Abstract
The best nutritional strategy to fight the rise in obesity remains a debated issue. The Mediterranean diet (MD) and the Very Low-Calorie Ketogenic diet (VLCKD) are effective at helping people lose body weight (BW) and fat mass (FM) while preserving fat-free mass (FFM). This study aimed to evaluate the time these two diets took to reach a loss of 5% of the initial BW and how body composition was affected. We randomized 268 subjects with obesity or overweight in two arms, MD and VLCKD, for a maximum of 3 months or until they reached 5% BW loss. This result was achieved after one month of VLCKD and 3 months of MD. Both diets were effective in terms of BW (p < 0.0001) and FM loss (p < 0.0001), but the MD reached a higher reduction in both waist circumference (p = 0.0010) and FM (p = 0.0006) and a greater increase in total body water (p = 0.0017) and FFM (p = 0.0373) than VLCKD. The population was also stratified according to gender, age, and BMI. These two nutritional protocols are both effective in improving anthropometrical parameters and body composition, but they take different time spans to reach the goal. Therefore, professionals should evaluate which is the most suitable according to each patient’s health status.
1. Introduction
Obesity is a multifactorial disease that deteriorates the quality of life, and it is now considered a growing pandemic that imposes a heavy burden on families and society [1]. It is a chronic condition defined as an abnormal or excessive fat accumulation that may impair health [2]. It is a risk factor for multiple comorbidities (i.e., type 2 diabetes (T2DM), hypertension, cardiovascular diseases (CVD), cancer, and sleep apnea), and it is associated with increased mortality risk [3]. Currently more than 1.9 billion adults are overweight, of which 650 million suffer from obesity [2]. In Italy, 4 out of 10 adults are overweight, and 1 out of them is affected by obesity [4]. Overweight and obesity are classified based on the Body Mass Index (BMI). A BMI range between 25.0 and 29.9 defines overweight, while a BMI > 30 determines obesity [5]. Achieving a healthy weight is considered a risk modifier and has favorable effects on blood pressure, glucose metabolism, and cardiac and vascular functions [1]. In the literature, it has been demonstrated that even 5% of body weight loss may improve health outcomes, and this value has been set as a goal standard in weight loss interventions [6,7]. Many patients with obesity [8,9] and type 2 diabetes [10] are not aware that losing at least 5% of their body weight could improve their quality of life. Indeed, losing at least 5% of body weight creates a significant reduction in fat mass (8 ± 3%) and not only an improvement in multi-organ insulin sensitivity and beta cell function but also in blood pressure and heart rate, as was seen in a recent RCT on 40 subjects with obesity [7]. This modest reduction has also shown beneficial effects on CVD risk factors at 1 year in patients with obesity and type 2 diabetes. In fact, the loss of 5% body weight created a significant reduction in diastolic and systolic blood pressure and glycemic and lipid metabolism (except for LDL cholesterol, which did not change significantly) [10]. Moreover, these studies showed that losing more than 5% provided further health benefits [7,10].
Sometimes the time necessary to reach the goal of losing 5% of body weight is a key factor, since people with overweight or with obesity may lose their motivation and abandon the nutritional protocol, starting the so-called yo-yo effect [11]. It is important to establish a feasible objective reachable through lifestyle changes and healthy eating habits [9]. Generally, these two behavioral changes require time to be adopted, and when choosing the most suitable dietary pattern, it is important to consider not only the general health benefits but also the individual [6,9].
The Mediterranean Diet (MD) and Very Low-Calorie Ketogenic Diet (VLCKD) are often recommended by health professionals for their beneficial effects on weight loss (especially fat mass, FM) and the preservation of fat-free mass (FFM) [12,13,14,15,16].
In 2010, the Mediterranean Diet (MD) became an intangible heritage of humanity by UNESCO [17]. This nutritional approach is considered sustainable and provides a high consumption of local fruit and vegetables, whole grains, legumes, nuts and seeds, blue fish, eggs, white meats, and dairy products, and a low consumption of red and processed meats with respect to correct portion sizes and weekly frequencies [18,19]. MD also supports correct hydration, extra virgin olive oil as a seasoning, home-made food preparation, sociable eating with family or friends, regular physical activity, relaxation, and rest [20,21]. The MD suggests consuming more low-energy-density foods [22], and compared with many other dietary patterns (i.e., the Western diet), it provides a low glycemic load because it is rich in foods high in dietary fibers, which give great satiety after a meal [23]. A hypocaloric MD showed greater weight loss than the low-fat diet at 12 and 24 months but similar weight loss compared to other diets (i.e., low-carbohydrate diets and calorie-restricted diets) [24]. Epidemiological studies have noticed increased longevity and reduced morbidity in Mediterranean countries, which follow the MD, compared to the USA or Northern Europe populations [25,26]. The MD not only helps with weight loss maintenance but also has beneficial effects on cardiovascular risk factors, cognitive functions, and mood [27,28].
