Empowerment for the Digital Transformation: Results of a Structured Blended-Learning On-the-Job Training for Practicing Physicians in Germany
Abstract
1. Introduction
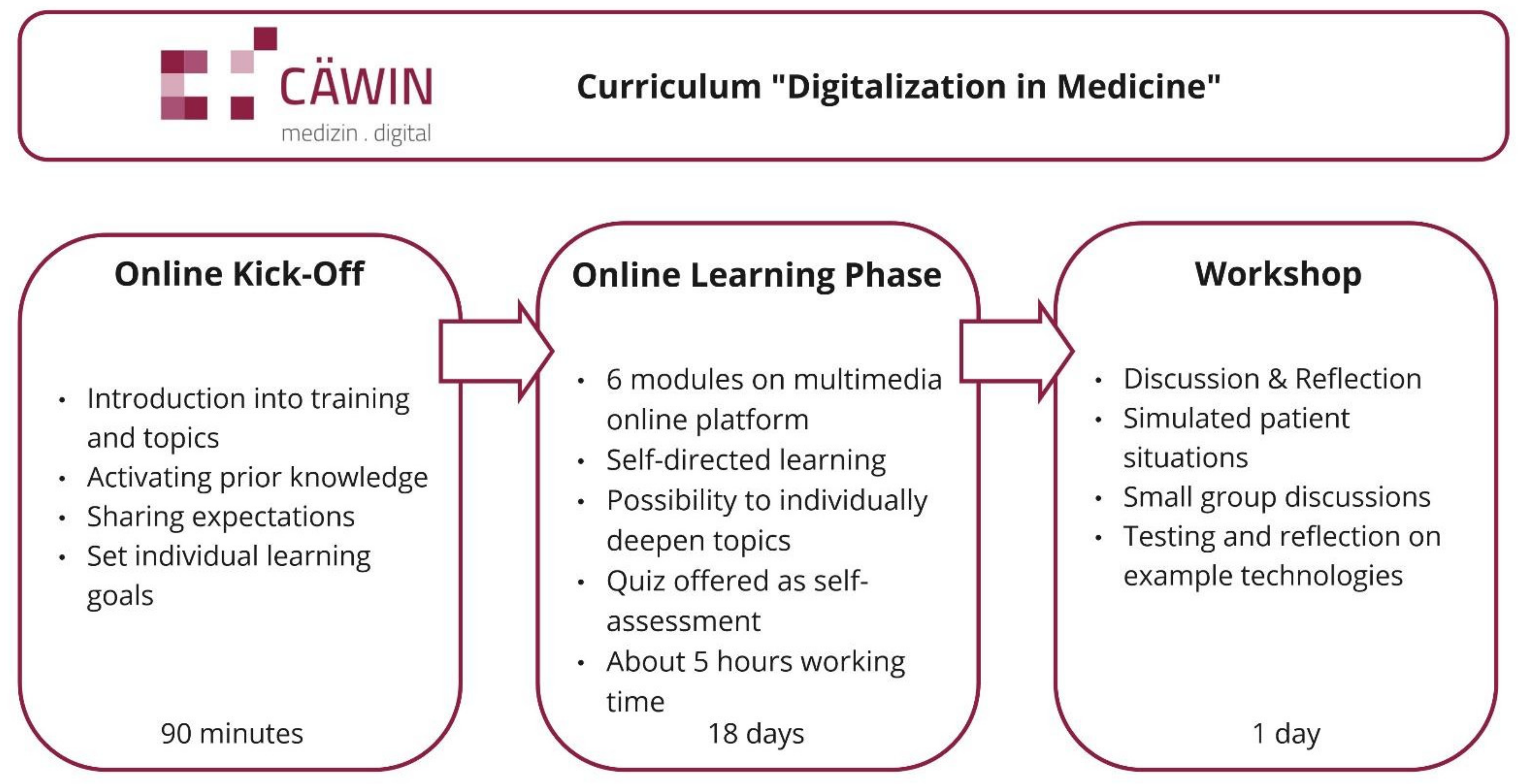
2. Materials and Methods
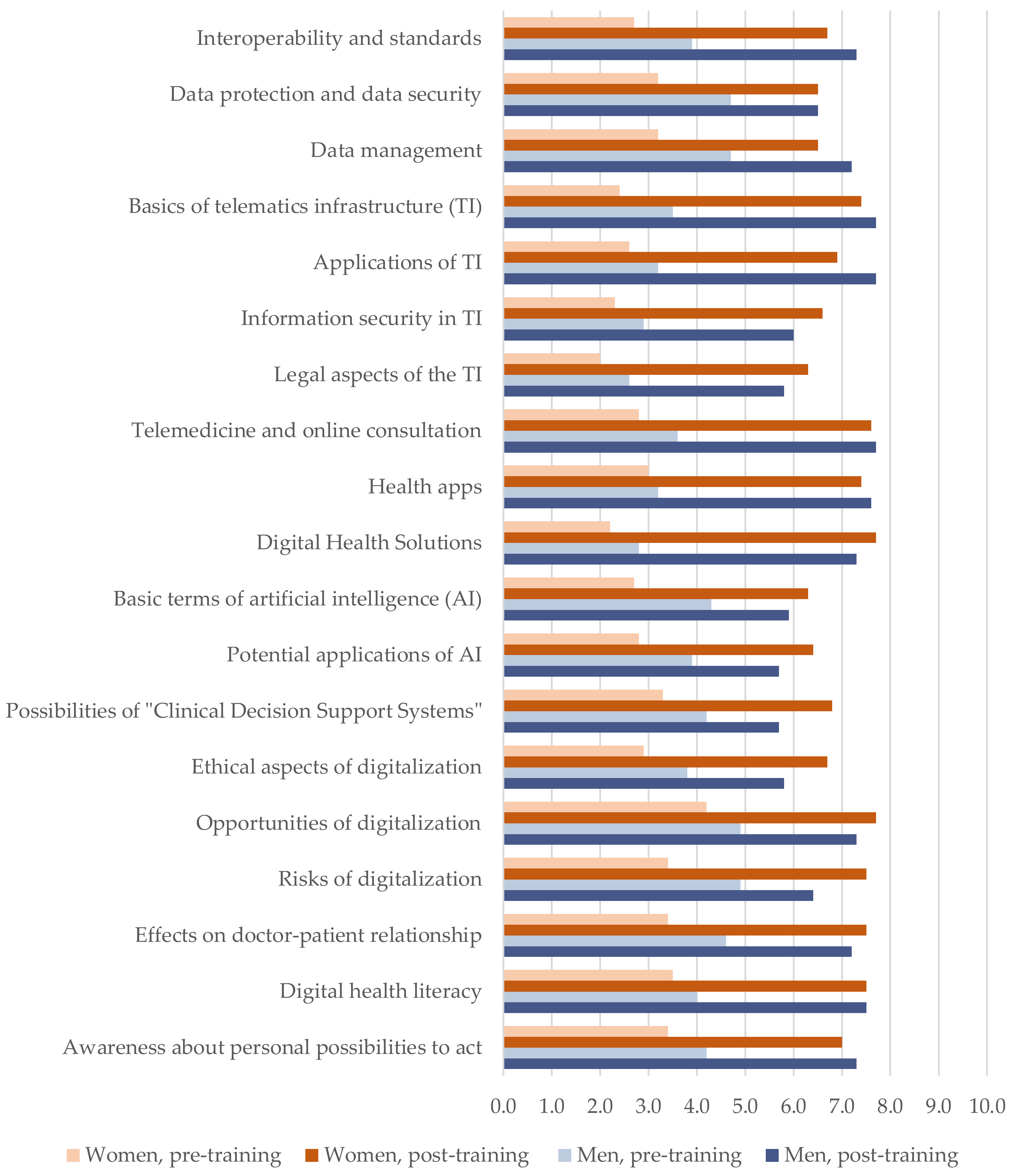
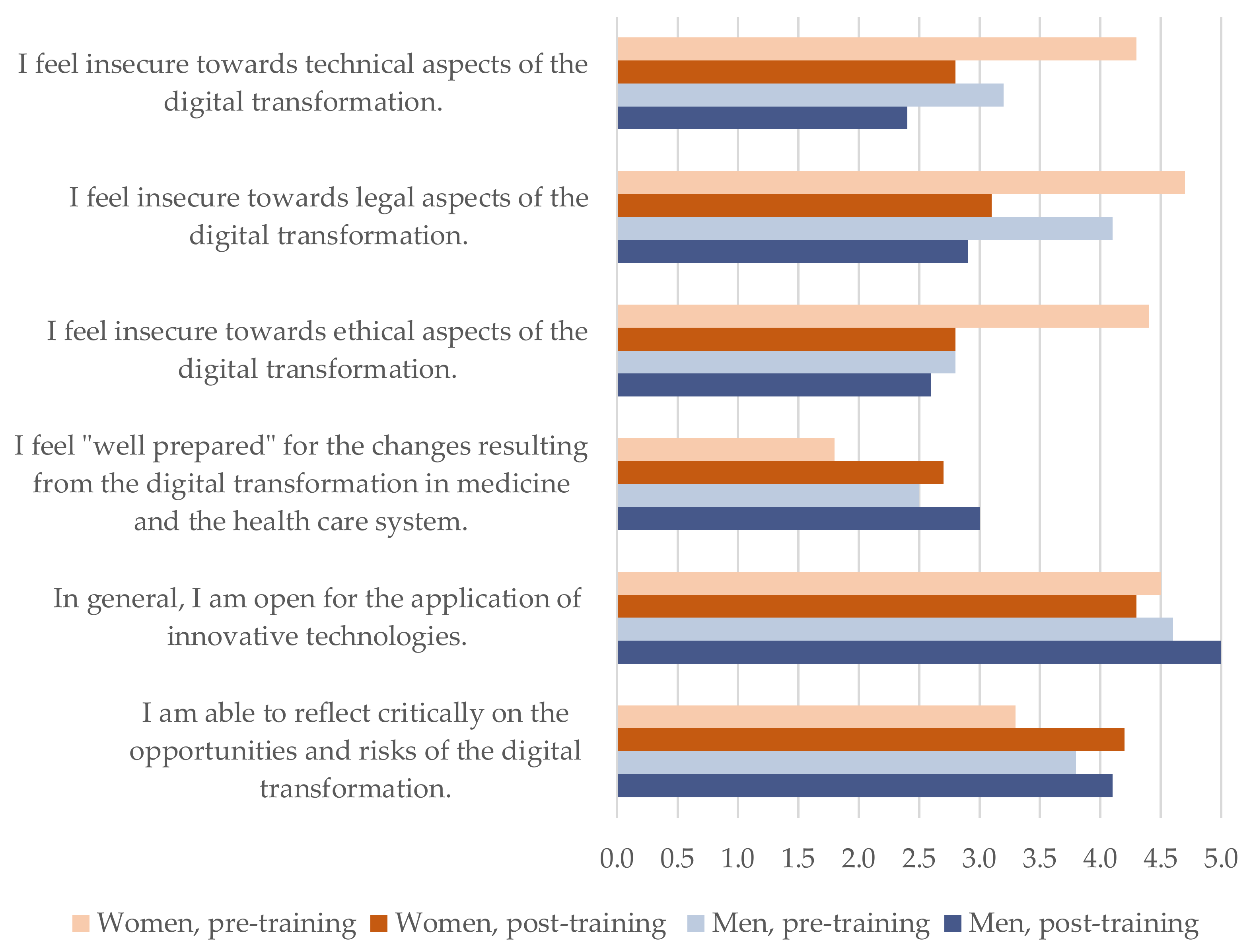
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kuhn, S.; Heusel-Weiss, M.; Kadioglu, D.; Michl, S. Digitale Transformation der Medizin: Die Zukunft aktiv gestalten. Dtsch. Arztebl. 2019, 116, A830–A834. [Google Scholar]
- Foadi, N.; Varghese, J. Digital competence: A Key Competence for Todays and Future Physicians. J. Eur. CME 2022, 11, 2015200. [Google Scholar] [CrossRef] [PubMed]
- Topol, E. The Topol Review. Preparing the Healthcare Workforce to Deliver the Digital Future. Political Report. NHS Health Education England. 2019. Available online: https://topol.hee.nhs.uk/ (accessed on 30 August 2022).
- Hofstetter, S.; Lehmann, L.; Zilezinski, M.; Steindorff, J.V.; Jahn, P.; Paulicke, D. Vermittlung digitaler Kompetenzen in der Pflegeausbildung: Eine Vergleichsanalyse der Rahmenpläne von Bund und Ländern. Teaching digital competences in nursing education: A comparative analysis of the federal and state framework curricula. Bundesgesundheitsblatt-Gesundh.-Gesundh. 2022, 65, 891–899. [Google Scholar] [CrossRef] [PubMed]
- OECD. Health in the 21st Century: Putting Data to Work for Stronger Health Systems; OECD Publishing: Paris, France, 2019. [Google Scholar]
- Fagherazzi, G.; Ravaud, P. Digital diabetes: Perspectives for diabetes prevention, management and research. Diabetes Metab. 2019, 45, 322–329. [Google Scholar] [CrossRef]
- Mesko, B.; Győrffy, Z. The Rise of the Empowered Physician in the Digital Health Era: Viewpoint. J. Med. Internet Res. 2019, 21, e12490. [Google Scholar] [CrossRef]
- Education Council. Recommendation of the European Parliament and the Council of 18 December 2006 on key competencies for lifelong learning. Off. J. Eur. Union 2006, 30, 2006. [Google Scholar]
- Giunti, G.; Guisado-Fernandez, E.; Belani, H.; Lacalle-Remigio, J.R. Mapping the access of future doctors to health information technologies training in the European Union: Cross-sectional descriptive study. J. Med. Internet Res. 2019, 21, e14086. [Google Scholar] [CrossRef]
