Use of Telemedicine Technology among General Practitioners during COVID-19: A Modified Technology Acceptance Model Study in Poland
Abstract
1. Introduction
2. Theoretical Basics
3. Materials and Methods
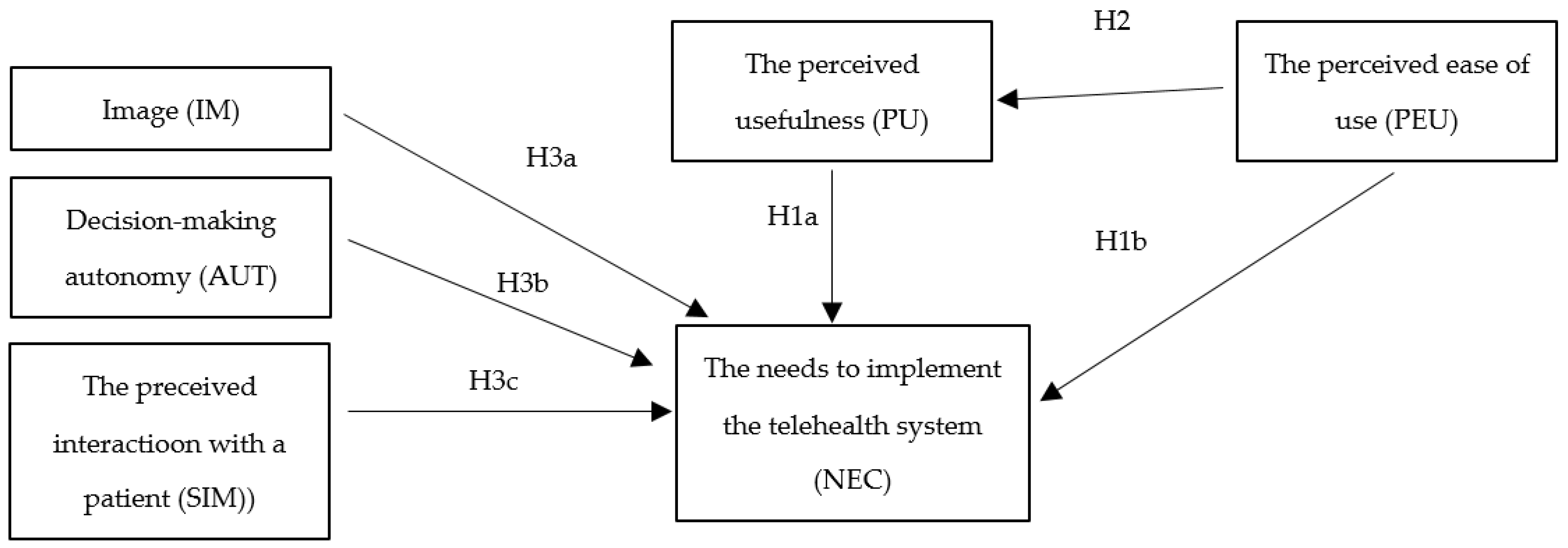
Theoretical Model and Hypotheses
4. Results
4.1. Exploratory Factor Analysis
4.2. Confirmatory Factor Analysis
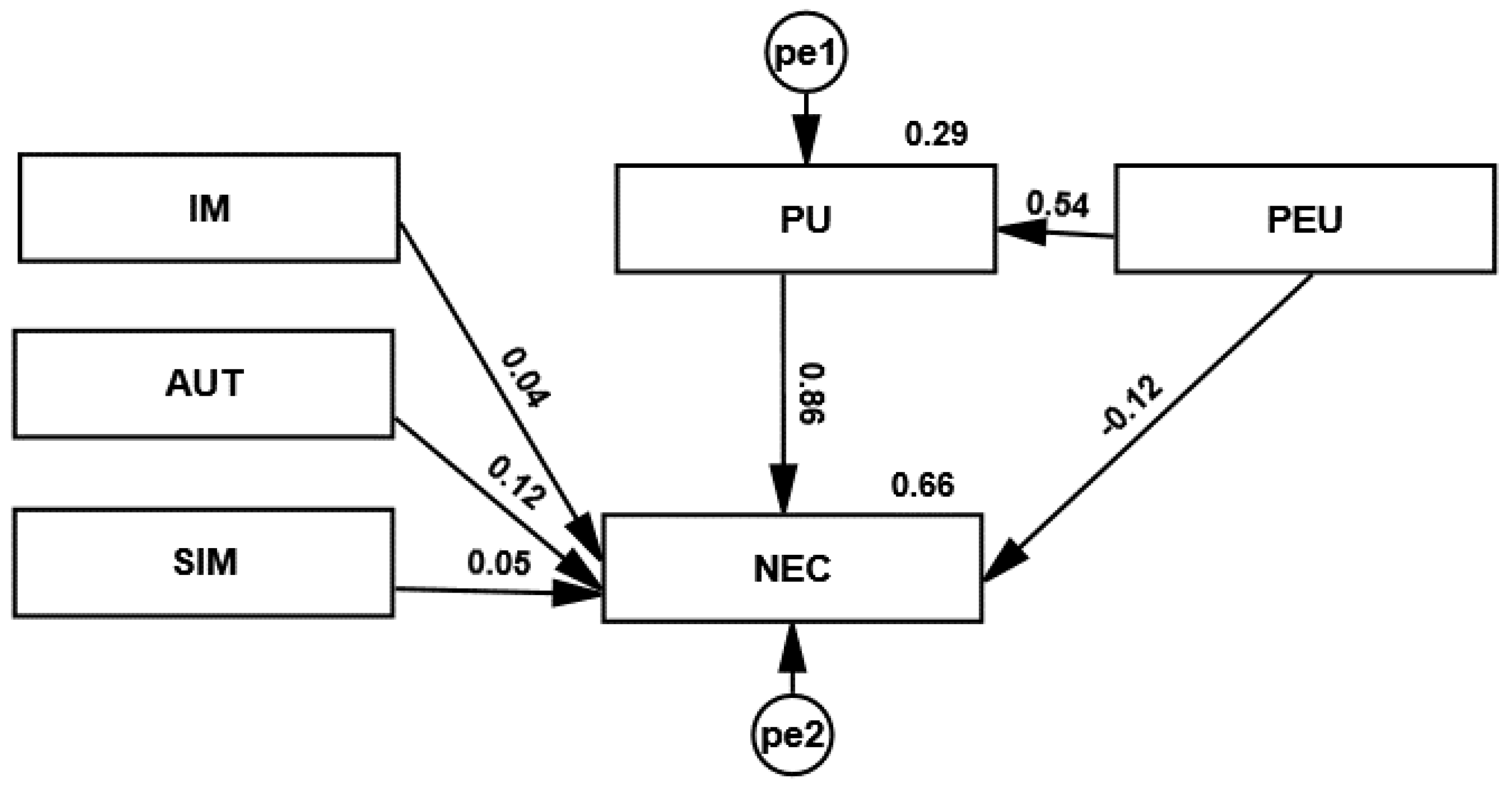
4.3. Structural Model
5. Discussion
5.1. Contribution
5.2. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Garavand, A.; Aslani, N.; Nadri, H.; Abedini, S.; Dehghan, S. Acceptance of telemedicine technology among physicians: A systematic review. Inform. Med. Unlocked 2022, 30, 100943. [Google Scholar] [CrossRef]
- Hyder, M.A.; Razzak, J. Telemedicine in the United States: An Introduction for Students and Residents. J. Med. Internet Res. 2020, 22, e20839. [Google Scholar] [CrossRef]
- Manyazewal, T.; Woldeamanuel, Y.; Blumberg, H.M.; Fekadu, A.; Marconi, V.C. The potential use of digital health technologies in the African context: A systematic review of evidence from Ethiopia. NPJ Digit. Med. 2021, 4, 125. [Google Scholar] [CrossRef]
- Ryu, S. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth 2009 (Global Observatory for eHealth Series, Volume 2). Healthc. Inform. Res. 2012, 18, 153. [Google Scholar] [CrossRef]
- Andrews, V. Using telemedicine in clinical decision-making. Pract. Nurs. 2014, 25, 42–46. [Google Scholar] [CrossRef]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef]
- Rho, M.J.; Choi, I.Y.; Lee, J. Predictive factors of telemedicine service acceptance and behavioral intention of physicians. Int. J. Med. Inform. 2014, 83, 559–571. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, D.; Peterburg, Y.; Vekstein, D.; Pliskin, J.S. Decisions to adopt new technologies at the hospital level: Insights from Israeli medical centers. Int. J. Technol. Assess. Health Care 2005, 21, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Robert, G.; Macfarlane, F.; Bate, P.; Kyriakidou, O. Diffusion of Innovations in Service Organizations: Systematic Review and Recommendations. Milbank Q. 2004, 82, 581–629. [Google Scholar] [CrossRef] [PubMed]
- Robert, G.; Greenhalgh, T.; MacFarlane, F.; Peacock, R. Adopting and assimilating new non-pharmaceutical technologies into health care: A systematic review. J. Health Serv. Res. Policy 2010, 15, 243–250. [Google Scholar] [CrossRef]
- Reyes, P.M.; Li, S.; Visich, J.K. Accessing antecedents and outcomes of RFID implementation in health care. Int. J. Prod. Econ. 2012, 136, 137–150. [Google Scholar] [CrossRef]
- Wernz, C.; Zhang, H.; Phusavat, K. International study of technology investment decisions at hospitals. Ind. Manag. Data Syst. 2014, 114, 568–582. [Google Scholar] [CrossRef]