On the other hand, a ketogenic diet is characterized by no more than 30–50 g/day of carbohydrates [29,30]. This carbohydrates deprivation depletes glycogen stores; thus, the body undergoes metabolic changes to provide an energy source for the body and the brain through gluconeogenesis and ketogenesis. Through this last process, ketone bodies (KB) (acetoacetate, beta-hydroxybutyrate, and acetone) are produced, and they are used as the primary energy source by cells with mitochondria and by all organs, particularly the brain [16]. This ketosis state, called “physiological ketosis”, should not be confused with diabetic ketoacidosis [31] because in the first case, ketonemia reaches maximum levels of 7–8 mmol/L with no changes in pH (7.4), whilst in the second case, ketonemia can exceed 20 mmol/L with a concomitant lowering of blood pH (<7.3) [32]. At present, there are different types of ketogenic diets, with or without calorie restriction: Isocaloric Ketogenic Diet (IKD), Low-Calorie Ketogenic Diet (LCKD), and the Very-Low-Calorie Ketogenic Diet (VLCKD) [12]. The VLCKD provides less than 700–800 kcal/day with carbohydrates ranging between 30 and 50 g per day, preferably <30 g, and <30–40 g/day of fats, mainly from extra virgin olive oil [12,13,32]. It is a normal protein diet; in fact, it should provide high values of biological proteins in the amount of 0.8–1.5 g/kg ideal body weight/day to preserve free fat mass [12,32,33]. The VLCKD must be supplemented with bicarbonate, micronutrients, and omega-3 fatty acids, and it should only be followed for short periods (8–16 weeks) [12,32]. A period of VLCKD may help control hunger and improve fat-oxidative metabolism, and therefore reduce body weight, but the transition from a VLCKD to a standard diet should be gradual and well-controlled [16]. In the literature, it has been seen that a VLCKD creates a significant reduction in body weight, BMI, waist circumference, and fat mass (especially visceral fat) while preserving lean mass [34,35,36,37]. These body composition changes seem to be associated with better food control and quality of life, which could contribute to maintaining weight loss over time [36]. Results obtained after a VLCKD seem to be better than results obtained with other nutritional protocols (very low-calorie diets, low-calorie diets, low-fat diets) in the same time span [36]. The Italian Society of Endocrinology recommends the VLCKD as an effective dietary treatment for people with obesity, hypertriglyceridemia, obesity associated with T2DM [14], hypertension [13,32], particularly for severe obesity and/or comorbidities (joint diseases, preoperative period of bariatric surgery, and cardiovascular and metabolic diseases) who need a rapid and substantial weight loss. The VLCKD can be prescribed to a specific population of patients after considering the potential contraindications and keeping the patients under medical surveillance. The VLCKD is contraindicated for people affected by type 1 diabetes mellitus (T1DM), recent cardiovascular or cerebrovascular events, severe hepatic and renal insufficiency, gout episodes, kidney stones, hydroelectrolytic alterations, psychiatric disease, and pregnant and breastfeeding women [15,32].
The present study aimed to observe how long a MD and a VLCKD took to create a loss of at least 5% of the initial body weight in subjects with overweight and obesity and how these two nutritional protocols affect anthropometrical measures and body composition parameters.
2. Materials and Methods
2.1. Study Population
Three hundred and seventy-four (374) males and females subjects with overweight or obesity were consecutively enrolled in the Endocrinology and Metabolic Diseases unit of the University Hospital Campus Bio-Medico of Rome from December 2021 to May 2022 according to the inclusion and exclusion criteria. Inclusion criteria were adults aged 18–70 years and BMI ≥ 25 kg/m2. Exclusion criteria comprised subjects with Type 1 Diabetes Mellitus (T1DM), T2DM, pregnancy and breastfeeding, kidney failure and severe chronic kidney disease, liver failure, hearth failure (NYHA III–IV), respiratory insufficiency, unstable angina, a recent stroke or myocardial infarction (<12 months), cardiac arrhythmias, eating disorders and other severe mental illnesses, alcohol and substance abuse, active/severe infections, and frail older adults. Consecutive enrolment was repeated in the two groups, either a Mediterranean diet (MD) or a Very Low-Calorie Ketogenic Diet (VLCKD), achieving casualty in allocation, and thus randomization from December 2021 to May 2022. The MD group comprised 191 subjects (54 males, 137 females), while the VLCKD group comprised 183 subjects (46 males, 137 females). The two groups were homogeneous for age, height, and weight.
To evaluate the effects of these two different nutritional protocols, the population was stratified according to gender (male and female), age (≤50 years old or ≥50 years old), and BMI (in subjects with overweight BMI comprised between 25–29.9 kg/m2; in subjects with obesity, BMI > 30 kg/m2).
2.2. Study Protocol
At baseline (T0), the subjects underwent an endocrinological visit to evaluate if they could be included in the study according to the exclusion and inclusion criteria. When enrolled, they were consecutively allocated to either the MD or VLCKD. Participants received nutritional counseling and were given the dietetic protocol to be followed for three months. Follow-up visits were set up once monthly until 5% body weight loss was achieved.
Every fortnight, a phone call was conducted by nutritionists to check the dietary adherence and patients’ motivation through a 24 h dietary recall (Figure 1). When patients reached the goal of losing at least 5% of their initial body weight, they were invited to stop following the nutritional protocol and to start a maintenance diet (for the MD group) or a reintroduction diet (for the VLCKD group).
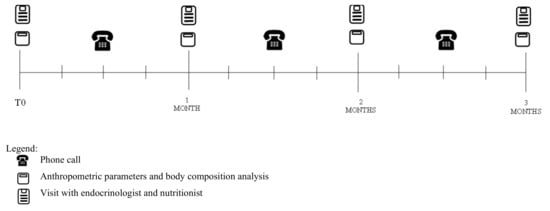
Figure 1.
Study protocol.
2.3. Anthropometric Parameters
At T0, body weight (BW) and height were recorded using a Seca 200 scale with a stadiometer. Measurements were taken in the morning after an overnight fast of at least 12 h. Subjects wore underwear and were without shoes. Height was measured only at T0, while body weight was recorded every month until participants lost at least 5% of their initial body weight for a maximum of three months for both diets.
BMI was calculated as weight (kg)/height (m2) [5] and waist circumference (WC) was measured in the medium point between the last rib and the iliac crest [38].
2.4. Body Composition Analysis
Body composition was assessed using bioelectrical impedance analysis (BIA, Akern 101 New Edition). BIA measurements were performed at T0 and once a month until the 5% weight loss for a maximum of three months. Measurements were conducted in the morning after an overnight fast of at least 12 h, in abstinence of alcohol consumption for 48 h and without strenuous physical activity for 24 h before the testing day. The parameters obtained by this exam were: phase angle, total body water (TBW), extracellular water (ECW), intracellular water (ICW), fat-free mass (FFM), fat mass (FM), and body cellular mass (BCM) [39].
