Abstract
The relationship between being a victim of physical violence by an intimate partner and binge drinking (BD) is a poorly explored line of research, especially in men. To determine the association between being a victim of physical violence by an intimate partner and BD in men and women in Peru in 2020, a secondary analytical cross-sectional study was conducted using the Demographic Health Survey. BD was categorized according to the Center of Disease Control definition for men and women, based on the type and amount of alcoholic beverage ingested. Physical violence was based the report of being hit with any part of the body or an object, by their intimate partner. To identify the association, a multivariable general linear model of the family and link log Poisson was used. The results were presented as prevalence ratios (PRs). In the adjusted models stratified by sex, a 90% greater likelihood of BD was found in male victims and an 80% higher probability among female victims (PRa 1.9, 95%CI 1.3;2.7, p < 0.001 vs. PRa 1.8, CI95% 1.1; 2.8, p = 0.013, respectively). An association was found between physical violence by an intimate partner and BD in the Peruvian population older than 15 years, in both men and women.
1. Introduction
Intimate partner violence is a normalized public health issue in many cultures worldwide, especially in developing countries [1,2,3,4]. According to the World Health Organization, one in three women in the world has suffered physical and/or sexual violence at some point in her life [5]. However, little is known about the actual proportion of male victims of intimate partner violence, especially in developing countries [6,7,8,9]. There is an information gap regarding its global prevalence [10], although 30% of men have reported suffering it in the United States [10]. In Peru, information on male victims of intimate partner violence is not as widely studied as in women, neither does include psychological or sexual violence [4]. In 2019, reports showed that 10.7% of women had been victims of physical violence by their intimate partners during the last 12 months [11]. Among the sequelae of violence mainly identified among women are physical injuries, as well as traumatic experiences, some of them permanent. Regarding relationships and interaction with society, victims of intimate partner violence are more likely to have depression and other mental health disorders [12,13], engage in risk behaviors, and contract sexually transmitted diseases [14]. They are also more likely to experience a reduction in their quality of life. In addition to these direct effects on the victims of physical violence, there is a great economic burden on the health system and on productive activity [15]. Despite the above, it is regarded as an everyday issue, and due to the stigma associated with being a victim, the different gender roles in each culture, and the lack of support networks for victims, the latter often choose to remain silent, which contributes to the chronification of the invisibility of this problem, mainly in developing countries [16].
A longitudinal study conducted on young people in Peru during the mandatory lockdown due to the COVID-19 pandemic in 2020, identified that 8.3% of this population experienced an increase in domestic physical violence without significant differences regarding sex, which was more significant in those individuals with a history of violence [17]. Social isolation and quarantine are associated with an increase in anxiety and stress and a drastic change in routines and habits, such as increased alcohol and tobacco consumption; these being risk factors that contribute to the increase in aggressive behaviors [18,19]. A study analyzing the characteristics of the COVID-19 pandemic and the lockdown context reveals that the increase in stress and maladaptive coping strategies, such as substance abuse, may lead to aggression and an increase in mental health disorders, which have been directly related to the escalation of intimate partner violence [20]. A direct relationship between global stress during the COVID-19 lockdown period and intimate partner violence has also been identified [21]. A systematic review investigating the changes in the prevalence and severity of domestic violence before the pandemic, and during the social mobility restrictions in 2020, found that, despite the increase in the severity of emotional, psychological, and sexual violence in the general population, no conclusive evidence could be found regarding changes in the prevalence of physical violence. This review also highlighted the scarcity of studies reporting men as victims [22].
On the other hand, alcohol consumption has been identified as one of the main risk factors for cancer, accidents, and communicable diseases, leading to premature death and disability worldwide [23]. The burden of disease related to alcohol consumption varies depending on the type of consumption: the highest average volume of alcohol consumed is more related to chronic consequences such as cancer, diseases derived from alcohol abuse, and liver and infectious diseases, while excessive consumption of alcoholic beverages in a short period, or binge drinking (BD), is more associated with ischemic and cardiovascular diseases, accidents, and communicable diseases [24]. BD varies in different populations and even between regions and is conditioned by social situations and norms, cultural, religious, and socioeconomic features; differences can even be observed throughout the life cycle. It is more common in men than in women and in early life stages (for example, during adolescence and youth) [25,26,27]. A relevant factor affecting BD is the alcohol content and the price of the different types of alcoholic beverages available in each area, which includes non-registered alcoholic beverages, such as fermented beverages and craft liqueurs [28]. BD refers to men consuming five or more alcoholic drinks and women consuming four or more within a two-hour period [29]. Increasing age, transition to different stages of life, greater accessibility, having home drinking habits, and tobacco consumption, as well as a low educational level, are all factors associated with BD [27,30]. Alcohol reduces the concentrations and sensitivity of brain serotonin and norepinephrine, depresses the nervous system [31], is detrimental to cognitive functioning, and causes disinhibition, which is why it is associated with the use of psychoactive drugs, aggressive behavior [28,30], drunk driving, and non-consensual sexual relations. Therefore, BD represents a public health issue worldwide [32].
As evidenced at a global level, intimate partner physical violence requires urgent attention and is associated with alcohol consumption [33]. On the other hand, being a victim of intimate partner violence is a traumatic event that leaves multiple chronic problems [15]. In Brazil, the male victim population showed excessive alcohol consumption [34]. Similarly, in Missouri, in 2015, intimate partner violence was found to be associated with smoking, a sedentary lifestyle, obesity, and BD in victims, as well as with a lack of motivation, fear, and trauma [35]. Among female victims from South Africa, excessive alcohol consumption was observed in 11.6% of cases, which was associated with childhood trauma, PTSD, depression, and bidirectional intimate partner violence [36]. Evidence suggests a bidirectionality and cyclical temporal dynamic between BD and IPV. The mechanisms in BD to victimization include settings where victims and perpetrators drink heavily, which increases disinhibited behaviors, as well as increased vulnerability to victimization. Contradictory IPV victims who commit BD after the aggression seek for an avoidant coping strategy, a distraction of psychological symptoms. Research in this last direction is less explored and there are some discrepant results, especially as these studies are been conducted predominantly in women [37].
In Peru, in 2018, 6.2% of women reported that their partners drank alcohol occasionally, while 52% of them stated that they had suffered physical violence when their partners were under the influence of alcohol [4]. Unfortunately, there are no values recorded for the male population. Although BD is known to exacerbate violent behaviors [32,35,36,38] worldwide, this reported consumption focuses on male perpetrators and female victims, but not on both female and male victims of violence in the same population [10,22]. For this reason, this study aimed to identify the association between physical violence by an intimate partner and BD in both male and female victims in Peru, during 2020.
