The Effects of Monetary Incentives on Physicians’ Effort and Patient Satisfaction: Understanding the Links between Monetary Incentives and Physicians’ Effort
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
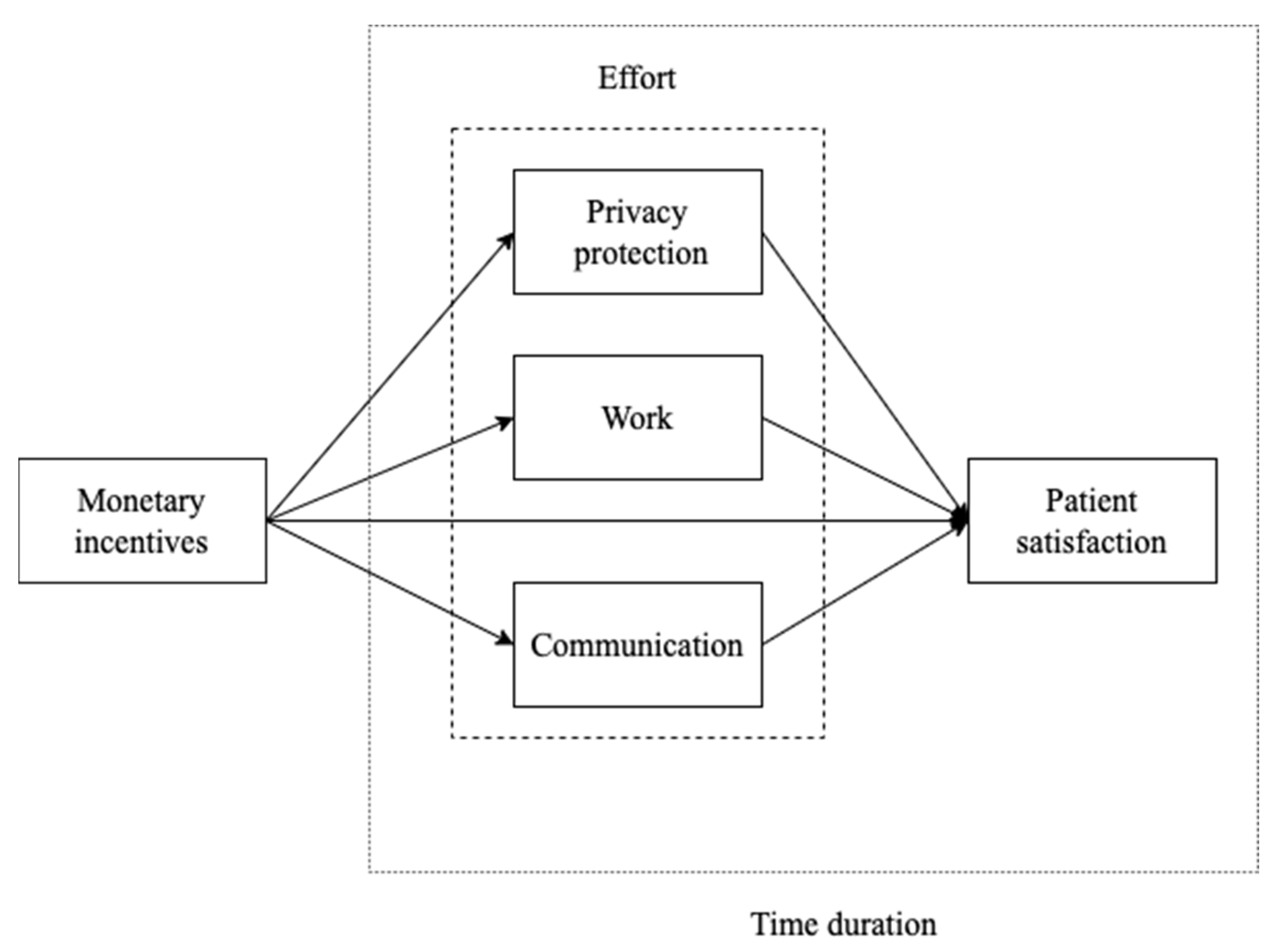
2.2. Identification Model
2.2.1. Variables and Model
2.2.2. Group Setting
3. Results
3.1. Summary Statistics
3.2. Empirical Results
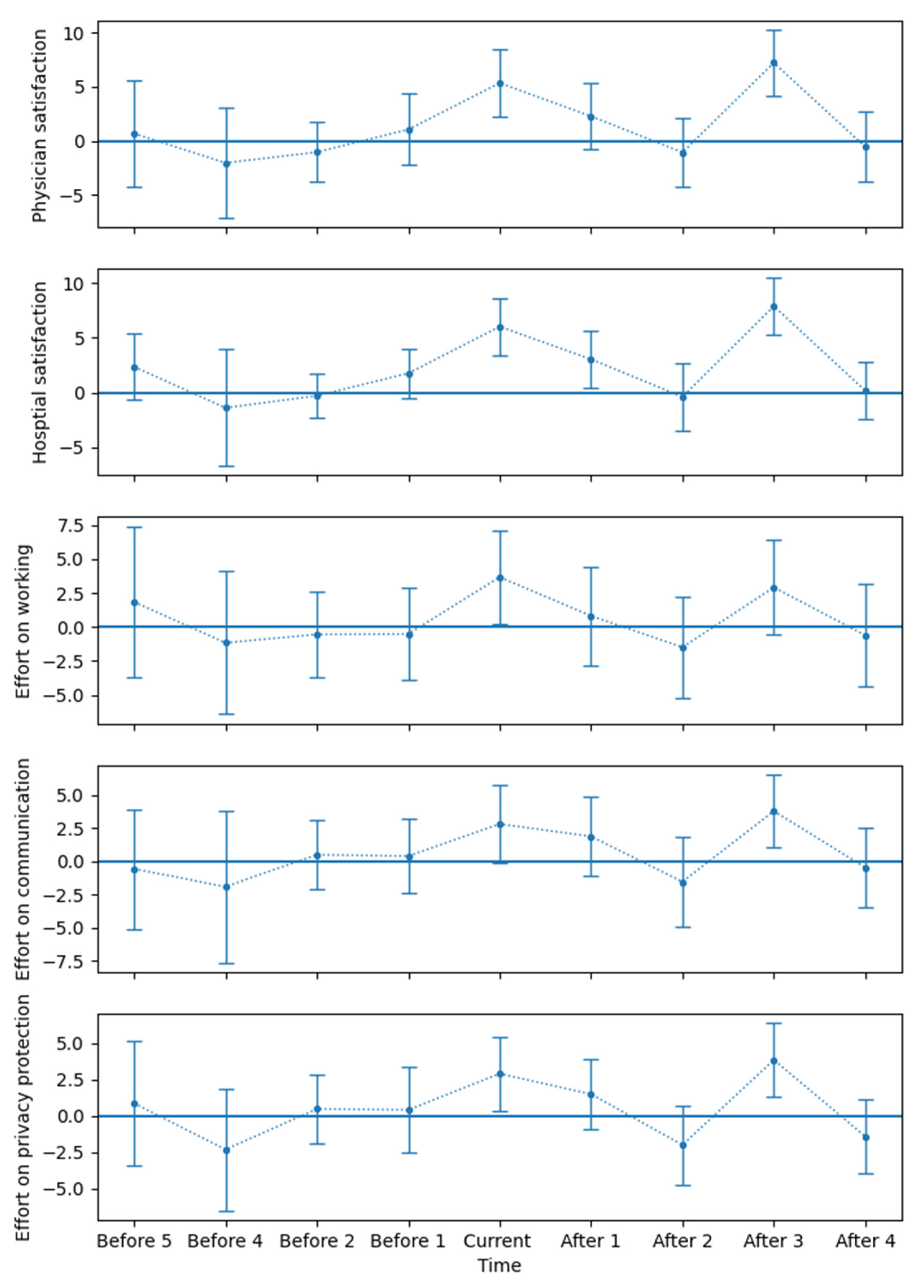
3.3. Event-Study Approach
4. Discussion
5. Conclusions
6. Limitation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Bogner, H.R.; McClintock, H.F.V.; Kurichi, J.E.; Kwong, P.L.; Xie, D.; Hennessy, S.; Streim, J.E.; Stineman, M.G. Patient Satisfaction and Prognosis for Functional Improvement and Deterioration, Institutionalization, and Death among Medicare Beneficiaries Over Two Years. Arch. Phys. Med. Rehabil. 2017, 98, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Rodeghier, M.; Lis, C.G. Patient Satisfaction with Service Quality in an Oncology Setting: Implications for Prognosis in Non-Small Cell Lung Cancer. Int. J. Qual. Health Care 2013, 25, 696–703. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bradley, M.; Chahar, P. Burnout of Healthcare Providers during COVID-19. Cleve. Clin. J. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Argentero, P.; Dell’Olivo, B.; Ferretti, M.S. Staff Burnout and Patient Satisfaction With the Quality of Dialysis Care. Am. J. Kidney Dis. 2008, 51, 80–92. [Google Scholar] [CrossRef] [PubMed]
- Baer, T.E.; Feraco, A.M.; Sagalowsky, S.T.; Williams, D.; Litman, H.J.; Vinci, R.J. Pediatric Resident Burnout and Attitudes Toward Patients. Pediatrics 2017, 139, e20162163. [Google Scholar] [CrossRef] [PubMed]
- Hall, L.H.; Johnson, J.; Watt, I.; Tsipa, A.; O’Connor, D.B. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS ONE 2016, 11, e0159015. [Google Scholar] [CrossRef]
- Boissy, A. Getting to Patient-Centered Care in a Post–COVID-19 Digital World: A Proposal for Novel Surveys, Methodology, and Patient Experience Maturity Assessment. NEJM Catal. Innov. Care Deliv. 2020, 1, 4. [Google Scholar]
- Itri, J.N.; Bruno, M.A.; Lalwani, N.; Munden, R.F.; Tappouni, R. The Incentive Dilemma: Intrinsic Motivation and Workplace Performance. J. Am. Coll. Radiol. 2019, 16, 39–44. [Google Scholar] [CrossRef]
