Abstract
Introduction: Adverse events in hospitals are prevented through risk reduction and reliable processes. Highly reliable hospitals are grounded by a robust patient safety culture with effective communication, leadership, teamwork, error reporting, continuous improvement, and organizational learning. Although hospitals regularly measure their patient safety culture for strengths and weaknesses, there have been no systematic reviews with meta-analyses reported from Latin America. Purpose: Our systematic review aims to produce evidence about the status of patient safety culture in Latin American hospitals from studies using the Hospital Survey on Patient Safety Culture (HSOPSC). Methods: This systematic review was guided by the JBI guidelines for evidence synthesis. Four databases were systematically searched for studies from 2011 to 2021 originating in Latin America. Studies identified for inclusion were assessed for methodological quality and risk of bias. Descriptive and inferential statistics, including meta-analysis for professional subgroups and meta-regression for subgroup effect, were calculated. Results: In total, 30 studies from five countries—Argentina (1), Brazil (22), Colombia (3), Mexico (3), and Peru (1)—were included in the review, with 10,915 participants, consisting primarily of nursing staff (93%). The HSOPSC dimensions most positive for patient safety culture were “organizational learning: continuous improvement” and “teamwork within units”, while the least positive were “nonpunitive response to error” and “staffing”. Overall, there was a low positive perception (48%) of patient safety culture as a global measure (95% CI, 44.53–51.60), and a significant difference was observed for physicians who had a higher positive perception than nurses (59.84; 95% CI, 56.02–63.66). Conclusions: Patient safety culture is a relatively unknown or unmeasured concept in most Latin American countries. Health professional programs need to build patient safety content into curriculums with an emphasis on developing skills in communication, leadership, and teamwork. Despite international accreditation penetration in the region, there were surprisingly few studies from countries with accredited hospitals. Patient safety culture needs to be a priority for hospitals in Latin America through health policies requiring annual assessments to identify weaknesses for quality improvement initiatives.
1. Introduction
All human work involves a margin of error [1,2], and health care is no exception [3,4]. Despite years of advancements since the seminal report “To Err Is Human” [5], patient safety continues to be a leading public health problem across countries [6]. Each year, 5.7 to 8.4 million deaths are attributed to poor-quality health services in low- and middle-income countries [7]. Errors in hospitals contribute to at least 15% of hospital costs in the countries of the Organization for Economic Cooperation and Development (OECD), which represents the most economically developed and socially advanced countries in the world [8]. People hospitalized in countries with developing economies are at higher risk for harm from health services because of resource scarcity and the fragility of facilities [9].
The Global Patient Safety Action Plan 2021–2030 urgently recommended that hospitals develop patient safety cultures to reduce the risk of errors and mitigate the harm caused by adverse events [10]. According to Sorra and Dyer [11], patient safety culture refers to the “management and staff values, beliefs, and norms about what is important in a health care organization, how organization members are expected to behave, what attitudes and actions are appropriate and inappropriate, and what processes and procedures are rewarded and punished with regard to patient safety” (p. 1). Creating the conditions for a patient safety culture requires mutual respect, professional collaboration, and the personal support of leaders, clinicians, and staff throughout the care delivery system [12]. Most importantly, the culture needs to shift to a shared mindset that positions patient safety as an important organizational outcome [13]. As such, everyone must be concerned with identifying and reporting latent, or hidden, system errors [14] through nonpunitive error reporting systems [15]. Furthermore, active errors resulting in adverse events should result in a blameless root cause analysis focused on prevention rather than punishment [16]. Resilience to system errors is a quality improvement strategy [17] resulting from an organization-wide concern with failure [18].
At the foundation of a robust patient safety culture is a balance of accountability and patient safety [19]. As a multidimensional organizational attribute linked to quality assurance [20], patient safety cultures positively impact leadership styles, ethical values, communication processes, evidence-based practices, organizational learning, continuous improvement, and person-centered care [21]. Leaders encourage all members of an organization to report latent errors identified from unreliable processes and prepare the organization to manage unexpected system failures caused by active errors [22]. Leaders cultivate positive cultures by affecting the attitudes and behaviors of people, as individuals and units, to embrace patient safety as the normative approach to working with people and caring for patients [23]. With effective leadership and continuous improvement, patient safety becomes a shared organizational property, embedded in the culture, with a collaborative lived experience within units, across departments, and throughout the organization [24]. Hospitals with excellent patient safety cultures have low-risk processes, exhibit highly reliable systems, and produce exceedingly effective outcomes [25].
2. Background
Measuring the patient safety culture of hospitals has been an important strategy to identify key areas for continued quality improvement [26] to strengthen patient safety as an organization-wide attribute. Hospital leaders need yearly patient safety culture assessments to learn how to work more effectively with people and where to focus resources to improve system processes, work procedures, and professional practices. Multiple instruments have been developed to measure hospital safety culture, including the Safety Attitudes Questionnaire [27], Safety Organizing Scale [28], and Hospital Survey on Patient Safety Culture (HSOPSC) versions 1.0 [29] and 2.0 [30].
Despite differences in theoretical foundations [31] and conceptual frameworks [32], the instruments similarly focus on measuring seven dimensions of patient safety culture including leadership support, staff attitudes, communication openness, safety systems, incident reporting, organizational learning: continuous improvement, and teamwork [33]. The patient safety culture instrument most often used for research across contexts, cultures, and countries is the HSOPSC [34], which originates from the Surveys on Patient Safety Culture™ program to advance the scientific understanding of patient safety culture in healthcare [35]. Since the release of the HSOPSC 1.0 in 2004, the survey has been translated into 56 languages and dialects for cross-cultural application in more than 100 countries [36]. In addition, studies have been published in journals from at least 32 countries in different regions of the world [37], including China [38], Colombia [39], Croatia [40], Ethiopia [41], Japan [42], Kuwait [33], Norway [43], Peru [44], Spain [45], and others [33,46]. Researchers have also begun to report data from studies using the translated version of the HSOPSC 2.0 [47,48], which was released at the end of 2019 [49].
2.1. Hospital Survey on Patient Safety Culture
The HSOPSC 1.0 [50,51] is a 42-item survey with 12 composites, or dimensions, for measuring perceptions about patient safety culture. Each dimension is measured with 3 to 4 items using a 5-point Likert scale with responses ranging from “totally disagree” to “totally agree” or from “never” to “always”. Each dimension and the global measure of patient safety culture can be analyzed at different levels, including individual, unit, department, hospital, and health system. An outcome variable of the survey (overall patient safety grade) is scored as “failing” to “excellent” on a five-point Likert scale [11]. Demographic information provides details about profession (e.g., administrator, nurse, pharmacist, or physician), organization work role (e.g., clerical staff, clinicians, supervisor, manager, or leader), and clinical specialty (e.g., cardiology, critical care, or orthopedics).
The HSOPSC 2.0 [52,53] is a 32-item survey with 10 dimensions. Although HSOPSC 1.0 and 2.0 measure the same areas of patient safety culture, the 2.0 version resulted in substantial changes, including 21 items dropped, 25 items reworded or response options changed, and 10 items added. Early findings suggest that translated versions of the HSOPSC 2.0 will perform better in international hospital environments than original version translations [54]. The HSOPSC 1.0 and 2.0 are available at the Agency for Healthcare Research and Quality resource center for the HSOPSC [49].
The HSOPSC, versions 1.0 [55,56] and 2.0 [30,57], exhibit moderate to strong reliability and validity. For scoring, the HSOPSC item responses can be totaled by dimension as a percentage of positive responses to assess a dimension or to determine the global measure of patient safety culture on a 100-point scale [58]. A dimension is a strength when the aggregate score is equal to or greater than 75% or a weakness when the score is less than 50% [59]. The range between these cut points is considered adequate but requires improvement. Spider diagrams can be used to compare dimensions and composite scores for the HSOPSC 1.0, where perception responses are classified by the percent of positive responses as “excellent” (>90), “good” (70–89), “adequate” (50–69), “fair” (26–49), or ”poor” (<26) [34]. Since the HSOPSC 2.0 scores were observed to be higher than the scores of the HSOPSC 1.0 during pilot studies [60], guidance was provided for version transition, including score interpretation and comparative analysis [61].
2.2. Latin America
Spanish language versions of the HSOPSC 1.0 [62] and 2.0 [63] were validated by Spanish-speaking healthcare workers in the United States [50,52]. Although lacking proper survey validation for cross-cultural research, the HSOPSC 1.0 has been also been has been translated, adapted, and validated in Portuguese [64] and Spanish [44] for use in Latin American countries and has been used in studies in Colombia [39], Mexico [65,66], and Peru [67]. These studies reported content validity and item equivalence, establishing language clarity (readability and understandability), and cultural relevance of the HSOPSC 1.0. However, no studies were identified from Latin America using a translated version of the HSOPSC 2.0. An item-level comparison of English and Spanish and versions of the HSOPSC 1.0 from the literature is provided in Supplementary File S1.
Since only one scoping review measured patient safety culture in Brazilian hospitals [68], a systematic review was necessary to produce the evidence for use of the HSOPSC in Latin America before the recommended migration to the HSOPSC 2.0 [49]. For this reason, the current review systematically searched and identified the available evidence for patient safety culture in Latin American hospitals through an analysis of studies that used the HSOPSC. The findings from this study will provide the status of patient safety culture in the region and may help hospitals identify common patient safety culture strengths and weaknesses, compare patient safety culture perceptions with other hospitals in the region, and guide applied research to implement strategies focused on improving patient safety culture. Finally, the findings may inform health policies focused on advancing patient safety culture and guide international accreditation organizations in patient safety culture assessments in Latin American hospitals.
3. Methods
This systematic review with meta-analysis was conducted according to the JBI guidelines for evidence synthesis [69]. The results of the study are reported according to the 2020 version of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [70]. Further, the study was designed as a living review [71,72] for periodic updates of patient safety culture in Latin America as measured with the HSOPSC.
3.1. Review Question
The SPICE (setting, perspective, intervention, comparison, and evaluation) strategy [73,74] was used to compose the review question that guided the search strategy. For the search strategy of the current review, the setting was Latin American hospitals, the perspective was the perception of health care professionals, the interventions were about patient safety culture, the comparison was patient safety culture in relation to organizational culture, and the evaluation was assessed by the HSOPSC measures. Although developing a research question can be complicated for some types of study designs [75,76], the SPICE strategy is flexible for searches that are likely to focus on observational and descriptive study designs [73,74,77]. The SPICE question results in search strategies that are thorough, comprehensive, transparent, and reproducible [78].
3.2. Databases
A search of studies was conducted in databases most prominent for research originating from Latin America. These databases included Biblioteca Virtual de Salud (BVS), PubMed, SciELO, and Scopus. In addition, manual searches were conducted from the bibliographic references of included studies, systematic reviews about patient safety, and searches in Google and Google Scholar in English, Portuguese, and Spanish.
3.3. Search Strategies
The search strategy included the following MeSH terms and keywords: “patient safety”, “safety culture”, “survey”, “questionnaire”, and “measurement” combined with the word “hospital” in English, Portuguese, and Spanish. These terms and keywords were linked with Boolean operators “and” and “or”. Each search strategy was adapted to the database and language requirements. Consultations were made with a reference librarian to review the search strategy and a linguistics expert for the search term translations. The search strategies were piloted in the databases using the three languages before the study search. The search was limited to Latin American countries, including Mexico. The example search strategies are provided in Supplementary File S2.
3.4. Eligibility Criteria
Observational and mixed-methods studies published between January 2011 and December 2021, where patient safety culture was measured with the HSOPSC 1.0 or 2.0 in hospitals located in Latin America, were included in the current review. Studies that did not report measurements for any of the dimensions and conference abstracts, theses, and dissertations were excluded. Narrative, scoping, and systematic reviews related to organization culture or patient safety were noted during the search for a reference list review to identify additional studies meeting the inclusion criteria.
3.5. Study Selection
The study selection process was completed sequentially from identification to inclusion according to the PRISMA 2020 flow diagram [79]. First, the documents for review were identified through the database and manual searches. Then, the documents were screened to eliminate duplicates in the reference manager. Next, the documents were added to an Excel spreadsheet for eligibility screening. Two researchers independently reviewed the document titles and abstracts against the inclusion criteria. Potentially relevant documents were retrieved in full-text format and reviewed for inclusion. The rationale for excluding studies was noted for additional review by another researcher. Discrepancies between the paired team of reviewers resulted in documents advancing to the next review round. At the final review round, discrepancies between paired reviewers were reviewed by a third reviewer. There were no unresolved discrepancies.
3.6. Data Extraction
Applying an extraction template, study data were independently extracted by two reviewers and organized in an Excel spreadsheet. The minimum information extracted from each study included the publication year, study location (city, country), sample size, sample distribution based on profession, and all data specific to any of the 12 dimensions evaluated by the HSOPSC 1.0 or the 10 dimensions of the HSOPSC 2.0. Reviewers were able to provide additional information during the data extraction by providing a notation about the inclusion rationale. This step provided an opportunity to collect unanticipated data from studies, note data sources requiring additional review, and record unusual or interesting information for later review.