2. Materials and Methods
This was a secondary analytical cross-sectional study that uses the ENDES (Demographic and Family Health Survey) 2020 database from the INEI (National Institute of Statistics and Information Technology). This study opted for a probability, balanced, stratified, and independent two-stage sample, which was carried out at the department level, considering urban and rural areas, and that regarded the dwelling as the sample unit [39].
The population consisted of Peruvian men and women aged 15 years or older in 2020. The study comprised those people meeting the inclusion criteria, such as being 15 years or older, being selected for the ENDES Health Questionnaire and having answered “yes” to the question of whether they had been married or in communal living situation in the last 12 months [40]. Those who did not answer questions regarding alcohol consumption and the frequency with which they had suffered physical violence by their intimate partners, with any part of the body or object during the last 12 months, were excluded. Lastly, pregnant women were also excluded [41,42].
2.1. Characteristics of the Primary Study
The primary study collected data about demographic health indicators in Peru [43]. The sampling framework of the ENDES 2020 was based on the statistical and cartographic information of the 11th Population Census and 6th Housing Census 2007, with the respective updates of the Household Targeting System (SISFOH, by its Spanish acronym) in 2012 and 2013, in addition to the 12th National Population Census and the 7th National Housing Census 2017 (PHC 2017) [39]. In this study, a probability, balanced, stratified, and independent two-stage sample was chosen. The study was conducted at the department level and based on urban and rural areas. Regarding urban areas, the sampling unit used considered conglomerate and private housing, while in rural areas, sampling was carried out based on the rural census area and private housing. For ENDES 2020, 37 to 390 homes were used: 15,098 dwellings in department capitals and in the 43 districts of metropolitan Lima; 9490 dwellings corresponding to the rest of the urban area and 12,802 dwellings from rural areas [39].
The power of the study was estimated using the statistical software Open Epi version 3.01, considering a 95% confidence interval and 14.5% prevalence of BD in female victims of intimate partner violence, and 36.3% of excessive alcohol consumption in male victims of intimate partner violence [43]. In the general population, 8.4% of women and 22.8% of men reported excessive alcohol consumption. Considering the information from ENDES 2020, which shows 238 men exposed to physical aggression by their intimate partner and 9685 unexposed, as well as 529 women exposed and 10,164 unexposed, the estimation was made by sex, and a power greater than 80% was identified considering a design effect of two.
2.2. Variables
The main independent variable was physical violence by the intimate partner in the last 12 months, according to sex. It was elaborated from questions asking whether the participant had been attacked by his or her partner in the last 12 months with any part of the body or an object, and the number of times. Each question was categorized as a dichotomous variable depending on the presence or absence of physical aggression by the intimate partner, considering “0” or “no” if the answer was never/do not remember, while “1” or “yes” was introduced when the answer was “rarely”, “sometimes” or “often”. Should the answer be “no” for both questions, the person was disregarded as a victim of physical violence by the intimate partner. Conversely, “yes” was recorded when any of the questions had an affirmative answer [40].
The dependent variable was excessive alcohol consumption in the last 30 days. The standard by the Center for Disease Control and Prevention (CDC) was used to measure it, which implies that a blood alcohol concentration between three and four grams increases the risk of suffering health consequences such as injuries, violence, accidents, and risky sexual behavior, among others [44]. A drink is defined as a beverage containing between 12 to 14 g of ethanol and that increases blood alcohol content by more than 0.08 g/dL [45].
In this study, the ethanol content was considered based on the type of alcoholic beverage consumed, to identify the number of drinks. One drink is equivalent to 300 mL of beer at 5%, 140 mL of wine or spirituous drinks at 12%, or 40 mL of liquors or distillates at 40% [46]. These data come from the ENDES question: “Have you drunk alcohol ‘more than once’ in the last 30 days? ”, and from the questions: “Think about the time you drank the most”, together with the specification of the type of alcoholic beverage, the quantity and number of glasses or bottles [40]. Excessive consumption was identified as “yes” or “1” if women had consumed the equivalent of four drinks or more according to the type and quantity of beverage on one single occasion during the last 30 days, or to the equivalent of five or more drinks according to the type and amount of drink in the case of men [45]. If the number of drinks was less, “no” or “0” was recorded.
Both variables considered a period of time, so that the physical violence by an intimate partner considers the last 12 months, while the excessive consumption of alcohol was measured by reporting the time that the largest amount of alcohol was consumed in the last 30 days.
Other variables considered in this study were the following: age in years; sex; educational level attained; marital status; area of residence (urban or rural); socioeconomic status classified in quintiles according to the characteristics of the dwelling; availability of specific goods and services according to the methodology adopted by the INEI [47]; ethnic self-identification; tobacco consumption in the last 30 days; and symptoms of depression in the last 14 days, measured by nine questions adapted from the PHQ9 scale with a score between 0 and 27, (0 to 4 being none or minimal symptoms, 5 to 9, mild symptoms, 10 to 14, moderate symptoms, 15 to 19, moderately severe symptoms and 20 to 27, severe symptoms). As a cut-off point, a score ≥10 was considered due to its high sensitivity and specificity for major depression [48,49], in addition to the type of alcoholic beverage most frequently consumed on more than one occasion during the last 30 days, such as beer, wine, anisette, etc.
2.3. Study Procedures
Procedures from ENDES to collect information on alcohol consumption and intimate partner violence included face-to-face interviews, which were conducted on site until March 16, due to the COVID-19 pandemic. Face-to-face activities resumed as of June 30. During this time span, the INEI adapted information from indicators that could be answered effectively by telephone. Likewise, during July to September, an information recovery strategy requiring attendance was implemented. Questions on intimate partner violence and alcohol consumption during the last 30 days, together with the type and quantity of drinks, remained in the face-to-face interviews [50].
The ENDES 2020 had a survey work team included a local supervisor, interviewers, and an anthropometrist [46]. The Health Questionnaire, which included the questions of the independent and dependent variables, considered one person aged 15 years or older per household, in which the ENDES was applied [46]. In the case of the dependent variable BD, the purpose was to know the amount of standardized alcohol drinks consumed in the last 30 days by people over 15 years of age, for which an Alcoholic Beverages Card was used to obtain the corresponding information. [46].
