assessment of functioning tools may be considered psychometrically sound, their content validity may vary depending on the population they are being used to assess. This aligns with the findings of a similar evaluation of the content validity of measures suitable for use with younger children suspected of neurodevelopmental conditions [89]. It is important for clinicians to be aware of the suitability of these measures of functioning for specific populations, as this may influence their decision to select one tool over another. The COSMIN initiative aims to support this process by providing methodological guidelines to assist clinicians in selecting the appropriate assessment tool for their purpose [90]. In recent years, further work has been conducted to update earlier COSMIN guidelines, providing greater clarity around the selection of tools based on content validity [91]. Poor content validity can influence other psychometric properties, reducing the quality of overall reliability, validity and responsiveness, suggesting that establishing content validity should be prioritised before other psychometric properties [91]. A factor to consider in the interpretation of the results presented in this review is that full assessment item banks were coded to the ICF. Some assessments, such as the Vineland-3, use basal and ceiling thresholds to determine which items are presented for scoring [50], meaning that not all items included in the full item bank are presented during an assessment, potentially reducing the content validity of an assessment in clinical application. Similarly, the PEDI-CAT and PEDI-CAT ASD are administered via Computer Adaptive Test, presenting users with questions based on their previous responses and therefore not including all items evaluated in this review [67].
The method of administration varied among the measures of functioning included in this review, with the majority being clinician-administered or proxy-report. There are very limited options available for children to self-report, providing their own perspectives and priorities for functioning. Since autism is a complex condition influenced by a variety of internal and external factors, using a variety of assessments to obtain information from multiple perspectives can again help to provide a more holistic understanding of an individual’s functional challenges and abilities [13]. In isolation, a clinician’s perspective may not adequately reflect the functional impact of autism in a home or school environment, and proxy-reporting caregivers may not have adequate knowledge or understanding to effectively report impacts on functioning that may be better observed by a clinician in a standardised environment [92,93]. It is important to also consider the context in which functioning is being assessed and the supports that may or may not be in place during the assessment [93]. There is inconsistency in the current measures regarding the ways in which functioning is assessed; some tools consider the person’s abilities with supports in place (e.g., PEDI-CAT/PEDI-CAT ASD) while others do not (e.g., ABAS-3 and Vineland-3). Inconsistencies such as these can lead to confusion regarding an individual’s true functioning and support needs, which may be better assessed by measures specifically developed to explore these needs [94]. Across measures included in this review there is limited consideration of the impact of cultural factors on functioning, with the majority of these assessments being developed and tested in Canada or the USA. In addition, there is a paucity of research investigating the utility of these tools outside of the teams who developed them. A previous review of adaptive behaviour scales by Floyd and colleagues [93] evaluated the psychometric evidence for a variety of scales, including earlier versions of the Vineland and ABAS, however, only considered the evidence available in the manuals of these tools. Similarly, during this review, no recently published peer-reviewed articles reporting on aspects of overall utility of either the Vineland-3 or ABAS-3 were identified, only the information provided by the publishers in the user manual.
Historically, the biomedical model of health and disability has concentrated on impairment, attributing disability to a particular health condition, with interventions focussed on preventing or treating the condition with the goal of ‘normalising’ functioning [95]. In contrast, the social model of disability views disability as a consequence of social, environmental and attitudinal barriers, secondary to the condition itself [96]. More recently, autism and other neurodevelopmental conditions have been conceptualised under the neurodiversity paradigm, which aligns in some regards with the social model of disability, considering disability to be the consequence of external rather than internal factors [97]. The neurodiversity paradigm re-frames the differences seen in neurodiverse individuals as strengths that may be used to support interventions and positively influence functioning [19]. As views of neurodiversity continue to evolve, so too does the need for measurement tools to accurately reflect the current contexts in which individuals on the spectrum live and function [19]. Researchers are beginning to acknowledge the importance of involving consumers in the research process, increasingly using methods of co-production to incorporate the views of the target population [98].
The authors acknowledge that there are limitations to this review. The inclusion criteria specified that only studies published in English were eligible for inclusion, which may account for the lack of cultural diversity represented among the measures and studies. In addition, only articles investigating elements of overall utility of the most recent version of the measure were considered which may influence the availability of psychometric information for measures where this has been established in earlier versions. Finally, although a comprehensive approach was taken to ensure a broad search of the literature, it is possible that these methods may not have captured every available article reporting on the overall utility of the included measures.