3.7. Risk of Bias and Internal Validity
The included studies were assessed for risk of bias using the JBI critical appraisal checklist for analytical cross-sectional studies [80]. The internal validity of each study was assessed with the National Heart, Lung, and Blood Institute quality tool for observational cohorts and cross-sectional studies according to their guideline [81].
3.8. Data Synthesis
Data extracted from the studies were organized and analyzed in an Excel spreadsheet. Means and standard deviations were calculated by HSOPSC dimension across studies. The means for the dimensions reported by each study were analyzed, including standard error measurement, followed by a descriptive exploration to assess the sample heterogeneity. Although a random-effects meta-analysis was also completed [82,83], fixed and random-effect analyses were used to compare the results, opting for the most conservative measure [83,84]. Then, a subgroup analysis was performed to account for differences in the sample size and composition [85]. For this analysis, the studies were regrouped into the following three professional categories: nursing teams, physicians, and more than one profession. Finally, a meta-regression was conducted to corroborate the subgroup effects [86]. Inferential statistical analyses were performed with the STATA 16.0 software [87].
3.9. Ethical Considerations
Ethics committee approval was not required because the extracted data from the studies were available through searches of publicly accessible databases. However, ethics committee approvals were reported for each study included in this review.
4. Results
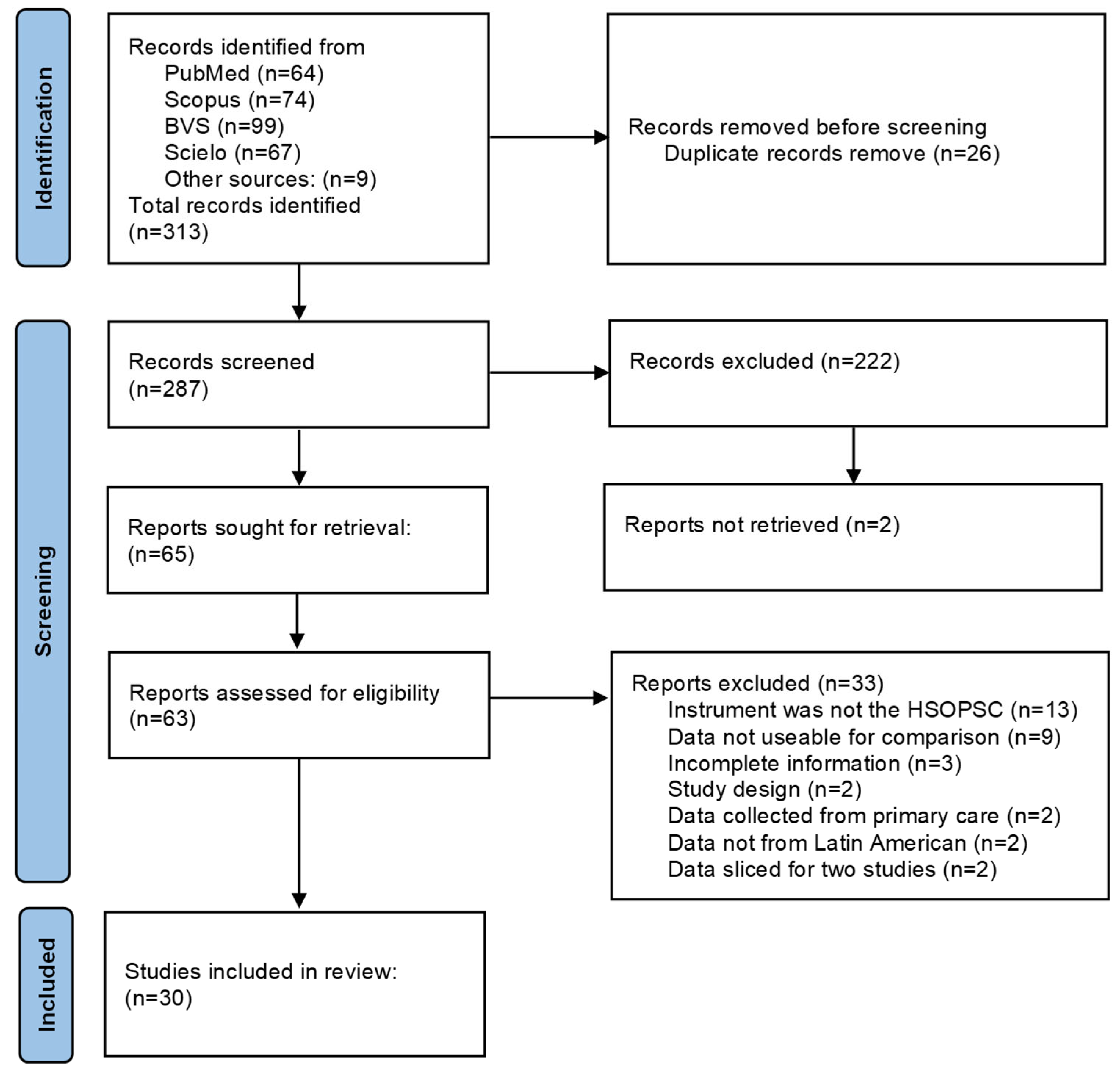
After removing duplicate documents, the searches resulted in 313 studies for screening and 63 studies for full-text review. The full screening process resulted in 30 studies included in the meta-analysis as detailed in the PRISMA flowchart in Figure 1.
Figure 1.
PRISMA 2020 flow diagram for systematic reviews.
During the quality assessment, two pairs of studies [88,89,90,91] were found to report analyzed data that were sliced from the same datasets (n = 158, n = 376). As such, the two studies with the more complete data were included for analysis [88,91], and the other two studies were excluded to limit bias [89,90]. Several studies reported small samples with a mixture of clinical and administrative professionals, but the average response rate reported across studies was nearly 80%. Therefore, all 30 studies were determined to be acceptable for meta-analysis.
4.1. Study Characteristics
The review included 30 studies from five Latin American countries: 22 studies in Brazil [88,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111], 3 studies in Mexico [112,113,114], 3 studies in Colombia [115,116,117], 1 study in Peru [67], and 1 study in Argentina [118]. All studies reported data from the HSOPSC 1.0; none reported data from the HSOPSC 2.0. The 30 studies totaled 10,915 participants with numbers ranging from 23 participants in a specialized service to 2500 participants in a national population of medical residents. In terms of types of professions, most studies included multiple professionals: 28 studies included nursing staff, 16 studies included physicians and residents, and 13 studies included other professionals and administrative staff. A small number of studies focused exclusively on nurses (7 studies) or physicians (2 studies). The information for studies by country and profession is provided in Table 1.

Table 1.
Characteristics of the reviewed studies (n = 30).
There were multiple hospitals included in some studies, ranging from one to six. Two studies from Mexico included data from a national [113] (n = 2500) and city [114] (n = 327) population of resident physicians working at different rather than specific hospitals. In general, the data collection process was completed in different venues. For example, most studies (n = 28) were conducted by researchers at hospitals, but one was conducted by a professional association [114] and another during an academic event [67]. In 25 studies, the surveys were delivered physically, but 5 were delivered online [67,95,113,114,117]. The majority of the studies (n = 17) included staff participation from more than one hospital service, including administrative staff and medical residents. In total, one study focused on a high complexity hospital [102], four studies focused on adult [93,99] and neonatal [92,100] intensive care units, five studies focused on perioperative and surgical services [88,101,109,115], and three studies focused on maternity services [103,104,105].
All studies were observational, and most reported cross-sectional designs (n = 29); a single longitudinal study reported three consecutive measurements with averaged results. None of the studies reported interventions as part of the study design. There were some studies (n = 3) with other instruments applied in addition to the HSOPSC 1.0. These instruments included the MISSCARE-Brasil to measure omitted nursing care [107], the Maslach Burnout Inventory to measure burnout, and the Safety Attitudes Questionnaire for construct comparison [93]. Finally, a single study compared the results of hospitals in Brazil and Portugal, but for the current review analysis, only the results from Brazil were extracted [96]. A summary of study characteristics is provided in Supplementary File S3.
4.2. HSOPSC 1.0 Dimensions
For measurement of the HSOPSC 1.0 dimensions across studies, the highest percentage of positive responses was observed for “organizational learning: continuous improvement” (68.34%) and “teamwork within units” (67.28%). The consolidated results by study and dimension are provided in Table 2.

Table 2.
The positive responses for patient safety culture dimensions by study (n = 30).
The least positive responses were observed for “nonpunitive response to error” (34.8%) and “staffing” (39.5%). By participant profession, the dimension “teamwork within units” was observed to have the most positive score (68.6%) for nurses. The dimensions observed with the least positive scores for nurses were “nonpunitive response to error” (36.5%) and “staffing” (37.1%). For physicians, the dimensions observed to have the least positive scores were “nonpunitive response to error” (27.9%) and “teamwork across hospital units” (37.0%). A detailed summary of the positive responses by dimension is presented for nurses, physicians, and other professionals in Supplementary File S4.
4.3. HSOPSC 1.0 Meta-Analysis
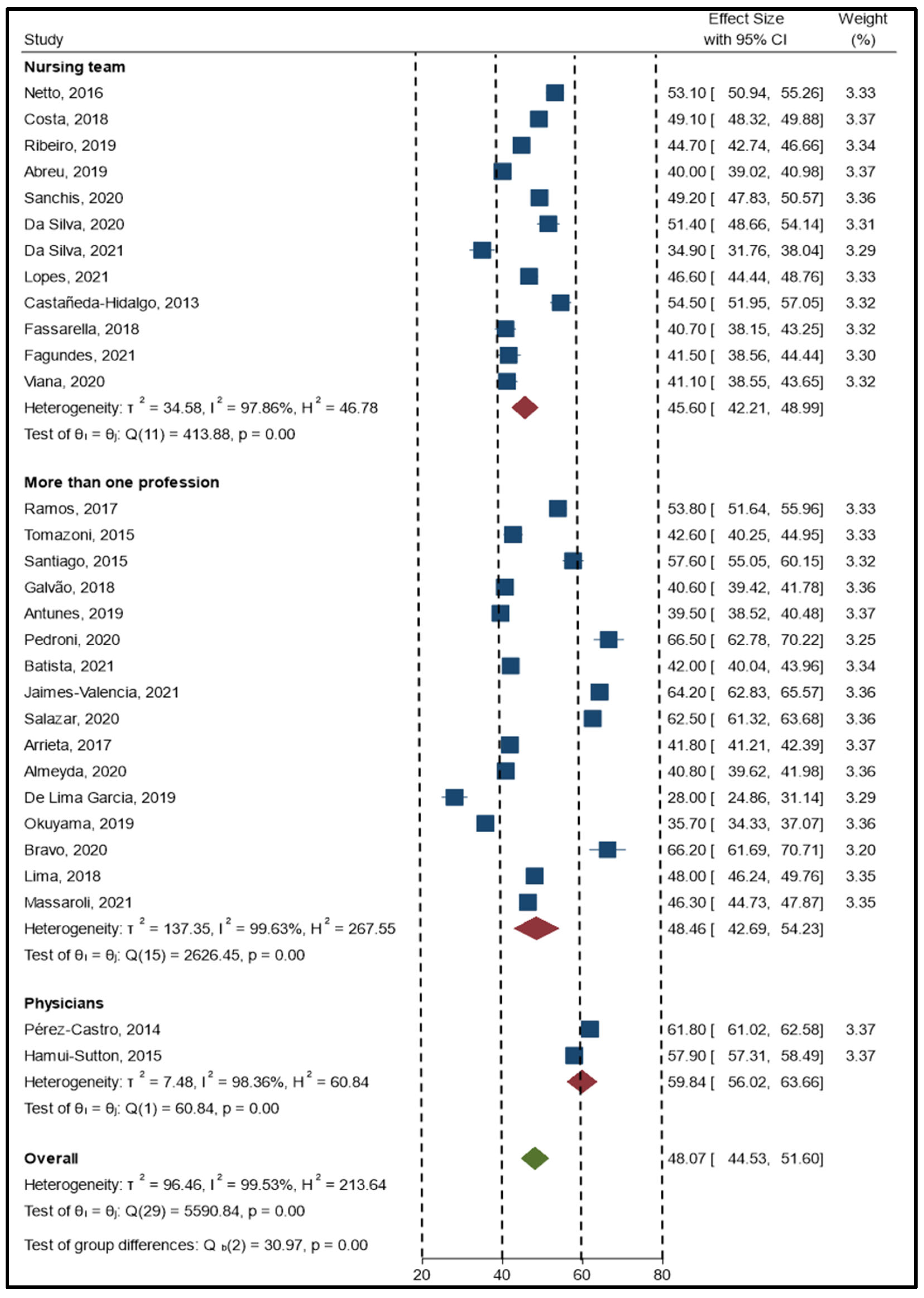
The meta-analysis resulted in an overall estimator of 48.07 (95% CI, 44.53–51.60), indicating a global perception of patient safety culture that requires improvement. A forest plot of studies with a positive percent response by professional category is provided in Figure 2. The estimator had high heterogeneity with an I2 of nearly 98%. For this reason, corroboration for statistically significant differences between groups was calculated.