2.4. Statistical Analysis
The statistical analysis was performed using the STATA® MP17 software with a confidence interval of 95%. For the entire analysis, the weights, primary sampling units, and strata were considered, using the svyset commands. For the descriptive analysis, the categorical variables were presented in frequencies, weighted percentages, and confidence intervals for the sociodemographic features and problematic behaviors in the population over 15 years of age in Peru in the year 2020. For the bivariate analysis, Pearson’s chi-squared test was used with Rao–Scott correction.
In order to identify the association between physical violence by an intimate partner and BD in the victim, a multivariable analysis was performed using a generalized linear model of the family, and Poisson log-link option in the crude and general adjusted model and in adjusted models stratified according to sex. Being a cross-sectional study, the results were presented as prevalence ratios (PRs). To enter the variables in the adjusted model, an epidemiological criterion was considered and multicollinearity was checked using the variance inflation factor with a reference value of 10. No higher value was found. Likewise, the correlation between the variables included in the adjusted model was reviewed using the estat vce command, correlation with a 0.5 criterion, and no correlation between the variables included in the adjusted models could be found.
The variables considered in the adjusted model were: age, socioeconomic level, sex, educational level, area of residence, ethnic self-identification, presence of depressive symptoms during the last 14 days, and tobacco consumption during the last 30 days [12,30,36,51].
3. Results
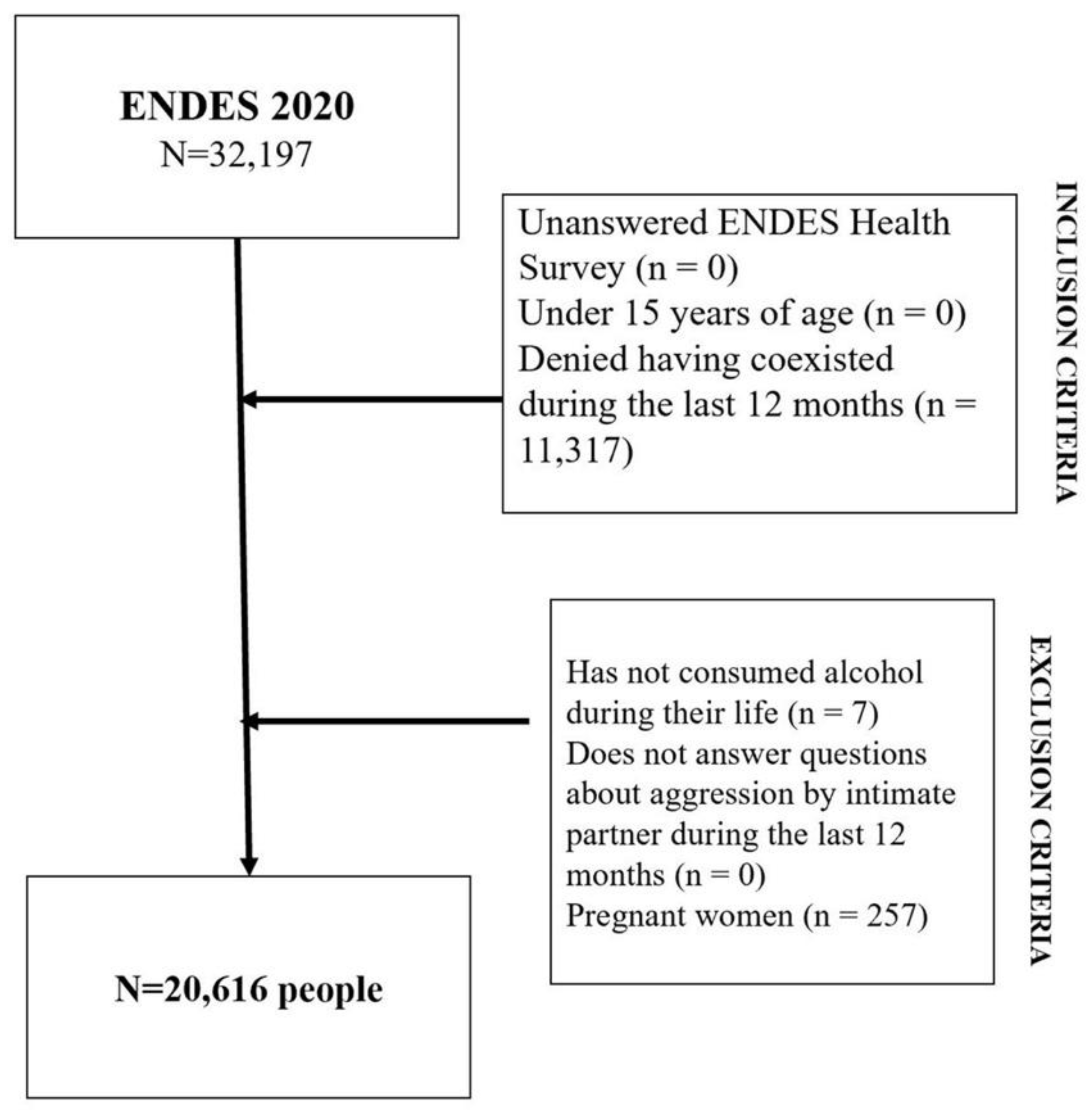
A total number of 20,616 people met the selection criteria for this study (Figure 1). Of the 11,317 participants who declared not having lived with a partner during the last 12 months, 6414 were women (54.2%) and 4903 were men (45.8%). As shown in Table 1, nearly seven out of 10 were 35 years old or older (66.8%), half of them were men (50.7%), almost five out of 10 identified themselves as being mestizos (48.4%), almost eight out of 10 lived in an urban area (78.9%), and more than two out of 10 had completed primary education or less (24%).
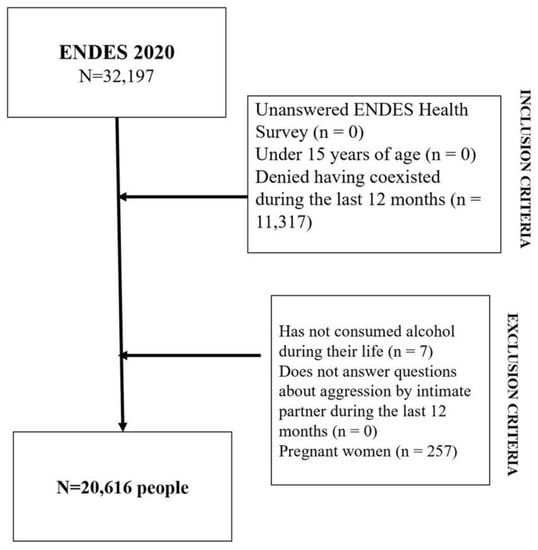
Figure 1.