5. Conclusions
This review contributes to the existing literature by providing a useful summary of the psychometric properties of measures of functioning that can be used by researchers and clinicians to facilitate the selection of suitable measures for assessing functioning of school-aged children on the autism spectrum. Effectively assessing functioning of school-aged children on the spectrum is increasingly important in both the Australian and international contexts given the shift towards disability support systems allocating funding based on level of functioning and support needs. For individuals on the spectrum, functioning can vary significantly, highlighting the need for reliable and valid methods of assessment that are capable of identifying the unique strengths and challenges of this population. There are a number of factors which should be considered when selecting a measure of functioning, including the purpose of the assessment, the population it is assessing, and the complete range of psychometric properties, including content validity. This review not only synthesises the properties of existing measures, but adds a comprehensive evaluation of the content validity of these measures for use with school-aged children on the spectrum. Further research in this area is required to ensure measures of functioning align with contemporary views of disability and are developed in collaboration with those most likely to benefit from them. Future research may seek to develop and evaluate holistic assessment of functioning tools based on the ICF Core Sets for Autism, with input from individuals on the spectrum and their families.
Author Contributions
Conceptualization, A.J.O.W., B.A., B.M., K.E., M.H.-E. and S.G.; methodology, B.M., E.D., K.E., M.H.-E. and S.G.; formal analysis, A.C., E.D. and M.H.-E.; resources, A.J.O.W., B.M., K.E. and S.G.; data curation, A.C., E.D. and M.H.-E.; writing—original draft preparation, M.H.-E.; writing—review and editing, A.C., A.J.O.W., B.A., B.M., E.D., K.E., M.H.-E., S.B. and S.G.; supervision, B.A., B.M., K.E., S.B. and S.G.; project administration, A.C., A.J.O.W., B.M., K.E., M.H.-E. and S.G.; funding acquisition, A.J.O.W., B.M., K.E., M.H.-E., S.B. and S.G. All authors have read and agreed to the published version of the manuscript.
Funding
The authors acknowledge the financial support of the National Disability Insurance Agency (NDIA) (project number 0.012) and Autism CRC (project numbers 3.061 and 0.012), established and supported under the Australian Government’s Cooperative Research Centre Program. A.J.O.W. is supported by an Investigator Grant from the National Health and Medical Research Council (grant no. 1173896).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are not publicly available.
Acknowledgments
The authors wish to acknowledge the research assistance of Sasha Johnston, Julia Tang and Kerry Wallace.
Conflicts of Interest
The authors declare no direct conflict of interest related to this article. S.B. declares no direct conflict of interest related to this article. S.B. reports grants from the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, FORMAS, VINNOVA, Trygg Hansa, Stiftelsen Clas Groschinskys Minnesfond, Stiftelsen Sunnerdahls Handikappfond, and Promobilia for his research on the ICF. S.B. discloses that he has in the last 3 years acted as an author, consultant or lecturer for Medice and Roche. He receives royalties for textbooks and diagnostic tools from Hogrefe, and Liber. S.B. is shareholder in SB Education/Psychological Consulting AB and NeuroSupportSolutions International AB. The funders had no role in the design of this study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results. The Autism CRC reviewed the manuscript prior to publication to ensure that it aligned with their Language and Terminology Guide.
Appendix A

Table A1.
Search Terms Used to Identify Relevant Articles.
Table A1.
Search Terms Used to Identify Relevant Articles.