2.5. Nutritional Protocols
2.5.1. Mediterranean Diet
The hypocaloric Mediterranean dietary plan was individualized according to participants’ nutritional needs and preferences. Each participant’s total energy expenditure (TEE) was calculated, and then a caloric restriction of 500 kcal was applied. On average, the diet provided 1500 kcal for women and 1700 kcal for men. The macronutrient composition of the diet was 15% protein, 30–35% lipids, and 50–55% carbohydrates, with less than 15% comprising simple sugars. The diet included five meals daily (breakfast, lunch, dinner, and two snacks) both for men and women. Participants were asked to prefer vegetables, wholegrain cereals, fish and legumes, lean white meat, and seeds, and to reduce red meat, eggs, and dairy products to only once a week. They were invited to consume fruit or low-fat yogurt as snacks and extra virgin olive oil as a seasoning in the amount of 30 mL (for women)–40 mL (for men) daily. Women were recommended to drink at least 2 L of water, while men were instructed to drink at least 2.5 L daily [40].
2.5.2. Very Low-Calorie Ketogenic Diet
The VLCKD provided <800 kcal and <30–50 g of carbohydrate/day. The amount of protein was calculated as 1.2–1.5 g of protein/kg ideal body weight/day, respectively, for women and men. The diet was composed of 4 daily meals for women and 5 daily meals for men, consisting of both meal replacements and natural foods. The diet was structured as follows: meal replacements for breakfast and snacks and white or red meat, fish, eggs, smoked salmon, ham, or canned fish with a vegetable side dish for lunch and dinner. Subjects were allowed to use extra virgin olive oil as a seasoning in the amount of 30 g/day, both for men and women. A standard sugar-free multivitamin, bicarbonate, minerals (potassium 2000 mg and magnesium 375 mg), and omega 3 fatty acids (1 g), were prescribed. Drinking at least 2–2.5 L of water was recommended for women and for men, respectively [40].
2.6. Statistical Analysis
Statistical analysis was performed with the statistical program GraphPad Prism version 9.4.0. A Pearson test was conducted to evaluate the normality distribution. Paired and unpaired student t-tests were performed for intragroup and intergroup comparisons, respectively. The significance level was assessed for p-value <0.05.
The sample size of 128 subjects (64 for each group) was calculated with an 80% power to detect changes at the 0.05 significance level, taking possible dropouts into account.
3. Results
3.1. Study Population
Out of 374 subjects, only 268 completed the study. The 106 dropouts missed either the 1 month visit or the 2-month visit without losing at least 5% of their initial body weight after the first month.
The group which followed the MD until the end of the study was composed of 133 subjects (37 males and 96 females; mean age 45.08 ± 14.19 years), while the group that followed the VLCKD comprised 135 subjects (34 males and 101 females; mean age 45.5 ± 11.63 years) (Figure 2).
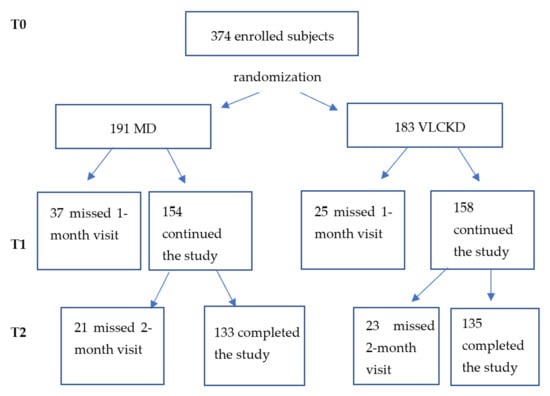
Figure 2.
Flow—chart of the enrollment phase.
3.2. Results on Anthropometric Parameters and Body Composition
VLCKD subjects lost at least 5% of their initial body weight after one month of the dietary regime, while the MD group reached this goal after 3 months. In the VLCKD group the percentage of body weight lost was 7.21 ± 1.57% after one month, while in the MD group the percentage was 7.68 ± 2.52% after three months. Both groups lost at least 5% of their initial body weight, but in two different time spans. There were no significant differences in body weight loss between the two groups.
The results of both diets on anthropometric and body composition parameters are reported in Table 1. Comparing the results obtained from MD and VLCKD, we observed a higher reduction in waist circumference (−6.86 ± 3.3 cm vs. −5.74 ± 2.07 cm; p = 0.0010) and fat mass percentage (−3.15 ± 2.49 vs. −2.17 ± 2.14; p = 0.0006) in the MD group compared to the VLCKD group. Moreover, the Mediterranean diet provided a greater increase of total body water percentage (2.27 ± 1.96% vs. 1.58 ± 1.61; p = 0.0017) and fat-free mass percentage (2.89 ± 3.08 vs. 2.23 ± 1.99; p = 0.0373) than the Very Low-Calorie Ketogenic diet.

Table 1.
Anthropometric and Body composition changes in MD and VLCKD groups (mean ± SD).
We stratified MD and VLCKD groups according to gender (male or female) to observe the effects of these two nutritional protocols on anthropometric and body composition parameters. There were 37 males (mean age: 45.22 ± 16.81 years) and 96 females (mean age: 45.03 ± 13.14 years) in the MD group, while in the VLCKD group, there were 34 males (mean age: 44.56 ± 13.25 years) and 101 females (mean age: 45.81 ± 11.09 years).
The results of both diets on anthropometrical and body composition parameters in males and females are reported in Table 1.
Comparing all parameters between MD and VLCKD in the male group, we did not observe any significant differences. In relation to females, we observed that the MD provided better results than the VLCKD in the reduction in waist circumference (−6.8 ± 3.5 cm vs. −5.54 ± 1.97 cm; p = 0.0020) and fat mass percentage (−3.27 ± 2.69% vs. −2.24 ± 2.21%; p = 0.0034). Moreover, a higher increase in total body water percentage (2.42 ± 2.09 vs. 1.72 ± 1.49; p = 0.0076) and fat-free mass percentage (3.06 ± 2.73% vs. 2.31 ± 1.92%; p = 0.0251) was observed in the MD group compared to the VLCKD group.