- Gold, H.T.; Pitrelli, K.; Hayes, M.K.; Murphy, M.M. Decision to adopt medical technology: Case study of breast cancer radiotherapy techniques. Med. Decis. Mak. 2014, 34, 1006–1015. [Google Scholar] [CrossRef]
- Barasa, E.W.; Molyneux, S.; English, M.; Cleary, S. Setting healthcare priorities in hospitals: A review of empirical studies. Health Policy Plan. 2015, 30, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User Acceptance of Computer Technology: A Comparison of Two Theoretical Models. Manage. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Nakajima, I.; Sawada, Y.; Maeda, T.; Martin, D.L.; Nagano, S.; Hamano, N. Telemedicine Using Small Satellite MEO/HICAT for International Medical Communications. COSPAR Colloq. Ser. 1999, 10, 258–267. [Google Scholar] [CrossRef]
- Aziz, S.R.; Ziccardi, V.B. Telemedicine Using Smartphones for Oral and Maxillofacial Surgery Consultation, Communication, and Treatment Planning. J. Oral Maxillofac. Surg. 2009, 67, 2505–2509. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.H. Integrating Social Capital Theory, Social Cognitive Theory, and the Technology Acceptance Model to Explore a Behavioral Model of Telehealth Systems. Int. J. Environ. Res. Public Health 2014, 11, 4905–4925. [Google Scholar] [CrossRef]
- Taherdoost, H. A review of technology acceptance and adoption models and theories. Procedia Manuf. 2018, 22, 960–967. [Google Scholar] [CrossRef]
- Lai, P. The Literature Review of Technology Adoption Models and Theories for the Novelty Technology. J. Inf. Syst. Technol. Manag. 2017, 14, 21–38. [Google Scholar] [CrossRef]
- Davis, F.D. Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Tarhini, A.; Hone, K.; Liu, X. The effects of individual differences on e-learning users’ behaviour in developing countries: A structural equation model. Comput. Human Behav. 2014, 41, 153–163. [Google Scholar] [CrossRef]
- Becker, D. Acceptance of Mobile Mental Health Treatment Applications. Procedia Comput. Sci. 2016, 98, 220–227. [Google Scholar] [CrossRef]
- Scherer, R.; Siddiq, F.; Tondeur, J. The technology acceptance model (TAM): A meta-analytic structural equation modeling approach to explaining teachers’ adoption of digital technology in education. Comput. Educ. 2019, 128, 13–35. [Google Scholar] [CrossRef]
- Faber, S.; van Geenhuizen, M.; de Reuver, M. eHealth adoption factors in medical hospitals: A focus on the Netherlands. Int. J. Med. Inform. 2017, 100, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Melas, C.D.; Zampetakis, L.A.; Dimopoulou, A.; Moustakis, V. Modeling the acceptance of clinical information systems among hospital medical staff: An extended TAM model. J. Biomed. Inform. 2011, 44, 553–564. [Google Scholar] [CrossRef]
- Khan, I.; Xitong, G.; Ahmad, Z.; Shahzad, F. Investigating Factors Impelling the Adoption of e-Health: A Perspective of African Expats in China. SAGE Open 2019, 9, 2158244019865803. [Google Scholar] [CrossRef]
