Physical Changes of Preschool Children during COVID-19 School Closures in Fujian, China
Abstract
1. Introduction
2. Methods
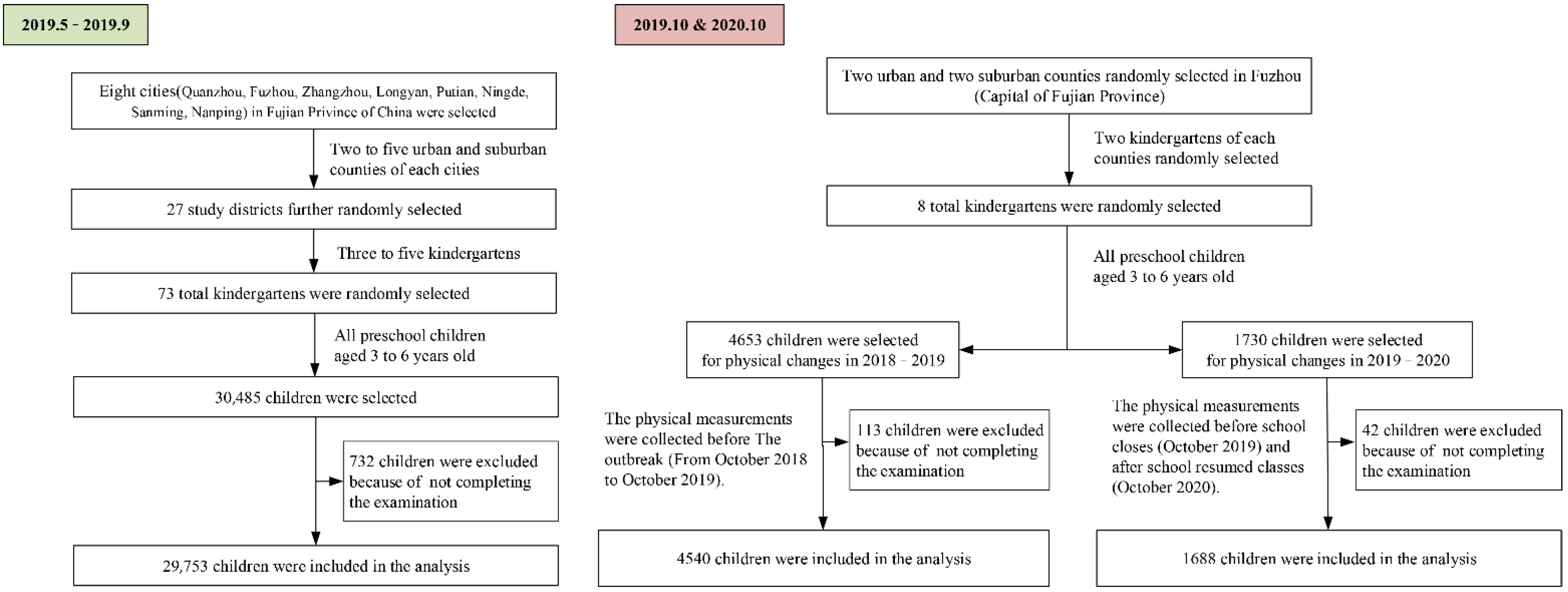
2.1. Study Design and Participants
2.2. Measurements
2.3. Statistical Analysis
3. Results
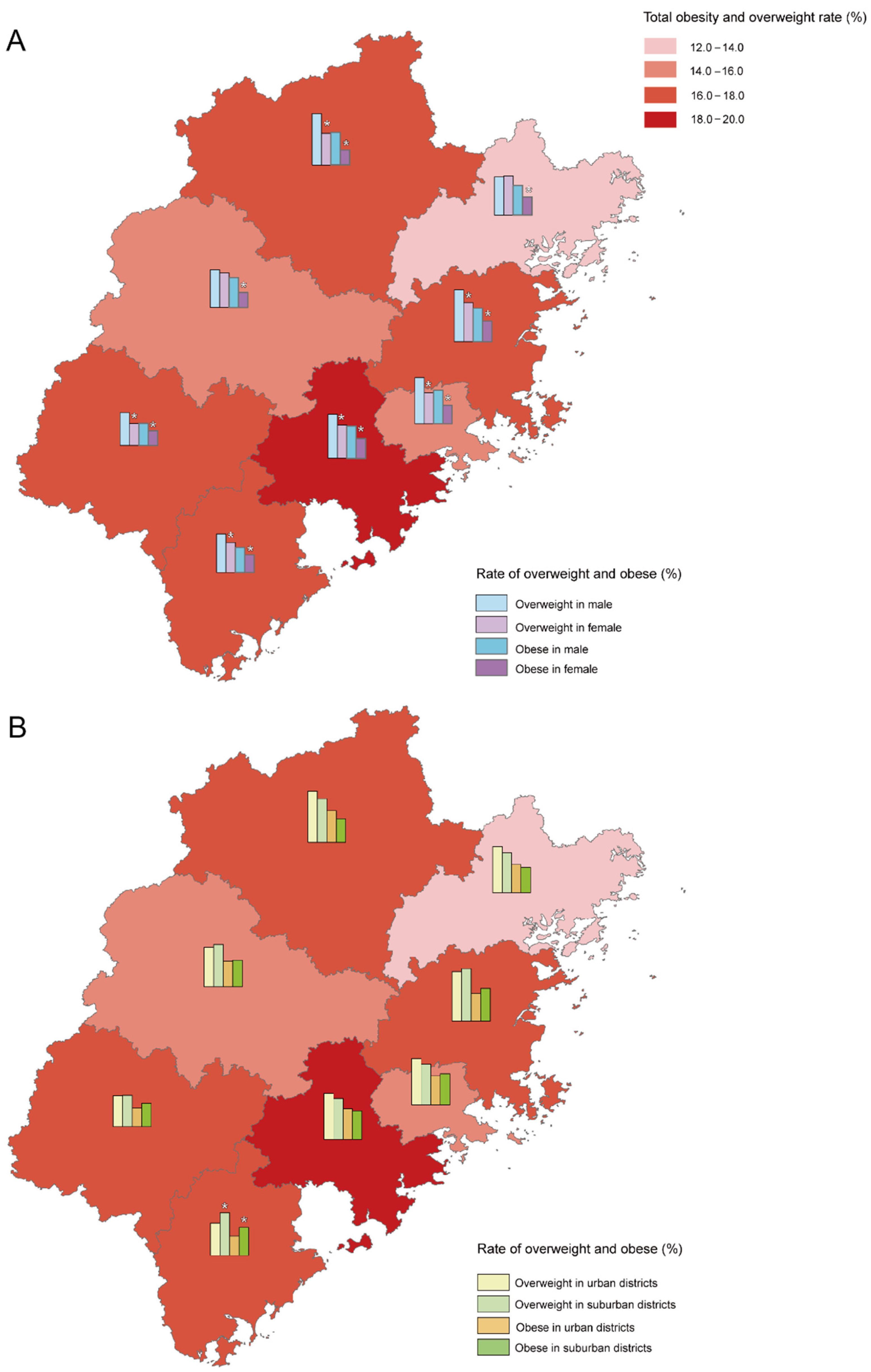
3.1. Physical Status of Preschool Children before the COVID-19 Outbreak in Fujian, China
3.2. Physical Development of Preschool Children of Different Age Groups before and after the Outbreak
3.3. Physical Development of Different Sexes after the Outbreak
3.4. Physical Development of Different Regions after the Outbreak
4. Discussion
4.1. Regional Factors
4.2. Sex Factors
4.3. Age Groups
4.4. Lifestyle Change by Public Health Policy
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Sample Size Calculation
Appendix A.1. PART I Physical Status of Preschool Children before the COVID-19 Outbreak in Fujian, China
Appendix A.2. PART II Physical Development of Preschool Children before and after the Outbreak
Appendix B. Investigation areas
| City | Districts and Counties | Number of Kindergartens |
|---|---|---|
| Fuzhou | Cangshan District | 4 |
| Gulou District | 4 | |
| Yongtai County | 4 | |
| Minqing County | 3 | |
| Longyan | Shilla District | 4 |
| Zhangping | 2 | |
| Wu Ping | 2 | |
| Nanping | Yanping District | 3 |
| Wuyi Mountain | 4 | |
| Ningde | Jiaocheng District | 4 |
| Fuding | 4 | |
| Putian | Chengxiang District | 4 |
| Xianyou | 4 | |
| Quanzhou | Licheng District | 4 |
| Fortress District | 5 | |
| Luojiang District | 2 | |
| Yongchun | 6 | |
| Jinjiang | 4 | |
| Sanming | Sanyuan District | 3 |
| Mellie District | 2 | |
| Youxi County | 2 | |
| Jianning County | 2 | |
| Zhangzhou | Xiangcheng District | 4 |
| Longwen District | 2 | |
| Longhai | 5 | |
| Total | 87 |
| City | Districts and Counties | Number of Kindergartens |
|---|---|---|
| Fuzhou | Cangshan District | 4 |
| Gulou District | 4 | |
| Yongtai County | 4 | |
| Minqing County | 3 |
References
- Graf, C. Health promotion in children and adolescents—A global challenge. Eur. J. Prev. Cardiol. 2017, 24, 1776–1778. [Google Scholar] [CrossRef]
- Reilly, J.J. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 2017, 377, 1496. [Google Scholar]
- Qiu, X.G.; Ou, P.; Chen, X. Analysis on the nutritional status of children under seven years in Fujian province in 2002 and 2008. Chin. J. Matern. Child Health 2012, 27, 1844–1847. [Google Scholar]