- Dahlhausen, F.; Zinner, M.; Bieske, L.; Ehlers, J.P.; Boehme, P.; Fehring, L. There’s an app for that, but nobody’s using it: Insights on improving patient access and adherence to digital therapeutics in Germany. Digit. Health 2022, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Leigh, S.; Ashall-Payne, L. The role of health-care providers in mHealth adoption. Lancet Digit. Health 2019, 1, e58–e59. [Google Scholar] [CrossRef]
- Jezrawi, R.; Balakumar, S.; Masud, R.; Gabizon, I.; Bhagirath, V.; Varughese, J.; Brown, M.S.; Trottier, D.; Schwalm, J.D.; McGillion, M.H.; et al. Patient and physician perspectives on the use and outcome measures of mHealth apps: Exploratory survey and focus group study. Digit. Health 2022, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Committee on Digital Skills for Health Professionals. Digital Skills for Health Professionals; European Health Parliament: Brussels, Belgium, 2016. [Google Scholar]
- Roda, S. Digital Skills for Doctors: Explaining European Doctors’ Position. J. Eur. CME 2021, 10, 2014097. [Google Scholar] [CrossRef]
- Bosch, J.; Ludwig, C.; Niebuhr, J.; Haucke, E.; Schwarz, K.; Prondzinsky, R.; Stoevesandt, D.; Gekle, M. Digitalisierung in der Medizin: Ein Curriculum für die ärztliche Weiterbildung an der Martin-Luther-Universität Halle-Wittenberg. Ärzteblatt Sachs. -Anhalt 2022, 20–25. [Google Scholar]
- Machleid, F.; Kaczmarczyk, R.; Johann, D.; Balčiūnas, J.; Atienza-Carbonell, B.; von Maltzahn, F.; Mosch, L. Perceptions of digital health education among European medical students: Mixed methods survey. J. Med. Internet Res. 2020, 22, e19827. [Google Scholar] [CrossRef] [PubMed]
- Dixon, B.E.; Barboza, K.; Jensen, A.E.; Bennett, K.J.; Sherman, S.E.; Schwartz, M.D. Measuring practicing clinicians’ information literacy. Appl. Clin. Inform. 2017, 26, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, G.; Spinazze, P.; Matchar, D.; Huat, G.K.C.; van der Kleij, R.M.; Chavannes, N.H.; Car, J. Digital health competencies for primary healthcare professionals: A scoping review. Int. J. Med. Inform. 2020, 143, 104260. [Google Scholar] [CrossRef]
- Lloyds Bank. Lloyds Bank UK Consumer Digital Index; Lloyds Bank: Birmingham, UK, 2020. [Google Scholar]
- Vossen, K.; Rethans, J.-J.; van Kuijk, S.M.J.; van der Vleuten, C.P.; Kubben, P.L. Understanding Medical Students’ Attitudes Toward Learning eHealth: Questionnaire Study. JMIR Med. Educ. 2020, 6, e17030. [Google Scholar] [CrossRef]