- Briz-Ponce, L.; García-Peñalvo, F.J. An Empirical Assessment of a Technology Acceptance Model for Apps in Medical Education. J. Med. Syst. 2015, 39, 176. [Google Scholar] [CrossRef]
- Ahlan, A.; Ahmad, B. An overview of patient acceptance of Health Information Technology in developing countries: A review and conceptual model. Int. J. Inf. Syst. Proj. Manag. 2015, 3, 29–48. [Google Scholar] [CrossRef]
- Gagnon, M.P.; Desmartis, M.; Labrecque, M.; Car, J.; Pagliari, C.; Pluye, P.; Frémont, P.; Gagnon, J.; Tremblay, N.; Légaré, F. Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals. J. Med. Syst. 2012, 36, 241–277. [Google Scholar] [CrossRef]
- Schnall, R.; Higgins, T.; Brown, W.; Carballo-Dieguez, A.; Bakken, S. Trust, Perceived Risk, Perceived Ease of Use and Perceived Usefulness as Factors Related to mHealth Technology Use. Stud. Health Technol. Inform. 2015, 216, 467. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, R.A.; Hueros, A.D. Motivational factors that influence the acceptance of Moodle using TAM. Comput. Human Behav. 2010, 26, 1632–1640. [Google Scholar] [CrossRef]
- Marangunić, N.; Granić, A. Technology acceptance model: A literature review from 1986 to 2013. Univers. Access Inf. Soc. 2014, 14, 81–95. [Google Scholar] [CrossRef]
- Ching-Ter, C.; Hajiyev, J.; Su, C.R. Examining the students’ behavioral intention to use e-learning in Azerbaijan? The General Extended Technology Acceptance Model for E-learning approach. Comput. Educ. 2017, 111, 128–143. [Google Scholar] [CrossRef]
- Khatun, F.; Heywood, A.E.; Ray, P.K.; Hanifi, S.M.A.; Bhuiya, A.; Liaw, S.T. Determinants of readiness to adopt mHealth in a rural community of Bangladesh. Int. J. Med. Inform. 2015, 84, 847–856. [Google Scholar] [CrossRef]
- Rahimi, B.; Nadri, H.; Afshar, H.L.; Timpka, T. A systematic review of the technology acceptance model in health informatics. Appl. Clin. Inform. 2018, 9, 604–634. [Google Scholar] [CrossRef] [PubMed]
- Mortenson, M.J.; Vidgen, R. A computational literature review of the technology acceptance model. Int. J. Inf. Manag. 2016, 36, 1248–1259. [Google Scholar] [CrossRef]
- Seehusen, D.A.; Deavers, J.; Mainous, A.G.; Ledford, C.J.W. The intersection of physician wellbeing and clinical application of diabetes guidelines. Patient Educ. Couns. 2018, 101, 894–899. [Google Scholar] [CrossRef]
- Hsieh, P.J. Healthcare professionals’ use of health clouds: Integrating technology acceptance and status quo bias perspectives. Int. J. Med. Inform. 2015, 84, 512–523. [Google Scholar] [CrossRef]
- Williams, A.; Turer, C.; Smith, J.; Nievera, I.; McCulloch, L.; Wareg, N.; Clary, M.; Rajagopalan, A.; Brownson, R.C.; Koopman, R.J.; et al. Adoption of an Electronic Medical Record Tool for Childhood Obesity by Primary Care Providers. Appl. Clin. Inform. 2020, 11, 210–217. [Google Scholar] [CrossRef]