- Sittenthaler, H.M.; Mohnen, A. Cash, Non-Cash, or Mix? Gender Matters! The Impact of Monetary, Non-Monetary, and Mixed Incentives on Performance. J. Bus. Econ. 2020, 90, 1253–1284. [Google Scholar] [CrossRef]
- Kanfer, R.; Frese, M.; Johnson, R.E. Motivation Related to Work: A Century of Progress. J. Appl. Psychol. 2017, 102, 338–355. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, S.A. Justifiability and the Motivational Power of Tangible Noncash Incentives. Hum. Perform. 2009, 22, 143–155. [Google Scholar] [CrossRef]
- Zahoor, S.; Yang, S.; Ren, X.; Haider, S.A. Corporate Governance and Humble Leadership as Antecedents of Corporate Financial Performance: Monetary Incentive as a Moderator. Front. Psychol. 2022, 13, 904076. [Google Scholar] [CrossRef] [PubMed]
- Braganza, O. Proxyeconomics, a Theory and Model of Proxy-Based Competition and Cultural Evolution. R. Soc. Open Sci. 2022, 9, 211030. [Google Scholar] [CrossRef] [PubMed]
- Mitra, A.; Shahriar, Q. Why Is Dishonesty Difficult to Mitigate? The Interaction between Descriptive Norm and Monetary Incentive. J. Econ. Psychol. 2020, 80, 102292. [Google Scholar] [CrossRef]
- Jensen, M.C.; Murphy, K.J.; Wruck, E.G. Remuneration: Where We’ve Been, How We Got to Here, What Are the Problems, and How to Fix Them. 2004. Available online: https://doi.org/10.2139/ssrn.561305 (accessed on 15 August 2022).
- Davis, A.M.; Hyndman, K. An Experimental Investigation of Managing Quality Through Monetary and Relational Incentives. Manag. Sci. 2018, 64, 2345–2365. [Google Scholar] [CrossRef]
- Bonner, S.E.; Sprinkle, G.B. The Effects of Monetary Incentives on Effort and Task Performance: Theories, Evidence, and a Framework for Research. Account. Organ. Soc. 2002, 27, 303–345. [Google Scholar] [CrossRef]
- Dunsch, F.; Evans, D.K.; Macis, M.; Wang, Q. Bias in Patient Satisfaction Surveys: A Threat to Measuring Healthcare Quality. BMJ Glob. Health 2018, 3, e000694. [Google Scholar] [CrossRef]
- Ng, J.H.Y.; Luk, B.H.K. Patient Satisfaction: Concept Analysis in the Healthcare Context. Patient Educ. Couns. 2019, 102, 790–796. [Google Scholar] [CrossRef]
- O’Malley, A.J.; Zaslavsky, A.M.; Elliott, M.N.; Zaborski, L.; Cleary, P.D. Case-Mix Adjustment of the CAHPS® Hospital Survey. Health Serv. Res. 2005, 40, 2162–2181. [Google Scholar] [CrossRef]