- Kirchberg, J.; Fritzmann, J.; Weitz, J.; Bork, U. eHealth Literacy of German Physicians in the Pre-COVID-19 Era: Questionnaire Study. JMIR Mhealth Uhealth 2020, 8, e20099. [Google Scholar] [CrossRef]
- Li, S.; Bamidis, P.D.; Konstantinidis, S.T.; Traver, V.; Car, J.; Zary, N. Setting priorities for EU healthcare workforce IT skills competence improvement. Health Inform. J. 2019, 25, 174–185. [Google Scholar] [CrossRef]
- Gordon, W.J.; Landman, A.; Zhang, H.; Bates, D.W. Beyond validation: Getting health apps into clinical practice. NPJ Digit. Med. 2020, 3, 14. [Google Scholar] [CrossRef]
- Kuhn, S.; Müller, N.; Kirchgässner, E.; Ulzheimer, L.; Deutsch, K.L. Digital skills for medical students—Qualitative evaluation of the curriculum 4.0 “Medicine in the digital age”. GMS J. Med. Educ. 2020, 37, Doc60. [Google Scholar]
- Spante, M.; Sofkova Hashemi, S.; Lundin, M.; Algers, A. Digital competence and digital literacy in higher education research: Systematic review of concept use. Cogent Educ. 2018, 5, 1519143. [Google Scholar] [CrossRef]
- Oberländer, M.; Beinicke, A.; Bipp, T. Digital competencies: A review of the literature and applications in the workplace. Comput. Educ. 2020, 146, 103752. [Google Scholar] [CrossRef]
- Lizzio, A.; Wilson, K. Action learning in higher education: An investigation of its potential to develop professional capability. Stud. High. Educ. 2004, 29, 469–488. [Google Scholar] [CrossRef]
- Ferrari, A. Digital competence in practice: An analysis of frameworks. Sevilla JRC IPTS 2012, 10, 82116. [Google Scholar]
- Nazeha, N.; Pavagadhi, D.; Kyaw, B.M.; Car, J.; Jimenez, G.; Tudor Car, L. A Digitally Competent Health Workforce: Scoping Review of Educational Frameworks. J. Med. Internet Res. 2020, 22, e22706. [Google Scholar] [CrossRef]
- Konttila, J.; Siira, H.; Kyngäs, H.; Lahtinen, M.; Elo, S.; Kääriäinen, M.; Kaakinen, P.; Oikarinen, A.; Yamakawa, M.; Fukui, S.; et al. Healthcare professionals’ competence in digitalisation: A systematic review. J. Clin. Nurs. 2019, 28, 745–761. [Google Scholar] [CrossRef] [PubMed]
- Traver, V.; Konstantinidis, S.T.; Bamidis, P.D.; Zary, N. Analysis of EU-USA cooperation opportunities on IT skills for healthcare workforce. Stud Health Technol Inf. 2015, 210, 561–563. [Google Scholar]