| Search terms relating to psychometric properties |
| (psychometric * OR validity OR “predictive validity” OR “internal validity” OR “face validity” OR “external validity” OR “discriminant validity” OR “criterion related validity” OR “concurrent validity” OR “construct validity” OR “content validity” OR “validation study” OR reliability OR “reliability and validity” OR “test–retest reliability” OR “intrarater reliability” OR “interrater reliability” OR psychometric* OR reliabil* OR valid* OR sensitivity OR specificit* OR bias OR reproducib* OR feasib* OR “clinical utility” OR usability OR appropriate* OR accessib* OR practiab* OR acceptab*) |
| AND |
| Assessment specific terms |
| Adaptive Behavior Assessment System |
| (“adaptive behavior assessment system” or “ABAS”) |
| Australian Therapy Outcome Measures for Occupational Therapy |
| (“Australian Therapy Outcome Measures for Occupational Therapy” or “AusTOMs-OT” or “AusTOMS OT”) |
| Canadian Occupational Performance Measure |
| (“Canadian Occupational Performance Measure” OR COPM) |
| Children’s Assessment of Participation and Enjoyment and Preferences for Activities of Children (CAPE-PAC) |
| (“Children’s assessment of participation and enjoyment” or CAPE or “Enjoyment and preferences for activities of children” or “CAPE-PAC”) |
| Children’s Participation Questionnaire |
| (“Children’s participation questionnaire” or CPQ) |
| Life Habits Assessment |
| (“Life habits assessment” or “LIFE H” or “LIFE-H”) |
| PEM-CY |
| (pem-cy OR “participation and environment measure” OR “participation and environment measure children and youth”) |
| PEDI-CAT/PEDI-CAT (ASD) |
| (pedicat OR “pedicat asd” OR pedi-cat OR “pediatric evaluation of disability inventory computer adaptive test”) |
| Perceived Efficacy and Goal Setting |
| (“Perceived efficacy and goal setting” or PEGS) |
| Rating of Perceived Participation |
| (“Rating of perceived participation” or ROPP) |
| Short Child Occupational Profile |
| (“Short child occupational profile” or SCOPE) |
| Vineland-3 |
| (vineland OR vineland-3 OR “vineland three” OR “vineland III” OR “vineland 3” OR vineland-III OR “vineland third edition” |
* Indicates a truncation wildcard, used to search for variations of the core word
References
- Monk, R.; Whitehouse, A.J.; Waddington, H. The use of language in autism research. Trends Neurosci. 2022, 45, 791–793. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. ICD-11 for Mortality and Morbidity Statistics; World Health Organisation: Geneva, Switzerland, 2018. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2022. [Google Scholar]
- Kasari, C.; Locke, J.; Gulsrud, A.; Rotheram-Fuller, E. Social Networks and Friendships at School: Comparing Children with and Without ASD. J. Autism Dev. Disord. 2011, 41, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Zeidan, J.; Fombonne, E.; Scorah, J.; Ibrahim, A.; Durkin, M.S.; Saxena, S.; Yusuf, A.; Shih, A.; Elsabbagh, M. Global prevalence of autism: A systematic review update. Autism Res. 2022, 15, 778–790. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Li, Y.; Liu, B.; Chen, Q.; Xing, X.; Xu, G.; Yang, W. Prevalence of Autism Spectrum Disorder Among Children and Adolescents in the United States from 2019 to 2020. JAMA Pediatr. 2022, 176, 934–945. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Disability, Ageing and Carers, Australia: Summary of Findings; Australian Bureau of Statistics: Canberra, Australia, 2019.
- Maree, J.G. The psychosocial development theory of Erik Erikson: Critical overview. Early Child Dev. Care 2021, 191, 1107–1121. [Google Scholar] [CrossRef]
- Australian Government Productivity Commission. Disability Care and Support (54); Commonwealth of Australia: Canberra, Australia, 2011.
- National Disability Insurance Agency. What Is the NDIS? Available online: https://www.ndis.gov.au/understanding/what-ndis (accessed on 24 August 2022).
- National Disability Insurance Agency. In Young People in the NDIS; National Disability Insurance Agency: Canberra, Australia, 2020.
- Levy, A.; Perry, A. Outcomes in adolescents and adults with autism: A review of the literature. Res. Autism Spectr. Disord. 2011, 5, 1271–1282. [Google Scholar] [CrossRef]
- Whitehouse, A.; Evans, K.; Eapen, V.; Wray, J. A National Guideline for the Assessment and Diagnosis of Autism Spectrum Disorders in Australia; National Disability Insurance Agency: Canberra, Australia, 2018.
- National Institute for Health and Care Excellence. Autism Spectrum Disorder in under 19s: Recognition, Referral and Diagnosis; National Institute for Health and Care Excellence: London, UK, 2011.
- Ministries of Health and Education. New Zealand Autism Spectrum Disorder Guideline; Ministry of Health: Wellington, New Zealand, 2016.
