Pilates and Cognitive Stimulation in Dual Task an Intervention Protocol to Improve Functional Abilities and Minimize the Rate of Age-Related Cognitive Decline in Postmenopausal Women
Abstract
1. Introduction
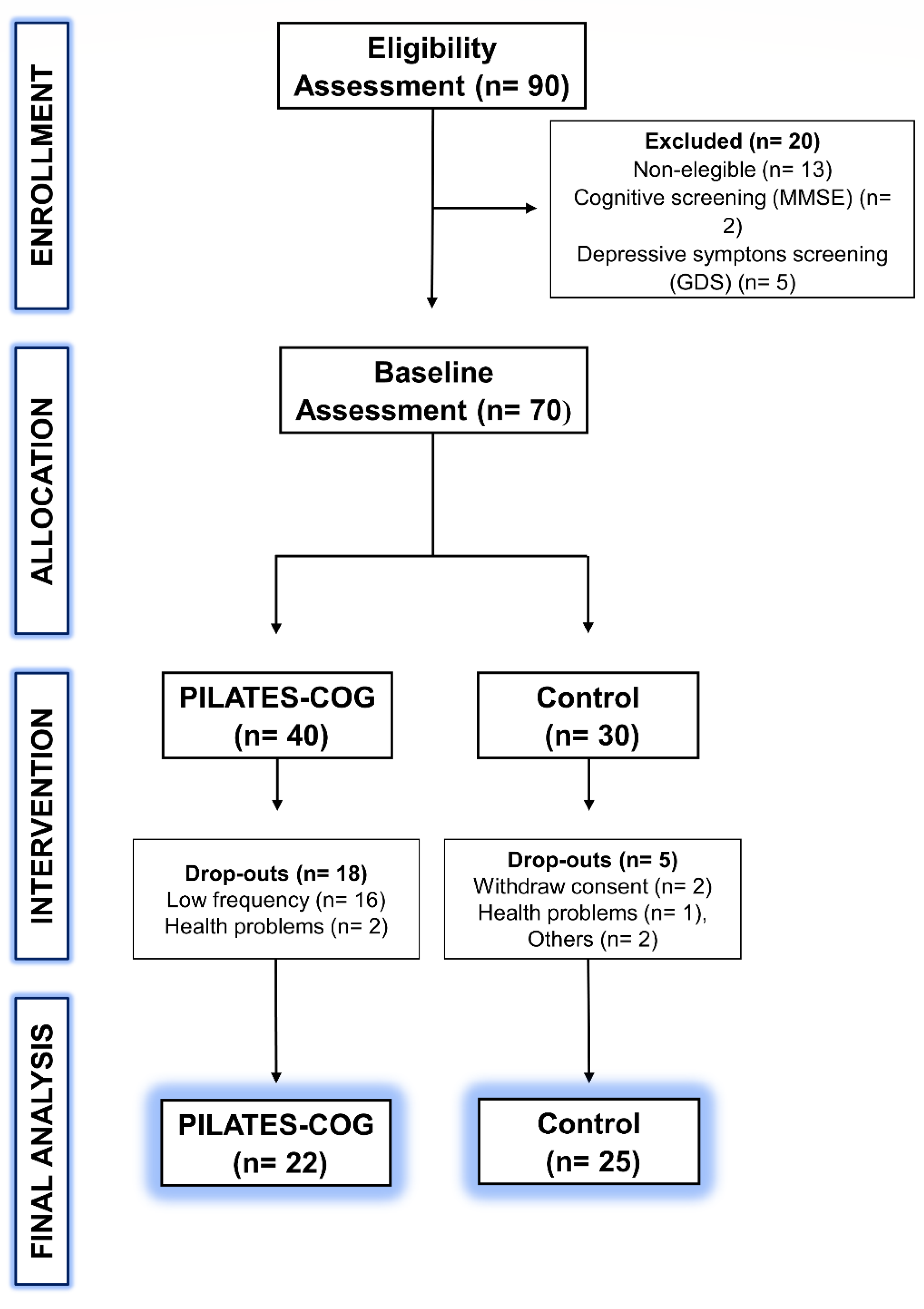
2. Materials and Methods
2.1. Trial Design
2.2. Eligibility Criteria
2.3. PILATES-COG Protocol and Control Group
2.4. Primary Outcome
2.5. Secondary Outcome
2.6. Sample Size
2.7. Allocation
2.8. Statistical Analyses
3. Results
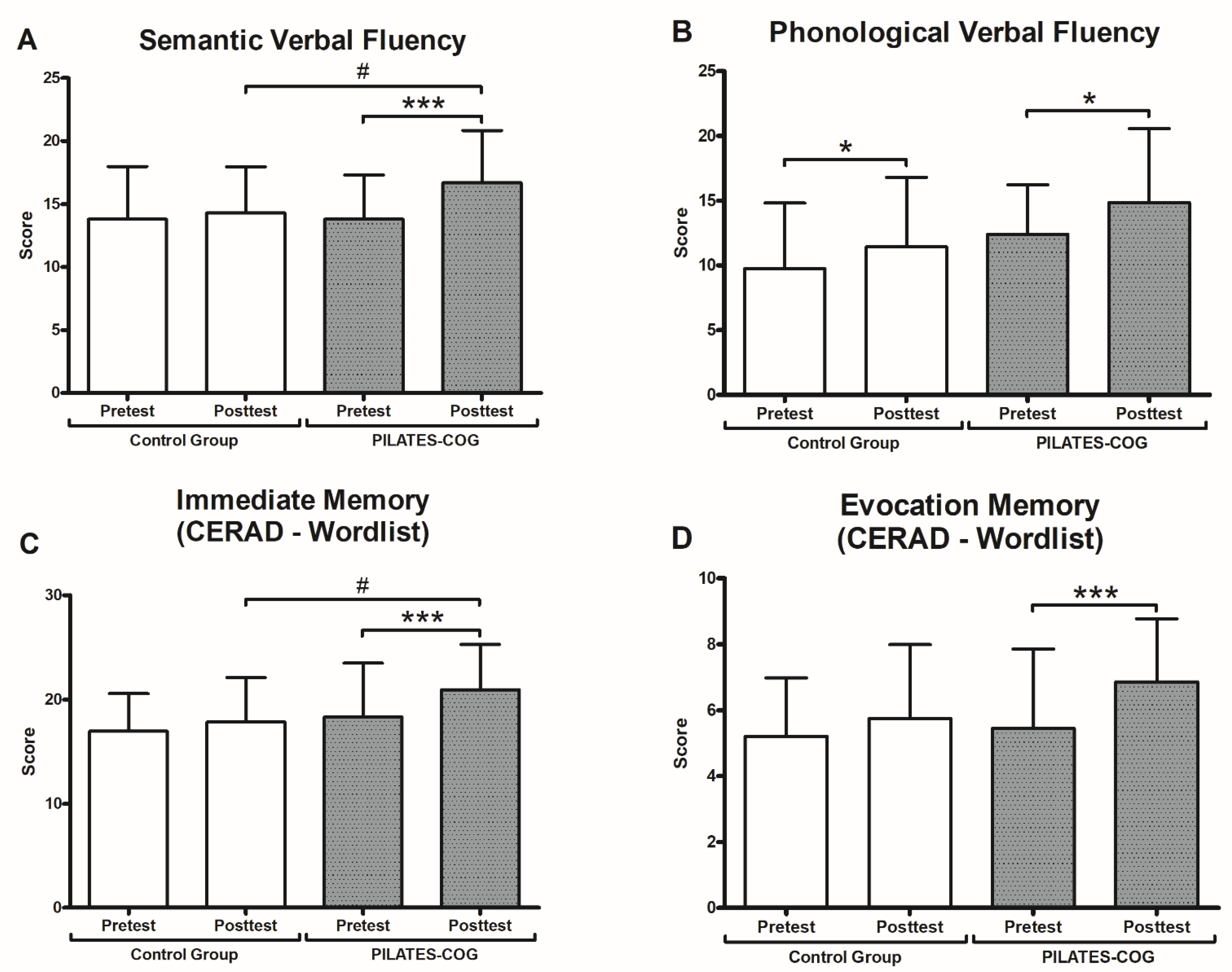
3.1. Cognitive Performance Results
3.2. Physical Functional Performance Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Erickson, K.I.; Donofry, S.D.; Sewell, K.R.; Brown, B.M.; Stillman, C.M. Cognitive Aging and the Promise of Physical Activity. Annu. Rev. Clin. Psychol. 2022, 18, 417–442. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.B.; Silver, R.E.; Das, S.K.; Fielding, R.A.; Gilhooly, C.H.; Jacques, P.F.; Kelly, J.M.; Mason, J.B.; McKeown, N.M.; Reardon, M.A.; et al. Healthy Aging—Nutrition Matters: Start Early and Screen Often. Adv. Nutr. 2021, 12, 1438–1448. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.J.; Veronese, N.; Vernuccio, L.; Catanese, G.; Inzerillo, F.; Salemi, G.; Barbagallo, M. Nutrition, Physical Activity, and Other Lifestyle Factors in the Prevention of Cognitive Decline and Dementia. Nutrients 2021, 13, 4080. [Google Scholar] [CrossRef] [PubMed]
- Sachdev, P.S. Social Health, Social Reserve and Dementia. Curr. Opin. Psychiatry 2022, 35, 111–117. [Google Scholar] [CrossRef]
- Seto, M.; Weiner, R.L.; Dumitrescu, L.; Hohman, T.J. Protective Genes and Pathways in Alzheimer’s Disease: Moving towards Precision Interventions. Mol. Neurodegener. 2021, 16, 29. [Google Scholar] [CrossRef]
- Bellver-Sanchis, A.; Pallàs, M.; Griñán-Ferré, C. The Contribution of Epigenetic Inheritance Processes on Age-Related Cognitive Decline and Alzheimer’s Disease. Epigenomes 2021, 5, 15. [Google Scholar] [CrossRef]
- Babaei, P.; Azari, H.B. Exercise Training Improves Memory Performance in Older Adults: A Narrative Review of Evidence and Possible Mechanisms. Front. Hum. Neurosci. 2022, 15, 771553. [Google Scholar] [CrossRef]
- Gkotzamanis, V.; Magriplis, E.; Panagiotakos, D. The Effect of Physical Activity Interventions on Cognitive Function of Older Adults: A Systematic Review of Clinical Trials. Psychiatriki 2022, 22, 983–998. [Google Scholar] [CrossRef]
- Jardim, N.Y.V.; Bento-Torres, N.V.O.; Costa, V.O.; Carvalho, J.P.R.; Pontes, H.T.S.; Tomás, A.M.; Sosthenes, M.C.K.; Erickson, K.I.; Bento-Torres, J.; Diniz, C.W.P. Dual-Task Exercise to Improve Cognition and Functional Capacity of Healthy Older Adults. Front. Aging Neurosci. 2021, 13, 589299. [Google Scholar] [CrossRef]
- Kaewkaen, K.; Wongsamud, P.; Ngaothanyaphat, J.; Supawarapong, P.; Uthama, S.; Ruengsirarak, W.; Chanabun, S.; Kaewkaen, P. The Influence of Audio-Visual Cueing (Traffic Light) on Dual Task Walking in Healthy Older Adults and Older Adults with Balance Impairments. Malays. J. Med. Sci. 2018, 25, 67–74. [Google Scholar] [CrossRef]
- Magnani, P.E.; Zanellato, N.F.G.; Genovez, M.B.; Alvarenga, I.C.; Faganello-Navega, F.R.; de Abreu, D.C.C. Usual and Dual-Task Gait Adaptations under Visual Stimulation in Older Adults at Different Ages. Aging Clin. Exp. Res. 2022, 34, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.; Cusack, T.; Blake, C. The Effect of a Dual Task on Gait Speed in Community Dwelling Older Adults: A Systematic Review and Meta-Analysis. Gait Posture 2016, 44, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Bruce, H.; Lai, L.; Bherer, L.; Lussier, M.; St.