- Wang, J.J.; Singh, R.K.; Miselis, H.H.; Stapleton, S.N. Technology Literacy in Undergraduate Medical Education: Review and Survey of the US Medical School Innovation and Technology Programs. JMIR Med. Educ. 2022, 8, e32183. [Google Scholar] [CrossRef]
- Kuhn, S. Kompetent für die Medizin im digitalen Zeitalter. Berl. Ärzt:Innen 2020, 6, 15–18. [Google Scholar]
- Bundesärztekammer. Curriculum Digitale Gesundheitsanwendungen in Praxis und Klinik; Bundesärztekammer: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Foadi, N.; Koop, C.; Behrends, M. Medizinische Ausbildung: Welche digitalen Kompetenzen braucht der Arzt. Dtsch. Arztebl. 2020, 117, 596–600. [Google Scholar]
- Smith, B.; Magnani, J.W. New technologies, new disparities: The intersection of electronic health and digital health literacy. Int. J. Cardiol. 2019, 292, 280–282. [Google Scholar] [CrossRef]
- Oxford University Press. Oxford Advanced Learner’s Dictionary. Available online: https://www.oxfordlearnersdictionaries.com/ (accessed on 31 August 2022).
- Frenk, J.; Chen, L.; Bhutta, Z.A.; Cohen, J.; Crisp, N.; Evans, T.; Fineberg, H.; Garcia, P.; Ke, Y.; Kelley, P. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet 2010, 376, 1923–1958. [Google Scholar] [CrossRef]
- Ross, J.; Stevenson, F.; Lau, R.; Murray, E. Factors that influence the implementation of e-health: A systematic review of systematic reviews (an update). Implement. Sci. 2016, 11, 146. [Google Scholar] [CrossRef]
- Bosch, J.; Maaz, A.; Hitzblech, T.; Holzhausen, Y.; Peters, H. Medical students’ preparedness for professional activities in early clerkships. BMC Med. Educ. 2017, 17, 140. [Google Scholar] [CrossRef]
- Fagerlind, A.-C.; Gustavsson, M.; Johansson, G.; Ekberg, K. Experience of work-related flow: Does high decision latitude enhance benefits gained from job resources? J. Vocat. Behav. 2013, 83, 161–170. [Google Scholar] [CrossRef]
- Wysham, N.G.; Howie, L.; Patel, K.; Cameron, C.B.; Samsa, G.P.; Roe, L.; Abernethy, A.P.; Zaas, A. Development and refinement of a learning health systems training program. eGEMs 2016, 4, 1236. [Google Scholar] [CrossRef]
- Golz, C.; Peter, K.A.; Müller, T.J.; Mutschler, J.; Zwakhalen, S.M.G.; Hahn, S. Technostress and digital competence among health professionals in Swiss psychiatric hospitals: Cross-sectional study. JMIR Ment. Health 2021, 8, e31408. [Google Scholar] [CrossRef]