- Hyman, S.L.; Levy, S.E.; Myers, S.M. Identification, Evaluation, and Management of Children with Autism Spectrum Disorder. Pediatrics 2020, 145, e20193447. [Google Scholar] [CrossRef]
- World Health Organisation. How to Use the ICF: A Practical Manual for Using the International Classification of Functioning, Disability and Health (ICF); World Health Organisation: Geneva, Switzerland, 2013. [Google Scholar]
- de Schipper, E.; Mahdi, S.; de Vries, P.; Granlund, M.; Holtmann, M.; Karande, S.; Almodayfer, O.; Shulman, C.; Tonge, B.; Wong, V.V.; et al. Functioning and disability in autism spectrum disorder: A worldwide survey of experts. Autism Res. 2016, 9, 959–969. [Google Scholar] [CrossRef]
- Bölte, S.; Lawson, W.B.; Marschik, P.B.; Girdler, S. Reconciling the seemingly irreconcilable: The WHO’s ICF system integrates biological and psychosocial environmental determinants of autism and ADHD: The International Classification of Functioning (ICF) allows to model opposed biomedical and neurodiverse views of autism and ADHD within one framework. BioEssays 2021, 43, 2000254. [Google Scholar] [CrossRef]
- Bölte, S.; Mahdi, S.; De Vries, P.J.; Granlund, M.; Robison, J.E.; Shulman, C.; Swedo, S.; Tonge, B.; Wong, V.; Zwaigenbaum, L.; et al. The Gestalt of functioning in autism spectrum disorder: Results of the international conference to develop final consensus International Classification of Functioning, Disability and Health core sets. Autism 2019, 23, 449–467. [Google Scholar] [CrossRef]
- Tudge, J.R.H.; Mercon-Vargas, E.A.; Liang, Y.; Payir, A. The importance of Urie Bronfenbrenner’s bioecological theory for early childhood education. In Theories of Early Childhood Education: Developmental, Behaviorist, and Critical; Cohen, L.E., Waite-Stupiansky, S., Eds.; Taylor and Francis: Florence, Italy, 2017; pp. 45–57. [Google Scholar]
- McConachie, H.; Parr, J.R.; Glod, M.; Hanratty, J.; Livingstone, N.; Oono, I.P.; Robalino, S.; Baird, G.; Beresford, B.; Charman, T.; et al. Systematic review of tools to measure outcomes for young children with autism spectrum disorder. Health Technol. Assess. 2015, 19, 1–506. [Google Scholar] [CrossRef] [PubMed]
- Hirota, T.; So, R.; Kim, Y.S.; Leventhal, B.; Epstein, R.A. A systematic review of screening tools in non-young children and adults for autism spectrum disorder. Res. Dev. Disabil. 2018, 80, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Thabtah, F.; Peebles, D. Early Autism Screening: A Comprehensive Review. Int. J. Environ. Res. Public Health 2019, 16, 3502. [Google Scholar] [CrossRef] [PubMed]
- Falkmer, T.; Anderson, K.; Falkmer, M.; Horlin, C. Diagnostic procedures in autism spectrum disorders: A systematic literature review. Eur. Child Adolesc. Psychiatry 2013, 22, 329–340. [Google Scholar] [CrossRef] [PubMed]
- CanChild. Outcome Measures Rating Form; McMaster University: Hamilton, ON, Canada, 2004. [Google Scholar]
- Smart, A. A multi-dimensional model of clinical utility. Int. J. Qual. Health Care 2006, 18, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Prinsen, C.A.C.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; de Vet, H.C.W.; Terwee, C.B. COSMIN methodology for systematic reviews of Patient-Reported Outcome Measures (PROMs): User Manual. Qual. Life Res. 2018, 27, 1147–1157. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C. COSMIN Checklist Manual; EMGO Institute for Health and Care Research: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Connell, J.; Carlton, J.; Grundy, A.; Buck, E.T.; Keetharuth, A.D.; Ricketts, T.; Barkham, M.; Robotham, D.; Rose, D.; Brazier, J. The importance of content and face validity in instrument development: Lessons learnt from service users when developing the Recovering Quality of Life measure (ReQoL). Qual. Life Res. 2018, 27, 1893–1902. [Google Scholar] [CrossRef]
- Bölte, S.; de Schipper, E.; Robison, J.E.; Wong, V.C.; Selb, M.; Singhal, N.; de Vries, P.J.; Zwaigenbaum, L. Classification of Functioning and Impairment: The Development of ICF Core Sets for Autism Spectrum Disorder. Autism Res. 2014, 7, 167–172. [Google Scholar] [CrossRef]
- Mahdi, S.; Viljoen, M.; Yee, T.; Selb, M.; Singhal, N.; Almodayfer, O.; Granlund, M.; De Vries, P.J.; Zwaigenbaum, L.; Bölte, S. An international qualitative study of functioning in autism spectrum disorder using the World Health Organization international classification of functioning, disability and health framework. Autism Res. 2018, 11, 463–475. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K.; Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Daudt, H.M.L.; Van Mossel, C.; Scott, S.J. Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med. Res. Methodol. 2013, 13, 48. [Google Scholar] [CrossRef]
- McGowan, J.; Straus, S.; Moher, D.; Langlois, E.V.; O’Brien, K.K.; Horsley, T.; Aldcroft, A.; Zarin, W.; Garitty, C.M.; Hempel, S.; et al. Reporting scoping reviews—PRISMA ScR extension. J. Clin. Epidemiol. 2020, 123, 177–179. [Google Scholar] [CrossRef] [PubMed]
- Kmet, L.M.; Cook, L.S.; Lee, R.C. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields; Alberta Heritage Foundation for Medical Research: Edmonton, AB, Canada, 2004.