-Onge, N.; Li, K.Z.H. The Effect of Simultaneously and Sequentially Delivered Cognitive and Aerobic Training on Mobility among Older Adults with Hearing Loss. Gait Posture 2019, 67, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Plummer-D’Amato, P.; Altmann, L.J.P.; Saracino, D.; Fox, E.; Behrman, A.L.; Marsiske, M. Interactions between Cognitive Tasks and Gait after Stroke: A Dual Task Study. Gait Posture 2008, 27, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Plummer, P.; Altmann, L.; Feld, J.; Zukowski, L.; Najafi, B.; Giuliani, C. Attentional Prioritization in Dual-Task Walking: Effects of Stroke, Environment, and Instructed Focus. Gait Posture 2020, 79, 3–9. [Google Scholar] [CrossRef]
- Brustio, P.R.; Rabaglietti, E.; Formica, S.; Liubicich, M.E. Dual-Task Training in Older Adults: The Effect of Additional Motor Tasks on Mobility Performance. Arch. Gerontol. Geriatr. 2018, 75, 119–124. [Google Scholar] [CrossRef]
- Doumas, M.; Krampe, R.T. Ecological Relevance Determines Task Priority in Older Adults’ Multitasking. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2015, 70, 377–385. [Google Scholar] [CrossRef]
- Al-Yahya, E.; Dawes, H.; Smith, L.; Dennis, A.; Howells, K.; Cockburn, J. Cognitive Motor Interference While Walking: A Systematic Review and Meta-Analysis. Neurosci. Biobehav. Rev. 2011, 35, 715–728. [Google Scholar] [CrossRef]
- Boisgontier, M.P.; Beets, I.A.M.; Duysens, J.; Nieuwboer, A.; Krampe, R.T.; Swinnen, S.P. Age-Related Differences in Attentional Cost Associated with Postural Dual Tasks: Increased Recruitment of Generic Cognitive Resources in Older Adults. Neurosci. Biobehav. Rev. 2013, 37, 1824–1837. [Google Scholar] [CrossRef]
- Brustio, P.R.; Magistro, D.; Zecca, M.; Rabaglietti, E.; Liubicich, M.E. Age-Related Decrements in Dual-Task Performance: Comparison of Different Mobility and Cognitive Tasks. A Cross Sectional Study. PLoS ONE 2017, 12, e0181698. [Google Scholar] [CrossRef]
- Ramírez, F.; Gutiérrez, M. Dual-Task Gait as a Predictive Tool for Cognitive Impairment in Older Adults: A Systematic Review. Front. Aging Neurosci. 2021, 13, 769462. [Google Scholar] [CrossRef] [PubMed]
- Akin, H.; Senel, A.; Taskiran, H.; Kaya Mutlu, E. Do Motor-Cognitive and Motor–Motor Dual Task Training Effect Differently Balance Performance in Older Adults? Eur. Geriatr. Med. 2021, 12, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Gill, D.P.; Gregory, M.A.; Zou, G.; Liu-Ambrose, T.; Shigematsu, R.; Hachinski, V.; Fitzgerald, C.; Petrella, R.J. The Healthy Mind, Healthy Mobility Trial: A Novel Exercise Program for Older Adults. Med. Sci. Sports Exerc. 2016, 48, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Joubert, C.; Chainay, H. Aging Brain: The Effect of Combined Cognitive and Physical Training on Cognition as Compared to Cognitive and Physical Training Alone—A Systematic Review. Clin. Interv. Aging 2018, 13, 1267–1301. [Google Scholar] [CrossRef] [PubMed]
- Nishiguchi, S.; Yamada, M.; Tanigawa, T.; Sekiyama, K.; Kawagoe, T.; Suzuki, M.; Yoshikawa, S.; Abe, N.; Otsuka, Y.; Nakai, R.; et al. A 12-Week Physical and Cognitive Exercise Program Can Improve Cognitive Function and Neural Efficiency in Community-Dwelling Older Adults: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2015, 63, 1355–1363. [Google Scholar] [CrossRef]
- Tait, J.L.; Duckham, R.L.; Milte, C.M.; Main, L.C.; Daly, R.M. Influence of Sequential vs. Simultaneous Dual-Task Exercise Training on Cognitive Function in Older Adults. Front. Aging Neurosci. 2017, 9, 368. [Google Scholar] [CrossRef] [PubMed]
- Eggenberger, P.; Theill, N.; Holenstein, S.; Schumacher, V.; de Bruin, E.D. Multicomponent Physical Exercise with Simultaneous Cognitive Training to Enhance Dual-Task Walking of Older Adults: A Secondary Analysis of a 6-Month Randomized Controlled Trial with I-Year Follow-Up. Clin. Interv. Aging 2015, 10, 1711–1732. [Google Scholar] [CrossRef]