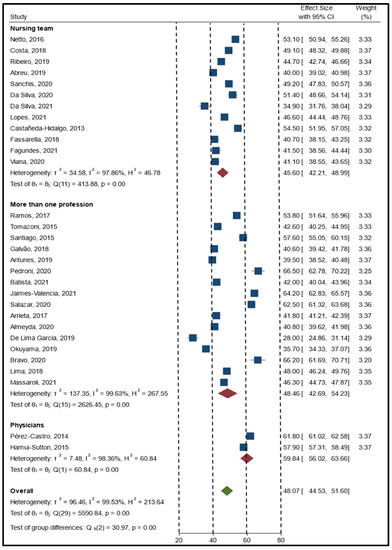
Figure 2.
Forest plot of the studies (n = 30) with a positive percent response by professional group.
Nurses were the group with the lowest score for patient safety culture perception with a mean score of 45.60 (95% CI, 42.21–48.99), followed by more than one profession with an average score of 48.46 (95% CI, 42.69–54.23) and physicians with an average score of 59.84 (95% CI, 56.02–63.66). The meta-regression analysis corroborated previous findings by highlighting a statistically significant difference (approximately 14.27 percentage points) between nurses and physicians.
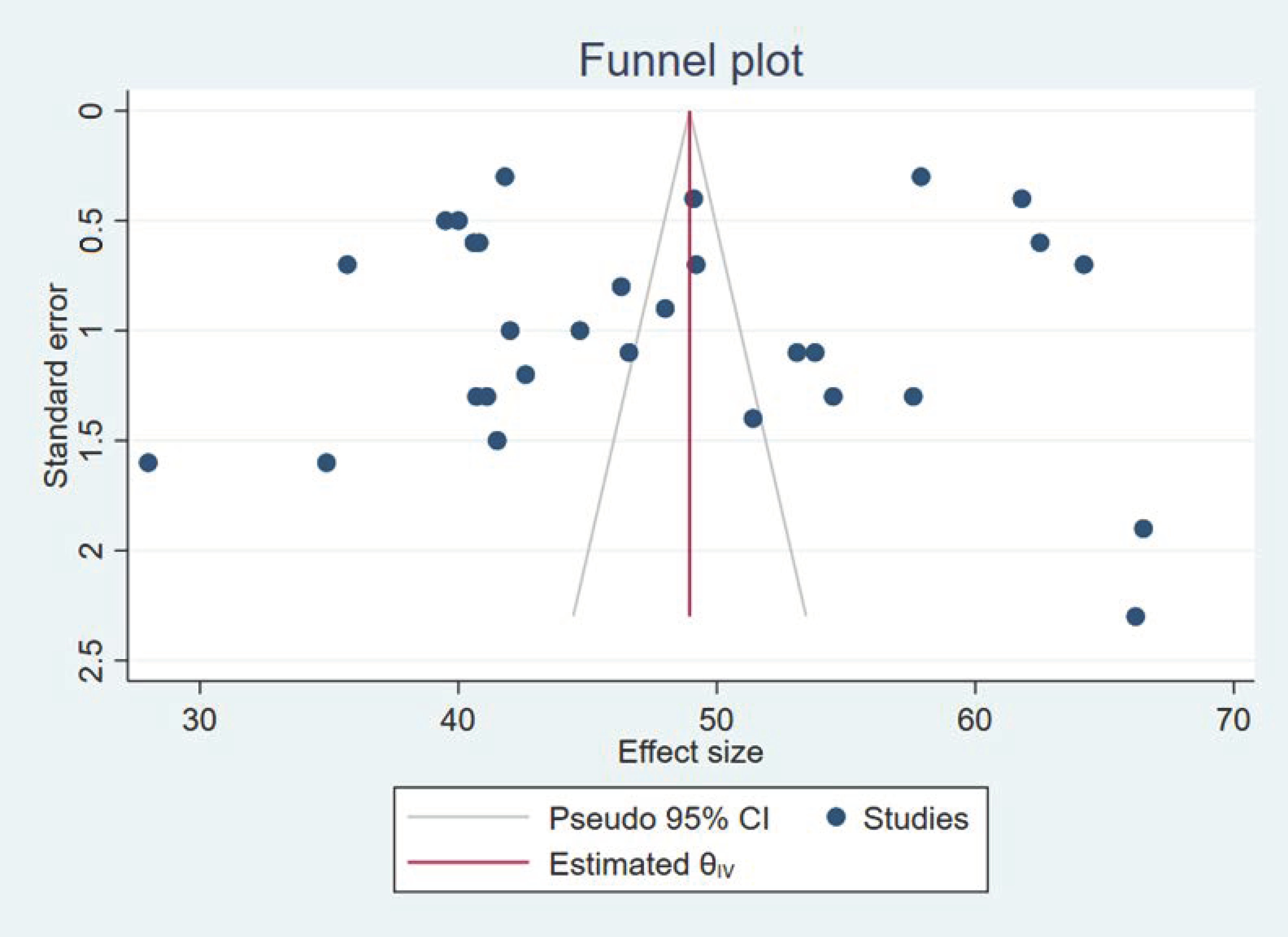
Finally, we performed a sensitivity analysis by eliminating studies that were outliers [103,116], but there was no significant change in the estimator. However, publication bias was likely observed because there were no studies with global patient safety culture perceptions of less than 50%. A funnel plot (Figure 3) of the studies confirms the resulting heterogeneity.
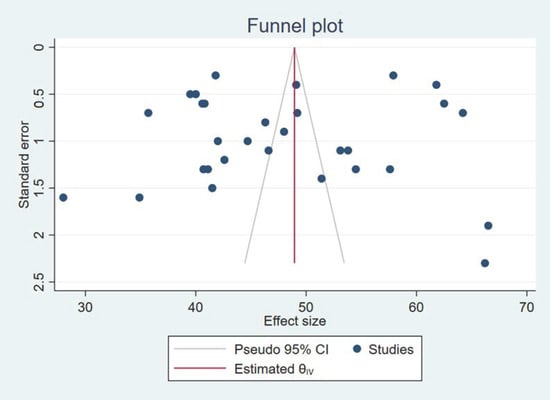
Figure 3.
Funnel plot of the studies (n = 30).
5. Discussion
The path to achieving patient safety, traveled by many developed countries [119], has not extended too far into Latin America. In the current review, only 30 studies from five countries reported evaluating patient safety culture with the HSOPSC 1.0; no studies used the HSOPSC 2.0. The studies included in this review were nearly all cross-sectional studies measuring the perception of patient safety culture; there were no interventions and few psychometric studies. Developed countries such as Norway, for example, have reported 20 studies using the HSOPSC 1.0, including 7 perception, 6 intervention, and 7 reliability and validity studies [120]. Although not the primary focus of the current review, the studies lacked reporting criteria for the reliability and validity of the translated version of the survey [121,122,123,124]. In the next sections of the discussion, the review findings are presented in terms of the perception of patient safety culture, clinical staffing, teamwork, punitive culture, other measures, and international accreditation. Finally, the limitations section presents several issues realized during this systematic review specific to conducting search strategies in three languages, namely checking citations for multiple analyses of the same dataset and assessing the impact of database selection for Latin American research literature.
5.1. Perception of Patient Safety Culture
The general perception of patient safety culture was 48.86% positive responses, which is an indicator that the quality of care should be a priority for the delivery of health services [125]. Spanish researchers reported patient safety culture to be a quality-of-care indicator that benefited the organization as leaders became more involved in the process to prevent risks from becoming repetitive problems [126]. Hospital leaders, managers, supervisors, and coordinators should report a more positive assessment of patient safety than clinicians because of their investment in the organization’s hierarchy and functions. With the advancement of quality improvement initiatives over time, everyone in the organization should report similar levels for the general perception of patient safety culture. If not, then more support and resources are necessary to implement strategies to strengthen patient safety, such as teamwork between units, notification of adverse events, and feedback on errors, to generate organizational learning and continuous improvement [127]. However, there is some contradictory research from intensive care units specific to general versus dimension-level perceptions. For example, intensive care nurses (n = 380) reported high positive perceptions about teamwork within units and organizational learning: continuous improvement, despite having an overall low perception of patient safety culture due to physical and mental demand and overall workload [128]. Importantly, general perceptions need to be carefully interpreted across time within the context, culture, and conditions of the health sector. Finally, general perceptions of patient safety culture may be important human resource indicators as suggested by the relationship between job satisfaction and safety culture reported in a study from Spain [129].
5.2. Clinical Staffing
In the current review, statistically significant differences were observed during the meta-analysis for the perception of patient safety culture across the different professional groups. Adequate clinical staffing in a hospital is essential for achieving improved clinical outcomes [130,131,132] and a more favorable patient safety culture [34,58]. The perception of patient safety has been related to the availability of adequate staffing [133]. For example, nurses from countries in different regions of the world, such as Ethiopia [41], Brazil [68], Hungary [134], Iran [135], Spain [136], and Norway [137], reported major concerns about inadequate staffing negatively impacting patient safety and clinical outcomes.
The current study findings about staffing across professions are relevant to the context and culture of the health sector in each country in Latin America. Similar to other studies [34,138,139,140], nurses were more concerned about staffing than physicians. This finding may be explained by most countries having as many or more physicians than nurses per 1000 people, despite nurses being responsible for staffing hospitals for 24 h each day of the year. When comparing similar groups of developed countries, such as members of the OECD, member countries outside Latin America often report having more nurses per capita than physicians. On average there are 8.8 nurses per 1000 population in OECD countries. The Latin American members have fewer nurses (2.6 per 1000 population) than the OECD. Further, the number of nurses per 1000 population in OECD countries ranges from 2.0 nurses in Turkey to 17.7 nurses in Norway. In contrast, there are 3.3 physicians per 1000 population, with a range of 0.5 physicians in Indonesia to 5.4 physicians in Austria. The number of nurses per 1000 population in Latin America varies, but there are more nurses in Costa Rica (3.4) and fewer in Mexico (2.9), Chile (2.7), and Colombia (1.3). When compared with physicians per 1000 population, Turkey (1.9) has an almost equal number of nurses and physicians, while Norway (5.1) has 70% fewer physicians than nurses. Observations from Turkey were similar to Latin American countries. These data are available from the World Bank [141,142,143] and the OECD [144,145,146].
The difference in findings between nurses and other participants in the current review may be related more to the quality of the work environment than the patient safety culture. In a large national hospital study in Chile, Aikens and colleagues [147] reported the nurse workload varied from 6 to 24 patients per nurse across 40 hospitals. Each patient added to the workload of an individual nurse increased mortality (odds ratio 1.04, 95% CI, 1.01–1.07, p < 0.01), readmissions (odds ratio 1.02, 95% CI, 1.01–1.03, p < 0.01), and length of stay (incident rate ratio 1.04, 95% CI, 1.01–1.06, p < 0.05). According to the authors, “Patients in hospitals with 18 patients per nurse, compared with those in hospitals with eight patients per nurse, had 41% higher risk of death, were 20% more likely to be readmitted within 30 days of discharge, had stays that were 41% longer, and were 68% less likely to rate the hospital highly and 55% less likely to recommend the hospital to family and friends” (p. e1151). These findings are consistent with similar large studies from other regions of the world [130,148,149].
The evidence from the current review coupled with the findings from Chile [147] suggests any agenda focused on strengthening patient safety culture requires a better understanding of the working conditions of healthcare professionals, especially nurses [150]. Improvements to the working conditions for nurses may require health policy interventions to establish a minimum staffing standard as an ethical obligation of governments to protect the human rights of patients and to support clinicians in providing safe and high-quality care [151]. Further, research should focus on understanding the relationship between hospital staffing in Latin American countries, such as work conditions and nursing-sensitive qualitative indicators, and patient safety culture.
5.3. Teamwork
Similar to studies conducted in other countries [38,120,152], the findings from the current review indicated nurses from Latin American countries perceived higher levels of quality improvement and teamwork contributed to patient safety culture despite poor staffing. The impact of teamwork on patient safety culture probably results from nurses being the core hospital staff with the most direct contact with patients since they are responsible for the continuity of care from diagnostic and therapeutic management to hospital discharge [153]. Nurses working together within units have the most direct impact on care quality and patient safety in hospitals through their continuous quality improvement activities [154] and education that focuses on working in multidisciplinary teams [129].