- Sobel, M.E. Direct and Indirect Effects in Linear Structural Equation Models. Sociol. Methods Res. 1987, 16, 155–176. [Google Scholar] [CrossRef]
- Jiang, X.; He, P.; Zhu, D.; Shi, X.; Meng, Q. Different Impacts of the Zero-Markup Drug Policy on County General and Traditional Chinese Medicine Hospitals: Evidence from Shandong Province, China. Int. J. Equity Health 2020, 19, 219. [Google Scholar] [CrossRef] [PubMed]
- Marcus, M.; Sant’Anna, P.H.C. The Role of Parallel Trends in Event Study Settings: An Application to Environmental Economics. J. Assoc. Environ. Resour. Econ. 2021, 8, 235–275. [Google Scholar] [CrossRef]
- Durant, R.F.; Kramer, R.; Perry, J.L.; Mesch, D.; Paarlberg, L. Motivating Employees in a New Governance Era: The Performance Paradigm Revisited. Public Adm. Rev. 2006, 66, 505–514. [Google Scholar] [CrossRef]
- Weibel, A.; Rost, K.; Osterloh, M. Pay for Performance in the Public Sector—Benefits and (Hidden) Costs. J. Public Adm. Res. Theory 2010, 20, 387–412. [Google Scholar] [CrossRef]
- Pandya, S.; Hamal, M.; Abuya, T.; Kintu, R.; Mwanga, D.; Warren, C.E.; Agarwal, S. Understanding Factors That Support Community Health Worker Motivation, Job Satisfaction, and Performance in Three Ugandan Districts: Opportunities for Strengthening Uganda’s Community Health Worker Program. Int. J. Health Policy Manag. 2022. [Google Scholar] [CrossRef] [PubMed]
- Roth, J. Pretest with Caution: Event-Study Estimates after Testing for Parallel Trends. Am. Econ. Rev. 2022, 4, 305–322. [Google Scholar] [CrossRef]
- Campello, M.; Larrain, M. Enlarging the Contracting Space: Collateral Menus, Access to Credit, and Economic Activity. Rev. Financ. Stud. 2016, 29, 349–383. [Google Scholar] [CrossRef]
- Vig, V. Access to Collateral and Corporate Debt Structure: Evidence from a Natural Experiment. J. Financ. 2013, 68, 881–928. [Google Scholar] [CrossRef]
| Department | Ratio | Ranking | Groups |
|---|---|---|---|
| Dermatology | 1.957 | 1 | Control |
| Dentistry | 1.921 | 2 | Control |
| Pediatrics | 1.597 | 3 | - |
| Ear, nose and throat | 1.450 | 4 | - |
| Pain medicine | 1.420 | 5 | - |
| Internal medicine | 1.292 | 6 | Treat |
| Obstetrics/gynecology | 1.239 | 7 | Treat |
| N | Mean | SD | Min | 25% | Median | 75% | Max | |
|---|---|---|---|---|---|---|---|---|