- Kayama, H.; Okamoto, K.; Nishiguchi, S.; Yamada, M.; Kuroda, T.; Aoyama, T. Effect of a Kinect-Based Exercise Game on Improving Executive Cognitive Performance in Community-Dwelling Elderly: Case Control Study. J. Med. Internet Res. 2014, 16, 3–6. [Google Scholar] [CrossRef]
- Bird, M.L.; Hill, K.D.; Fell, J.W. A Randomized Controlled Study Investigating Static and Dynamic Balance in Older Adults after Training with Pilates. Arch. Phys. Med. Rehabil. 2012, 93, 43–49. [Google Scholar] [CrossRef]
- Długosz-Boś, M.; Filar-Mierzwa, K.; Stawarz, R.; Ścisłowska-Czarnecka, A.; Jankowicz-Szymańska, A.; Bac, A. Effect of Three Months Pilates Training on Balance and Fall Risk in Older Women. Int. J. Environ. Res. Public Health 2021, 18, 3663. [Google Scholar] [CrossRef]
- Bergamin, M.; Gobbo, S.; Bullo, V.; Zanotto, T.; Vendramin, B.; Duregon, F.; Cugusi, L.; Camozzi, V.; Zaccaria, M.; Neunhaeuserer, D.; et al. Effects of a Pilates Exercise Program on Muscle Strength, Postural Control and Body Composition: Results from a Pilot Study in a Group of Post-Menopausal Women. Age 2015, 37, 118. [Google Scholar] [CrossRef] [PubMed]
- Bueno De Souza, R.O.; Marcon, L.D.F.; De Arruda, A.S.F.; Pontes Junior, F.L.; De Melo, R.C. Effects of Mat Pilates on Physical Functional Performance of Older Adults: A Meta-Analysis of Randomized Controlled Trials. Am. J. Phys. Med. Rehabil. 2018, 97, 414–425. [Google Scholar] [CrossRef] [PubMed]
- Buttelli, A.C.K.; Costa, R.R.; Farinha, J.B.; de Oliveira Fagundes, A.; Vieira, A.F.; Barroso, B.M.; Bracht, C.G.; Coconcelli, L.; Reichert, T.; de Mello Bones daRocha, V.; et al. Pilates Training Improves Aerobic Capacity, but Not Lipid or Lipoprotein Levels in Elderly Women with Dyslipidemia: A Controlled Trial. J. Bodyw. Mov. Ther. 2021, 26, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Meikis, L.; Wicker, P.; Donath, L. Effects of Pilates Training on Physiological and Psychological Health Parameters in Healthy Older Adults and in Older Adults with Clinical Conditions over 55 Years: A Meta-Analytical Review. Front. Neurol. 2021, 12, 724218. [Google Scholar] [CrossRef] [PubMed]
- Patti, A.; Zangla, D.; Sahin, F.N.; Cataldi, S.; Lavanco, G.; Palma, A.; Fischietti, F. Physical Exercise and Prevention of Falls. Effects of a Pilates Training Method Compared with a General Physical Activity Program A Randomized Controlled Trial. Medicine 2021, 100, e25289. [Google Scholar] [CrossRef]
- Gárcia-Garro, A.P.; Hita-contreras, F.; Mart, A.; Achalandabaso-ochoa, A.; Jim, D.; Cruz-d, D. Effectiveness of A Pilates Training Program on Cognitive and Functional Abilities in Postmenopausal Women. Int. J. Environ. Res. Public Health 2020, 17, 3580. [Google Scholar] [CrossRef]
- Vieira, N.D.; Testa, D.; Ruas, P.C.; de Fátima Salvini, T.; Catai, A.M.; Melo, R.C. The Effects of 12 Weeks Pilates-Inspired Exercise Training on Functional Performance in Older Women: A Randomized Clinical Trial. J. Bodyw. Mov. Ther. 2017, 21, 251–258. [Google Scholar] [CrossRef]
- Bertolucci, P.H.F.; Brucki, S.M.D.; Campacci, S.R.; Juliano, Y. O Mini-Exame Do Estado Mental Em Uma População Geral: Impacto Da Escolaridade. Arq. De Neuro-Psiquiatr. 1994, 52, 1–7. [Google Scholar] [CrossRef]
- Hoyl, M.T.; Alessi, C.A.; Harker, J.O.; Josephson, K.R.; Pietruszka, F.M.; Koelfgen, M.; Mervis, J.R.; Fitten, L.J.; Rubenstein, L.Z. Development and Testing of a Five-Item Version of the Geriatric Depression Scale. J. Am. Geriatr. Soc. 1999, 47, 873–878. [Google Scholar] [CrossRef]