When performing the meta-analysis for the current review by the professional group, the highest scoring dimension for all groups was “teamwork within units”. Similarly, the teamwork dimension was also the highest scoring for studies conducted in Spain among physicians [155] and other health professions [156]. The quality of teamwork has long been reported to affect the performance of health professionals [157], resulting in organizational outcomes, such as adverse events. From an organizational perspective, the quality of teamwork is impacted by clinical competency, effective care coordination, reliable communication, and seamless collaboration across the organization that extends beyond disciplinary boundaries [158].
Effective teams are better prepared to protect patients from risks and to improve clinical outcomes [159]. In a systematic review investigating the most effective strategies for providing teamwork education programs in hospitals, Eddy et al. [160] recommended six strategies to facilitate programs aligned with cultivating a patient safety culture. The recommendations included suggestions for leaders, such as encouraging clinicians to participate in teamwork education programs, having organizers identify learning needs before implementing a program, providing learning strategies that foster collaboration through debriefing and reflection activities, and using high-fidelity simulation for more realistic opportunities that enhance the communication skills essential for better teamwork. In addition, managers were encouraged to provide opportunities for clinicians to apply their new skills in daily practice.
5.4. Punitive Culture
The most concerning perception of nurses in this study was the punitive culture in response to errors. This finding was similar to studies reported from other developing countries [161,162,163]. Since women working in developing countries often experience gender inequality and discrimination, the punitive culture perceived by nurses may result from hospitals being gendered organizations. In this regard, Latin American nurses historically experienced adverse working conditions related to misogynistic attributes, such as machismo culture, paternalistic leaders, and medicalized systems. However, the COVID-19 pandemic resulted in an emerging body of evidence about the widespread abuse, discrimination, harassment, and mistreatment of hospital nurses [164]. Even with greater visibility about the problems female nurses encounter at work, more research is needed to assess the work environment in internationally accredited and non-accredited hospitals in Latin America. However, internationally accredited hospitals should have less gendered cultures and better work environments, resulting in a less punitive culture.
Establishing a nonpunitive culture with open communication is essential to cultivate a robust incident reporting system and facilitating adverse event disclosure [165]. As such, the dimension with the lowest score for physicians was “communication openness”, which suggests a need to strengthen communication [89]. Although more research is necessary, this finding could be related to the punitive culture in some hospitals, where nurses may be less inclined to communicate with physicians or other professionals with positional authority at the hospital. The Healthcare Attribution Error Model [166] was proposed to explain how clinician cynicism, learned helplessness, and organizational inertia result from punitive cultures that silence clinician communication in the context of patient safety and speaking up in the context of error reporting. In a scoping review [167], attribution theory was linked to poor decision-making, errors in judgment, and engagement in two-way communication for speaking-up initiatives with parents of hospitalized children, but there has been no research investigating clinicians speaking up about patient safety concerns. Regardless of the etiology, a nonpunitive response to error reporting and adverse event disclosure is more than a management desire or a hospital policy; instead, a nonpunitive response is an essential tenant for a just culture to improve interpersonal, professional, and institutional capacities for achieving a level of patient safety [168,169] appropriate for the culture and context of Latin America [107].
5.5. HSOPSC Studies and Other Measures
There were two studies from Brazil that used another measure in addition to the Portuguese version of the HSOPSC 1.0 [64]. One of these studies [93] applied the HSOPSC 1.0 and the Safety Attitudes Questionnaire and reported a moderate correlation between them (r = 0.66). The other study [107], applied the MISSCARE-Brasil instrument, not the HSOPSC 1.0, to measure omitted nursing care. Although the authors found a more positive patient safety culture was associated with fewer omissions in nursing care, other studies [170] reported that the HSOPSC 1.0 dimensions explained up to 30% of the variance in missed nursing care, 26% of quality-of-care concerns, and 15% of vascular access device events. Further, missed care was significantly associated with falls. Missing nursing care is also proportional to the perceptive lack of patient safety [107] and staffing adequacy [171]. Finally, all lower-scoring dimensions of the HSOPSC 1.0 have correlated to some degree of burnout in other studies [98]. Lower scores for teamwork were most significantly associated with all three dimensions of burnout, including depersonalization, emotional exhaustion, and low professional achievement.
5.6. International Accreditation
International hospital accreditation penetration is a useful comparative measurement for health system maturity in developing countries. Specifically, hospital accreditation provides a robust framework for developing the systems, processes, and procedures essential for evidence-based practice, quality improvement, risk management, and patient safety [9,172,173]. However, a recent systematic review (n = 76) described the impact of hospital accreditation on care quality and patient safety as areas requiring more research [174]. Although the review included studies from 22 countries [174], the only country from Latin America was Brazil (n = 9), and few studies (n = 5) addressed organizational culture, including patient safety culture. Because the current literature is focused on understanding the impact of hospital accreditation on organizational culture, the environment of care, and clinical outcomes [175,176,177] (including patient safety culture [174]), we compared the international hospital accreditation penetration in each country of Latin America with the studies included in the current meta-analysis. Brazil reported nearly three-quarters of the hospital-based studies (n = 22) included in this meta-analysis and had nearly five times the total facility accreditations (n = 106) and seven times the hospital accreditations when compared with the next closest country, which was Peru. Despite 18 total accreditations with 12 specifics to hospitals in Peru, there was only one study reported in the literature with data collected at a patient safety conference. There were six other countries with hospital accreditations, but no studies were reported in the literature. The total accreditation activity in Latin America by Accreditation Canada International [178], Acreditas Global [179], Health Facility Accreditation Program [180], and The Joint Commission International [181] is summarized in Table 3.

Table 3.
International accreditation and HSOPSC 1.0 studies (N = 30) by country.
International hospital accreditation is strongly associated with patient safety culture in other regions of the world [174] and is likely the result of improved systems and more robust processes [182] associated with reporting medication errors [183], disclosing near misses [184], preventing adverse events [185], enhancing organizational learning, and improving teamwork [182]. In a pre- and post-accreditation evaluation of nurses (n = 605) in a Saudi Arabian hospital, a small but statistically significant improvement was observed across all HSOPSC 1.0 dimensions [186]. In a Danish hospital, hospital accreditation was reported to positively impact management priorities that strengthened patient safety culture during accreditation preparation [187]. In South Korea, medication error reporting significantly increased following hospital accreditation [188]. Finally, a recent observational study of nurses reported a weak but statistically significant association between patient safety culture and the hospital accreditation experience [189]. Since compliance with accreditation standards are relatively consistent across the accreditation cycle [190], patient safety culture in internationally accredited healthcare organizations results in sustainable organizational outcomes. For this reason, more research is necessary in Latin America to understand the impact of hospital accreditation on patient safety culture and on other clinical, organizational, and patient outcomes.
5.7. Limitations
There are strengths and limitations associated with all systematic reviews. The current review analyzes literature from a world region with multiple developing countries prone to publication bias. The limitations are areas for quality improvement in designing systematic reviews for Latin America. Although the most recognized databases in Latin America were included in the search strategy, national databases were not searched because of resource constraints. Many countries in Latin America maintain national databases for undergraduate and graduate research projects, theses, and dissertations. Some countries require the final research resulting from academic programs to be published in the public domain. Furthermore, professional organizations, scientific societies, and universities commonly publish scientific journals. In the context of Latin America, the research published in these journals is usually captured in the SciELO database. Although theses and dissertations were not included in this review, selection bias was minimized by including the SciELO [191] database in the search strategy. This database provides access to the scientific literature from Latin America published in local, national, and regional journals.
HSOPSC 1.0 studies originating from Latin America often report internal consistency and construct validity but lack power for factor analysis and methodological rigor. For example, a psychometric study reported from Colombia was likely underpowered [192,193] and did not include the expert evaluation of items and dimensions [194,195] or cognitive interviews with bilingual participants to establish content validity and survey equivalence [196,197] before data collection [198,199]. The 12-dimension HSOPSC 1.0 was reported as “not directly applicable to Colombian personnel in a surgical setting”, resulting in the authors recommending a 9-factor, 36-item version. The structural difference can be explained by weak factors consistent with inadequate item wording that caused a high measurement error and a small percentage of common variance [200]. Although the current review did not include a psychometric evaluation, we recognized the potential bias resulting from the HSOPSC 1.0 version selected to measure patient safety culture. For this reason, we recommend increased transparency in reporting the HSOPSC version used for data collection, including source citation and psychometric properties and whether the recommended guidelines for survey translation [201] were followed by the source.
Finally, in the current review, as in others [162,163], a high heterogeneity of studies was observed in the results. Because some studies involved one or several services of an institution, multiple institutions, or the participation of various groups of health professionals, the search strategy was limited to the hospital environment with discernable data related to the research question eligible for data extraction and analysis. All studies included in this review were also evaluated in the databases by the first, corresponding, and last authors and by funding and ethical approval numbers, if available, to identify multiple publications from single data sources. For systematic reviews that include meta-analysis [202], this kind of citation check strategy can minimize the potential for bias from multiple analyses of data from the same database [203] or overlapping portions of data due to salami slicing [203,204,205]. During the full-text assessment of reviewed studies, two sets of studies were found to originate from the same data source [88,89,90,91], which was not disclosed in the subsequent studies despite matching ethical approval numbers.
6. Conclusions
Patient safety culture measurement across hospitals in Latin America provides an opportunity to identify common areas for quality improvement to reduce the risk of adverse events and strengthen the overall quality of care. Surprisingly, the literature was limited to studies in only five countries, most of which were in South America and none in Central America. Because patient safety culture may be a relatively unknown or unmeasured concept in most Latin American countries, health professional programs should incorporate more patient safety content into curriculums, with an emphasis on communication, leadership, nonpunitive error reporting, quality improvement, and teamwork.
Despite some penetration of international hospital accreditation in Latin America, there were few studies from countries with accredited hospitals. For this reason, more research should evaluate the impact of accreditation on the patient safety culture in hospitals. Furthermore, quality improvement strategies aligned with advancing patient safety culture in hospitals should be included in the national health policies of Latin American countries. Finally, patient safety culture measurements should be required annually for hospitals and health systems to identify weak dimensions for quality improvement projects and to provide a longitudinal assessment of the organizational culture.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192114380/s1. Four Supplementary files are provided with the manuscript. Supplementary File S1: Item comparison across English and Spanish versions of the HSOPSC 1.0; Supplementary File S2: Search strategy examples; Supplementary File S3: Characteristics of reviewed studies; Supplementary File S4: Positive responses for safety culture by dimension.
Author Contributions
Conceptualization, D.E.C.-R., D.A.C.-B., K.A.D.-C. and P.A.P.; Methodology, D.E.C.-R., K.A.D.-C. and P.A.P.; Software, K.A.D.-C. and P.A.P.; Formal Analysis, D.E.C.-R., D.A.C.-B., K.A.D.-C. and P.A.P.; Resources, D.E.C.-R. and P.A.P.; Data Curation, D.E.C.-R., D.A.C.-B. and K.A.D.-C.; Writing—Original Draft Preparation, D.E.C.-R., D.A.C.-B. and K.A.D.-C.; Writing—Review and Editing, K.A.D.-C. and P.A.P.; Visualization, K.A.D.-C. and P.A.P.; Supervision, K.A.D.-C. and P.A.P.; Project Administration, D.E.C.-R.; Funding Acquisition, D.E.C.-R. and P.A.P. All authors have read and agreed to the published version of the manuscript.
Funding
This project was partially supported through a research dissemination grant (VRI-D-2022-05-001-RDG) received from the Dirección de Desarrollo de la Investigación, Universidad Norbert Wiener to promote the availability of scientific knowledge for low- and middle-income countries.
Institutional Review Board Statement
This systematic review was not required to have ethical approval as all the data for the research was available in the public domain of databases. Each study included in the review provided an ethics statement about conducting research in accordance with the Declaration of Helsinki and approval by an institutional review board or ethics committee.
Informed Consent Statement
The studies included in this review indicated an informed consent was provided by all participants.
Data Availability Statement
All the data for this study are provided in the figures, tables, and Supplementary Files.