- Tubaishat, A. Perceived usefulness and perceived ease of use of electronic health records among nurses: Application of Technology Acceptance Model. Inform. Health Soc. Care 2018, 43, 379–389. [Google Scholar] [CrossRef] [PubMed]
- Idoga, P.E.; Toycan, M.; Nadiri, H.; Çelebi, E. Factors Affecting the Successful Adoption of e-Health Cloud Based Health System from Healthcare Consumers’ Perspective. IEEE Access 2018, 6, 71216–71228. [Google Scholar] [CrossRef]
- Zayyad, M.A.; Toycan, M. Factors affecting sustainable adoption of e-health technology in developing countries: An exploratory survey of Nigerian hospitals from the perspective of healthcare professionals. PeerJ 2018, 2018, e4436. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Li, H.; Gagnon, M.P. Health IT acceptance factors in long-term care facilities: A cross-sectional survey. Int. J. Med. Inform. 2009, 78, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Vandecasteele, B.; Geuens, M. Motivated Consumer Innovativeness: Concept, measurement, and validation. Int. J. Res. Mark. 2010, 27, 308–318. [Google Scholar] [CrossRef]
- Goldsmith, R.E. The Validity Of A Scale To Measure Global Innovativeness. J. Appl. Bus. Res. 1991, 7, 89–97. [Google Scholar] [CrossRef]
- Aggelidis, V.P.; Chatzoglou, P.D. Using a modified technology acceptance model in hospitals. Int. J. Med. Inform. 2009, 78, 115–126. [Google Scholar] [CrossRef]
- Carter, L.; Bélanger, F. The utilization of e-government services: Citizen trust, innovation and acceptance factors. Inf. Syst. J. 2005, 15, 5–25. [Google Scholar] [CrossRef]
- Venkatesh, V.; Davis, F.D. Theoretical extension of the Technology Acceptance Model: Four longitudinal field studies. Manage. Sci. 2000, 46, 186–204. [Google Scholar] [CrossRef]
- Wu, J.H.; Chen, Y.C.; Lin, L.M. Empirical evaluation of the revised end user computing acceptance model. Comput. Human Behav. 2007, 23, 162–174. [Google Scholar] [CrossRef]
- Venkatesh, V.; Davis, F.D. A Model of the Antecedents of Perceived Ease of Use: Development and Test. Decis. Sci. 1996, 27, 451–481. [Google Scholar] [CrossRef]
- Amoako-Gyampah, K.; Salam, A.F. An extension of the technology acceptance model in an ERP implementation environment. Inf. Manag. 2004, 41, 731–745. [Google Scholar] [CrossRef]
- Ward, R.; Stevens, C.; Brentnall, P.; Briddon, J. The attitudes of health care staff to information technology: A comprehensive review of the research literature. Health. Inf. Libr. J. 2008, 25, 81–97. [Google Scholar] [CrossRef] [PubMed]
- Nazi, K.M. The Personal Health Record Paradox: Health Care Professionals’ Perspectives and the Information Ecology of Personal Health Record Systems in Organizational and Clinical Settings. J. Med. Internet Res. 2013, 15, e2443. [Google Scholar] [CrossRef]