- Cieza, A.; Fayed, N.; Bickenbach, J.; Prodinger, B. Refinements of the ICF Linking Rules to strengthen their potential for establishing comparability of health information. Disabil. Rehabil. 2019, 41, 574–583. [Google Scholar] [CrossRef]
- Harrison, P.; Oakland, T. Adaptive Behavior Assessment System, 3rd ed.; Western Psychological Services: Washington, DC, USA, 2015. [Google Scholar]
- Unsworth, C.; Duncombe, D. AusTOMs for Occupational Therapy; LaTrobe University: Melbourne, Australia, 2004. [Google Scholar]
- Law, M.; Baptiste, S.; Carswell, A.; McColl, M.A.; Polatajko, H.; Pollock, N. Canadian Occupational Performance Measure, 5th ed.; Canadian Association of Occupational Therapists: Ottawa, ON, Canada, 2000. [Google Scholar]
- King, G.; Law, M.; King, S.; Hurley, P.; Hanna, S.; Kertoy, M.; Rosenbaum, P.; Young, N. Children’s Assessment of Participation and Enjoyment (CAPE) and Preferences for Activities of Children (PAC); Harcourt Assessment Inc.: San Antonio, TX, USA, 2004. [Google Scholar]
- Rosenberg, L.; Jarus, T.; Bart, O. Development and initial validation of the Children Participation Questionnaire (CPQ). Disabil. Rehabil. 2010, 32, 1633–1644. [Google Scholar] [CrossRef]
- Coster, W.; Law, M.; Bedell, G. Participation and Environment Measure for Children and Youth (PEM-CY); Boston University: Boston, MA, USA, 2010. [Google Scholar]
- Haley, S.M.; Coster, W.; Dumas, H.; Fragala-Pinkham, M.; Moed, R. PEDI-CAT: Development, Standardisation an Administration Manual; CRECare LLC: Boston, MA, USA, 2012. [Google Scholar]
- Haley, S.M.; Coster, W.; Dumas, H.; Fragala-Pinkham, M.; Moed, R.; Kramer, J.; Ni, P.; Feng, T.; Kao, Y.C.; Ludlow, L.H. Pediatric Evaluation of Disability Inventory: Development, Standardisation and Aministration Manual; (Version 1.4.3); Boston University: Boston, MA, USA, 2019. [Google Scholar]
- Missiuna, C.; Pollock, N.; Law, M. PEGS, The Perceived Efficacy and Goal Setting System; Harcourt Assessment: San Antonio, TX, USA, 2004. [Google Scholar]
- Sandström, M.; Lundin-Olsson, L. Development and evaluation of a new questionnaire for rating perceived participation1. Clin. Rehabil. 2007, 21, 833–845. [Google Scholar] [CrossRef]
- Bowyer, P.; Kramer, J.; PLoSzaj, A.; Ross, M.; Schwartz, O.; Kielhofner, G.; Kramer, K. A Users Manual for the Short Child Occupational Profile (SCOPE) Version 2.2. The Model of Human Occupation Clearinghouse; University of Illinois: Chicago, IL, USA, 2008. [Google Scholar]
- Sparrow, S.; Cicchetti, D.; Saulnier, C. Vineland Adaptive Behavior Scales, 3rd ed.; Pearson: San Antonio, TX, USA, 2016. [Google Scholar]
- Scott, F.; Unsworth, C.A.; Fricke, J.; Taylor, N. Reliability of the Australian Therapy Outcome Measures for Occupational Therapy Self-care scale. Aust. Occup. Ther. J. 2006, 53, 265–276. [Google Scholar] [CrossRef]
- Unsworth, C.A. Measuring outcomes using the Australian therapy outcome measures for occupational therapy (AusTOMs-OT): Data description and tool sensitivity. Br. J. Occup. Ther. 2005, 68, 354–366. [Google Scholar] [CrossRef]
- Unsworth, C.A.; Coulson, M.; Swinton, L.; Cole, H.; Sarigiannis, M. Determination of the minimal clinically important difference on the Australian Therapy Outcome Measures for Occupational Therapy (AusTOMs—OT). Disabil. Rehabil. 2015, 37, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Unsworth, C.A.; Timmer, A.; Wales, K. Reliability of the Australian Therapy Outcome Measures for Occupational Therapy (AusTOMs-OT). Aust. Occup. Ther. J. 2018, 65, 376–386. [Google Scholar] [CrossRef] [PubMed]
- Unsworth, C.A.; Duckett, S.J.; Duncombe, D.; Perry, A.; Skeat, J.; Taylor, N. Validity of the AusTOM scales: A comparison of the AusTOMs and EuroQol-5D. Health Qual. Life Outcomes 2004, 2, 64. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brown, T.; Thyer, L. The convergent validity of the Children’s Leisure Assessment Scale (CLASS) and Children’s Assessment of Participation and Enjoyment and Preferences for Activities of Children (CAPE/PAC). Scand. J. Occup. Ther. 2019, 27, 349–363. [Google Scholar] [CrossRef] [PubMed]