- Capital Institute of Pediatrics; The Coordinating Study Group of Nine Cities on the Physical. A national epidemiological survey on obesity of children under seven years of age in nine cities of China in 2016. Chin. J. Pediatr. 2018, 56, 745–752. [Google Scholar]
- Jenssen, B.P.; Kelly, M.K.; Powell, M.; Bouchelle, Z.; Mayne, S.L.; Fiks, A.G. COVID-19 and changes in child obesity. Pediatrics 2021, 147, e2021050123. [Google Scholar] [CrossRef] [PubMed]
- Ventura, P.S.; Ortigoza, A.F.; Castillo, Y.; Herrero, F.J. Children’s health habits and COVID-19 lockdown in catalonia: Implications for obesity and non-communicable diseases. Nutrients 2021, 13, 1657. [Google Scholar] [CrossRef]
- Kang, H.M.; Jeong, D.C.; Suh, B.K.; Ahn, M.B. The Impact of the Coronavirus Disease-2019 Pandemic on Childhood Obesity and Vitamin D Status. J. Korean Med. Sci. 2021, 36, e21. [Google Scholar] [CrossRef]
- Moore, J.B. COVID-19, childhood obesity, and NAFLD: Colliding pandemics. Lancet Gastroenterol. Hepatol. 2022, 7, 499–501. [Google Scholar] [CrossRef]
- Jenssen, B.P.; Kelly, M.K.; Powell, M.; Bouchelle, Z.; Mayne, S.L.; Fiks, A.G. Association of Changes in Obesity Prevalence with the COVID-19 Pandemic in Youth in Massachusetts. JAMA Pediatr. 2022, 176, 198–201. [Google Scholar]
- Shalitin, S.; Phillip, M.; Yackobovitch-Gavan, M. Changes in body mass index in children and adolescents in Israel during the COVID-19 pandemic. Int. J. Obes. 2022, 46, 1160–1167. [Google Scholar] [CrossRef]
- Patel, B.P.; Sathiyamoorthy, T.; Giruparajah, M.; Toulany, A.; Hamilton, J.K. Weighing in on COVID-19: The impact of the pandemic on children and adolescents with obesity participating in a weight management program. Pediatr. Obes. 2022, 17, e12948. [Google Scholar] [CrossRef]
- He, Y.; Luo, B.; Zhao, L.; Liao, S. Influences of the COVID-19 Pandemic on Obesity and Weight-Related Behaviors among Chinese Children: A Multi-Center Longitudinal Study. Nutrients 2022, 14, 3744. [Google Scholar] [CrossRef]
- González-Muniesa, P.; Mártinez-González, M.A.; Hu, F.B. Obesity. Nat. Rev. Dis. Prim. 2017, 3, 17034. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020, 382, 1708–1720. [Google Scholar]
- Androutsos, O.; Perperidi, M.; Georgiou, C.; Chouliaras, G. Lifestyle changes and determinants of children’s and adolescents’ body weight increase during the first COVID-19 lockdown in Greece: The COV-EAT study. Nutrients 2021, 13, 930. [Google Scholar] [CrossRef]