- De Oliveira, T.C.G.; Soares, F.C.; De Macedo, L.D.E.D.; Diniz, D.L.W.P.; Bento-Torres, N.V.O.; Picanço-Diniz, C.W. Beneficial Effects of Multisensory and Cognitive Stimulation on Age-Related Cognitive Decline in Long-Term-Care Institutions. Clin. Interv. Aging 2014, 9, 309–321. [Google Scholar] [CrossRef]
- Matsudo, S.; Araújo, T.; Matsudo, V.; Andrade, D.; Andrade, E.; Oliveira, L.C.; Braggion, G. Questionário Internacional De Atividade Física (Ipaq): Estudo De Validade E Reprodutibilidade No Brasil. Rev. Bras. Ativ. Fís. Saúde 2012, 6, 5–18. [Google Scholar] [CrossRef]
- Balduino, E.; De Melo, B.A.R.; De Sousa Mota Da Silva, L.; Martinelli, J.E.; Cecato, J.F. The SuperAgers Construct in Clinical Practice: Neuropsychological Assessment of Illiterate and Educated Elderly. Int. Psychogeriatr. 2020, 32, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Caramelli, P.; Carthery-Goulart, M.T.; Porto, C.S.; Charchat-Fichman, H.; Nitrini, R. Category Fluency as a Screening Test for Alzheimer Disease in Illiterate and Literate Patients. Alzheimer Dis. Assoc. Disord. 2007, 21, 65–67. [Google Scholar] [CrossRef] [PubMed]
- Fillenbaum, G.G.; Van Belle, G.; Morris, J.C.; Mohs, R.C.; Mirra, S.S.; Davis, P.C.; Tariot, P.N.; Silverman, J.M.; Clark, C.M.; Welsh-Bohmer, K.A.; et al. CERAD. The First 20 Years. Alzheimer’s Dement. 2008, 4, 96–109. [Google Scholar] [CrossRef] [PubMed]
- Bertolucci, P.H.F.; Okamoto, I.H.; Brucki, S.M.D.; Siviero, M.O.; Neto, J.T.; Ramos, L.R. Applicability of the CERAD Neuropsychological Battery to Brazilian Elderly. Arq. Neuropsiquiatr. 2001, 59, 532–536. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.; Dobson, F.; Hinman, R. Measures of Physical Performance Assessments: Self-Paced Walk Test (SPWT), Stair Climb Test (SCT), Six-Minute Walk Test (6MWT), Chair Stand Test (CST), Timed Up & Go (TUG), Sock Test, Lift and Carry Test (LCT), and Car Task. Arthritis Care Res. 2011, 63, S350–S370. [Google Scholar] [CrossRef]
- Hall, C.D.; Echt, K.V.; Wolf, S.L.; Rogers, W.A. Cognitive and Motor Mechanisms Underlying Older Adults’ Ability to Divide Attention While Walking. Phys. Ther. 2011, 91, 1039–1050. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed ”up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Rikli, R.E.; Jones, C.J. Development and Validation of a Functional Fitness Test for Community-Residing Older Adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Bjerregaard, P.; Ottendahl, C.B.; Jørgensen, M.E. Hand Grip Strength and Chair Stand Test amongst Greenlandic Inuit: Reference Values and International Comparisons. Int. J. Circumpolar Health 2021, 80, 1966186. [Google Scholar] [CrossRef]
- Franchignoni, F.; Godi, M.; Guglielmetti, S.; Nardone, A.; Giordano, A. Enhancing the Usefulness of the Mini-BESTest for Measuring Dynamic Balance: A Rasch Validation Study. Eur. J. Phys. Rehabil. Med. 2015, 51, 429–437. [Google Scholar] [PubMed]
- O’Hoski, S.; Sibley, K.M.; Brooks, D.; Beauchamp, M.K. Construct Validity of the BESTest, Mini-BESTest and BriefBESTest in Adults Aged 50 Years and Older. Gait Posture 2015, 42, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go Test a Useful Predictor of Risk of Falls in Community Dwelling Older Adults: A Systematic Review and Meta- Analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef]
- Asai, T.; Oshima, K.; Fukumoto, Y.; Yonezawa, Y.; Matsuo, A.; Misu, S. Does Dual-Tasking Provide Additional Value in Timed “up and Go” Test for Predicting the Occurrence of Falls? A Longitudinal Observation Study by Age Group (Young-Older or Old-Older Adults). Aging Clin. Exp. Res. 2021, 33, 77–84. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and Reporting Effect Sizes to Facilitate Cumulative Science: A Practical Primer for t-Tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [PubMed]