Flowchart showing data obtained from the population through inclusion and exclusion criteria.

Table 1.
General characteristics of the population older than 15 years of age in Peru 2020 (n = 20,616).
According to Table 2 and regarding problem behaviors according to sex, a higher percentage of women who had not consumed any type of alcoholic beverage in the last 30 days could be observed when compared to that of men (84.6% vs. 78.0%, respectively, p < 0.001). Women were found to present a greater depressive symptomatology (from moderate to more than moderate) than men (7.5% vs. 3.9%, respectively, p < 0.001). On the other hand, having been a victim of physical aggression by an intimate partner in the last 12 months was more common among women than in men (4.7% vs. 3.0%, respectively, p < 0.001).

Table 2.
Problem behaviors according to sex in the population older than 15 years of age in Peru 2020 (n = 20,616).
Table 3 shows the association between sociodemographic characteristics and BD in individuals. The study found that 10.2% of the population BD. It is evident that the male sex (15.1%) has a higher rate of BD than female participants (7.1%). The population under 35 years of age presented higher rates of BD than those over 35 (30% and 17.8%, respectively, p < 0.001). Individuals who self-identified as Quechua and Aymara presented lower binge-drinking rates compared to Afro-descendants, Caucasians, and Mestizos (9.3% and 8.8% vs. 13.3%, 12.1%, and 11.7%, respectively, p < 0.001). People belonging to the bottom quintile were less prone to BD than those from the top quintile (6.3% vs. 14.4%, respectively, p < 0.001). On the other hand, coast inhabitants had a higher excessive consumption of alcohol compared to jungle and mountain dwellers (12.3%, 11.7%, and 8.0%, respectively, p < 0.001). In addition, people consuming tobacco in the last 30 days presented higher BD rates compared with those who had not consumed it (34.8% vs. 10.9%, respectively, p < 0.001).

Table 3.
Association between sociodemographic characteristics and excessive alcohol consumption in individuals (n = 20,616).
With regards to the association between physical violence by an intimate partner and BD, Table 4 shows in the crude model that people who suffered physical violence by their intimate partner have a 90% greater likelihood of BD, when compared with those who did not suffer it (PRc 1.9, 95% CI 1.5–2.5, p < 0.001). Likewise, when adjusting for sex, age, self-identification, socioeconomic status, educational level, area of residence, tobacco consumption in the last 30 days, and depressive symptoms, the study found a 90% greater probability of BD (PRa 1.9, 95% CI 1.4–2.5, p < 0.001). In the sex-adjusted models, a 90% greater probability of BD was observed in men who were victims of violence, while in the female population the percentage was 80% (PRa 1.9, 95% CI 1.3–2.7, p < 0.05 vs. PRa 1.8, CI 1.1–2.8, p < 0.05, respectively).

Table 4.
Association between intimate partner physical aggression and excessive alcohol consumption in the population over 15 years of age in Peru 2020 (n = 20,616).
4. Discussion
This study has found an association between being a victim of physical violence by an intimate partner and BD in men and women over 15 years of age in Peru. This association of victimization and BD is different from what was identified in a previous study in Brazil, where it could only be demonstrated in male victims, but not in females (OR 2.37, 95% CI 1.2; 4.9 and OR 1.17, 95% CI 0.6; 2.5, respectively) [34]. On the other hand, research conducted in the United States showed similar results as this study, revealing an association between being a victim of physical violence by an intimate partner and BD in both men and women [52]. In a longitudinal study of adolescents of both sexes, this association was also identified. One of the explanations considers that the personality and characteristics of people who engage in BD make them more vulnerable to becoming victims of intimate partner violence and choosing violent partners. Moreover, the social background in which this consumption occurs makes them more prone to sexual harassment, and their behavior under the influence of alcohol makes them even more susceptible to becoming victims of physical aggression by their intimate partner [53]. It is important to consider the COVID-19 context, since the research is based on data obtained throughout 2020, and therefore, most of this information was obtained under confinement conditions in which the couples’ relationships suffered modifications [17,19]. Similarly to the findings in the US, high levels of stress in couples during COVID-19 is related to a high number of physical violence attacks by the intimate partner, associated with risk behaviors such as those presented in this study [21].
As evidenced by other longitudinal studies [34,53], the abuse is not unidirectional, nor is it an isolated episode, but it is part of a cycle of abuse that can begin with violence or BD [54]. The latter can be the response by the victim or the perpetrator to the abuse [30], or a trigger for the perpetrator. However, the most frequently observed pattern in the victim is anticipation and fear of abuse [54]. Besides, behaviors against physical aggression are of the dose-response type. In other words, they are cumulative; the greater the violence, the riskier the behavior. It is important to highlight the contrast in the consumption between the rural and urban population, as people who live in rural areas tend to present lower excessive consumption of alcohol associated with a weaker culture of consumption and a more complicated access to alcohol [55]. Therefore, this is another factor that is included in the cycle of abuse, in addition to educational level, socioeconomic status, tobacco consumption [51], the presence of depression [56], age, and sex [34].
Some proposed mechanisms for understanding BD as a consequence of partner or ex-partner victimization in men or women include the interaction of factors at different levels, such as individual characteristics and background. For example, genetics, personality, the level of self-esteem, adverse childhood events, and alcohol consumption may condition a greater predisposition to conscious or unconscious binge drinking in response to negative psychological symptoms resulting from victimization, either from the incident or from incident-related problems, according to the dose-response hypothesis [57,58]. In addition to allowing that in some cases this excessive consumption, which was given as an action to buffer the symptoms, instead of achieving the desired effect, results in more negative emotions generating a vicious cycle [59].
This interaction also encompasses factors at the relationship level, such as the type of partner (e.g., current partner, ex-partner, same sex partner), alcohol consumption (habitual use, frequency of BD, relation to the perpetration of violence), and characteristics of the place where the violence and excessive alcohol consumption occur, whether in private and alone or in bars, parties or social gatherings, or others [60]. Further, social factors and the cultural norms of each setting have a role here, such as social stigmatization and the resources available to identify, prevent and manage IPV and BD situations, which may vary in different populations and cultures [37]. Additionally, alcohol is not exclusive to binging; food and substance abuse are included as well [61,62].