| Age | 994 | 44.36 | 19.28 | 3 | 29 | 38 | 60 | 95 |
| Gender (female = 0) | 994 | 0.34 | 0.48 | 0 | 0 | 0 | 1 | 1 |
| Non-resident (yes = 1) | 994 | 0.46 | 0.49 | 0 | 0 | 0 | 1 | 1 |
| Education | 994 | 0.98 | 1.12 | 0 | 0 | 1 | 2 | 4 |
| Hospital satisfaction | 994 | 95.14 | 7.27 | 50 | 90 | 100 | 100 | 100 |
| Physician satisfaction | 994 | 95.61 | 6.94 | 50 | 90 | 100 | 100 | 100 |
| Communication | 994 | 96.748 | 6.52 | 50 | 95 | 100 | 100 | 100 |
| Privacy protection | 994 | 97.38 | 5.56 | 60 | 98 | 100 | 100 | 100 |
| Working effort | 994 | 96.51 | 6.86 | 50 | 95 | 100 | 100 | 100 |
| Treat | 994 | 0.84 | 0.36 | 0 | 1 | 1 | 1 | 1 |
| Post | 994 | 0.38 | 0.49 | 0 | 0 | 0 | 1 | 1 |
| DiD | 994 | 0.34 | 0.47 | 0 | 0 | 0 | 1 | 1 |
| Physician Satisfaction | Communication | Working | Privacy Protection | Physician Satisfaction | |
|---|---|---|---|---|---|
| DiD | 2.7905 | 1.6614 | 1.0416 | 1.0997 | 1.6309 |
| (0.0000) | (0.0000) | (0.0349) | (0.0004) | (0.0000) | |
| Age | 0.0117 | 0.0093 | −0.0088 | 0.0064 | 0.0107 |
| (0.1106) | (0.1908) | (0.2453) | (0.3717) | (0.0334) | |
| Education | −0.5040 | −0.5086 | −0.4851 | −0.2676 | −0.1090 |
| (0.0000) | (0.0012) | (0.0000) | (0.0080) | (0.0543) | |
| Non-resident | −0.2307 | −0.1234 | −0.7805 | −0.4937 | 0.2581 |
| (0.4387) | (0.7798) | (0.0017) | (0.1712) | (0.1633) | |
| Gender | 0.7935 | 0.8245 | 0.7405 | 1.1465 | −0.0661 |
| (0.0070) | (0.0876) | (0.1830) | (0.0040) | (0.7787) | |
| Communication | 0.2410 | ||||
| (0.0015) | |||||
| Working | 0.3782 | ||||
| (0.0000) | |||||
| Privacy protection | 0.3322 | ||||
| (0.0000) | |||||
| Intercept | 94.484 | 96.051 | 97.136 | 96.823 | 2.4368 |
| (0.0000) | (0.0000) | (0.0000) | (0.0000) | (0.4446) | |
| Fixed effect | Control | Control | Control | Control | Control |
| Time effect | Control | Control | Control | Control | Control |
| R-squared | 0.130 | 0.119 | 0.085 | 0.126 | 0.595 |
| No. of observations | 994 | 994 | 994 | 994 | 994 |
| Hospital Satisfaction | Communication | Working | Privacy Protection | Hospital Satisfaction | |
|---|---|---|---|---|---|
| DiD | 2.7920 | 1.6614 | 1.0416 | 1.0997 | 1.5594 |
| (0.0000) | (0.0000) | (0.0349) | (0.0004) | (0.0000) | |
| Age | 0.0144 | 0.0093 | −0.0088 | 0.0064 | 0.0129 |
| (0.1098) | (0.1908) | (0.2453) | (0.3717) | (0.1051) | |