- Abasıyanık, Z.; Yiğit, P.; Özdoğar, A.T.; Kahraman, T.; Ertekin, Ö.; Özakbaş, S. A Comparative Study of the Effects of Yoga and Clinical Pilates Training on Walking, Cognition, Respiratory Functions, and Quality of Life in Persons with Multiple Sclerosis: A Quasi-Experimental Study. Explore 2021, 17, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Küçük, F.; Kara, B.; Poyraz, E.Ç.; İdiman, E. Improvements in Cognition, Quality of Life, and Physical Performance with Clinical Pilates in Multiple Sclerosis: A Randomized Controlled Trial. J. Phys. Ther. Sci. 2016, 28, 761–768. [Google Scholar] [CrossRef]
- Marques, K.A.P.; Trindade, C.B.B.; Almeida, M.C.V.; Bento-Torres, N.V.O. Pilates for Rehabilitation in Patients with Multiple Sclerosis: A Systematic Review of Effects on Cognition, Health-Related Physical Fitness, General Symptoms and Quality of Life. J. Bodyw. Mov. Ther. 2020, 24, 26–36. [Google Scholar] [CrossRef]
- Briegas, J.J.M.; Iglesias, A.I.S.; Ballester, S.G.; Castro, F.V. The Well-Being of the Elderly: Memory and Aging. Front. Psychol. 2020, 11, 778. [Google Scholar] [CrossRef]
- Hall, J.R.; Harvey, M.; Vo, H.T.; O’Bryant, S.E. Performance on a Measure of Category Fluency in Cognitively Impaired Elderly. Aging Neuropsychol. Cogn. 2011, 18, 353–361. [Google Scholar] [CrossRef]
- Singh-Manoux, A.; Kivimaki, M.; Glymour, M.M.; Elbaz, A.; Berr, C.; Ebmeier, K.P.; Ferrie, J.E.; Dugravot, A. Timing of Onset of Cognitive Decline: Results from Whitehall II Prospective Cohort Study. BMJ 2012, 344, d7622. [Google Scholar] [CrossRef] [PubMed]
- Bussy, A.; Patel, R.; Plitman, E.; Tullo, S.; Salaciak, A.; Bedford, S.A.; Farzin, S.; Béland, M.L.; Valiquette, V.; Kazazian, C.; et al. Hippocampal Shape across the Healthy Lifespan and Its Relationship with Cognition. Neurobiol. Aging 2021, 106, 153–168. [Google Scholar] [CrossRef] [PubMed]
- Nobis, L.; Manohar, S.G.; Smith, S.M.; Alfaro-Almagro, F.; Jenkinson, M.; Mackay, C.E.; Husain, M. Hippocampal Volume across Age: Nomograms Derived from over 19,700 People in UK Biobank. NeuroImage Clin. 2019, 23, 101904. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.J.; Lin, C.H.; Lane, H.Y. From Menopause to Neurodegeneration—Molecular Basis and Potential Therapy. Int. J. Mol. Sci. 2021, 22, 8654. [Google Scholar] [CrossRef]
- Yokoyama, H.; Okazaki, K.; Imai, D.; Yamashina, Y.; Takeda, R.; Naghavi, N.; Ota, A.; Hirasawa, Y.; Miyagawa, T. The Effect of Cognitive-Motor Dual-Task Training on Cognitive Function and Plasma Amyloid β Peptide 42/40 Ratio in Healthy Elderly Persons: A Randomized Controlled Trial. BMC Geriatr. 2015, 15, 60. [Google Scholar] [CrossRef]
- Rezola-Pardo, C.; Arrieta, H.; Gil, S.M.; Zarrazquin, I.; Javier, J.; López, M.A.; Irazusta, J.; Rodriguez-larrad, A. Comparison between Multicomponent and Simultaneous Dual-Task Exercise Interventions in Long-Term Nursing Home Residents: The Ageing-ON DUAL-TASK Randomized Controlled Study. Age Ageing 2019, 2019, 817–823. [Google Scholar] [CrossRef]
- Hita-Contreras, F.; Martínez-Amat, A.; Cruz-Díaz, D.; Pérez-López, F.R. Fall Prevention in Postmenopausal Women: The Role of Pilates Exercise Training. Climacteric 2016, 19, 229–233. [Google Scholar] [CrossRef]
- Bergquist, R.; Nerz, C.; Taraldsen, K.; Mellone, S.; Ihlen, E.A.F.; Vereijken, B.; Helbostad, J.L.; Becker, C.; Stefanie Mikolaizak, A. Predicting Advanced Balance Ability and Mobility with an Instrumented Timed up and Go Test. Sensors 2020, 20, 4987. [Google Scholar] [CrossRef]