- Downing, N.L.; Bates, D.W.; Longhurst, C.A. Physician burnout in the electronic health record era. Ann. Intern. Med. 2019, 170, 216–217. [Google Scholar] [CrossRef]
- Salmela-Aro, K.; Mutanen, P.; Vuori, J. Promoting career preparedness and intrinsic work-goal motivation: RCT intervention. J. Vocat. Behav. 2012, 80, 67–75. [Google Scholar] [CrossRef]
- Ochsmann, E.B.; Zier, U.; Drexler, H.; Schmid, K. Well prepared for work? Junior doctors’ self-assessment after medical education. BMC Med. Educ. 2011, 11, 99. [Google Scholar] [CrossRef]
- Villamañán, E.; Larrubia, Y.; Ruano, M.; Vélez, M.; Armada, E.; Herrero, A.; Álvarez-Sala, R. Potential medication errors associated with computer prescriber order entry. Int. J. Clin. Pharm. 2013, 35, 577–583. [Google Scholar] [CrossRef]
- Han, Y.Y.; Carcillo, J.A.; Venkataraman, S.T.; Clark, R.S.B.; Watson, R.S.; Nguyen, T.C.; Bayir, H.; Orr, R.A. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics 2005, 116, 1506–1512. [Google Scholar] [CrossRef]
- Zhao, Y.; Llorente, A.M.P.; Gómez, M.C.S. Digital competence in higher education research: A systematic literature review. Comput. Educ. 2021, 168, 104212. [Google Scholar] [CrossRef]
- Thomas, P.A.; Kern, D.E.; Hughes, M.T.; Chen, B.Y. Curriculum Development for Medical Education: A Six-Step Approach; Johns Hopkins University Press: Baltimore, MD, USA, 2009. [Google Scholar]
- Tolks, D.; Schäfer, C.; Raupach, T.; Kruse, L.; Sarikas, A.; Gerhardt-Szép, S.; Kllauer, G.; Lemos, M.; Fischer, M.R.; Eichner, B. An introduction to the inverted/flipped classroom model in education and advanced training in medicine and in the healthcare professions. GMS J. Med. Educ. 2016, 33, Doc46. [Google Scholar]
- De Gagne, J.C.; Park, H.K.; Hall, K.; Woodward, A.; Yamane, S.; Kim, S.S. Microlearning in health professions education: Scoping review. JMIR Med. Educ. 2019, 5, e13997. [Google Scholar] [CrossRef]
- Graham, J.W. Missing data analysis: Making it work in the real world. Annu. Rev. Psychol. 2009, 60, 549–576. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2007. [Google Scholar]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Lenhard, W.; Lenhard, A. Berechnung von Effektstärken. Available online: https://www.psychometrica.de (accessed on 31 August 2022).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Liu, Q.; Peng, W.; Zhang, F.; Hu, R.; Li, Y.; Yan, W. The effectiveness of blended learning in health professions: Systematic review and meta-analysis. J. Med. Internet Res. 2016, 18, e4807. [Google Scholar] [CrossRef]