The female victims of intimate partner violence (whether physical, sexual, or psychological) most likely present schizoid, schizotypal, “borderline”, paranoid personality traits; they also have low self-esteem, little attachment to their families and 40% of them even blame themselves for the abuse [63]. Likewise, the cycle of abuse in women is associated with the presence of child abuse, depression, as well as with post-traumatic stress disorder [36]. The culture of alcohol consumption is less prevalent among women [23]. Although women also show excessive consumption of alcohol, social and work isolation, and depressive symptoms, are more common [30,56]. In the case of the male sex, there is often a previous history of child abuse, violence normalization, and a culture of domestic violence. For men, experiencing intimate partner aggression directly contravenes the generalized stereotype of the “superiority” of men over women in Western and patriarchal cultures [64], and their victimization is taboo, being therefore under-reported and stigmatized in most cultures and countries [64,65]. Their personality is associated with lability and being complacent. The most common type of violence is psychological [64]. Regarding men’s response to excessive alcohol consumption, it is globally known that too much drinking is synonymous with “drinking as a man”, so culturally, men have a greater tendency to consume in excess [64,66]. Consequently, when faced with aggression by an intimate partner, one of the most frequent coping strategies is BD [66].
In 2019, it was found that 10% of women between 15 and 49 years old had been victims of physical violence by their intimate partner in the last 12 months. Conversely, for 2020, this study focused on the population over 15 years of age according to sex, and found that 4.7% of women and 3% of men had been victims of intimate partner violence. Regarding alcohol consumption, the national indicators of the ENDES for 2020 report prevalence values of disorder by alcohol abuse in both men (5.2% of the population) and women (0.8%) [50]. A contribution of our study is the information about BD in 2020, which was 10.2% (15.1% in men and 7.1% in women), indicating a lower prevalence of BD than that reported for the Japanese population, which was of 29.3%, being higher for men than for women (40.6% vs. 18.7%, respectively). The measurement of excessive consumption followed the same CDC criteria and included the last 30 days; however, for the sake of convenience, the study was carried out online in a population over 18 years of age, to which only one-fifth of those invited to participate responded [65]. The prevalence of excessive alcohol consumption varies according to the way in which consumption is measured. The prevalence of excessive consumption changed in 2020. It increased in some people and decreased in others, due to the social circumstances of isolation related with the pandemic [67,68].
This is one of the first studies to identify the association between physical violence perpetrated by an intimate partner and BD according to sex in the Peruvian population. However, despite being a novel and nationally-representative study, it has some limitations. One of them is the design of the study which, being cross-sectional, did not allow to show the direction in which the variables interact, the path between BD and victimization and vice versa, and even the exercise of bidirectional violence within the couple. Additionally, the data used to conduct the study did not specify the gender of the interviewees’ partner or their sexual orientation. It is known that there are homosexual and heterosexual couples in Peru, so it is important to be able to discriminate between violence from both types of couples, information that is not available for this study. Currently, an increase in same-sex couples’ violence has been observed, but there are still limitations for the study of these cases [53]. During the investigation, we could detect another important limitation, which is the lack of questions about the emotional or sexual violence exerted on men, which restricts the investigation only to physical violence and limits the real impact of all types of violence against men. This aspect is relevant, since a systemic review found that the most prevalent violence exerted on men is psychological [64]. Additionally, there is a gap in information about the identity of the perpetrator of violence. Even though questions inquire if, in the last 12 months, they have been living with a partner, and if they have been a victim of physical violence by them, it does not specify the time period in which the physical violence occurred, if there has been more than one partner in that period of time, nor if it was their current partner but also a previous partner [60]. On the other hand, neither religion nor the consumption of other substances were included in the variables.
Despite the training and standardization of interviewers and supervisors of the Peruvian Demographic Health Survey in highly sensitive issues such as violence, the validation and review of how questions were asked, the selection of language, the training in situations such as the presence of other people during the interview, and the interviewer’s attitude, can influence the estimation of violence, possibly biased toward violence underestimation. This also affects in more recent and severe cases [69,70].
A memory bias could have been present due to the period of time considered in the questions, as well as a desirability bias, since the interviewee could have thought that some of the answers were more socially acceptable. Due to the fact that the information had already been collected, no further investigation could be carried out on aspects not included in the original study (such as the number of partners, whether the aggressor partner lived with the victim, or if the aggressor’s partner and the victim were married or cohabiting, in addition to other sociodemographic information about the couple). Likewise, no information could be gathered about participants’ history of violence during childhood, since the questions about violence were limited to the last 12 months.
5. Recommendations
The development of longitudinal studies including early exposure to violence, a history of post-traumatic stress disorder, depression, and patterns of alcohol consumption that delve into the causal association between BD and physical aggression, is suggested [35]. Additionally, the development of comparative studies between the years before and after the pandemic is recommended. Gender-based strategies concerning health should be applied to improve visibility and prevent intimate partner aggression against both men and women. Early identification of intimate partner violence and strategies to prevent BD in victims of violence should be our target.
6. Conclusions
The results of this study found an association between having been a victim of physical violence by an intimate partner and BD, in both men and women, in the Peruvian population over 15 years of age. It was identified that the prevalence of physical violence victimization was higher in women than in men (4.7% vs. 3%, respectively). Male and female victims of aggression were more susceptible to present an excessive consumption of alcohol, which was higher in men than in women. Further investigation on these findings is needed, with longitudinal studies taking into account genetic characteristics, as well as social and cultural determinants in various populations.
Author Contributions
M.d.l.C. and F.C. contributed to the conceptualization and research idea; M.d.l.C., F.C. and D.B.-W. contributed equally to the election and application of design, methodology, statistical analysis, validation, research data interpretation, writing of the first draft of the manuscript, critical review and editing of the actual version. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Universidad de Ciencias Aplicadas/UPC-EXPOST-2022-2.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the School of Health Sciences of the Universidad Peruana de Ciencias Aplicadas (Peruvian University of Applied Sciences) under number FCS-SCEI/1153-11-21.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. This research did not violate the principles of medical bioethics. Being information collected through the INEI from a database, the people who took part in the survey did so on a voluntary basis and their privacy was guaranteed, that is, the principle of the autonomy of the participants was followed. At no time during the investigation was a person exposed or segregated due to prejudices based on sex, ethnicity, educational level, or socioeconomic status, so the principle of nonmaleficence was applied.
Data Availability Statement
The data presented in this study are openly available at http://iinei.inei.gob.pe/microdatos/ (accessed on 9 October 2022).