3.3. Subgroups Evaluation: Age and BMI
3.3.1. Age
We also evaluated the two diets according to age (≤50 years old or ≥50 years old) to observe if, in older adults, there could be a greater reduction in fat-free mass and body cellular mass, increasing the risk of sarcopenia.
In the MD group there were 78 subjects (23 males and 55 females) ≤ 50 years old (mean age 35.5 ± 9.50 years) and 55 subjects (14 males and 41 females) ≥ 50 years old (mean age 58.6 ± 6.80 years), while in the VLCKD group, there were 78 subjects (20 males and 58 females) ≤ 50 years old (mean age 38.17 ± 9.67 years) and 57 (14 males and 43 females) ≥ 50 years old (mean age 55.52 ± 4.26 years).
Observing the effects of the two nutritional protocols in people under 50, the MD was more efficient than the VLCKD in the reduction in waist circumference (6.96 ± 3.26 cm vs. 5.75 ± 2.2 cm, respectively; p = 0.0076), total body water percentage (2.39 ± 2.06% vs. 1.54 ± 1.52%, respectively; p = 0.0040), fat-free mass percentage (3.12 ± 2.76% vs. 2.31 ± 1.79%, respectively; p = 0.0326), and increase in fat mass percentage (3.33 ± 2.64% vs. 2.15 ± 1.97%, respectively; p = 0.0019). No significant differences were seen comparing the results between the two over 50 groups. We did not observe any changes in the body cellular mass percentage in both groups under and over 50 years old, so we can assume that these two diets preserve the body cellular mass at every age.
The results of both diets on anthropometrical and body composition parameters in subjects under and over 50 years old are reported in Table 2.

Table 2.
Anthropometric and Body composition changes in MD and VLCKD groups according to age (mean ± SD).
3.3.2. BMI
Finally, we divided the population according to BMI: subjects with overweight (BMI comprised between 25.0–29.9 kg/m2) and with obesity (BMI > 30 kg/m2).
In the MD group, we had 46 subjects with overweight (37 females and 9 males; mean BMI: 27.55 ± 1.56 kg/m2) and 87 with obesity (59 females and 28 males; mean BMI: 34.57 ± 3.89 kg/m2), while in the VLCKD group we had 38 subjects with overweight (33 females and 5 males, mean age: 43.11 ± 13.41; mean BMI: 27.67 ± 1.37 kg/m2) and 97 with obesity (68 females and 29 males; mean BMI: 35.84 ± 4.72 kg/m2).
Comparing the two nutritional protocols in subjects with overweight, we observed that the MD was more efficient than the VLCKD in the reduction in waist circumference (6.64 ± 2.68 cm vs. 5.00 ± 1.81 cm, respectively; p = 0.0020) and fat mass percentage (3.84 ± 2.59% vs. 2.58 ± 1.72%, respectively; p = 0.0126). The MD also caused a higher increase in total body water percentage (2.79 ± 2.02 with MD and 1.99 ± 1.19 with VLCKD; p = 0.0340). There were no significant differences in fat-free mass percentage between the two nutritional protocols.
Among subjects with obesity, we observed that the MD determined a higher reduction than the VLCKD in terms of waist circumference (6.98 ± 3.59 cm vs. 6.03 ± 2.11 cm, respectively; p = 0.0289) and of fat mass percentage (2.79 ± 2.38% vs. 2.01 ± 2.27%, respectively; p = 0.0237). No significant differences were observed for the fat-free mass percentage between the two diets. Regarding water balance, the Mediterranean diet caused a higher increase compared to the Very Low-Calorie Ketogenic diet’s total body water percentage (2.00 ± 1.88% vs. of 1.42 ± 1.73%, respectively; p = 0.0301). The extracellular water percentage decreased significantly in the VLCKD group compared to the MD group (p = 0.0409).
The results of both diets on anthropometrical and body composition parameters in subjects with overweight or with obesity are reported in Table 3.

Table 3.
Anthropometric and body composition changes in MD and VLCKD groups according to BMI (mean ± SD).
4. Discussion
The reduction by at least 5% of one’s body weight is linked to improved health outcomes and quality of life for people with overweight and obesity [9]. The European Guidelines for obesity management in adults set this modest weight loss as a goal for people affected by overweight or obesity, underlining that the more weight lost, the more beneficial health effects are seen [41], as also confirmed in other studies [7,10].
In the literature, few studies have evaluated the effects of reaching 5% body weight loss in terms of anthropometric parameters and body composition [7]. Our study focused on observing the time necessary to reach this target at different ages and BMIs by comparing two nutritional protocols on anthropometric and body composition parameters.
The results of this study confirmed those of other ones in the literature where both the MD and VLCKD were efficient in reducing body weight, waist circumference, and fat mass while preserving FFM and BCM in subjects with overweight or obesity [24,34,35,36,37,42,43]. The goal to lose at least 5% of one’s body weight was reached after a month of VLCKD and after 3 months of MD. In the study of Magkos et al., after 3.5 months, participants lost 5% of their initial body weight following a hypocaloric diet, and they decreased FM by 8%± 3% but also had a 2%± 2% reduction in FFM [7]. This result is not in line with ours, because in our study we did not observe an FFM reduction. The preservation of FFM, especially of body cellular mass, is an important issue, as its reduction alters energy metabolism and decreases muscle strength as well as lung and immune capacity [44,45]. Maximizing fat loss while preserving lean mass and its function is a central goal of overweight and obesity treatment [46]; in fact, fat-free mass represents a key determinant of the magnitude of one’s resting metabolic rate (RMR) [47].