- Miller, G.E. The assessment of clinical skills/competence/performance. Acad. Med. 1990, 65, S63–S67. [Google Scholar] [CrossRef]
- Jarva, E.; Oikarinen, A.; Andersson, J.; Tuomikoski, A.-M.; Kääriäinen, M.; Meriläinen, M.; Mikkonen, K. Healthcare professionals’ perceptions of digital health competence: A qualitative descriptive study. Nurs. Open 2022, 9, 1379–1393. [Google Scholar] [CrossRef] [PubMed]
- Pfob, A.; Sidey-Gibbons, C.; Schuessler, M.; Lu, S.-C.; Xu, C.; Dubsky, P.; Golatta, M.; Heil, J. Contrast of digital and health literacy between IT and health care specialists highlights the importance of multidisciplinary teams for digital health: A pilot study. JCO Clin. Cancer Inform. 2021, 5, 734–745. [Google Scholar] [CrossRef] [PubMed]
- Baartman, L.K.J.; de Bruijn, E. Integrating knowledge, skills and attitudes: Conceptualising learning processes towards vocational competence. Educ. Res. Rev. 2011, 6, 125–134. [Google Scholar] [CrossRef]
- Panadero, E.; Jonsson, A.; Botella, J. Effects of self-assessment on self-regulated learning and self-efficacy: Four meta-analyses. Educ. Res. Rev. 2017, 22, 74–98. [Google Scholar] [CrossRef]
- Hinz, A.; Schumacher, J.; Albani, C.; Schmid, G.; Brähler, E. Bevölkerungsrepräsentative Normierung der Skala zur Allgemeinen Selbstwirksamkeitserwartung. Diagnostica 2006, 52, 26–32. [Google Scholar] [CrossRef]
- Geist, L.; Immenschuh, U.; Jahn, P.; Paulicke, D.; Zilezinski, M.; Buhtz, C.; Hofstetter, S. Identifikation von lernfördernden Maßnahmen zur Einführung von digitalen und assistiven Technologien (DAT) in Prozesse der pflegerischen Versorgung: Eine qualitative Studie [Teaching digital competences in nursing education—A comparative analysis of the federal and state framework curricula.]. Bundesgesundheitsblatt-Gesundh.-Gesundh. 2022, 1–9. [Google Scholar]
- Bertelsmann Stiftung. Smart Health Systems: Digitalisierungsstrategien im internationalen Vergleich. Spotlight Gesundh. 2018. [Google Scholar]
- NHS England. A Plan for Digital Health and Social Care. Policy Paper. Available online: https://www.gov.uk/government/publications/a-plan-for-digital-health-and-social-care/a-plan-for-digital-health-and-social-care#summary (accessed on 30 August 2022).