Acknowledgments
To the Research Department of the Universidad Peruana de Ciencias Aplicadas for the support provided to carry out this research work through the professional editing for English language of the manuscript and the UPC-EXPOST-2022-2 incentive. To Martha Alvarez Ribera and Graciela Alvarez Provensal for their contribution in edition review.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tran, T.D.; Nguyen, H.; Fisher, J. Attitudes towards Intimate Partner Violence against Women among Women and Men in 39 Low- and Middle-Income Countries. PLoS ONE 2016, 11, e0167438. [Google Scholar] [CrossRef] [PubMed]
- Cripe, S.M.; Espinoza, D.; Rondon, M.B.; Jimenez, M.L.; Sanchez, E.; Ojeda, N.; Sanchez, S.; Williams, M.A. Preferences for Intervention Among Peruvian Women in Intimate Partner Violence Relationships. Hisp. Health Care Int. 2015, 13, 27–37. [Google Scholar] [CrossRef]
- Changing cultural and social norms that support violence. In Changing Cultural and Social Norms Supportive of Violent Behaviour; World Health Organization: Geneva, Switzerland, 2009; p. 15.
- INEI. Perú: Indicadores de Violencia Familiar y Sexual, 2012–2019: Lima. 2019. Available online: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1686/libro.pdf (accessed on 1 November 2022).
- Abramsky, T.; Watts, C.H.; Garcia-Moreno, C.; Devries, K.; Kiss, L.; Ellsberg, M.; Jansen, H.A.; Heise, L. What factors are associated with recent intimate partner violence? findings from the WHO multi-country study on women’s health and domestic violence. Bmc Public Health 2011, 11, 109. [Google Scholar] [CrossRef]
- Carthy, N.L.; Bates, E.A.; Policek, N. Promoting Inclusivity in Intimate Partner Abuse Research: Exploring Gender and Age. Partn. Abus. 2019, 10, 359–372. [Google Scholar] [CrossRef]
- Wörmann, X.; Wilmes, S.; Seifert, D.; Anders, S. Males as victims of intimate partner violence—Results from a clinical-forensic medical examination centre. Int. J. Leg. Med. 2021, 135, 2107–2115. [Google Scholar] [CrossRef] [PubMed]
- Tarzia, L.; Forsdike, K.; Feder, G.; Hegarty, K. Interventions in Health Settings for Male Perpetrators or Victims of Intimate Partner Violence. Trauma Violence Abus. 2020, 21, 123–137. [Google Scholar] [CrossRef]
- Amole, T.G.; Bello, S.; Odoh, C.; Aliyu, M.H.; Iliyasu, Z. Correlates of female-perpetrated intimate partner violence in Kano, Northern Nigeria. J. Interpers. Violence 2016, 31, 2240–2254. [Google Scholar] [CrossRef]
- Kolbe, V.; Büttner, A. Domestic Violence Against Men-Prevalence and Risk Factors. Dtsch. Ärzteblatt Int. 2020, 117, 534–541. [Google Scholar] [CrossRef]
- INEI. Informe Principal ENDES 2019: Peru. 2020. Available online: https://proyectos.inei.gob.pe/endes/2019/INFORME_PRINCIPAL_2019/INFORME_PRINCIPAL_ENDES_2019.pdf (accessed on 1 November 2022).
- Silva, A.N.; Azeredo, C.M. Associação entre vitimização por violência entre parceiros íntimos e depressão em adultos brasileiros. Ciência Saúde Coletiva 2019, 24, 2691–2700. [Google Scholar] [CrossRef]
- Aguerrebere, M.; Frías, S.M.; Fawzi, M.C.S.; López, R.; Raviola, G. Intimate partner violence types and symptoms of common mental disorders in a rural community of Chiapas, Mexico: Implications for global mental-health practice. PLoS ONE 2021, 16, e0256850. [Google Scholar] [CrossRef]
- Bauer, H.M.; Gibson, P.; Hernandez, M.; Kent, C.; Klausner, J.; Bolan, G. Intimate partner violence and high-risk sexual behaviors among female patients with sexually transmitted diseases. Sex. Transm. Dis. 2002, 29, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Rapport Mondial Sur La Violence Et La Santé: Résumé Genève; Organisation mondiale de la santé: Geneva, Switzerland. 2002. Available online: https://www.who.int/violence_injury_prevention/violence/world_report/en/summary_es.pdf (accessed on 1 November 2022).
- Herrero-Arias, R.; Truong, A.N.; Ortiz-Barreda, G.; Briones-Vozmediano, E. Keeping silent or running away. The voices of Vietnamese women survivors of Intimate Partner Violence. Glob. Health Action 2021, 14, 1863128. [Google Scholar] [CrossRef] [PubMed]
- Porter, C.; Favara, M.; Sánchez, A.; Scott, D. The impact of COVID-19 lockdowns on physical domestic violence: Evidence from a list randomization experiment. SSM-Popul. Health 2021, 14, 100792. [Google Scholar] [CrossRef]
- Gulati, G.; Kelly, B.D. Domestic violence against women and the COVID-19 pandemic: What is the role of psychiatry? Int. J. Law Psychiatry 2020, 71, 101594. [Google Scholar] [CrossRef]
- Abdo, C.; Miranda, E.P.; Santos, C.S.; Júnior, J.d.B.; Bernardo, W.M. Domestic violence and substance abuse during COVID-19: A systematic review. Indian J. Psychiatry 2020, 62, S337–S342. [Google Scholar] [CrossRef] [PubMed]
- Ceroni, T.L.; Ennis, C.R.; Franklin, C.L. The COVID-19 pandemic: Implications for intimate partner violence. Couple Fam. Psychol. Res. Pract. 2021. [Google Scholar] [CrossRef]
- Cannon, C.E.B.; Ferreira, R.; Buttell, F.; First, J. COVID-19, Intimate Partner Violence, and Communication Ecologies. Am. Behav. Sci. 2021, 65, 992–1013. [Google Scholar] [CrossRef]
- Thiel, F.; Büechl, V.C.S.; Rehberg, F.; Mojahed, A.; Daniels, J.K.; Schellong, J.; Garthus-Niegel, S. Changes in Prevalence and Severity of Domestic Violence During the COVID-19 Pandemic: A Systematic Review. Front. Psychiatry 2022, 13, 874183. [Google Scholar] [CrossRef]