As in other studies in the literature, we observed a significant reduction in body weight, BMI, WC, and FM after both diets in both male and female groups. The comparison between male groups of both diets showed no significant differences. A couple of literature studies that evaluated the effects of a VLCKD on the male population were focused on its effect on testicular function [48] or metabolic hypogonadism and beta cell function [49]. Both studies were longer than ours (at least 12 weeks) and had a different aim, so they did not evaluate body composition changes, only body weight and BMI as anthropometrical parameters. In any case, even in these studies, the researchers observed a significant reduction in body weight and BMI compared to baseline [48,49]. Moreover, the effects of MD on anthropometric and body composition parameters in a male population could be seen in the study of Carneiro-Barrera et al., in which 75 males were randomized to a usual care group or an eight-week weight loss and lifestyle intervention group to observe an improvement in sleep apnea. They reached their goal after a significant reduction in body weight (p < 0.0001) and fat mass (p < 0.0001) thanks to a Mediterranean diet [50]. In terms of female results, in our MD group, there was both a greater reduction in waist circumference and fat mass percentage and a higher increase in total body water percentage and fat-free mass percentage compared to the VLCKD group. Our study confirmed other results in the literature about weight loss, BMI, and WC reduction after one month of VLCKD, and they are also in line with FFM preservation [51]. The study of Barrea et al. observed a significant increase in the phase angle (considered an inflammation marker) in 260 women after 1 month of VLCKD, but in our study, we did not observe any changes in the phase angle in all subgroups [52]. Similar results on anthropometric parameters in women with overweight or obesity were seen in the study of Tragni et al. [53]. This study used 24 weeks of the VLCKD because it also accounted for the reintroduction phase. In the whole study, patients reduced body weight (−14.6%) and waist circumference (−12.4%), and at the end of the protocol, 33% of participants reached a normal weight [53]. We observed similar results on anthropometric parameters, but our study was shorter because it only considered the active phase.
To evaluate the effects of these two different nutritional protocols on FFM, we stratified the population according to age. We chose the threshold of 50 years old because generally, after the 50th year, significant aging processes take place, and every year after the 50th there could be a small physiological loss of fat-free mass and strength [54]. Even if muscle mass tends to decrease physiologically with age, we did not observe any reductions in fat-free mass and body cellular mass after both dietary regimes. Although a diet poor in carbohydrates may increase muscle catabolism [55], exacerbating fat-free mass loss during weight loss, the VLCKD preserved FFM and body cellular mass. The same result was seen after the MD. Indeed, both dietary plans could be considered safe for the risk of sarcopenia. We noticed that in subjects younger than 50 years, the MD was more effective than the VLCKD in reducing waist circumference (p = 0.0076) and fat mass percentage (p = 0.0019) and in increasing free-fat mass percentage (p = 0.0326) and total body water percentage (p = 0.0040). In the >50 group, there was no difference between the MD and VLCKD, but we noticed that intragroup, there was a significant increase in FFM (p < 0.0001 for both diets), and BCM was not affected by weight loss. Other studies in the literature did not divide by age, and they usually observed the results on the whole population, which comprised both younger and elder subjects.
5. Conclusions
The original aspect of this study was evaluating the time necessary to at least achieve the goal of 5% of body weight loss with two different dietary treatments. We observed that this result was achieved through one month of the Very-Low-Calorie Ketogenic diet and three months of the Mediterranean diet.
These two nutritional protocols are adequate for both men and women of different age groups with overweight or obesity. Both dietary programs induced weight and fat mass loss without affecting free-fat mass and body cellular mass.
It is clear that the MD is a nutritional protocol useful for the prevention and management of non-communicable diseases such as obesity and metabolic and cardiovascular diseases with high diet adherence and satisfaction by patients [56], but nowadays, the Very-Low-Calorie Ketogenic diet has become even more popular, especially due its rapid effect on weight loss. Thus, people, especially those with severe obesity, are more motivated to follow this nutritional protocol to attain faster results. However, it is important to remember that a VLCKD is not sustainable in the long term, and it requires a gradual transition to a Mediterranean diet [57]. Therefore, combining these two nutritional therapies might be a winning strategy to help people healthily lose weight, increasing their motivation [11,29,32,33].
The results of this study are promising. The large number of participants and the small number of dropouts are surely a strength of the study. Amongst limitations of the study there is that we did not monitor levels of physical activity and diet adherence with a food diary but relied on participants’ reports of their food intakes during the fortnight phone calls and follow-up visits. This could determine a bias, as subjects might forget some details about their food and drink intakes, as recently highlighted in a systematic review. People tend to frequently misestimate their food portions and sometimes forget their consumptions of some food, such as vegetables or seasonings [58]. In the present study, patients’ reports about their food intakes, in terms of portion sizes and frequencies, were in accordance with those established by the study protocol. Moreover, in our study we focused only on anthropometrical and body composition changes rather than on biochemical assessment (i.e., glycemia and lipid profile). The European Guidelines for obesity management in adults underline that VLCKDs determine greater reduction of total cholesterol and serum triglycerides but do not improve glycemic levels, HbA1c, LDL cholesterol, or HDL cholesterol compared to other nutritional protocols for the same time span [14]. For a future study, it could be interesting to evaluate the effects of the two nutritional patterns considered in the study on glycemic and lipid profile once the goal of 5% of body weight loss is reached. Another limitation of this study is that our results refer to a short period of time, while it would be interesting to know if these improvements are maintained over time. Studies in the literature show that after 6 months a VLCKD determines more significant results compared to a hypocaloric diet on weight loss, but after 12 months this difference is no more significant. In fact, people who follow a hypocaloric diet are able to continue losing weight over time, while people who follow a VLCKD tend to regain a bit of weight during or after the reintroduction phase [59]. Our study, in fact, showed that in two different time spans the results on body weight and body composition are similar, but it could be interesting to schedule a follow-up visit after 6 or 12 months to check weight maintenance, as this is the most challenging aspect of diet therapy [60]. To avoid weight gain after a diet period, it is important to define realistic goals to gradually change lifestyle habits and maintain weight loss over time [41]. These lifestyle changes could be obtained through nutrition education and the permanent acquisition of healthy habits. Counseling, positive reinforcement, and motivation could help patients avoid weight regain [61].