- Moore, D.E., Jr.; Green, J.S.; Gallis, H.A. Achieving desired results and improved outcomes: Integrating planning and assessment throughout learning activities. J. Contin. Educ. Health Prof. 2009, 29, 1–15. [Google Scholar] [CrossRef]
| T1 | T2 | T3 | Sum | |
|---|---|---|---|---|
| Number of participants (training completed) | 7 | 11 | 14 | 32 |
| Women | 2 | 4 | 7 | 13 |
| Men | 5 | 7 | 7 | 19 |
| Resident physician | 2 | 4 | 6 | 12 |
| Specialist | 0 | 2 | 4 | 6 |
| Senior physician | 3 | 3 | 3 | 9 |
| Chief physician | 1 | 1 | 0 | 2 |
| Professional position not indicated | 1 | 1 | 1 | 3 |
| Pre-Training | Post-Training | g | ||||||
|---|---|---|---|---|---|---|---|---|
| Nr. | Item | n | M | SD | n | M | SD | |
| Knowledge | ||||||||
| 1 | Interoperability and standards | 32 | 3.5 | 2.3 | 31 | 7.2 | 1.3 | 1.98 |
| 2 | Data protection and data security | 32 | 4.3 | 2.3 | 31 | 6.5 | 1.8 | 1.06 |
| 3 | Data management | 32 | 4.4 | 2.1 | 31 | 6.9 | 1.7 | 1.31 |
| 4 | Basics of telematics infrastructure (TI) | 32 | 3.2 | 1.8 | 31 | 7.7 | 1.7 | 2.57 |
| 5 | Applications of TI | 31 | 3.0 | 1.9 | 31 | 7.5 | 2.0 | 2.31 |
| 6 | Information security in TI | 32 | 2.7 | 1.5 | 31 | 6.5 | 2.0 | 2.16 |
| 7 | Legal aspects of the TI | 32 | 2.4 | 1.2 | 31 | 6.2 | 2.0 | 2.31 |
| 8 | Telemedicine and online consultation | 32 | 3.3 | 1.8 | 31 | 7.7 | 1.5 | 2.65 |
| 9 | Health apps | 32 | 3.3 | 1.8 | 31 | 7.6 | 1.7 | 2.46 |
| 10 | Digital health solutions | 32 | 2.8 | 1.7 | 31 | 7.6 | 1.7 | 2.82 |
| 11 | Basic terms of artificial intelligence (AI) | 32 | 3.9 | 2.0 | 31 | 6.3 | 2.1 | 1.17 |
| 12 | Potential applications of AI | 32 | 3.7 | 2.0 | 31 | 6.2 | 2.1 | 1.22 |
| 13 | Possibilities of clinical decision-support systems | 31 | 4.0 | 2.2 | 31 | 6.4 | 1.8 | 1.19 |
| 14 | Ethical aspects of digitalization | 32 | 3.5 | 1.6 | 31 | 6.4 | 1.4 | 1.93 |
| 15 | Opportunities of digitalization | 32 | 4.7 | 2.1 | 31 | 7.5 | 1.5 | 1.53 |
| 16 | Risks of digitalization | 32 | 4.4 | 1.9 | 31 | 7.0 | 1.5 | 1.52 |
| 17 | Effects on doctor–patient relationship | 32 | 4.1 | 2.0 | 31 | 7.4 | 1.4 | 1.91 |
| 18 | Digital health literacy | 32 | 3.8 | 1.9 | 31 | 7.6 | 1.6 | 2.16 |
| 19 | Awareness about personal possibilities to act | 32 | 3.9 | 2.1 | 31 | 7.3 | 1.5 | 1.86 |
| Attitude | ||||||||
| 1 | I feel insecure towards technical aspects of the digital transformation. | 24 | 3.7 | 1.0 | 25 | 2.6 | 1.2 | −0.99 |
| 2 | I feel insecure towards legal aspects of the digital transformation. | 23 | 4.3 | 0.7 | 25 | 3.0 | 1.1 | −1.40 |
| 3 | I feel insecure towards ethical aspects of the digital transformation. | 24 | 3.5 | 1.2 | 25 | 2.6 | 1.0 | −0.82 |
| 4 | I feel well-prepared for the changes resulting from the digital transformation in medicine and the health care system. | 24 | 2.3 | 1.2 | 25 | 2.8 | 1.0 | 0.45 |
| 5 | In general, I am open for the application of innovative technologies. | 24 | 4.6 | 0.6 | 25 | 4.6 | 0.8 | 0.00 |
| 6 | I am able to reflect critically on the opportunities and risks of the digital transformation. | 24 | 3.7 | 0.8 | 25 | 4.1 | 0.5 | 0.60 |
| Dependent Variable | df | F | p | ηp2 |
|---|---|---|---|---|