| Education | −0.4955 | −0.5086 | −0.4851 | −0.2676 | −0.0759 |
| (0.0004) | (0.0012) | (0.0000) | (0.0080) | (0.3054) | |
| Non-resident | −0.2311 | −0.1234 | −0.7805 | −0.4937 | 0.2341 |
| (0.4274) | (0.7798) | (0.0017) | (0.1712) | (0.1652) | |
| Gender | 1.0108 | 0.8245 | 0.7405 | 1.1465 | 0.1500 |
| (0.0282) | (0.0876) | (0.1830) | (0.0040) | (0.5220) | |
| Communication | 0.3271 | ||||
| (0.0000) | |||||
| Working | 0.3689 | ||||
| (0.0000) | |||||
| Privacy protection | 0.2774 | ||||
| (0.0000) | |||||
| Intercept | 93.805 | 96.051 | 97.136 | 96.823 | −0.3016 |
| (0.0000) | (0.0000) | (0.0000) | (0.0000) | (0.9182) | |
| Fixed effect | Control | Control | Control | Control | Control |
| Time effect | Control | Control | Control | Control | Control |
| R-squared | 0.135 | 0.119 | 0.085 | 0.126 | 0.582 |
| No. of observations | 994 | 994 | 994 | 994 | 994 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, C.; Li, X.; Liang, H.; Zhang, Z.; Fang, D. The Effects of Monetary Incentives on Physicians’ Effort and Patient Satisfaction: Understanding the Links between Monetary Incentives and Physicians’ Effort. Int. J. Environ. Res. Public Health 2022, 19, 13075. https://doi.org/10.3390/ijerph192013075
Yu C, Li X, Liang H, Zhang Z, Fang D. The Effects of Monetary Incentives on Physicians’ Effort and Patient Satisfaction: Understanding the Links between Monetary Incentives and Physicians’ Effort. International Journal of Environmental Research and Public Health. 2022; 19(20):13075. https://doi.org/10.3390/ijerph192013075
Chicago/Turabian StyleYu, Chenhao, Xiaoyan Li, Huigang Liang, Zhiruo Zhang, and Dong Fang. 2022. "The Effects of Monetary Incentives on Physicians’ Effort and Patient Satisfaction: Understanding the Links between Monetary Incentives and Physicians’ Effort" International Journal of Environmental Research and Public Health 19, no. 20: 13075. https://doi.org/10.3390/ijerph192013075
APA StyleYu, C., Li, X., Liang, H., Zhang, Z., & Fang, D. (2022). The Effects of Monetary Incentives on Physicians’ Effort and Patient Satisfaction: Understanding the Links between Monetary Incentives and Physicians’ Effort. International Journal of Environmental Research and Public Health, 19(20), 13075. https://doi.org/10.3390/ijerph192013075