Our study demonstrates that there is not a single strategy for body weight management; in fact, different nutritional protocols (even if in different time spans) can reach the same result in terms of both anthropometrical parameters and body composition changes. It is still necessary to understand patients’ needs and health status to define a “tailor-made” nutritional treatment.
Author Contributions
Conceptualization, Y.M.K. and C.D.R.; methodology, Y.M.K., C.D.R., G.L., S.P., I.B. and C.S.; formal analysis, C.D.R., Y.M.K. and N.V.; data curation, C.D.R., F.D.J., G.G., V.M. and M.C.; writing—original draft preparation, C.D.R., E.I. and Y.M.K.; writing—review and editing, C.D.R., G.D., E.I., Y.M.K. and C.S.; visualization, S.P., G.L., G.G., I.B., C.S. and V.M.; supervision, Y.M.K., S.M., G.D., C.S. and M.C.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee Campus Bio-Medico University of Rome” for studies involving humans (approval code of the study 130.21 OSS).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Yu, W.; Rohli, K.E.; Yang, S.; Jia, P. Impact of obesity on COVID-19 patients. J. Diabetes Complicat. 2021, 35, 107817. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity and Overweight Fact Sheet; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Batch, J.T.; Lamsal, S.P.; Adkins, M.; Sultan, S.; Ramirez, M.N. Advantages and Disadvantages of the Ketogenic Diet: A Review Article. Cureus 2020, 12, e9639. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. PASSI Surveillance System. 2019. Available online: https://www.epicentro.iss.it/passi/dati/sovrappeso?tab-container-1=tab1 (accessed on 9 March 2022).
- WHO Consultation on Obesity; World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; WHO Technical Report Series; World Health Organization: Geneva, Switzerland, 2000; Volume 894, 252. [Google Scholar]
- Varkevisser, R.D.M.; Van Stralen, M.M.; Kroeze, W.; Ket, J.C.F.; Steenhuis, H.M. Determinants of weight loss maintenance: A systematic review. Obes. Rev. 2019, 20, 171–211. [Google Scholar] [CrossRef] [PubMed]
- Magkos, F.; Fraterrigo, G.; Yoshino, J.; Luecking, C.; Kirbach, K.; Kelly, S.C.; de las Fuentes, L.; He, S.; Okunade, A.L.; Patterson, B.W.; et al. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016, 23, 591–601. [Google Scholar] [CrossRef]
- Standard Italiani per la Cura Dell’obesità SIO—ADI 2016–2017; Società Italiana dell’Obesità: Milan, Italy, 2017.
- Kushner, R. Obesity 2021: Current clinical management of a chronic serious disease. Supplement to the journal of family practice. J. Fam. Pract. 2021, 70, S35–S40. [Google Scholar]
- Wing, R.R.; Lang, W.; Wadden, T.A.; Safford, M.; Knowler, W.C.; Bertoni, A.G.; Hill, J.O.; Brancati, F.L.; Peters, A.; Wagenknecht, L.; et al. Benefit of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011, 34, 1481–1486. [Google Scholar] [CrossRef]
- Paoli, A.; Bianco, A.; Grimaldi, K.A.; Lodi, A.; Bosco, G. Long term successful weight loss with a combination biphasic ketogenic Mediterranean diet and Mediterranean diet maintenance protocol. Nutrients 2013, 5, 5205–5217. [Google Scholar] [CrossRef]
- Di Rosa, C.; Lattanzi, G.; Taylor, S.F.; Manfrini, S.; Khazrai, Y.M. Very low—Calorie ketogenic diets in overweight and obesity treatment: Effects on anthropometric parameters, body composition, satiety, lipid profile and microbiota. Obes. Res. Clin. Pract. 2020, 14, 491–503. [Google Scholar] [CrossRef]
- Kim, J.Y. Optimal Diet Strategies for Weight Loss and Weight Loss Maintenance. J. Obes. Metab. Syndr. 2021, 30, 20–31. [Google Scholar] [CrossRef]
- Muscogiuri, G.; El Goch, M.; Colao, A.; Hassapidou, M.; Yumuk, V.; Busetto, L. Obesity Management Task Force (OMTF) of the European Association for the study of Obesity (EASO) European Guidelines for Obesity Management in Adults with a Very Low-Calorie Ketogenic Diet: A Systematic Review and Meta-Analysis. Obes. Facts 2021, 14, 222–245. [Google Scholar] [CrossRef]
- Castellana, M.; Conte, E.; Cignarelli, A.; Perrini, S.; Giustina, A.; Giovanella, L.; Giorgino, F.; Trimboli, P. Efficacy and safety of very low—Calorie ketogenic diet (VLCKD) in patients with overweight and obesity: A systematic review and meta-analysis. Rev. Endocr. Metab. Disord. 2019, 21, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Masood, W.; Annamaraju, P.; Uppaluri, K.R. Ketogenic Diet; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Serra-Majem, L.; Tomaino, L.; Dernini, S.; Berry, E.M.; Lairon, D.; de la Cruz, J.N.; Bach-Faig, A.; Donini, L.M.; Medina, F.X.; Belahsen, R.; et al. Updating the Mediterranean Diet Pyramid towards sustainability: Focus on environmental concerns. Int. J. Environ. Res. Public Health 2020, 17, 8758. [Google Scholar] [CrossRef] [PubMed]