Acknowledgments
We appreciate the participants from each study included in this review for providing their perspectives on patient safety culture. We also want to recognize the work of the research teams responsible for reporting the results of each study. Finally, we appreciate the excellent editorial review provided by Deborah Goggin, scientific writer and professional editor from the Department of Research Support at A.T. Still University.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Reason, J. Human Error; Cambridge University Press: New York, NY, USA, 1990. [Google Scholar]
- Perrow, C. Normal Accidents: Living with High-Risk Technologies; Basic Books: New York, NY, USA, 1984. [Google Scholar]
- Holden, R.J. People or systems? To blame is human. The fix is to engineer. Prof. Saf. 2009, 54, 34–41. [Google Scholar] [PubMed]
- Reason, J. Human error: Models and management. Br. Med. J. 2000, 320, 768–770. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine; Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System; Kohn, L.T., Corrigan, J.M., Donaldson, M.S., Eds.; National Academies Press: Washington, DC, USA, 2000. [Google Scholar]
- Lark, M.E.; Kirkpatrick, K.; Chung, K.C. Patient safety movement: History and future directions. J. Hand Surg. 2018, 43, 174–178. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences Engineering and Medicine. Crossing the Global Quality Chasm: Improving Health Care Worldwide; National Academies Press: Washington, DC, USA, 2018; p. 334. [Google Scholar]
- Auraaen, A.; Slawomirski, L.; Klazinga, N. The Economics of Patient Safety in Primary and Ambulatory Care; Organisation for Economic Cooperation and Development: Paris, France, 2018. [Google Scholar]
- Wilson, R.M.; Michel, P.; Olsen, S.; Gibberd, R.W.; Vincent, C.; El-Assady, R.; Rasslan, O.; Qsous, S.; Macharia, W.M.; Sahel, A.; et al. Patient safety in developing countries: Retrospective estimation of scale and nature of harm to patients in hospital. BMJ 2012, 344, e832. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Patient Safety Action Plan 2021–2030: Towards Eliminating Avoidable Harm in Health Care; WHO Press: Geneva, Switzerland, 2021. [Google Scholar]
- Sorra, J.S.; Dyer, N. Multilevel psychometric properties of the AHRQ hospital survey on patient safety culture. BMC Health Serv. Res. 2010, 10, 199. [Google Scholar] [CrossRef] [PubMed]
- Olds, D.M.; Aiken, L.H.; Cimiotti, J.P.; Lake, E.T. Association of nurse work environment and safety climate on patient mortality: A cross-sectional study. Int. J. Nurs. Stud. 2017, 74, 155–161. [Google Scholar] [CrossRef]
- Arfanis, K.; Fioratou, E.; Smith, A. Safety culture in anaesthesiology: Basic concepts and practical application. Best Pract. Res. Clin. Anaesthesiol. 2011, 25, 229–238. [Google Scholar] [CrossRef]
- Petschnig, W.; Haslinger-Baumann, E. Critical Incident Reporting System (CIRS): A fundamental component of risk management in health care systems to enhance patient safety. Saf. Health 2017, 3, 9. [Google Scholar] [CrossRef]
- Feeser, V.R.; Jackson, A.K.; Savage, N.M.; Layng, T.A.; Senn, R.K.; Dhindsa, H.S.; Santen, S.A.; Hemphill, R.R. When safety event reporting is seen as punitive: “I’ve Been PSN-ed!”. Ann. Emerg. Med. 2021, 77, 449–458. [Google Scholar] [CrossRef]
- Peerally, M.F.; Carr, S.; Waring, J.; Dixon-Woods, M. The problem with root cause analysis. BMJ Qual. Saf. 2017, 26, 417–422. [Google Scholar] [CrossRef]
- Wagner, C.; Kristensen, S.; Sousa, P.; Panteli, D. Patient safety culture as a quality strategy. In Improving Healthcare Quality in Europe: Characteristics, Effectiveness and Implementation of Different Strategies; Busse, R., Klazinga, N., Panteli, D., Quentin, W., Eds.; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2019; pp. 287–308. [Google Scholar]
- Etchegaray, J.M.; Thomas, E.J.; Profit, J. Preoccupation with failure and adherence to shared baselines: Measuring high-reliability organizational culture. J. Patient Saf. Risk Manag. 2019, 24, 147–152. [Google Scholar] [CrossRef]
- Boysen, P.G. Just culture: A foundation for balanced accountability and patient safety. Ochsner J. 2013, 13, 400–406. [Google Scholar]
- Manzanera, R.; Moya, D.; Guilabert, M.; Plana, M.; Gálvez, G.; Ortner, J.; Mira, J.J. Quality assurance and patient safety measures: A comparative longitudinal analysis. Int. J. Environ. Res. Public Health 2018, 15, 1568. [Google Scholar] [CrossRef]
- Brittain, A.C.; Carrington, J.M. Organizational health and patient safety: A systematic review. J. Hosp. Manag. Health Policy 2020, 5, 2. [Google Scholar] [CrossRef]
- Singer, S.J.; Vogus, T.J. Reducing hospital errors: Interventions that build safety culture. Annu. Rev. Public Health 2013, 34, 373–396. [Google Scholar] [CrossRef]
- Barnsteiner, J. Teaching the culture of safety. Online J. Issues Nurs. 2011, 16, 5. [Google Scholar] [CrossRef]
- Palmieri, P.A.; DeLucia, P.R.; Peterson, L.T.; Ott, T.E.; Green, A. The anatomy and physiology of error in adverse health care events. In Patient Safety and Health Care Management; Savage, G.T., Ford, E.W., Eds.; Emerald Group Publishing Limited: Bingley, UK, 2008; Volume 7, pp. 33–68. [Google Scholar]
- Lee, S.E.; Scott, L.D. Hospital nurses’ work environment characteristics and patient safety outcomes: A literature review. West. J. Nurs. Res. 2018, 40, 121–145. [Google Scholar] [CrossRef]
- Hughes, R.G. Quality methods, benchmarking, and measuring performance. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Hughes, R.G., Ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. [Google Scholar]
- Sexton, J.B.; Helmreich, R.L.; Neilands, T.B.; Rowan, K.; Vella, K.; Boyden, J.; Roberts, P.R.; Thomas, E.J. The Safety Attitudes Questionnaire: Psychometric properties, benchmarking data, and emerging research. BMC Health Serv. Res. 2006, 6, 44. [Google Scholar] [CrossRef]
- Vogus, T.J.; Sutcliffe, K.M. The safety organizing scale: Development and validation of a behavioral measure of safety culture in hospital nursing units. Med. Care 2007, 45, 46–54. [Google Scholar] [CrossRef]
- Nieva, V.F.; Sorra, J. Safety culture assessment: A tool for improving patient safety in healthcare organizations. Qual. Saf. Health Care 2003, 12 (Suppl. S2), ii17–ii23. [Google Scholar] [CrossRef] [PubMed]
- Sorra, J.; Zebrak, K.; Yount, N.; Famolaro, T.; Gray, L.; Franklin, M.; Smith, S.A.; Streagle, S. Development and pilot testing of survey items to assess the culture of value and efficiency in hospitals and medical offices. BMJ Qual. Saf. 2022, 31, 493–502. [Google Scholar] [CrossRef] [PubMed]
- Halligan, M.; Zecevic, A. Safety culture in healthcare: A review of concepts, dimensions, measures and progress. BMJ Qual. Saf. 2011, 20, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, P.A.; Peterson, L.T.; Pesta, B.J.; Flit, M.A.; Saettone, D.M. Safety culture as a contemporary healthcare construct: Theoretical review, research assessment, and translation to human resource management. In Strategic Human Resource Management in Health Care; Fottler, M.D., Khatri, N., Savage, G.T., Eds.; Advances in Health Care Management; Emerald Group Publishing Limited: Bingley, UK, 2010; Volume 9, pp. 97–133. [Google Scholar]
- Alsalem, G.; Bowie, P.; Morrison, J. Assessing safety climate in acute hospital settings: A systematic review of the adequacy of the psychometric properties of survey measurement tools. BMC Health Serv. Res. 2018, 18, 353. [Google Scholar] [CrossRef] [PubMed]
- Granel-Giménez, N.; Palmieri, P.A.; Watson-Badia, C.E.; Gómez-Ibáñez, R.; Leyva-Moral, J.M.; Bernabeu-Tamayo, M.D. Patient safety culture in European hospitals: A comparative mixed methods study. Int. J. Environ. Res. Public Health 2022, 19, 939. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. Surveys on Patient Safety Culture™ (SOPS®) Program. Available online: https://www.ahrq.gov/sops/about/index.html (accessed on 14 October 2022).
- Agency for Healthcare Research and Quality. International Use of SOPS. Available online: https://www.ahrq.gov/sops/international/index.html (accessed on 15 October 2022).
- Waterson, P.; Carman, E.M.; Manser, T.; Hammer, A. Hospital survey on patient safety culture (HSPSC): A systematic review of the psychometric properties of 62 international studies. BMJ Open 2019, 9, e026896. [Google Scholar] [CrossRef]
- Nie, Y.; Mao, X.; Cui, H.; He, S.; Li, J.; Zhang, M. Hospital survey on patient safety culture in China. BMC Health Serv. Res. 2013, 13, 228. [Google Scholar] [CrossRef]
- Ramírez, O.G.; Gutiérrez, W.A.; Vega, L.G.; Salamanca, J.G.; Galeano, E.M.; Gámez, A.S. Cultura de seguridad del paciente por personal de enfermeria en Bogota, Colombia. Cienc. Y Enfermería 2011, 17, 97–111. [Google Scholar] [CrossRef]
- Brborovic, H.; Sklebar, I.; Brborovic, O.; Brumen, V.; Mustajbegovic, J. Development of a Croatian version of the US Hospital Survey on Patient Safety Culture questionnaire: Dimensionality and psychometric properties. Postgrad. Med. J. 2014, 90, 125–132. [Google Scholar] [CrossRef]
- Wami, S.D.; Demssie, A.F.; Wassie, M.M.; Ahmed, A.N. Patient safety culture and associated factors: A quantitative and qualitative study of healthcare workers’ view in Jimma zone Hospitals, Southwest Ethiopia. BMC Health Serv. Res. 2016, 16, 495. [Google Scholar] [CrossRef]
- Fujita, S.; Seto, K.; Kitazawa, T.; Matsumoto, K.; Hasegawa, T. Characteristics of unit-level patient safety culture in hospitals in Japan: A cross-sectional study. BMC Health Serv. Res. 2014, 14, 508. [Google Scholar] [CrossRef]
- Sørskår, L.I.K.; Abrahamsen, E.B.; Olsen, E.; Sollid, S.J.M.; Abrahamsen, H.B. Psychometric properties of the Norwegian version of the hospital survey on patient safety culture in a prehospital environment. BMC Health Serv. Res. 2018, 18, 784. [Google Scholar] [CrossRef]
- Palmieri, P.A.; Leyva-Moral, J.M.; Camacho-Rodriguez, D.E.; Granel-Gimenez, N.; Ford, E.W.; Mathieson, K.M.; Leafman, J.S. Hospital survey on patient safety culture (HSOPSC): A multi-method approach for target-language instrument translation, adaptation, and validation to improve the equivalence of meaning for cross-cultural research. BMC Nurs. 2020, 19, 23. [Google Scholar] [CrossRef]
- Pinheiro, M.D.P.; Junior, O.C.D.S. Evaluación de la cultura de seguridad del paciente en una organización hospitalaria de un hospital universitario. Enfermería Glob. 2016, 16, 309–352. [Google Scholar] [CrossRef][Green Version]
- Flin, R.; Burns, C.; Mearns, K.; Yule, S.; Robertson, E.M. Measuring safety climate in health care. Qual. Saf. Health Care 2006, 15, 109–115. [Google Scholar] [CrossRef]
- Lee, S.E.; Dahinten, V.S. Adaptation and validation of a Korean-language version of the revised hospital survey on patient safety culture (K-HSOPSC 2.0). BMC Nurs. 2021, 20, 12. [Google Scholar] [CrossRef]
- Suryani, L.; Letchmi, S.; Said, F.B.M. Cross-culture adaptation and validation of the Indonesian version of the Hospital Survey on Patient Safety Culture (HSOPSC 2.0). Belitung Nurs. J. 2022, 8, 169–175. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. Hospital Survey on Patient Safety Culture. Available online: https://www.ahrq.gov/sops/surveys/hospital/index.html (accessed on 14 October 2022).