- King, G.A.; Law, M.; King, S.; Hurley, P.; Hanna, S.; Kertoy, M.; Rosenbaum, P. Measuring children’s participation in recreation and leisure activities: Construct validation of the CAPE and PAC. Child Care, Health Dev. 2007, 33, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Potvin, M.-C.; Snider, L.; Prelock, P.; Kehayia, E.; Wood-Dauphinee, S. Children’s Assessment of Participation and Enjoyment/Preference for Activities of Children: Psychometric Properties in a Population with High-Functioning Autism. Am. J. Occup. Ther. 2013, 67, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Eyssen, I.C.J.M.; Beelen, A.; Dedding, C.; Cardol, M.; Dekker, J. The reproducibility of the Canadian Occupational Performance Measure. Clin. Rehabil. 2005, 19, 888–894. [Google Scholar] [CrossRef] [PubMed]
- McColl, M.A.; Paterson, M.; Davies, D.; Doubt, L.; Law, M. Validity and Community Utility of the Canadian Occupational Performance Measure. Can. J. Occup. Ther. 2000, 67, 22–30. [Google Scholar] [CrossRef]
- Tuntland, H.; Aaslund, M.K.; Langeland, E.; Espehaug, B.; Kjeken, I. Psychometric properties of the Canadian Occupational Performance Measure in home-dwelling older adults. J. Multidiscip. Health 2016, 9, 411–423. [Google Scholar] [CrossRef]
- Verkerk, G.J.Q.; Wolf, M.J.M.A.G.; Louwers, A.M.; Meester-Delver, A.; Nollet, F. The reproducibility and validity of the Canadian Occupational Performance Measure in parents of children with disabilities. Clin. Rehabil. 2006, 20, 980–988. [Google Scholar] [CrossRef]
- Cusick, A.; Lannin, N.; Lowe, K. Adapting the Canadian Occupational Performance Measure for use in a paediatric clinical trial. Disabil. Rehabil. 2007, 29, 761–766. [Google Scholar] [CrossRef]
- Noreau, L.; Desrosiers, J.; Robichaud, L.; Fougeyrollas, P.; Rochette, A.; Viscogliosi, C. Measuring social participation: Reliability of the LIFE-H in older adults with disabilities. Disabil. Rehabil. 2004, 26, 346–352. [Google Scholar] [CrossRef]
- Noreau, L.; Lepage, C.; Boissiere, L.; Picard, R.; Fougeyrollas, P.; Mathieu, J.; Desmarais, G.; Nadeau, L. Measuring participation in children with disabilities using the Assessment of Life Habits. Dev. Med. Child Neurol. 2007, 49, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Dumas, H.M.; Fragala-Pinkham, M.A. Concurrent validity and reliability of the pediatric evaluation of disability inventory-computer adaptive test mobility domain. Pediatr. Phys. Ther. 2012, 24, 171–176; discussion 176. [Google Scholar] [CrossRef] [PubMed]
- Dumas, H.M.; Fragala-Pinkham, M.A.; Haley, S.M.; Ni, P.; Coster, W.; Kramer, J.M.; Kao, Y.-C.; Moed, R.; Ludlow, L.H. Computer adaptive test performance in children with and without disabilities: Prospective field study of the PEDI-CAT. Disabil. Rehabil. 2012, 34, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Dumas, H.M.; Fragala-Pinkham, M.A.; Rosen, E.L.; O’Brien, J.E. Construct validity of the pediatric evaluation of disability inventory computer adaptive test (PEDI-CAT) in children with medical complexity. Disabil. Rehabil. 2017, 39, 2446–2451. [Google Scholar] [CrossRef] [PubMed]