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19–Related School Closings and Risk of Weight Gain Among Children. Obesity 2020, 28, 1008–1009. [Google Scholar] [CrossRef] [PubMed]
- Von-Hippel, P.T.; Workman, J. From Kindergarten Through Second Grade, U.S. Children’s Obesity Prevalence Grows Only During Summer Vacations. Obesity 2016, 24, 2296–2300. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Geserick, M.; Vogel, M.; Gausche, R. Acceleration of BMI in Early Childhood and Risk of Sustained Obesity. N. Engl. J. Med. 2018, 379, 1303–1312. [Google Scholar] [CrossRef]
- Wen, J.; Zhu, L.; Ji, C. Changes in weight and height among Chinese preschool children during COVID-19 school closures. Int. J. Obes. 2021, 45, 2269–2273. [Google Scholar] [CrossRef]
- Ministry of Health of the People’s Republic of China. Technical Specifications for the Management of Nutritional Diseases in Children (Excerpt). Chin. Community Physician 2012, 28, 28. [Google Scholar]
- Lobstein, T.; Jackson-Leach, R.; Moodie, M.L. Child and adolescent obesity: Part of a bigger picture. Lancet 2015, 385, 2510–2520. [Google Scholar] [CrossRef]
- Song, Y.; Wang, H.J.; Ma, J. BMI-for-age Z-score distribution shifts among Chinese children: Gender disparity. Obesity 2014, 22, 1187–1193. [Google Scholar] [CrossRef]
- Gao, L.; Ma, L.; Xue, H.; Min, J.; Wang, H.; Wang, Y. A 3-year longitudinal study of effects of parental perception of children’s ideal body image on child weight change: The Childhood Obesity Study in China mega-cities. Prev. Med. 2020, 132, 105971. [Google Scholar] [CrossRef] [PubMed]
- Qiu, N.; He, H.; Qiao, L.; Ding, Y.; Ji, S.; Guo, X.; Luo, J.; Luo, Z.; Li, Y.; Pang, H.; et al. Sex differences in changes in BMI and blood pressure in Chinese school-aged children during the COVID-19 quarantine. Int. J. Obes. 2021, 45, 2132–2136. [Google Scholar] [CrossRef] [PubMed]
- An, R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: A microsimulation model. J. Sport Health Sci. 2020, 9, 302–312. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Maltoni, G.; Zioutas, M.; Deiana, G.; Biserni, G.B.; Pession, A.; Zucchini, S. Gender differences in weight gain during lockdown due to COVID-19 pandemic in adolescents with obesity. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2181–2185. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Roso, M.B.; de Carvalho Padilha, P.; Mantilla-Escalante, D.C.; Ulloa, N.; Brun, P.; Acevedo-Correa, D.; Peres, W.; Martorell, M.; Aires, M.T. Covid-19 confifinement and changes of adolescent’s dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients 2020, 12, 1807. [Google Scholar]