- Sorra, J.; Gray, L.; Streagle, S.; Famolaro, T.; Yount, N.; Behm, J. Hospital Survey on Patient Safety Culture: User’s Guide; 18-0036-EF; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2018. [Google Scholar]
- Famolaro, T.; Hare, R.; Yount, N.D.; Fan, L.; Liu, H.; Sorra, J. Surveys on Patient Safety Culture (SOPS) Hospital Survey 1.0: 2021 User Database Report 21-0016; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2021. [Google Scholar]
- Sorra, J.; Yount, N.; Famolaro, T.; Gray, L. Hospital Survey on Patient Safety Culture Version 2.0: User’s Guide, 19(21)-0076; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2021. [Google Scholar]
- Famolaro, T.; Hare, R.; Yount, N.D.; Fan, L.; Liu, H.; Sorra, J. Surveys on Patient Safety Culture (SOPS) Hospital Survey 2.0: 2021 User Database Report, 21-0017; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2021. [Google Scholar]
- Draganović, Š.; Offermanns, G.; Davis, R.E. Adaptation of the Agency for Healthcare Research and Quality’s ‘Hospital Survey on Patient Safety Culture’ to the Bosnia and Herzegovina context. BMJ Open 2021, 11, e045377. [Google Scholar] [CrossRef]
- Blegen, M.A.; Gearhart, S.; O’Brien, R.; Sehgal, N.L.; Alldredge, B.K. AHRQ’s hospital survey on patient safety culture: Psychometric analyses. J. Patient Saf. 2009, 5, 139–144. [Google Scholar] [CrossRef]
- Sorra, J.; Gray, L.; Streagle, S.; Famolaro, T.; Yount, N.; Behm, J. Pilot Study: Validity and Reliability of the Hospital Survey on Patient Safety; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2004. [Google Scholar]
- Sorra, J.; Famolaro, T.; Yount, N.D.; Caporaso, A.; Gray, L.; Zebrak, K.; Hare, R.; Thornto, S.; Fan, L.; Birch, R. Pilot Test Results from the 2019 AHRQ Surveys on Patient Safety Culture™ (SOPS™) Hospital Survey Version 2.0–Part I: Overall Results, 19-0068; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2019. [Google Scholar]
- Danielsson, M.; Nilsen, P.; Rutberg, H.; Årestedt, K. A national study of patient safety culture in hospitals in Sweden. J. Patient Saf. 2019, 15, 328–333. [Google Scholar] [CrossRef]
- El-Jardali, F.; Sheikh, F.; Garcia, N.A.; Jamal, D.; Abdo, A. Patient safety culture in a large teaching hospital in Riyadh: Baseline assessment, comparative analysis and opportunities for improvement. BMC Health Serv. Res. 2014, 14, 122. [Google Scholar] [CrossRef]
- Sorra, J.; Famolaro, T.; Yount, N.D. Transitioning to the SOPS™ Hospital Survey Version 2.0: What’s Different and What to Expect—Part II: Appendixes, 19-0076-1-EF; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2019. [Google Scholar]
- Sorra, J.; Famolaro, T.; Yount, N.D. Transitioning to the SOPS™ Hospital Survey Version 2.0: What’s Different and What to Expect, Part I: Main Report, 19-0076-1-EF; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2019. [Google Scholar]
- Agency for Healthcare Research and Quality. Cuestionario Sobre La De Seguridad De Los Pacientes En Los Hospitales (Version 1.0); Agency for Healthcare Research and Quality: Rockville, MD, USA, 2009. [Google Scholar]
- Agency for Healthcare Research and Quality. Cuestionario Sobre La De Seguridad De Los Pacientes En Los Hospitales (Version 2.0); Agency for Healthcare Research and Quality: Rockville, MD, USA, 2019. [Google Scholar]
- Fajardo-Dolci, G.; Rodriguez-Suarez, J.; Arboleya-Casanova, H.; Rojano-Fernandez, C.; Hernandez-Torres, F.; Santacruz-Varela, J. Cultura sobre seguridad del paciente en profesionales de la salud. Cirugía Y Cir. 2010, 78, 522–527. [Google Scholar]
- Ramirez-Martinez, M.E.; Gonzalez Pedraza-Aviles, A. Cultura de seguridad y eventos adversos en una clínica de primer nivel. Enfermería Univ. 2017, 14, 111–117. [Google Scholar] [CrossRef]
- Arrieta, A.; Suárez, G.; Hakim, G. Assessment of patient safety culture in private and public hospitals in Peru. Int. J. Qual. Health Care 2018, 30, 186–191. [Google Scholar] [CrossRef]
- Reis, C.T.; Laguardia, J.; Martins, M. Adaptação transcultural da versão brasileira do Hospital Survey on Patient Safety Culture: Etapa inicial. Cad. Saude Publica 2012, 28, 2199–2210. [Google Scholar] [CrossRef] [PubMed]
- Nascimento Prieto, M.M.; Pagotti da Fonseca, R.E.; Zem-Mascarenhas, S.H. Avaliação da cultura de segurança do paciente em hospitais brasileiros através do HSOPSC: Scoping review. Rev. Bras. Enferm. 2021, 74, e20201315. [Google Scholar] [CrossRef]
- Aromataris, E.; Munn, Z. JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2020. [Google Scholar]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. Br. Med. J. 2021, 372, 160. [Google Scholar] [CrossRef]
- Elliott, J.H.; Synnot, A.; Turner, T.; Simmonds, M.; Akl, E.A.; McDonald, S.; Salanti, G.; Meerpohl, J.; MacLehose, H.; Hilton, J.; et al. Living systematic review: 1. Introduction–the why, what, when, and how. J. Clin. Epidemiol. 2017, 91, 23–30. [Google Scholar] [CrossRef]
- Kelly, S.E.; Curran, J.A.; Tricco, A.C. Managing unmanageable loads of evidence: Are living reviews the answer? JBI Evid. Synth. 2022, 20, 1–2. [Google Scholar] [CrossRef]
- Booth, A. Clear and present questions: Formulating questions for evidence based practice. Libr. Hi Tech 2006, 24, 355–368. [Google Scholar] [CrossRef]
- Booth, A.; Noyes, J.; Flemming, K.; Moore, G.; Tunçalp, Ö.; Shakibazadeh, E. Formulating questions to explore complex interventions within qualitative evidence synthesis. BMJ Glob. Health 2019, 4, e001107. [Google Scholar] [CrossRef]
- Squires, J.E.; Valentine, J.C.; Grimshaw, J.M. Systematic reviews of complex interventions: Framing the review question. J. Clin. Epidemiol. 2013, 66, 1215–1222. [Google Scholar] [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef]
- Booth, A. Qualitative evidence synthesis. In Patient Involvement in Health Technology Assessment; Facey, K.M., Hansen, H.P., Single, A.N.V., Eds.; Springer: Singapore, 2017; pp. 187–199. [Google Scholar]
- Cooper, C.; Booth, A.; Varley-Campbell, J.; Britten, N.; Garside, R. Defining the process to literature searching in systematic reviews: A literature review of guidance and supporting studies. BMC Med. Res. Methodol. 2018, 18, 85. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; et al. Systematic reviews of etiology and risk. In JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2020. [Google Scholar]
- National Heart Lung and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 10 December 2021).
- Brockwell, S.E.; Gordon, I.R. A comparison of statistical methods for meta-analysis. Stat. Med. 2001, 20, 825–840. [Google Scholar] [CrossRef]
- Sheldon, T.A.; Sutton, A.J.; Song, F.; Jones, D.R.; Abrams, K.R. Methods for Meta-Analysis in Medical Research; John Wiley & Sons: New York, NY, USA, 2000. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- Barker, T.H.; Migliavaca, C.B.; Stein, C.; Colpani, V.; Falavigna, M.; Aromataris, E.; Munn, Z. Conducting proportional meta-analysis in different types of systematic reviews: A guide for synthesisers of evidence. BMC Med. Res. Methodol. 2021, 21, 189. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley and Sons: Hoboken, NJ, USA, 2019; pp. 241–284. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 16. Available online: https://www.stata.com/order/ (accessed on 10 October 2022).
- Batista, J.; de Almeida Cruz, E.D.; Alpendre, F.T.; da Silva, D.P.; Brandão, M.B.; Gabriel, C.S. Diferencias entre los profesionales de enfermería y medicina respecto a la cultura de la seguridad del paciente quirúrgico. Enfermería Glob. 2021, 20, 86–126. [Google Scholar] [CrossRef]
- Batista, J.; de Almeida Cruz, E.D.; Alpendre, F.T.; da Silva Stalisz da Paixão, D.P.; Gaspari, A.P.; Mauricio, A.B. Cultura de segurança e comunicação sobre erros cirúrgicos na perspectiva da equipe de saúde. Rev. Gauch. Enferm. 2019, 40, e20180192. [Google Scholar] [CrossRef]
- Viana, K.E.; Matsuda, L.M.; Ferreira, A.M.D.; dos Reis, G.A.X.; Souza, V.S.; Marcon, S.S. Cultura de segurança do paciente na ótica de profissionais de enfermagem. Texto Contexto—Enferm. 2021, 30, e20200219. [Google Scholar] [CrossRef]
- Viana, K.E.; Matsuda, L.M.; Pereira, A.C.S.; Oliveira, J.L.C.; Inoue, K.C.; Cruz, E.D.A. Cultura de segurança do paciente em hospitais públicos de ensino: Estudo comparativo. Rev. Enferm. UERJ 2020, 28, e51949. [Google Scholar] [CrossRef]
- Tomazoni, A.; Rocha, P.K.K.; de Souza, S.; Anders, J.C.; de Malfussi, H.C. Cultura de segurança do paciente em unidades de terapia intensiva neonatal: Perspectivas da equipe de enfermagem e médica. Rev. Lat. Am. Enferm. 2014, 22, 755–763. [Google Scholar] [CrossRef]
- Santiago, T.H.; Turrini, R.N. Cultura e clima organizacional para segurança do paciente em unidades de terapia intensiva. Rev. Esc. Enferm. USP 2015, 49, 123–127. [Google Scholar] [CrossRef]
- Costa, D.B.; Ramos, D.; Gabriel, C.S. Cultura de segurança do paciente sob a ótica da equipe de enfermagem em serviços hospitalares, apresentada ao programa de pós-graduação em enfermagem. Texto Contexto Enferm. 2018, 27, e2670016. [Google Scholar] [CrossRef]
- Galvão, T.F.; Lopes, M.C.C.; Oliva, C.C.C.; Araújo, M.E.A.; Silva, M.T. Cultura de segurança do paciente em um hospital universitário. Rev. Lat. Am. Enferm. 2018, 26, e3014. [Google Scholar] [CrossRef]
- Fassarella, C.S.; Camerini, F.G.; Henrique, D.M.; Almeida, L.F.; Figueiredo, M. Avaliação da cultura de segurança do paciente: Estudo comparativo em hospitais universitários. Rev. Esc. Enferm. USP 2018, 52, e03379. [Google Scholar] [CrossRef]
- Andrade, L.E.L.; Lopes, J.M.; Filho, M.C.M.S.; Júnior, R.F.V.; Farias, L.P.C.C.; dos Santos, C.C.M.; da Silva Gama, Z.A. Cultura de segurança do paciente em três hospitais brasileiros com diferentes tipos de gestão. Ciência Saúde Coletiva 2018, 23, 161–172. [Google Scholar] [CrossRef]
- De Lima Garcia, C.; Bezerra, I.M.P.; Ramos, J.L.S.; do Valle, J.E.T.M.R.; de Oliveira, M.L.B.; Abreu, L.C.d. Association between culture of patient safety and burnout in pediatric hospitals. PLoS ONE 2019, 14, e0218756. [Google Scholar] [CrossRef]
- Ribeiro, A.C.; Nogueira, P.C.; Tronchin, D.M.R.; Rossato, V.; Serpa, L.F. Cultura de segurança do paciente: Percepção dos enfermeiros em um centro de referência em cardiopneumologia. Texto E Contexto Enferm. 2019, 28, e20180118. [Google Scholar] [CrossRef]
- Notaro, K.A.M.; Corrêa, A.R.; Tomazoni, A.; Rocha, P.K.; Manzo, B.F. Cultura de segurança da equipe multiprofissional em unidades de terapia intensiva neonatal de hospitais públicos. Rev. Lat. Am. Enferm. 2019, 27, e3167. [Google Scholar] [CrossRef]