- Haley, S.M.; Coster, W.J.; Dumas, H.M.; Fragala-Pinkham, M.A.; Kramer, J.; Ni, P.; Tian, F.; Kao, Y.-C.; Moed, R.; Ludlow, L.H. Accuracy and precision of the Pediatric Evaluation of Disability Inventory computer-adaptive tests (PEDI-CAT). Dev. Med. Child Neurol. 2011, 53, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Shore, B.J.; Allar, B.G.; Miller, P.E.; Matheney, T.H.; Snyder, B.D.; Fragala-Pinkham, M. Measuring the Reliability and Construct Validity of the Pediatric Evaluation of Disability Inventory–Computer Adaptive Test (PEDI-CAT) in Children with Cerebral Palsy. Arch. Phys. Med. Rehabil. 2019, 100, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Shore, B.J.; Allar, B.G.; Miller, P.E.; Matheney, T.H.; Snyder, B.D.; Fragala-Pinkham, M.A. Evaluating the Discriminant Validity of the Pediatric Evaluation of Disability Inventory: Computer Adaptive Test in Children with Cerebral Palsy. Phys. Ther. 2017, 97, 669–676. [Google Scholar] [CrossRef]
- Coster, W.J.; Kramer, J.M.; Tian, F.; Dooley, M.; Liljenquist, K.; Kao, Y.-C.; Ni, P. Evaluating the appropriateness of a new computer-administered measure of adaptive function for children and youth with autism spectrum disorders. Autism 2016, 20, 14–25. [Google Scholar] [CrossRef]
- Kramer, J.M.; Coster, W.J.; Kao, Y.-C.; Snow, A.; Orsmond, G.I. A New Approach to the Measurement of Adaptive Behavior: Development of the PEDI-CAT for Children and Youth with Autism Spectrum Disorders. Phys. Occup. Ther. Pediatr. 2012, 32, 34–47. [Google Scholar] [CrossRef]
- Kramer, J.M.; Liljenquist, K.; Coster, W.J. Validity, reliability, and usability of the Pediatric Evaluation of Disability Inventory-Computer Adaptive Test for autism spectrum disorders. Dev. Med. Child Neurol. 2015, 58, 255–261. [Google Scholar] [CrossRef]
- Missiuna, C.; Pollock, N. Perceived Efficacy and Goal Setting in Young Children. Can. J. Occup. Ther. 2000, 67, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Missiuna, C.; Pollock, N.; Law, M.; Walter, S.; Cavey, N. Examination of the Perceived Efficacy and Goal Setting System (PEGS) With Children with Disabilities, Their Parents, and Teachers. Am. J. Occup. Ther. 2006, 60, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Coster, W.; Bedell, G.; Law, M.; Khetani, M.A.; Teplicky, R.; Liljenquist, K.; Gleason, K.; Kao, Y.-C. Psychometric evaluation of the Participation and Environment Measure for Children and Youth. Dev. Med. Child Neurol. 2011, 53, 1030–1037. [Google Scholar] [CrossRef]
- Coster, W.; Law, M.; Bedell, G.; Khetani, M.; Cousins, M.; Teplicky, R. Development of the participation and environment measure for children and youth: Conceptual basis. Disabil. Rehabil. 2012, 34, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Khetani, M.; Marley, J.; Baker, M.; Albrecht, E.; Bedell, G.; Coster, W.; Anaby, D.; Law, M. Validity of the Participation and Environment Measure for Children and Youth (PEM-CY) for Health Impact Assessment (HIA) in sustainable development projects. Disabil. Health J. 2014, 7, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Noonan, V.K.; Kopec, J.A.; Noreau, L.; Singer, J.; Chan, A.; Mâsse, L.C.; Dvorak, M.F. Comparing the content of participation instruments using the International Classification of Functioning, Disability and Health. Health Qual. Life Outcomes 2009, 7, 93. [Google Scholar] [CrossRef]
- Bowyer, P.L.; Kramer, J.; Kielhofner, G.; Maziero-Barbosa, V.; Girolami, G. Measurement Properties of the Short Child Occupational Profile (SCOPE). Phys. Occup. Ther. Pediatr. 2007, 27, 67–85. [Google Scholar] [CrossRef]
- Kramer, J.; Bowyer, P.; Maziero-Barbosa, V.; Kielhofner, G.; O’Brien, J. Examining Rater Behavior on a Revised Version of the Short Child Occupational Profile (SCOPE). OTJR Occup. Particip. Health 2009, 29, 88–96. [Google Scholar] [CrossRef]
- Bowyer, P.; Lee, J.; Kramer, J.; Taylor, R.R.; Kielhofner, G. Determining the Clinical Utility of the Short Child Occupational Profile (SCOPE). Br. J. Occup. Ther. 2012, 75, 19–28. [Google Scholar] [CrossRef]
- World Health Organization. ICD-11 for Mortality and Morbidity Statistics: 6A02 Autism Spectrum Disorder. Available online: https://icd.who.int/browse11/l-m/en#/http%253a%252f%252fid.who.int%252ficd%252fentity%252f437815624 (accessed on 25 September 2022).