- Arvidsson, L.; Eiben, G.; Hunsberger, M. Bidirectional associations between psychosocial well-being and adherence to healthy dietary guidelines in European children: Prospective findings from the IDEFICS study. BMC Public Health 2017, 17, 926. [Google Scholar] [CrossRef]
- Holmes, K.L.; Rollo, M.E.; Collins, C.E. Do the contemporary dietary patterns of children align with national food and nutrient recommendations? J. Hum. Nutr. Diet. 2018, 31, 670–682. [Google Scholar] [CrossRef]
- Qin, Z.; Liang, G.; Hu, Y. Relationship between outdoor activities, body mass index and vitamin D nutritional status in children. Chin. J. Child Health 2017, 25, 334–337. [Google Scholar]
- Calcaterra, V.; Vandoni, M.; Pellino, V.C.; Cena, H. Special Attention to Diet and Physical Activity in Children and Adolescents with Obesity During the Coronavirus Disease-2019 Pandemic. Front. Pediatr. 2020, 8, 407. [Google Scholar] [CrossRef]
- Poti, J.M.; Braga, B.; Qin, B. Ultra-processed Food Intake and Obesity: What Really Matters for Health—Processing or Nutrient Content? Curr. Obes. Rep. 2017, 6, 420–431. [Google Scholar] [CrossRef]
- Guan, H.; Okely, A.D.; Aguilar-Farias, N.; Del Pozo Cruz, B.; Draper, C.E.; El Hamdouchi, A.; Florindo, A.A.; Jáuregui, A.; Katzmarzyk, P.T.; Kontsevaya, A.; et al. Promoting healthy movement behaviours among children during the COVID-19 pandemic. Lancet Child Adolesc. Health 2020, 4, 416–418. [Google Scholar] [CrossRef]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020, 20, 1351. [Google Scholar] [CrossRef]
- Fang, K.; Mu, M.; Liu, K.; He, Y. Screen time and childhood overweight/obesity: A systematic review and meta-analysis. Child Care Health Dev. 2019, 45, 744–753. [Google Scholar] [CrossRef]
- Nagata, J.M.; Abdel-Magid, H.S.; Pettee-Gabriel, K. Screen Time for Children and Adolescents during the Coronavirus Disease Pandemic. Obesity 2020, 28, 1582–1583. [Google Scholar] [CrossRef]
- Robinson, T.N.; Banda, J.A.; Hale, L. Screen Media Exposure and Obesity in Children and Adolescents. Pediatrics 2017, 140, S97–S101. [Google Scholar] [CrossRef]