- Coni, A.; Van Ancum, J.M.; Bergquist, R.; Mikolaizak, A.S.; Mellone, S.; Chiari, L.; Maier, A.B.; Pijnappels, M. Comparison of Standard Clinical and Instrumented Physical Performance Tests in Discriminating Functional Status of High-Functioning People Aged 61–70 Years Old. Sensors 2019, 19, 449. [Google Scholar] [CrossRef]
- Svinøy, O.E.; Hilde, G.; Bergland, A.; Strand, B.H. Timed up and Go: Reference Values for Community-Dwelling Older Adults with and without Arthritis and Non-Communicable Diseases: The Tromsø Study. Clin. Interv. Aging 2021, 16, 335–343. [Google Scholar] [CrossRef]
- Plummer, P.; Zukowski, L.A.; Giuliani, C.; Hall, A.M.; Zurakowski, D. Effects of Physical Exercise Interventions on Gait-Related Dual-Task Interference in Older Adults: A Systematic Review and Meta-Analysis. Gerontology 2015, 62, 94–117. [Google Scholar] [CrossRef] [PubMed]
- De Souza Cavina, A.P.; Pizzo Junior, E.; MacHado, A.F.; Biral, T.M.; Pastre, C.M.; Vanderlei, F.M. Load Monitoring on Pilates Training: A Study Protocol for a Randomized Clinical Trial. Trials 2019, 20, 597. [Google Scholar] [CrossRef] [PubMed]
- de Souza Cavina, A.P.; Junior, E.P.; Machado, A.F.; Biral, T.M.; Lemos, L.K.; Rodrigues, C.R.D.; Pastre, C.M.; Vanderlei, F.M. Effects of the Mat Pilates Method on Body Composition: Systematic Review with Meta-Analysis. J. Phys. Act. Health 2020, 17, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Plummer, P.; Eskes, G. Measuring Treatment Effects on Dual-Task Performance: A Framework for Research and Clinical Practice. Front. Hum. Neurosci. 2015, 9, 225. [Google Scholar] [CrossRef] [PubMed]
- Agmon, M.; Kelly, V.E.; Logsdon, R.G.; Nguyen, H.; Belza, B. The Effects of Enhancefitness (EF) Training on Dual-Task Walking in Older Adults. J. Appl. Gerontol. 2015, 34, NP128–NP142. [Google Scholar] [CrossRef] [PubMed]
- Jutten, R.J.; Grandoit, E.; Foldi, N.S.; Sikkes, S.A.M.; Jones, R.N.; Choi, S.E.; Lamar, M.L.; Louden, D.K.N.; Rich, J.; Tommet, D.; et al. Lower Practice Effects as a Marker of Cognitive Performance and Dementia Risk: A Literature Review. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2020, 12, e12055. [Google Scholar] [CrossRef]
- Goldberg, T.E.; Harvey, P.D.; Wesnes, K.A.; Snyder, P.J.; Schneider, L.S. Practice Effects Due to Serial Cognitive Assessment: Implications for Preclinical Alzheimer’s Disease Randomized Controlled Trials. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2015, 1, 103–111. [Google Scholar] [CrossRef]
- Fiatarone Singh, M.A.; Gates, N.; Saigal, N.; Wilson, G.C.; Meiklejohn, J.; Brodaty, H.; Wen, W.; Singh, N.; Baune, B.T.; Suo, C.; et al. The Study of Mental and Resistance Training (SMART) Study—Resistance Training and/or Cognitive Training in Mild Cognitive Impairment: A Randomized, Double-Blind, Double-Sham Controlled Trial. J. Am. Med. Dir. Assoc. 2014, 15, 873–880. [Google Scholar] [CrossRef]
- Spiteri, K.; Broom, D.; Hassan Bekhet, A.; Xerri de Caro, J.; Laventure, B.; Grafton, K. Barriers and Motivators of Physical Activity Participation in Middle-Aged and Older Adults—A Systematic Review. J. Aging Phys. Act. 2019, 27, 929–944. [Google Scholar] [CrossRef]

| Session | Pilates Exercise | Cognitive Training Simultaneous to Exercise |
|---|---|---|
| 1 & 2 | One Leg Circles, One Leg Up and Down, Side Kicks Up and Down, Side Kick Inner Thigh Lift, Knee to Chest, Shoulder Bridge. | A participant started a grocery store shopping list sequence saying: “I went to the grocery and bought an…” (e.g., apple). The closest participant was asked to repeat the previous statement and add a new item to the shopping list. The process was continuous and items cumulative until everyone in the group had contributed. |