| Interoperability and standards | 1, 55 | 71.29 | <0.0001 | 0.56 |
| Data protection and data security | 1, 55 | 22.16 | <0.0001 | 0.29 |
| Data management | 1, 55 | 35.25 | <0.0001 | 0.39 |
| Basics of telematics infrastructure (TI) | 1, 55 | 97.09 | <0.0001 | 0.64 |
| Applications of TI | 1, 55 | 75.14 | <0.0001 | 0.58 |
| Information security in TI | 1, 55 | 62.79 | <0.0001 | 0.53 |
| Legal aspects of the TI | 1, 55 | 80.62 | <0.0001 | 0.59 |
| Telemedicine and online consultation | 1, 55 | 104.61 | <0.0001 | 0.66 |
| Health apps | 1, 55 | 102.49 | <0.0001 | 0.65 |
| Digital health solutions | 1, 55 | 122.54 | <0.0001 | 0.69 |
| Basic terms of artificial intelligence (AI) | 1, 55 | 22.16 | <0.0001 | 0.29 |
| Potential applications of AI | 1, 55 | 26.96 | <0.0001 | 0.33 |
| Possibilities of clinical decision-support systems | 1, 55 | 19.76 | <0.0001 | 0.26 |
| Ethical aspects of digitalization | 1, 55 | 53.84 | <0.0001 | 0.49 |
| Opportunities of digitalization | 1, 55 | 32.10 | <0.0001 | 0.37 |
| Risks of digitalization | 1, 55 | 31.37 | <0.0001 | 0.36 |
| Effects on doctor–patient relationship | 1, 55 | 46.08 | <0.0001 | 0.46 |
| Digital health literacy | 1, 55 | 63.57 | <0.0001 | 0.54 |
| Awareness about personal possibilities to act | 1, 55 | 46.96 | <0.0001 | 0.46 |
| Dependent Variable | df | F | p | ηp2 |
|---|---|---|---|---|
| Insecurity towards technical aspects | 1, 41 | 11.87 | 0.001 | 0.22 |
| Insecurity towards legal aspects | 1, 41 | 21.61 | <0.0001 | 0.35 |
| Insecurity towards ethical aspects | 1, 41 | 5.90 | 0.020 | 0.13 |
| Preparedness for digital transformation | 1, 41 | 3.57 | 0.066 | 0.08 |
| Open for innovative technology | 1, 41 | 0.18 | 0.675 | 0.00 |
| Critical reflection on opportunities and risks | 1, 41 | 6.21 | 0.017 | 0.13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bosch, J.; Ludwig, C.; Fluch-Niebuhr, J.; Stoevesandt, D. Empowerment for the Digital Transformation: Results of a Structured Blended-Learning On-the-Job Training for Practicing Physicians in Germany. Int. J. Environ. Res. Public Health 2022, 19, 12991. https://doi.org/10.3390/ijerph192012991
Bosch J, Ludwig C, Fluch-Niebuhr J, Stoevesandt D. Empowerment for the Digital Transformation: Results of a Structured Blended-Learning On-the-Job Training for Practicing Physicians in Germany. International Journal of Environmental Research and Public Health. 2022; 19(20):12991. https://doi.org/10.3390/ijerph192012991
Chicago/Turabian StyleBosch, Josefin, Christiane Ludwig, Johannes Fluch-Niebuhr, and Dietrich Stoevesandt. 2022. "Empowerment for the Digital Transformation: Results of a Structured Blended-Learning On-the-Job Training for Practicing Physicians in Germany" International Journal of Environmental Research and Public Health 19, no. 20: 12991. https://doi.org/10.3390/ijerph192012991
APA StyleBosch, J., Ludwig, C., Fluch-Niebuhr, J., & Stoevesandt, D. (2022). Empowerment for the Digital Transformation: Results of a Structured Blended-Learning On-the-Job Training for Practicing Physicians in Germany. International Journal of Environmental Research and Public Health, 19(20), 12991. https://doi.org/10.3390/ijerph192012991