- Abreu, I.M.; Rocha, R.C.; Avelino, F.; Guimarães, D.B.O.; Nogueira, L.T.; Madeira, M.Z.A. Cultura de segurança do paciente em centro cirúrgico: Visão da enfermagem. Rev. Gauch. Enferm. 2019, 40, e20180198. [Google Scholar] [CrossRef]
- Sanchis, D.Z.; Haddad, M.C.F.L.; Girotto, E.; Silva, A.M.R. Cultura de segurança do paciente: Percepção de profissionais de enfermagem em instituições de alta complexidade. Rev. Bras. Enferm. 2020, 73, e20190174. [Google Scholar] [CrossRef]
- Pedroni, V.S.; Gouveia, H.G.; Vieira, L.B.; Wegner, W.; Oliveira, A.C.S.; Santos, M.C.D.; Carlotto, F.D. Cultura de segurança do paciente na área materno-infantil de hospital universitário. Rev. Gauch. Enferm. 2020, 41, e20190171. [Google Scholar] [CrossRef]
- Da Silva, P.L.; de Oliveira, G.M.T.; de Brito, M.R.L.; de Sousa, B.B.V.; Cardoso, R.R.; Melo, G.T.M. Cultura de seguridad del paciente en la perspectiva del equipo de enfermería en una maternidad pública. Enfermería Glob. 2020, 19, 427–462. [Google Scholar] [CrossRef]
- Do Carmo, J.M.A.; Mendoza, I.Y.Q.; Goveia, V.R.; de Souza, K.V.; Manzo, B.F.; de Lima Guimarães, G. Cultura de segurança do paciente em unidades hospitalares de ginecologia e obstetrícia: Estudo transversal. Rev. Bras. Enferm. 2020, 73, e20190576. [Google Scholar] [CrossRef]
- Netto, F.C.D.B.; Severino, F.G. Resultados da avaliação da cultura de segurança em um hospital público de ensino do Ceará. Rev. Bras. Promoção Da Saúde 2016, 29, 334–341. [Google Scholar] [CrossRef][Green Version]
- Da Silva, S.C.; Morais, B.X.; Munhoz, O.L.; Dal Ongaro, J.; de Souza Urbanetto, J.; de Souza Magnago, T.S.B. Cultura de segurança do paciente, cuidados de enfermagem omitidos e suas razões na obstetrícia. Rev. Lat. Am. Enferm. 2021, 29, e3461. [Google Scholar] [CrossRef]
- Campelo, C.L.; Nunes, F.D.O.; Silva, L.D.C.; Guimarães, L.F.; Sousa, S.M.A.; de Souza Paiva, S. Cultura de segurança do paciente entre profissionais de enfermagem no ambiente da terapia intensiva. Rev. Esc. Enferm. USP 2021, 55, 1–8. [Google Scholar] [CrossRef]
- Fagundes, T.E.; Acosta, A.S.; Gouvea, P.B.; Massaroli, R.; Rangel, R.C.T.; Andrade, P.D. Cultura de segurança do paciente em centro cirúrgico na perspectiva da equipe de enfermagem. J. Nurs. Health 2021, 11, e2111219510. [Google Scholar]
- Massaroli, A.; De Carli Rodrigues, M.E.; Kooke, K.; De Brito Pitilin, É.; Haag, F.B.; Araújo, J.S. Avaliação da cultura de segurança do paciente em um hospital do sul do brasil. Cienc. Y Enfermería 2021, 27, 1–12. [Google Scholar] [CrossRef]
- Okuyama, J.H.H.; Galvão, T.F.; Crozatti, M.T.L.; Silva, M.T. Health professionals’ perception of patient safety culture in a university hospital in São Paulo: A cross-sectional study applying the hospital survey on patient safety culture. Sao Paulo Med. J. 2019, 137, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Castañeda-Hidalgo, H.; Hernández, R.G.; Salinas, J.F.G.; Zúñiga, M.P.; Porras, G.A.; Pérez, A.A. Percepción de la cultura de la seguridad de los pacientes por personal de enfermería. Cienc. Y Enfermería 2013, 19, 77–88. [Google Scholar] [CrossRef]
- Hamui-Sutton, A.; Pérez-Castro, V.J.A.; Durán-Pérez, V.D.; García-Téllez, S.E.; Fernández-Cantón, S.B.; Lezana-Fernández, M.Á.; Carrasco-Rojas, J.A. Percepción de los médicos residentes sobre la cultura de seguridad del paciente en México. Rev. CONAMED 2015, 20, 54–63. [Google Scholar]
- Perez-Castro, J.A.; Esparza, C.M.J.; Martinez, L.D.O.; Martine, L.A.B.; Gomez, A.A.P.; Olvera, A.I.G.; Bernal, M.D.; Villarreal, H.G.M.; Tovar, F.R. Percepción de la cultura de seguridad del paciente en médicos pasantes del servicio social. Rev. CONAMED 2014, 19, 52–58. [Google Scholar]
- Maya, S.; Maria, A.; Marín, R.; Marcela, D. Cultura de la seguridad del paciente en seis centros quirúrgicos de Antioquia. Rev. Cuid. 2020, 11, e1040. [Google Scholar] [CrossRef]
- Bravo Gómez, M.; de Pérez, L.B.A.; Arguello, D.K.; Moreno, X.B.; Vega, M.P.; Naranjo, D.J.O.; Carvajal, R.R. Cultura de seguridad en profesionales del quirófano en una institución de atención materno infantil. Rev. Cuba. Enfermería 2020, 36, e3155. [Google Scholar]
- Jaimes-Valencia, M.L.; Alvarado-Alvarado, A.L.; Mejía-Arciniegas, C.N.; López-Galán, A.V.; Mancilla-Jiménez, V.A.; Padilla-García, C.I. Correlación del grado de percepción y cultura de seguridad del paciente en una Institución de tercer nivel 2015–2019. Rev. Cuid. 2021, 12, e1092. [Google Scholar] [CrossRef]
- Ramos, F.; Coca, S.M.; Abeldaño, R.A. Percepción de la cultura de seguridad de pacientes en profesionales de una institución argentina. Enfermería Univ. 2017, 14, 47–53. [Google Scholar] [CrossRef]
- Longo, D.R.; Hewett, J.E.; Ge, B.; Schubert, S. The long road to patient safety: A status report on patient safety systems. JAMA 2005, 294, 2858–2865. [Google Scholar] [CrossRef]
- Olsen, E.; Leonardsen, A.-C.L. Use of the Hospital Survey of Patient Safety Culture in Norwegian hospitals: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 6518. [Google Scholar] [CrossRef]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: Report of the ISPOR task force for translation and cultural adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef]
- Eremenco, S.; Pease, S.; Mann, S.; Berry, P. Patient-reported outcome (PRO) consortium translation process: Consensus development of updated best practices. J. Patient-Rep. Outcomes 2018, 2, 12. [Google Scholar] [CrossRef]
- Acquadro, C.; Conway, K.; Hareendran, A.; Aaronson, N. Literature review of methods to translate health-related quality of life questionnaires for use in multinational clinical trials. Value Health 2008, 11, 509–521. [Google Scholar] [CrossRef]
- Sousa, V.D.; Rojjanasrirat, W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J. Eval. Clin. Pract. 2011, 17, 268–274. [Google Scholar] [CrossRef]
- Zwijnenberg, N.C.; Hendriks, M.; Hoogervorst-Schilp, J.; Wagner, C. Healthcare professionals’ views on feedback of a patient safety culture assessment. BMC Health Serv. Res. 2016, 16, 199. [Google Scholar] [CrossRef]
- Giménez-Júlvez, T.; Hernández-García, I.; Aibar-Remón, C.; Gutiérrez-Cía, I.; Febrel-Bordejé, M. Cultura de la seguridad del paciente en directivos y gestores de un servicio de salud. Gac. Sanit. 2017, 31, 423–426. [Google Scholar] [CrossRef]
- Lee, S.E.; Dahinten, V.S. The enabling, enacting, and elaborating factors of safety culture associated with patient safety: A multilevel analysis. J. Nurs. Scholarsh. 2020, 52, 544–552. [Google Scholar] [CrossRef]
- Alrabae, Y.M.A.; Aboshaiqah, A.E.; Tumala, R.B. The association between self-reported workload and perceptions of patient safety culture: A study of intensive care unit nurses. J. Clin. Nurs. 2021, 30, 1003–1017. [Google Scholar] [CrossRef]
- Merino-Plaza, M.J.; Carrera-Hueso, F.J.; Roca-Castello, M.R.; Morro-Martin, M.D.; Martinez-Asensi, A.; Fikri-Benbrahim, N. Relacion entre la satisfaccion laboral y la cultura de seguridad del paciente. Gac. Sanit. 2018, 32, 352–361. [Google Scholar] [CrossRef]
- Aiken, L.H.; Cerón, C.; Simonetti, M.; Lake, E.T.; Galiano, A.; Garbarini, A.; Soto, P.; Bravo, D.; Smith, H.L. Hospital nurse staffing and patient outcomes. Rev. Médica Clínica Las Condes 2018, 29, 322–327. [Google Scholar] [CrossRef]
- Bruyneel, L.; Li, B.; Ausserhofer, D.; Lesaffre, E.; Dumitrescu, I.; Smith, H.L.; Sloane, D.M.; Aiken, L.H.; Sermeus, W. Organization of hospital nursing, provision of nursing care, and patient experiences with care in Europe. Med. Care Res. Rev. 2015, 72, 643–664. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, P.; Ball, J.; Drennan, J.; Dall’Ora, C.; Jones, J.; Maruotti, A.; Pope, C.; Saucedo, A.R.; Simon, M. Nurse staffing and patient outcomes: Strengths and limitations of the evidence to inform policy and practice. Int. J. Nurs. Stud. 2016, 63, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Azyabi, A.; Karwowski, W.; Davahli, M.R. Assessing patient safety culture in hospital settings. Int. J. Environ. Res. Public Health 2021, 18, 2466. [Google Scholar] [CrossRef] [PubMed]
- Granel, N.; Manresa-Domínguez, J.M.; Barth, A.; Papp, K.; Bernabeu-Tamayo, M.D. Patient safety culture in Hungarian hospitals. Int. J. Health Care Qual. Assur. 2019, 32, 412–424. [Google Scholar] [CrossRef] [PubMed]
- Kakemam, E.; Albelbeisi, A.H.; Davoodabadi, S.; Ghafari, M.; Dehghandar, Z.; Raeissi, P. Patient safety culture in Iranian teaching hospitals: Baseline assessment, opportunities for improvement and benchmarking. BMC Health Serv. Res. 2022, 22, 403. [Google Scholar] [CrossRef]
- Granel, N.; Manresa-Domínguez, J.M.; Watson, C.E.; Gómez-Ibáñez, R.; Bernabeu-Tamayo, M.D. Nurses’ perceptions of patient safety culture: A mixed-methods study. BMC Health Serv. Res. 2020, 20, 584. [Google Scholar] [CrossRef]
- Jabarkhil, A.Q.; Tabatabaee, S.S.; Jamali, J.; Moghri, J. Assessment of patient safety culture among doctors, nurses, and midwives in a public hospital in Afghanistan. Risk Manag. Healthc. Policy 2021, 14, 1211–1217. [Google Scholar] [CrossRef]
- Alzahrani, N.; Jones, R.; Rizwan, A.; Abdel-Latif, M.E. Safety attitudes in hospital emergency departments: A systematic review. Int. J. Health Care Qual. Assur. 2019, 32, 1042–1054. [Google Scholar] [CrossRef]
- Verbeek-Van Noord, I.; Wagner, C.; Van Dyck, C.; Twisk, J.W.R.; De Bruijne, M.C. Is culture associated with patient safety in the emergency department? A study of staff perspectives. Int. J. Qual. Health Care 2013, 26, 64–70. [Google Scholar] [CrossRef]
- Shaw, K.N.; Ruddy, R.M.; Olsen, C.S.; Lillis, K.A.; Mahajan, P.V.; Dean, J.M.; Chamberlain, J.M. Pediatric patient safety in emergency departments: Unit characteristics and staff perceptions. Pediatrics 2009, 124, 485–493. [Google Scholar] [CrossRef]
- The World Bank. Physicians (per 1000 People). Available online: https://data.worldbank.org/indicator/SH.MED.PHYS.ZS (accessed on 30 May 2022).
- The World Bank. Number of Surgical Procedures (per 100,000 Population). Available online: https://data.worldbank.org/indicator/SH.SGR.PROC.P5 (accessed on 30 May 2022).
- The World Bank. Hospital Beds (per 1000 People). Available online: https://data.worldbank.org/indicator/SH.MED.BEDS.ZS (accessed on 30 May 2022).
- Organisation for Economic Co-Operation and Development. Doctors (Indicator). Available online: https://data.oecd.org/healthres/doctors.htm (accessed on 30 May 2022).
- Organisation for Economic Co-Operation and Development. Nurses (Indicator). Available online: https://data.oecd.org/healthres/nurses.htm (accessed on 30 May 2022).
- Organisation for Economic Co-Operation and Development. Health Spending (Indicator). Available online: https://data.oecd.org/healthres/health-spending.htm (accessed on 30 May 2022).