- Ribeiro, K.D.D.S.; Garcia, L.R.S.; Dametto, J.F.D.S.; Assunção, D.G.F.; Maciel, B.L.L. COVID-19 and Nutrition: The Need for Initiatives to Promote Healthy Eating and Prevent Obesity in Childhood. Child. Obes. 2020, 16, 235–237. [Google Scholar] [CrossRef]
- Asigbee, F.M.; Davis, J.N.; Markowitz, A.K. The Association Between Child Cooking Involvement in Food Preparation and Fruit and Vegetable Intake in a Hispanic Youth Population. Curr. Dev. Nutr. 2020, 4, nzaa028. [Google Scholar] [CrossRef] [PubMed]
- Brazendale, K.; Beets, M.W.; Weaver, R.G. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- US Preventive Services Task Force; Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W., Jr.; Kemper, A.R.; Krist, A.H.; et al. Screening for obesity in children and adolescents: US preventive services task force recommendation statement. JAMA 2017, 31, 2417–2426. [Google Scholar]
- Dabas, A.; Seth, A. Prevention and management of childhood obesity. Indian J. Pediatr. 2018, 85, 546–553. [Google Scholar] [CrossRef]
- Lambrinou, C.P.; Androutsos, O.; Karaglani, E.; Cardon, G.; Huys, N.; Wikström, K.; Kivelä, J.; Ko, W.; Karuranga, E.; Tsochev, K. Effective strategies for childhood obesity prevention via school based, family involved interventions: A critical review for the development of the Feel 4 Diabetes-study school based component. BMC Endocr. Disord. 2020, 20, 52. [Google Scholar] [CrossRef]
- Wethington, H.R.; Finnie, R.K.C.; Buchanan, L.R. Healthier food and beverage interventions in schools: Four community guide systematic reviews. Am. J. Prev. Med. 2020, 59, e15–e26. [Google Scholar] [CrossRef]
- Escaron, A.L.; Martinez, C.; Lara, M.; Vega-Herrera, C.; Rios, D.; Lara, M.; Hochman, M. Program Evaluation of Environmental and Policy Approaches to Physical Activity Promotion in a Lower Income Latinx School District in Southeast Los Angeles. Int. J. Environ. Res. Public Health 2020, 17, 8405. [Google Scholar] [CrossRef]
- Alsharairi, N.A. Current Government Actions and Potential Policy Options for Reducing Obesity in Queensland Schools. Children 2018, 5, 18. [Google Scholar] [CrossRef]
- Vandoni, M.; Carnevale Pellino, V.; Gatti, A.; Lucini, D.; Mannarino, S.; Larizza, C.; Rossi, V.; Tranfaglia, V.; Pirazzi, A.; Biino, V.; et al. Effects of an Online Supervised Exercise Training in Children with Obesity during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 9421. [Google Scholar] [CrossRef]