- Autism Spectrum Disorder in under 19s: Recognition, Referral and Diagnosis. Available online: https://www.nice.org.uk/guidance/cg128 (accessed on 25 September 2022).
- van Leeuwen, L.M.; Pronk, M.; Merkus, P.; Goverts, S.T.; Terwee, C.B.; Kramer, S.E. Operationalization of the Brief ICF Core Set for Hearing Loss: An ICF-Based e-Intake Tool in Clinical Otology and Audiology Practice. Ear Heart 2020, 41, 1533–1544. [Google Scholar] [CrossRef]
- Coelho, J.N.; de Almeida, C.; Vianna, P.C.; Dalto, V.F.; Castro, F.F.S.; Rabeh, S.A.N.; Riberto, M. Development of an ICF Core Set Based Instrument for Individuals with Non-traumatic Spinal Cord Injury. Int. J. Phys. Med. Rehabil. 2017, 5, 2. [Google Scholar] [CrossRef]
- Yang, E.J.; Shin, E.-K.; Shin, H.-I.; Lim, J.-Y. Psychometric properties of scale constructed from the International Classification of Functioning, Disability and Health (ICF) core set for breast cancer based on Rasch analysis. Support. Care Cancer 2014, 22, 2839–2849. [Google Scholar] [CrossRef] [PubMed]
- D’Arcy, E.; Wallace, K.; Chamberlain, A.; Evans, K.; Milbourn, B.; Bölte, S.; Whitehouse, A.J.; Girdler, S. Content validation of common measures of functioning for young children against the International Classification of Functioning, Disability and Health and Code and Core Sets relevant to neurodevelopmental conditions. Autism 2022, 26, 928–939. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Prinsen, C.A.C.; Bouter, L.M.; de Vet, H.C.W.; Terwee, C.B. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) and how to select an outcome measurement instrument. Braz. J. Phys. Ther. 2016, 20, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Terwee, C.B.; Prinsen, C.A.C.; Chiarotto, A.; Westerman, M.J.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; de Vet, H.C.W.; Mokkink, L.B. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: A Delphi study. Qual. Life Res. 2018, 27, 1159–1170. [Google Scholar] [CrossRef]
- Goldstein, S. Assessment of Autism Spectrum Disorders; Guilford Publications: New York, NY, USA, 2012. [Google Scholar]
- Floyd, R.G.; Shands, E.I.; Alfonso, V.C.; Phillips, J.F.; Autry, B.K.; Mosteller, J.A.; Skinner, M.; Irby, S. A Systematic Review and Psychometric Evaluation of Adaptive Behavior Scales and Recommendations for Practice. J. Appl. Sch. Psychol. 2015, 31, 83–113. [Google Scholar] [CrossRef]
- Arnold, S.R.C.; Riches, V.C.; Stancliffe, R.J. Does a Measure of Support Needs Predict Funding Need Better Than a Measure of Adaptive and Maladaptive Behavior? Am. J. Intellect. Dev. Disabil. 2015, 120, 375–394. [Google Scholar] [CrossRef]
- Smart, J.F.; Smart, D.W. Models of Disability: Implications for the Counseling Profession. J. Couns. Dev. 2006, 84, 29–40. [Google Scholar] [CrossRef]
- Dirth, T.P.; Branscombe, N.R. Disability Models Affect Disability Policy Support through Awareness of Structural Discrimination: Models of Disability. J. Soc. Issues 2017, 73, 413–442. [Google Scholar] [CrossRef]
- Pellicano, E.; Houting, J.D. Annual Research Review: Shifting from ‘normal science’ to neurodiversity in autism science. J. Child Psychol. Psychiatry 2022, 63, 381–396. [Google Scholar] [CrossRef]
- Cargo, M.; Mercer, S.L. The Value and Challenges of Participatory Research: Strengthening Its Practice. Annu. Rev. Public Health 2008, 29, 325–350. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).