| 3 & 4 | Spine and Hamstring Stretch (Standing), Squat + shoulder flexion, One Leg Circles with a stick (Standing), Side Kicks (Hip abduction), Shoulder bridge, Shoulder Bridge with gluteal lift, leg circles and leg Up and Down. | The participants had to speak three words, and then make simple arithmetical task, and then recall the three words previously said. |
| 5 & 6 | Shoulder bridge with a ball, leg circles, Leg Up and Down, Bird Dog, roll over and dorsal extension | Serial addition and subtraction calculations of 3, 5, and 7. |
| 7 & 8 | Shoulder bridge with a ball, hip flexion holding ball, push-ups with knee support, air squat, leg Up and Down with hip extension (airplane), lunge with a stick | The participants were encouraged to speak letters from the alphabet, intercalate, and/or try listing objects from different rooms of a house. |
| 9 &10 | Single Leg Stretch, Leg Inclination, Plank, Rolling Back Down, Plank with Leg lift, spine stretch with stick | The group was asked to listen and pay attention to a song and to complete the lyrics after it was paused. Participants were also asked to mention words present in the lyrics. |
| 11 & 12 | Double Leg Stretch, Hip Abduction, Knee Flexion and Extension with Ball, Spine Stretch with a stick | Participants were engaged in a collaborative storytelling. A participant initiated a new story, continued by others one by one |
| 13 & 14 | Double Leg Stretch with a ball (roll over), Leg Inclination with a ball, Plank, Plank with leg-lift, Lunge with a ball and stick, Spine Stretch with a stick, Bird Dog, Squats with a ball and shoulder flexion. | A participant started a sequence of grocery store shopping list saying: “I went to the grocery and bought an…” (e.g., apple). The closest participant was asked to repeat the previous statement and add a new item to the shopping list. The process was continuous and items cumulative until everyone in the group had contributed. |
| 15 & 16 | Bird Dogs, Plank with a ball, Hip Flexion with extended leg with a ball, Lunge with ball, rolling back, one leg circle, double leg circle | Verbal fluency task: the participants were instructed do evoke as many words as they could remember. The categories were fruits, animals, house objects, or personal names. |
| 17 & 18 | Shoulder bridge with leg lift, single leg stretch, spine stretch with a stick, Leg Pull Front, Hip Abduction, Knee Flexion and Extension with ball, Swan, and Swimming | Stroop Test—A word list was displayed. The participants had to read the names of the words instead of their colors. |
| 19 & 20 | Bird Dog with a ball, roll up, spine stretch with a stick, single leg stretches, Side Plank, Lunge with a Stick | During the exercise, newspaper news was read out loud by the researchers followed by questions to the participants regarding the information. |
| 21 & 22 | Plank with arms on a ball, knee extension sitting on a ball, lunge with a stick, bird dog, squat, and shoulder flexion | Based on researcher tips, participants were asked to guess personal names, song, or objects names. |
| 23 & 24 | Knee Flexion and Extension with a ball between the calves, leg inclination with a ball, lunges, squat with the back on the wall. | During the exercise, newspaper news was read out loud by the researchers followed by questions to the participants regarding the information. This activity was intercalated with a serial subtraction by multiples of 6, 7 and 8. |
| Index | Group | Pre- Intervention | Post-Intervention | CI 95% | ηρ² | Interaction (F) | Time (F) | Group (F) |
|---|---|---|---|---|---|---|---|---|
| Semantic Verbal Fluency (SVF) | PILATES-COG Control | 13.78 ± 3.51 13.80 ± 4.18 | 16.96 ± 4.14 ***# 14.28 ± 3.66 | 1.428–4.929 1.790–−0.830 | 0.268 0.015 | 6.256 * | 11.498 ** | 1.268 |