- Aiken, L.H.; Simonetti, M.; Sloane, D.M.; Cerón, C.; Soto, P.; Bravo, D.; Galiano, A.; Behrman, J.R.; Smith, H.L.; McHugh, M.D.; et al. Hospital nurse staffing and patient outcomes in Chile: A multilevel cross-sectional study. Lancet Glob. Health 2021, 9, e1145–e1153. [Google Scholar] [CrossRef]
- You, L.-M.; Aiken, L.H.; Sloane, D.M.; Liu, K.; He, G.-P.; Hu, Y.; Jiang, X.-L.; Li, X.-H.; Li, X.-M.; Liu, H.-P.; et al. Hospital nursing, care quality, and patient satisfaction: Cross-sectional surveys of nurses and patients in hospitals in China and Europe. Int. J. Nurs. Stud. 2013, 50, 154–161. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.M.; Bruyneel, L.; Van den Heede, K.; Griffiths, P.; Busse, R.; Diomidous, M.; Kinnunen, J.; Kózka, M.; Lesaffre, E.; et al. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 2014, 383, 1824–1830. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.M.; Clarke, S.; Poghosyan, L.; Cho, E.; You, L.; Finlayson, M.; Kanai-Pak, M.; Aungsuroch, Y. Importance of work environments on hospital outcomes in nine countries. Int. J. Qual. Health Care 2011, 23, 357–364. [Google Scholar] [CrossRef]
- Tønnessen, S.; Scott, A.; Nortvedt, P. Safe and competent nursing care: An argument for a minimum standard? Nurs. Ethics 2020, 27, 1396–1407. [Google Scholar] [CrossRef]
- Skoogh, A.; Baath, C.; Hall-Lord, M.L. Healthcare professionals’ perceptions of patient safety culture and teamwork in intrapartum care: A cross-sectional study. BMC Health Serv. Res. 2022, 22, 820. [Google Scholar] [CrossRef]
- Hernández-Cruz, R.; Moreno-Monsiváis, M.G.; Cheverría-Rivera, S.; Díaz-Oviedo, A. Fatores que influenciam o cuidado de enfermagem omitido em pacientes de um hospital particular. Rev. Lat. Am. Enferm. 2017, 25, e2877. [Google Scholar] [CrossRef]
- Vaismoradi, M.; Tella, S.; Logan, P.; Khakurel, J.; Vizcaya-Moreno, F. Nurses’ adherence to patient safety principles: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 2028. [Google Scholar] [CrossRef]
- Romero, M.P.; González, R.B.; Calvo, M.S.R. La cultura de seguridad del paciente en los médicos internos residentes de medicina familiar y comunitaria de Galicia. Atención Primaria 2017, 49, 343–350. [Google Scholar] [CrossRef]
- Laborde, M.M.; Velázquez, M.T.G.; Andrés, J.M.A.; Forner, G.R.; Rosique, A.F.C. Análisis de la cultura de seguridad del paciente en un hospital universitario. Gac. Sanit. 2020, 34, 500–513. [Google Scholar] [CrossRef]
- Firth-Cozens, J. Cultures for improving patient safety through learning: The role of teamwork. Qual. Health Care 2001, 10 (Suppl. S2), ii26–ii31. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.A.; DiazGranados, D.; Dietz, A.S.; Benishek, L.E.; Thompson, D.; Pronovost, P.J.; Weaver, S.J. Teamwork in healthcare: Key discoveries enabling safer, high-quality care. Am. Psychol. 2018, 73, 433–450. [Google Scholar] [CrossRef] [PubMed]
- Lyubovnikova, J.; West, M.A.; Dawson, J.F.; Carter, M.R. 24-Karat or fool’s gold? Consequences of real team and co-acting group membership in healthcare organizations. Eur. J. Work. Organ. Psychol. 2015, 24, 929–950. [Google Scholar] [CrossRef]
- Eddy, K.; Jordan, Z.; Stephenson, M. Health professionals’ experience of teamwork education in acute hospital settings: A systematic review of qualitative literature. JBI Evid. Synth. 2016, 14, 96–137. [Google Scholar] [CrossRef] [PubMed]
- Elmontsri, M.; Almashrafi, A.; Banarsee, R.; Majeed, A. Status of patient safety culture in Arab countries: A systematic review. BMJ Open 2017, 7, e013487. [Google Scholar] [CrossRef]
- Azami-Aghdash, S.; Azar, F.E.; Rezapour, A.; Azami, A.; Rasi, V.; Klvany, K. Patient safety culture in hospitals of Iran: A systematic review and meta-analysis. Med. J. Islam. Repub. Iran 2015, 29, 251. [Google Scholar]
- Okuyama, J.H.H.; Galvao, T.F.; Silva, M.T. Healthcare professional’s perception of patient safety measured by the Hospital Survey on Patient Safety Culture: A systematic review and meta-analysis. Sci. World J. 2018, 2018, 9156301. [Google Scholar] [CrossRef]
- Labrague, L.J.; De los Santos, J.A.A.; Fronda, D.C. Perceived COVID-19-associated discrimination, mental health and professional-turnover intention among frontline clinical nurses: The mediating role of resilience. Int. J. Ment. Health Nurs. 2021, 30, 1674–1683. [Google Scholar] [CrossRef]
- Wu, A.W.; Boyle, D.J.; Wallace, G.; Mazor, K.M. Disclosure of adverse events in the United States and Canada: An update, and a proposed framework for improvement. J. Public Health Res. 2013, 2, e2032. [Google Scholar] [CrossRef]
- Palmieri, P.A.; Peterson, L.T. Attribution theory and healthcare culture: Translational management science contributes a framework to identify the etiology of punitive clinical environments. In Biennial Review of Health Care Management: Meso Perspective; Advances in Health Care Management; Savage, G.T., Fottler, M.D., Eds.; Emerald Group Publishing Limited: Bingley, UK, 2009; Volume 8, pp. 81–111. [Google Scholar]
- Thirsk, L.M.; Panchuk, J.T.; Stahlke, S.; Hagtvedt, R. Cognitive and implicit biases in nurses’ judgment and decision-making: A scoping review. Int. J. Nurs. Stud. 2022, 133, 104284. [Google Scholar] [CrossRef]
- Sameera, V.; Bindra, A.; Rath, G.P. Human errors and their prevention in healthcare. J. Anaesthesiol. Clin. Pharmacol. 2021, 37, 328–335. [Google Scholar] [CrossRef]
- The Joint Commission. Developing a reporting culture: Learning from close calls and hazardous conditions. Sentin. Event 2018, 60, 1–8. [Google Scholar]
- Hessels, A.J.; Paliwal, M.; Weaver, S.H.; Siddiqui, D.; Wurmser, T.A. Impact of patient safety culture on missed nursing care and adverse patient events. J. Nurs. Care Qual. 2019, 34, 287–294. [Google Scholar] [CrossRef]
- Labrague, L.J. Linking nurse practice environment, safety climate and job dimensions to missed nursing care. Int. Nurs. Rev. 2022, 69, 350–358. [Google Scholar] [CrossRef]
- Jha, A.K. Accreditation, quality, and making hospital care better. JAMA 2018, 320, 2410–2411. [Google Scholar] [CrossRef]
- Mansour, W.; Boyd, A.; Walshe, K. The development of hospital accreditation in low- and middle-income countries: A literature review. Health Policy Plan. 2020, 35, 684–700. [Google Scholar] [CrossRef]
- Hussein, M.; Pavlova, M.; Ghalwash, M.; Groot, W. The impact of hospital accreditation on the quality of healthcare: A systematic literature review. BMC Health Serv. Res. 2021, 21, 1057. [Google Scholar] [CrossRef]
- Lam, M.B.; Figueroa, J.F.; Feyman, Y.; Reimold, K.E.; Orav, E.J.; Jha, A.K. Association between patient outcomes and accreditation in US hospitals: Observational study. BMJ 2018, 363, k4011. [Google Scholar] [CrossRef]
- Desveaux, L.; Mitchell, J.I.; Shaw, J.; Ivers, N.M. Understanding the impact of accreditation on quality in healthcare: A grounded theory approach. Int. J. Qual. Health Care 2017, 29, 941–947. [Google Scholar] [CrossRef]
- Avia, I.; Hariyati, R.T.S. Impact of hospital accreditation on quality of care: A literature review. Enfermería Clínica 2019, 29, 315–320. [Google Scholar] [CrossRef]
- Accreditation Canada International. Internationally Accredited Organizations. Available online: https://accreditation.ca/find-intl-accredited-service-provider/ (accessed on 1 April 2022).
- Acreditas Global. Accreditation for international HCPs. Available online: https://www.aaahc.org/accreditation/international/ (accessed on 1 April 2022).
- Health Facility Accreditation Program. Search Facilities. Available online: https://www.hfap.org/search-facilities/ (accessed on 1 April 2022).
- The Joint Commission International. JCI-Accredited Organizations. Available online: https://www.jointcommissioninternational.org/about-jci/accredited-organizations/ (accessed on 1 April 2022).
- Masciale, J.N.; Samedy, P.; Ogden, S.; Brauer, S.; Sepkowitz, K.; Granovsky, S. Is hospital patient safety culture relevant? J. Clin. Oncol. 2018, 36, e18775. [Google Scholar] [CrossRef]
- Lee, H.Y.; Lee, E.-K. Safety climate, nursing organizational culture and the intention to report medication errors: A cross-sectional study of hospital nurses. Nurs. Pract. Today 2020, 8, 284–292. [Google Scholar] [CrossRef]
- Toren, O.; Dokhi, M.; Ganz, F.D. Hospital nurses’ intention to report near misses, patient safety culture and professional seniority. Int. J. Qual. Health Care 2021, 33, mzab031. [Google Scholar] [CrossRef]
- Yesilyaprak, T.; Demir Korkmaz, F. The relationship between surgical intensive care unit nurses’ patient safety culture and adverse events. Nurs. Crit. Care 2021. [Google Scholar] [CrossRef] [PubMed]
- Al-Awa, B.; Mazrooa, A.A.; Rayes, O.; Hati, T.E.; Devreux, I.; Al-Noury, K.; Habib, H.; El-Deek, B.S. Benchmarking the post-accreditation patient safety culture at King Abdulaziz University Hospital. Ann. Saudi Med. 2012, 32, 143–150. [Google Scholar] [CrossRef]
- Bogh, S.B.; Blom, A.; Raben, D.C.; Braithwaite, J.; Thude, B.; Hollnagel, E.; Plessen, C.V. Hospital accreditation: Staff experiences and perceptions. Int. J. Health Care Qual. Assur. 2018, 31, 420–427. [Google Scholar] [CrossRef]
- Lee, E. Safety climate and attitude toward medication error reporting after hospital accreditation in South Korea. Int. J. Qual. Health Care 2016, 28, 508–514. [Google Scholar] [CrossRef]
- Kwan, M.R.; Seo, H.J.; Lee, S.J. The association between experience of hospital accreditation and nurses’ perception of patient safety culture in South Korean general hospitals: A cross-sectional study. BMC Nurs. 2021, 20, 195. [Google Scholar] [CrossRef]
- Devkaran, S.; O’Farrell, P.N. The impact of hospital accreditation on clinical documentation compliance: A life cycle explanation using interrupted time series analysis. BMJ Open 2014, 4, e005240. [Google Scholar] [CrossRef]
- Scientific Electronic Library Online. About SciELO. Available online: https://scielo.org/en/about-scielo (accessed on 4 December 2021).
- Nunnally, J.C. Psychometric Theory, 2nd ed.; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 4th ed.; Allyn and Bacon: Needham Heights, MA, USA, 2001. [Google Scholar]
- Squires, A. Methodological challenges in cross-language qualitative research: A research review. Int. J. Nurs. Stud. 2009, 46, 277–287. [Google Scholar] [CrossRef]
- Maneesriwongul, W.; Dixon, J.K. Instrument translation process: A methods review. J. Adv. Nurs. 2004, 48, 175–186. [Google Scholar] [CrossRef]
- Van de Vijver, F.J.R.; Poortinga, Y.H. Towards an integrated analysis of bias in cross-cultural assessment. Eur. J. Psychol. Assess. 1997, 13, 29–37. [Google Scholar] [CrossRef]
- Squires, A.; Aiken, L.H.; van den Heede, K.; Sermeus, W.; Bruyneel, L.; Lindqvist, R.; Schoonhoven, L.; Stromseng, I.; Busse, R.; Brzostek, T.; et al. A systematic survey instrument translation process for multi-country, comparative health workforce studies. Int. J. Nurs. Stud. 2013, 50, 264–273. [Google Scholar] [CrossRef]
- Erkut, S. Developing multiple language versions of instruments for intercultural research. Child Dev. Perspect. 2010, 4, 19–24. [Google Scholar] [CrossRef]
- Mason, T.C. Cross-cultural instrument translation: Assessment, translation, and statistical applications. Am. Ann. Deaf. 2005, 150, 67–72. [Google Scholar] [CrossRef]
- Ximénez, C. Recovery of weak factor loadings when adding the mean structure in confirmatory factor analysis: A simulation study. Front. Psychol. 2016, 6, 1943. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. Translation Guidelines for the AHRQ Surveys on Patient Safety Culture™ (SOPS®); Agency for Healthcare Research and Quality: Rockville, MD, USA, 2022. [Google Scholar]
- Hilgard, J.; Sala, G.; Boot, W.R.; Simons, D.J. Overestimation of action-game training effects: Publication bias and salami slicing. Collabra Psychol. 2019, 5, 30. [Google Scholar] [CrossRef]
- Wallace, M.B.; Bowman, D.; Hamilton-Gibbs, H.; Siersema, P.D. Ethics in publication, part 2: Duplicate publishing, salami slicing, and large retrospective multicenter case series. Endoscopy 2018, 50, 463–465. [Google Scholar] [CrossRef]
- Watson, R.; Pickler, R.; Noyes, J.; Perry, L.; Roe, B.; Hayter, M.; Hueter, I. How many papers can be published from one study? J. Adv. Nurs. 2015, 71, 2457–2460. [Google Scholar] [CrossRef][Green Version]
- Tolsgaard, M.G.; Ellaway, R.; Woods, N.; Norman, G. Salami-slicing and plagiarism: How should we respond? Adv. Health Sci. Educ. 2019, 24, 3–14. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).