- Landry, M.J.; Crimarco, A.; Perelman, D.; Lindsay, R.D.; Petlura, C.; Aronica, L.; Robinson, J.L.; Kim, S.H.; Gardner, D. Adherence to Ketogenic and Mediterranean Study Diets in a Crossover Trial: The Keto—Med Randomized Trial. Nutrients 2021, 13, 967. [Google Scholar] [CrossRef] [PubMed]
- Keys, A.B. How to Eat Well and Stay Well the Mediterranean Way; Doubleday: Garden City, NY, USA, 1975; p. 488. [Google Scholar]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef]
- Diolintzi, A.; Panagiotakos, D.B.; Sidossis, L.S. From Mediterranean diet to Mediterranean lifestyle: A narrative review. Public Health Nutr. 2019, 22, 2703–2713. [Google Scholar] [CrossRef]
- Schroder, H. Protective mechanisms of the Mediterranean diet in obesity and type 2 diabetes. J. Nutr. Biochem. 2007, 18, 149–160. [Google Scholar] [CrossRef]
- Willett, W.C.; Leibel, R.L. Dietary fat is not a major determinant of body fat. Am. J. Med. 2002, 113 (Suppl. 9B), 47S–59S. [Google Scholar] [CrossRef]
- Mancini, J.G.; Filion, K.B.; Atallah, R.; Eisenberg, M.J. Systematic review of the Mediterranean diet for long-term weight loss. Am. J. Med. 2016, 129, 407–415. [Google Scholar] [CrossRef]
- Cheskin, L.J.; Kahan, S. Low-carbohydrate and Mediterranean diets led to greater weight loss than a low-fat diet in moderately obese adults. EBM 2008, 13, 6. [Google Scholar] [CrossRef]
- Keys, A.; Menotti, A.; Karvonen, M.J.; Aravanis, C.; Blackburn, H.; Buzina, R.; Djordjevic, B.S.; Dontas, A.S.; Fidanza, F.; Keys, M.H.; et al. The diet and 15-year death rate in the seven countries study. Am. J. Epidemiol. 1986, 124, 903–915. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Barrea, L.; Laudisio, D.; Pugliese, G.; Salzano, C.; Savastano, S.; Colao, A. The management of very low-calorie ketogenic diet in obesity outpatient clinic: A practical guide. J. Transl. Med. 2019, 17, 356. [Google Scholar] [CrossRef]
- Trimboli, P.; Castellana, M.; Bellido, D.; Casanueva, F.F. Confusion in the nomenclature of ketogenic diets blurs evidence. Rev. Endocr. Metab. Disord. 2020, 21, 1–3. [Google Scholar] [CrossRef]
- Krebs, H.A. The regulation of the release of ketone bodies by the liver. Adv. Enzym. Regul. 1966, 4, 339–354. [Google Scholar] [CrossRef]
- Caprio, M.; Infante, M.; Moriconi, E.; Armani, A.; Fabbri, A.; Mantovani, G.; Mariani, S.; Lubrano, C.; Poggiogalle, E.; Migliaccio, S.; et al. Very-low-calorie ketogenic diet (VLCKD) in the management of metabolic diseases: Systematic review and consensus statement from the Italian Society of Endocrinology (SIE). J. Endocrinol. Investig. 2019, 45, 1365–1386. [Google Scholar] [CrossRef]
- Spera, G.; Mariani, S. Diete chetogeniche: Ruolo nel trattamento di sovrappeso e obesità. L’endocrinologo 2017, 18, 285–290. [Google Scholar] [CrossRef]
- Moreno, B.; Bellido, D.; Sajoux, I.; Goday, A.; Saavedra, D.; Crujeiras, A.B.; Casanueva, F.F. Comparison of a very low-calorie-ketogenic diet with a standard low-calorie diet in the treatment of obesity. Endocrine 2014, 47, 793–805. [Google Scholar] [CrossRef]
- Moreno, B.; Crujeiras, A.B.; Bellido, D.; Sajoux, I.; Casanueva, F.F. Obesity treatment by very low-calorie-ketogenic diet at two years: Reduction in visceral fat and on the burden of disease. Endocrine 2016, 54, 681–690. [Google Scholar] [CrossRef]
- Castro, A.I.; Gomez-Arbelaez, D.; Crujeiras, A.B.; Granero, R.; Aguera, Z.; Jimenez-Murcia, S.; Sajoux, I.; Lopez-Jaramillo, P.; Fernandez-Aranda, F.; Casanueva, F.F. Effect of a very low-calorie ketogenic diet on food and alcohol cravings physical and sexual activity, sleep disturbances, and quality of life in obese patients. Nutrients 2018, 10, 1348. [Google Scholar] [CrossRef]
- Gomez-Arbelaez, D.; Bellido, D.; Castro, A.I.; Ordoñez-Mayan, L.; Carreira, J.; Galban, C.; Martinez-Olmos, M.A.; Crujeiras, A.B.; Sajoux, I.; Casanueva, F.F. Body composition changes after very low-calorie- ketogenic diet in obesity evaluated by three standardized methods. J. Clin. Endocrinol. Metab. 2016, 102, 488–498. [Google Scholar] [CrossRef]
- Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation. 2008. Available online: https://www.who.int/publications/i/item/9789241501491 (accessed on 13 September 2022).
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gomez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.-C.; Pirlich, M.; et al. Bioelectrical impedance analysis-part I: Review of principles and methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef]
- Livelli di Assunzione di Riferimento di Nutrienti ed Energia per la Popolazione Italiana, LARN; IV Revisione; Società Italiana di Nutrizione Umana (SINU): Milan, Italy, 2014.