- Guo, J.; Lin, H.; Ou, P. Investigation on the prevalence of simple obesity in preschool children in Fuzhou and analysis of high risk factors. Chin. J. Contemp. Pediatr. 2018, 20, 60–64. [Google Scholar]

| Variable | Age 3–4 | t/Z | p | Age 4–5 | t/Z | p | Age 5–6 | t/Z | p | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prepandemic | After the Outbreak | Prepandemic | After the Outbreak | Prepandemic | After the Outbreak | |||||||
| Total | 1307 | 435 | 1143 | 706 | 669 | 215 | ||||||
| Height, cm | 7.76 ± 1.79 | 9.31 ± 1.55 | −17.344 | <0.001 | 6.85 ± 1.88 | 7.00 ± 3.79 | −0.931 | 0.352 | 6.27 ± 2.02 | 7.69 ± 7.40 | −4.483 | <0.001 |
| Weight, kg | 2.71 ± 1.17 | 3.56 ± 1.61 | −10.086 | <0.001 | 2.43 ± 1.40 | 2.80 ± 1.41 | −5.485 | <0.001 | 2.66 ± 1.37 | 2.67 ± 1.33 | −0.178 | 0.859 |
| BMI | 0.08 | 0.24 | −4.195 | <0.001 | 0.56 | 0.15 | −3.589 | <0.001 | 0.29 | 0.04 | −4.787 | <0.001 |
| (−0.38–0.59) | (−0.21–0.89) | (−0.53–0.64) | (−0.28–0.68) | (−0.16–0.81) | (−0.45–0.67) | |||||||
| Girl | 615 | 180 | 484 | 308 | 294 | 88 | ||||||
| Height, cm | 7.87 ± 1.76 | 9.53 ± 1.73 * | −11.110 | <0.001 | 6.92 ± 1.83 | 6.91 ± 1.40 | 0.074 | 0.941 | 6.20 ± 1.95 | 7.12 ± 1.35 | −8.076 | <0.001 |
| Weight, kg | 2.68 ± 1.14 | 3.48 ± 1.45 | −6.772 | <0.001 | 2.34 ± 1.25 | 2.69 ± 1.24 | −3.888 | <0.001 | 2.64 ± 1.32 | 2.35 ± 0.92 * | 0.233 | 0.021 |
| BMI | 0.01 (−0.35–0.50) | 0.21 (−0.26–0.68) | −2.536 | 0.011 | 0.03 (−0.54–0.51) | 0.11 (−0.30–0.64) | −2.279 | 0.023 | 0.35 (−0.14–0.89) | 0.10 (−0.42–0.32) | −4.972 | <0.001 |
| Boy | 692 | 255 | 658 | 398 | 375 | 127 | ||||||
| Height, cm | 7.66 ± 1.81 | 9.16 ± 1.40 | −13.466 | <0.001 | 6.81 ± 1.91 | 7.07 ± 4.89 | −1.187 | 0.236 | 6.32 ± 2.07 | 8.08 ± 9.56 | −3.353 | 0.001 |
| Weight, kg | 2.73 ± 1.18 | 3.61 ± 1.72 | −7.494 | <0.001 | 2.50 ± 1.50 | 2.88 ± 1.52 | −4.003 | <0.001 | 2.67 ± 1.40 | 2.89 ± 1.53 | −1.511 | 0.116 |
| BMI | 0.08 (−0.38–0.59) | 0.24 (−0.21–0.88) | −3.264 | 0.001 | 0.07 (−0.53–0.63) | 0.15 (−0.28–0.68) | −2.819 | 0.005 | 0.25 (−0.19–0.80) | 0.04 (−0.46–0.68) | 2.109 | 0.035 |
| Variable | Age 3–4 | t/Z | p | Age 4–5 | t/Z | p | Age 5–6 | t/Z | p | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Girl (n = 180) | Boy (n = 255) | Girl (n = 308) | Boy (n = 398) | Girl (n = 88) | Boy (n = 127) | |||||||
| Height, cm | 9.53 ± 1.73 | 9.16 ± 1.40 | 2.429 | 0.016 | 6.91 ± 1.40 | 7.06 ± 4.89 | −0.616 | 0.538 | 7.12 ± 1.35 | 8.08 ± 9.56 | −1.047 | 0.295 |