- Griswold, M.G.; Fullman, N.; Hawley, C.; Arian, N.; Zimsen, S.R.; Tymeson, H.D.; Venkateswaran, V.; Tapp, A.D.; Forouzanfar, M.H.; Salama, J.S.; et al. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 392, 1015–1035. [Google Scholar] [CrossRef]
- Rehm, J.; Gmel Sr, G.E.; Gmel, G.; Hasan, O.S.; Imtiaz, S.; Popova, S.; Probst, C.; Roerecke, M.; Room, R.; Samokhvalov, A.V.; et al. The relationship between different dimensions of alcohol use and the burden of disease—An update. Addiction 2017, 112, 968–1001. [Google Scholar] [CrossRef]
- Silveira, C.M.; Silveira, C.C.; Da Silva, J.G.; Silveira, L.M.; De Andrade, A.G.; De Andrade, L.H.S.G. Epidemiology of heavy drinking and heavy episodic drinking in Brazil: A systematic review of literature. Rev. Psiquiatr. Clin. 2008, 35, 31–38. [Google Scholar] [CrossRef]
- Khamis, A.A.; Salleh, S.Z.; Ab Karim, M.S.; Mohd Rom, N.A.; Janasekaran, S.; Idris, A.; Abd Rashid, R.B. Alcohol Consumption Patterns: A Systematic Review of Demographic and Sociocultural Influencing Factors. Int. J. Environ. Res. Public Health 2022, 19, 8103. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Martínez, A.M.; Trapero-Bertran, M.; Mora, T.; Lima-Serrano, M. Social, economic and family factors associated with binge drinking in Spanish adolescents. BMC Public Health 2020, 20, 519. [Google Scholar] [CrossRef]
- Rehm, J.; Kailasapillai, S.; Larsen, E.; Rehm, M.X.; Samokhvalov, A.V.; Shield, K.D.; Roerecke, M.; Lachenmeier, D.W. A systematic review of the epidemiology of unrecorded alcohol consumption and the chemical composition of unrecorded alcohol. Addiction 2014, 109, 880–893. [Google Scholar] [PubMed]
- Spear, L.P. Effects of adolescent alcohol consumption on the brain and behaviour. Nat. Rev. Neurosci. 2018, 19, 197–214. [Google Scholar] [PubMed]
- Silumbwe, A.; Sabastian, M.S.; Michelo, C.; Zulu, J.M.; Johansson, K. Sociodemographic factors associated with daily tobacco smoking and binge drinking among Zambians: Evidence from the 2017 STEPS survey. BMC Public Health 2022, 22, 205. [Google Scholar] [CrossRef]
- Mosquera, J.T.; Menéndez, M.C. Un tóxico de alto riesgo para la salud humana socialmente aceptado. Rev. Fac. Med. 2006, 54, 32–47. [Google Scholar]
- Nasui, B.A.; Popa, M.; Buzoianu, A.D.; Pop, A.L.; Varlas, V.N.; Armean, S.M.; Popescu, C.A. Alcohol Consumption and Behavioral Consequences in Romanian Medical University Students. Int. J. Environ. Res. Public Health 2021, 18, 7531. [Google Scholar] [CrossRef]
- McKinney, C.M.; Caetano, R.; Harris, T.R.; Ebama, M.S. Alcohol Availability and Intimate Partner Violence among US Couples. Alcohol. Clin. Exp. Res. 2009, 33, 169–176. [Google Scholar] [CrossRef]
- Ally, E.Z.; Laranjeira, R.; Viana, M.C.; Pinsky, I.; Caetano, R.; Mitsuhiro, S.; Madruga, C.S. Intimate partner violence trends in Brazil: Data from two waves of the Brazilian National Alcohol and Drugs Survey. Braz. J. Psychiatry 2016, 38, 98–105. [Google Scholar] [CrossRef]
- Bosch, J.; Weaver, T.L.; Arnold, L.D.; Clark, E.M. The Impact of Intimate Partner Violence on Women’s Physical Health: Findings From the Missouri Behavioral Risk Factor Surveillance System. J. Interpers. Violence 2017, 32, 3402–3419. [Google Scholar] [CrossRef] [PubMed]
- Machisa, M.T.; Christofides, N.; Jewkes, R. Mental ill health in structural pathways to women’s experiences of intimate partner violence. PLoS ONE 2017, 12, e0175240. [Google Scholar]
- Dardis, C.M.; Ullman, S.E.; Rodriguez, L.M.; Waterman, E.A.; Dworkin, E.R.; Edwards, K.M. Bidirectional associations between alcohol use and intimate partner violence and sexual assault victimization among college women. Addict. Behav. 2021, 116, 106833. [Google Scholar] [CrossRef] [PubMed]
- Leonard, K.E. Alcohol and intimate partner violence: When can we say that heavy drinking is a contributing cause of violence? Addiction 2005, 100, 422–425. [Google Scholar] [PubMed]
- INEI. Ficha Técnica Encuesta Demografica de Salud 2020: Peru. 2020. Available online: http://iinei.inei.gob.pe/iinei/srienaho/Descarga/FichaTecnica/739-Ficha.pdf. (accessed on 1 November 2022).
- INEI. Documentos Metodologicos 2020. Available online: http://iinei.inei.gob.pe/microdatos/ (accessed on 1 November 2022).
- Teshome, A.; Gudu, W.; Bekele, D.; Asfaw, M.; Enyew, R.; Compton, S.D. Intimate partner violence among prenatal care attendees amidst the COVID-19 crisis: The incidence in Ethiopia. Int. J. Gynecol. Obstet. 2021, 153, 45–50. [Google Scholar] [CrossRef]
- Terplan, M.; McNamara, E.J.; Chisolm, M.S. Pregnant and Non-Pregnant Women with Substance Use Disorders: The Gap Between Treatment Need and Receipt. J. Addict. Dis. 2012, 31, 342–349. [Google Scholar] [CrossRef]
- Breiding, M.J.; Black, M.C.; Ryan, G.W. Chronic Disease and Health Risk Behaviors Associated with Intimate Partner Violence—18 U.S. States/Territories, 2005. Ann. Epidemiol. 2008, 18, 538–544. [Google Scholar] [CrossRef]
- El Consumo de Alcohol y su Salud | Hojas Informativas | Alcohol | CDC 2021. Updated 2021/05/11/T05:44:31Z. Available online: https://www.cdc.gov/alcohol/hojas-informativas/consumo-alcohol-salud.html (accessed on 1 November 2022).
- Binge Drinking Is a Serious But Preventable Problem of Excessive Alcohol Use | CDC 2020. updated 2020/07/27/T09:54:24Z. Available online: https://www.cdc.gov/alcohol/fact-sheets/binge-drinking.htm (accessed on 1 November 2022).
- INEI. Manual de Encuesta de Salud Encuesta Demografica de Salud Peru 2020. 2020. Available online: http://iinei.inei.gob.pe/iinei/srienaho/Descarga/DocumentosMetodologicos/2020-5/CuestionarioSalud.pdf (accessed on 1 November 2022).