- Yumuk, V.; Tsigos, C.; Fried, M.; Schndler, K.; Busetto, L.; Micic, D.; Toplak, H. European Guidelines for Obesity Management in adults. Obes. Facts 2015, 8, 402–424. [Google Scholar] [CrossRef]
- Esposito, K.; Marfella, R.; Ciotola, M.; Di Palo, C.; Giugliano, F.; Giugliano, G.; D’Armiento, M.; D’Andrea, F.; Giugliano, D. Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA 2004, 292, 1440–1446. [Google Scholar] [CrossRef]
- Bautista-Castaño, I.; Molina-Cabrillana, J.; Montoya-Alonso, J.A.; Serra-Majem, L. Variables predictive of adherence to diet and physical-activity recommendations in the treatment of obesity and overweight, in a group of Spanish Subjects. Int. J. Obes. Relat. Metab. Disord. 2004, 28, 697–705. [Google Scholar] [CrossRef][Green Version]
- Andreoli, A.; Lauro, S.; Di Daniele, N.; Sorge, R.; Celi, M.; Volpe, S.L. Effect of a moderately hypoenergetic Mediterranean diet and exercise program on body cell mass and cardiovascular risk factors in obese women. Eur. J. Clin. Nutr. 2008, 62, 892–897. [Google Scholar] [CrossRef]
- Martins, P.C.; Hansen, F.; Silva, A.M.; Silva, D.A.S. Fluid distribution and cell integrity indicators evaluated by bioelectrical impedance in university athletes: Comparison between team sports and individual sports. Physiol. Meas. 2019, 40, 015004. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Gonzalez, M.C.; Shen, W.; Redman, L.; Thomas, D. Weight loss composition is one-fourth fat-free mass: A critical review and critique of this widely cited rule. Obes. Rev. 2014, 15, 310–321. [Google Scholar] [CrossRef]
- Johannsen, D.L.; Knuth, N.D.; Huizenga, R.; Rood, J.C.; Ravussin, E.; Hall, K.D. Metabolic slowing with massive weight loss despite preservation of fat-free mass. J. Clin. Endocrinol. Metab. 2012, 97, 2489–2496. [Google Scholar] [CrossRef]
- Mongioì, L.M.; Cimino, L.; Condorelli, R.A.; Magagnini, M.C.; Barbagallo, F.; Cannarella, R.; La Vignera, S.; Calogero, A.E. Effectiveness of a Very Low Calorie Ketogenic Diet on Testicular Function in Overweight/Obese Men. Nutrients 2020, 12, 2967. [Google Scholar] [CrossRef]
- La Vignera, S.; Cannarella, R.; Galvano, F.; Grillo, A.; Aversa, A.; Cimino, L.; Magagnini, C.M.; Mongioì, L.M.; Condorelli, R.A.; Calogero, A.E. The ketogenic diet corrects metabolic hypogonadism and preserves pancreatic ß-cell function in overweight/obese men: A single-arm uncontrolled study. Endocrine 2021, 72, 392–399. [Google Scholar] [CrossRef]
- Carneiro-Barrera, A.; Amaro-Gahete, F.J.; Jurado-Fasoli, L.; Sáez-Roca, G.; Martín-Carrasco, C.; Tinahones, F.J.; Ruiz, J.R. Effect of a Weight Loss and Lifestyle Intervention on Dietary Behavior in Men with Obstructive Sleep Apnea: The INTERAPNEA Trial. Nutrients 2022, 14, 2731. [Google Scholar] [CrossRef]
- Rondanelli, M.; Perna, S.; Ilyas, Z.; Peroni, G.; Bazire, P.; Sajuox, I.; Maugeri, R.; Nichetti, M.; Gasparri, C. Effect of very low-calorie ketogenic diet in combination with omega-3 on inflammation, satiety hormones, body composition, and metabolic markers. A pilot study in class I obese subjects. Endocrine 2022, 75, 129–136. [Google Scholar] [CrossRef]
- Barrea, L.; Muscogiuri, G.; Aprano, S.; Vetrani, C.; de Alteriis, G.; Varcamonti, L.; Verde, L.; Colao, A.; Savastano, S. Phase angle as an easy diagnostic tool for the nutritionist in the evaluation of inflammatory changes during the active stage of a very low-calorie ketogenic diet. Int. J. Obes. 2022, 46, 1591–1597. [Google Scholar] [CrossRef]
- Tragni, E.; Vigna, L.; Ruscica, M.; Macchi, C.; Casula, M.; Santelia, A.; Catapano, A.L.; Magni, P. Reduction of Cardio-Metabolic Risk and Body Weight through a Multiphasic Very-Low Calorie Ketogenic Diet Program in Women with Overweight/Obesity: A Study in a Real-World Setting. Nutrients 2021, 13, 1804. [Google Scholar] [CrossRef]
- Keller, K.; Engelhardt, M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 2014, 3, 346–350. [Google Scholar] [CrossRef]
- Wood, R.J.; Gregory, S.M.; Sawyer, J.; Milch, C.M.; Matthews, T.D.; Headley, S.A. Preservation of fat-free mass after two distinct weight loss diets with and without progressive resistance exercise. Metab. Syndr. Relat. Disord. 2012, 10, 167–174. [Google Scholar] [CrossRef]
- Silva, A.M.; Heymsfield, S.B.; Gallagher, D.; Albu, J.; Pi-Sunyer, X.-F.; Pierson, R.N.J.; Wang, J.; Heska, S.; Sardinha, L.B.; Wang, Z. Evaluation of between-methods agreement of extracellular water measurements in adults and children. Am. J. Clin. Nutr. 2008, 88, 315–323. [Google Scholar] [CrossRef][Green Version]
- Joshi, S.; Mohan, V. Pros & cons of some popular extreme weight-loss diets. Indian J. Med. Res. 2018, 148, 642–647. [Google Scholar]
- Whitton, C.; Ramos-Garcìa, C.; Kirkpatrick, S.I.; Healy, J.D.; Dhaliwal, S.S.; Boushey, C.J.; Collins, C.E.; Rollo, M.E.; Kerr, D.A. A Systematic Review Examining Contributors to Misestimation of Food and Beverage Intake Based on Short-Term Self-Report Dietary Assessment Instruments Administered to Adults. Adv. Nutr. 2022, nmac085. [Google Scholar] [CrossRef]
- Stern, L.; Iqbal, N.; Seshadri, P.; Chicano, K.L.; Daily, D.; McGrory, J.; Williams, M.; Gracely, E.J.; Samaha, F.F. The Effects of Low-Carbohydrate versus Conventional Weight Loss Diets in Severely Obese Adults: One-Year Follow-up of a Randomized Trial. Ann. Intern. Med. 2004, 140, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Thom, G.; Lean, M. Is There an Optimal Diet for Weight Management and Metabolic Health? Gastroenterology 2017, 152, 1739–1751. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Khan, S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med. Clin. N. Am. 2018, 102, 183–197. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).