| Phonological Verbal Fluency (PVF) | PILATES-COG Control | 12.39 ± 3.81 9.75 ± 5.04 | 14.85 ± 5.69 * 11.41 ± 5.36 * | 0.429–4.500 0.112–3.221 | 0.143 0.116 | 0.399 | 10.702 ** | 3.672 |
| Immediate Memory (CERAD–Wordlist) | PILATES-COG Control | 18.32 ± 5.16 16.96 ± 3.61 | 20.95 ± 4.29 ***# 17.84 ± 4.23 | 1.294–3.979 −0.379–2.139 | 0.258 0.042 | 3.694 | 14.807 *** | 3.583 |
| Evocation Memory (CERAD–Wordlist) | PILATES-COG Control | 5.45 ± 2.40 5.21 ± 1.76 | 6.86 ± 1.91 *** 5.75 ± 2.23 | 0.726–2.092 −0.113–1.196 | 0.282 0.060 | 3.415 | 17.272 *** | 1.420 |
| Recognition Memory (CERAD–Wordlist) | PILATES-COG Control | 8.41 ± 1.50 8.42 ± 1.61 | 8.86 ± 1.16 8.58 ± 1.41 | −0.120–1.030 −0.384–0.717 | 0.055 0.008 | 0.531 | 2.474 | 0.132 |
| Lower-limb strength (CSTS 30) | PILATES-COG Control | 11.64 ± 1.90 + 8.74 ± 1.78 | 13.86 ± 2.14 ***### 9.61 ± 1.67* | 1.369–3.060 0.210–1.529 | 0.447 0.170 | 6.482 * | 34.093 *** | 39.675 *** |
| Dynamic balance (mini-BESTest) | PILATES-COG Control | 22.27 ± 2.96 20.86 ± 3.97 | 26.00 ± 1.57 ***### 21.71 ± 2.47 | 2.280–5.174 −0.624–2.388 | 0.398 0.032 | 7.839 ** | 19.999 *** | 16.134 *** |
| Functional mobility (TUG) | PILATES-COG Control | 8.16 ± 0.99 + 11.55 ± 1.79 | 8.15 ± 1.33 11.68 ± 1.62 | −0.677–0.654 −0.593–0.839 | <0.001 0.006 | 0.077 | 0.053 | 81.549 *** |
| Functional mobility with dual-task (TUG-DT) | PILATES-COG Control | 10.81 ± 2.13 + 14.80 ± 4.39 | 9.92 ± 2.30 13.65 ± 3.45 | −2.373–0.598 −2.798–0.504 | 0.039 0.052 | 0.056 | 3.452 | 20.424 *** |
| Dual Task Cost (%) | PILATES-COG Control | 31.84 ± 25.46 28.76 ± 23.64 | 18.87 ± 14.79 * 18.27 ± 20.44 | 0.568–25.372 −2.583–23.562 | 0.111 0.069 | 0.078 | 6.971 * | 0.118 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva, D.J.F.; Torres, J.L.; Ericeira, L.P.; Jardim, N.Y.V.; da Costa, V.O.; Carvalho, J.P.R.; Corrêa, P.G.R.; Bento-Torres, J.; Picanço-Diniz, C.W.; Bento-Torres, N.V.O. Pilates and Cognitive Stimulation in Dual Task an Intervention Protocol to Improve Functional Abilities and Minimize the Rate of Age-Related Cognitive Decline in Postmenopausal Women. Int. J. Environ. Res. Public Health 2022, 19, 13333. https://doi.org/10.3390/ijerph192013333
da Silva DJF, Torres JL, Ericeira LP, Jardim NYV, da Costa VO, Carvalho JPR, Corrêa PGR, Bento-Torres J, Picanço-Diniz CW, Bento-Torres NVO. Pilates and Cognitive Stimulation in Dual Task an Intervention Protocol to Improve Functional Abilities and Minimize the Rate of Age-Related Cognitive Decline in Postmenopausal Women. International Journal of Environmental Research and Public Health. 2022; 19(20):13333. https://doi.org/10.3390/ijerph192013333
Chicago/Turabian Styleda Silva, Daniel José Fontel, Juliana Lima Torres, Luiza Pimentel Ericeira, Naina Yuki Vieira Jardim, Victor Oliveira da Costa, Josilayne Patrícia Ramos Carvalho, Paola Geaninne Reis Corrêa, João Bento-Torres, Cristovam Wanderley Picanço-Diniz, and Natáli Valim Oliver Bento-Torres. 2022. "Pilates and Cognitive Stimulation in Dual Task an Intervention Protocol to Improve Functional Abilities and Minimize the Rate of Age-Related Cognitive Decline in Postmenopausal Women" International Journal of Environmental Research and Public Health 19, no. 20: 13333. https://doi.org/10.3390/ijerph192013333
APA Styleda Silva, D. J. F., Torres, J. L., Ericeira, L. P., Jardim, N. Y. V., da Costa, V. O., Carvalho, J. P. R., Corrêa, P. G. R., Bento-Torres, J., Picanço-Diniz, C. W., & Bento-Torres, N. V. O. (2022). Pilates and Cognitive Stimulation in Dual Task an Intervention Protocol to Improve Functional Abilities and Minimize the Rate of Age-Related Cognitive Decline in Postmenopausal Women. International Journal of Environmental Research and Public Health, 19(20), 13333. https://doi.org/10.3390/ijerph192013333