| Weight, kg | 3.48 ± 1.45 | 3.61 ± 1.72 | −0.846 | 0.398 | 2.69 ± 1.23 | 2.88 ± 1.52 | −1.787 | 0.074 | 2.35 ± 0.92 | 2.89 ± 1.52 | −3.255 | 0.001 |
| BMI | 0.21 (−0.26–0.68) | 0.24 (−0.21–0.88) | −1.158 | 0.247 | 0.11 (−0.30–0.64) | 0.15 (−0.28–0.68) | −1.132 | 0.258 | −0.10 (−0.42–0.32) | 0.04 (−0.45–0.67) | −1.888 | 0.059 |
| Variable | Age 3–4 | t/Z | p | Age 4–5 | t/Z | p | Age 5–6 | t/Z | p | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Urban (n = 184) | Suburban (n = 251) | Urban (n = 555) | Suburban (n = 151) | Urban (n = 104) | Suburban (n = 111) | |||||||
| Height, cm | 9.53 ± 1.70 | 9.15 ± 1.42 | 2.538 | 0.011 | 6.77 ± 1.21 | 7.84 ± 7.81 | −3.204 | 0.001 | 6.91 ± 1.25 | 8.42 ± 10.19 | −4.167 | <0.001 |
| Weight, kg | 3.81 ± 1.86 | 3.37 ± 1.38 | 2.624 | 0.009 | 2.91 ± 1.44 | 2.38 ± 1.18 | 4.584 | <0.001 | 2.96 ± 1.43 | 2.41 ± 1.19 | 3.063 | 0.002 |
| BMI | 0.23 | 0.24 | −1.194 | 0.232 | 0.19 | −0.12 | 4.64 | <0.001 | 0.18 | −0.19 | 2.819 | 0.005 |
| (−0.22–0.93) | (−0.25–0.69) | (−0.23–0.70) | (−0.54–0.34) | (−0.35–0.71) | (−0.49–0.33) | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, G.; Yang, L.; Xu, X.; Chen, M.; Cai, Y.; Wen, Y.; Xie, X.; Lu, X.; Luo, S.; Lin, S.; et al. Physical Changes of Preschool Children during COVID-19 School Closures in Fujian, China. Int. J. Environ. Res. Public Health 2022, 19, 13699. https://doi.org/10.3390/ijerph192013699
Li G, Yang L, Xu X, Chen M, Cai Y, Wen Y, Xie X, Lu X, Luo S, Lin S, et al. Physical Changes of Preschool Children during COVID-19 School Closures in Fujian, China. International Journal of Environmental Research and Public Health. 2022; 19(20):13699. https://doi.org/10.3390/ijerph192013699
Chicago/Turabian StyleLi, Guobo, Le Yang, Xingyan Xu, Mingjun Chen, Yingying Cai, Yeying Wen, Xiaoxu Xie, Xinyue Lu, Suping Luo, Shaowei Lin, and et al. 2022. "Physical Changes of Preschool Children during COVID-19 School Closures in Fujian, China" International Journal of Environmental Research and Public Health 19, no. 20: 13699. https://doi.org/10.3390/ijerph192013699
APA StyleLi, G., Yang, L., Xu, X., Chen, M., Cai, Y., Wen, Y., Xie, X., Lu, X., Luo, S., Lin, S., Li, H., & Wu, S. (2022). Physical Changes of Preschool Children during COVID-19 School Closures in Fujian, China. International Journal of Environmental Research and Public Health, 19(20), 13699. https://doi.org/10.3390/ijerph192013699