- INEI. Metodologias Estadisticas: Pobreza. 2021. Available online: https://www.inei.gob.pe/estadisticas/metodologias/ (accessed on 1 November 2022).
- Calderón, M.; Gálvez-Buccollini, J.A.; Cueva, G.; Ordoñez, C.; Bromley, C.; Fiestas, F. Validación de la versión peruana del PHQ-9 para el diagnóstico de depresión. Rev. Peru. Med. Exp. Salud Pública 2012, 29, 578–579. [Google Scholar] [CrossRef]
- Gilbody, S.; Richards, D.; Brealey, S.; Hewitt, C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): A diagnostic meta-analysis. J. Gen. Intern. Med. 2007, 22, 1596–1602. [Google Scholar] [CrossRef]
- INEI. Informe Principal ENDES 2020. 2021. Available online: https://proyectos.inei.gob.pe/endes/2020/INFORME_PRINCIPAL_2020/INFORME_PRINCIPAL_ENDES_2020.pdf (accessed on 1 November 2022).
- Veloso, C.; Monteiro, C.F.d.S. Consumption of alcohol and tobacco by women and the occurrence of violence by intimate partner. Texto Contexto-Enferm. 2019, 28, e20170581. [Google Scholar] [CrossRef]
- Davis, J.P.; Dumas, T.M.; Berey, B.L.; Merrin, G.J.; Cimpian, J.R.; Roberts, B.W. Effect of victimization on impulse control and binge drinking among serious juvenile offenders from adolescence to young adulthood. J. Youth Adolesc. 2017, 46, 1515–1532. [Google Scholar] [CrossRef] [PubMed]
- Waterman, E.A.; Lee, K.D.M.; Edwards, K.M. Longitudinal Associations of Binge Drinking with Interpersonal Violence Among Adolescents. J. Youth Adolesc. 2019, 48, 1342–1352. [Google Scholar] [CrossRef] [PubMed]
- Wilson, I.M.; Graham, K.; Taft, A. Living the cycle of drinking and violence: A qualitative study of women’s experience of alcohol-related intimate partner violence. Drug Alcohol Rev. 2017, 36, 115–124. [Google Scholar] [CrossRef]
- Devries, K.M.; Child, J.C.; Bacchus, L.J.; Mak, J.; Falder, G.; Graham, K.; Watts, C.; Heise, L. Intimate partner violence victimization and alcohol consumption in women: A systematic review and meta-analysis. Addiction 2014, 109, 379–391. [Google Scholar] [CrossRef]
- Archie, S.; Kazemi, A.Z.; Akhtar-Danesh, N. Concurrent binge drinking and depression among Canadian youth: Prevalence, patterns, and suicidality. Alcohol 2012, 46, 165–172. [Google Scholar] [CrossRef]
- Khantzian, E.J. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harv. Rev. Psychiatry 1997, 4, 231–244. [Google Scholar] [CrossRef]
- Khantzian, E.J. The self-medication hypothesis revisited: The dually diagnosed patient. Prim. Psychiatry 2003, 10, 47–54. [Google Scholar]
- Overup, C.S.; DiBello, A.M.; Brunson, J.A.; Acitelli, L.K.; Neighbors, C. Drowning the pain: Intimate partner violence and drinking to cope prospectively predict problem drinking. Addict. Behav. 2015, 41, 152–161. [Google Scholar] [CrossRef]
- Johnson, M.P.; Leone, J.M.; Xu, Y.L. Intimate Terrorism and Situational Couple Violence in General Surveys: Ex-Spouses Required. Violence Against Women 2014, 20, 186–207. [Google Scholar] [CrossRef]
- Yalch, M.M.; Christodoulou, J.; Rotheram-Borus, M.J.; Tomlinson, M. Longitudinal Association Between Intimate Partner Violence and Alcohol Use in a Population Cohort of South African Women. J. Interpers. Violence 2022. [Google Scholar] [CrossRef]
- Ullman, S.E.; Sigurvinsdottir, R. Intimate Partner Violence and Drinking Among Victims of Adult Sexual Assault. J. Aggress. Maltreat. Trauma 2015, 24, 117–130. [Google Scholar] [CrossRef]
- Adan, A.; Forero, D.A.; Navarro, J.F. Personality Traits Related to Binge Drinking: A Systematic Review. Front. Psychiatry 2017, 8, 134. [Google Scholar] [CrossRef] [PubMed]
- Scott-Storey, K.; O’Donnell, S.; Ford-Gilboe, M.; Varcoe, C.; Wathen, N.; Malcolm, J.; Vincent, C. What About the Men? A Critical Review of Men’s Experiences of Intimate Partner Violence. Trauma Violence Abus. 2022. [Google Scholar] [CrossRef] [PubMed]
- Hellemans, S.; Loeys, T.; Dewitte, M.; De Smet, O.; Buysse, A. Prevalence of intimate partner violence victimization and victims’ relational and sexual well-being. J. Fam. Violence 2015, 30, 685–698. [Google Scholar] [CrossRef][Green Version]
- Fugitt, J.L.; Ham, L.S. Beer for “brohood”: A laboratory simulation of masculinity confirmation through alcohol use behaviors in men. Psychol. Addict. Behav. 2018, 32, 358. [Google Scholar] [CrossRef]
- Stickley, A.; Shirama, A.; Inagawa, T.; Sumiyoshi, T. Binge drinking in Japan during the COVID-19 pandemic: Prevalence, correlates and association with preventive behaviors. Drug Alcohol Depend. 2022, 234, 109415. [Google Scholar] [CrossRef]
- Patrick, M.E.; Terry-McElrath, Y.M.; Miech, R.A.; Keyes, K.M.; Jager, J.; Schulenberg, J.E. Alcohol use and the COVID-19 pandemic: Historical trends in drinking, contexts, and reasons for use among US adults. Soc. Sci. Med. 2022, 301, 114887. [Google Scholar] [CrossRef]
- Abramsky, T.; Harvey, S.; Mosha, N.; Mtolela, G.; Gibbs, A.; Mshana, G.; Lees, S.; Kapiga, S.; Stöckl, H. Longitudinal inconsistencies in women’s self-reports of lifetime experience of physical and sexual IPV: Evidence from the MAISHA trial and follow-on study in North-western Tanzania. BMC Women Health 2022, 22, 120. [Google Scholar] [CrossRef]
- Singh, A.; Kumar, K.; Arnold, F. How Interviewers Affect Responses to Sensitive Questions on the Justification for Wife Beating, the Refusal to have Conjugal Sex, and Domestic Violence in India. Stud. Fam. Plan. 2022, 53, 259–279. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).