- Simpao, A.F.; Ahumada, L.M.; Gálvez, J.A.; Rehman, M.A. A Review of Analytics and Clinical Informatics in Health Care. J. Med. Syst. 2014, 38, 45. [Google Scholar] [CrossRef]
- Kalayou, M.H.; Endehabtu, B.F.; Tilahun, B. The Applicability of the Modified Technology Acceptance Model (TAM) on the Sustainable Adoption of eHealth Systems in Resource-Limited Settings. J. Multidiscip. Healthc. 2020, 13, 1827. [Google Scholar] [CrossRef]
- Irani, T. Prior Experience, Perceived Usefulness and the Web: Factors Influencing Agricultural Audiences’ Adoption of Internet Communication Tools. J. Appl. Commun. 2000, 84, 49–63. [Google Scholar] [CrossRef]
- Chismar, W.G.; Wiley-Patton, S. Test of the technology acceptance model for the internet in pediatrics. Proc. AMIA Symp. 2002, 155–159. [Google Scholar]
- Schaper, L.K.; Pervan, G.P. ICT and OTs: A model of information and communication technology acceptance and utilisation by occupational therapists. Int. J. Med. Inform. 2007, 76, S212–S221. [Google Scholar] [CrossRef]
- Chau, P.Y.K.; Hu, P.J.H. Investigating healthcare professionals’ decisions to accept telemedicine technology: An empirical test of competing theories. Inf. Manag. 2002, 39, 297–311. [Google Scholar] [CrossRef]
- Hu, P.J.; Chau, P.Y.K.; Liu Sheng, O.R.; Tam, K.Y. Examining the Technology Acceptance Model Using Physician Acceptance of Telemedicine Technology. J. Manag. Inf. Syst. 1999, 16, 91–112. [Google Scholar] [CrossRef]
- Chau, P.Y.K.; Hu, P.J. Examining a Model of Information Technology Acceptance by Individual Professionals: An Exploratory Study. J. Manag. Inf. Syst. 2014, 18, 191–229. [Google Scholar] [CrossRef]
- Vance Wilson, E.; Lankton, N.K. Modeling patients’ acceptance of provider-delivered E-health. J. Am. Med. Inform. Assoc. 2004, 11, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.J.; Yang, K.F.; Tang, F.I.; Huang, C.H.; Yu, S. Applying the technology acceptance model to explore public health nurses’ intentions towards web-based learning: A cross-sectional questionnaire survey. Int. J. Nurs. Stud. 2008, 45, 869–878. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.H.; Wang, S.C.; Lin, L.M. Mobile computing acceptance factors in the healthcare industry: A structural equation model. Int. J. Med. Inform. 2007, 76, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Tung, F.C.; Chang, S.C.; Chou, C.M. An extension of trust and TAM model with IDT in the adoption of the electronic logistics information system in HIS in the medical industry. Int. J. Med. Inform. 2008, 77, 324–335. [Google Scholar] [CrossRef]
- Tilahun, B.; Fritz, F. Modeling antecedents of electronic medical record system implementation success in low-resource setting hospitals Healthcare Information Systems. BMC Med. Inform. Decis. Mak. 2015, 15, 61. [Google Scholar] [CrossRef]
- Biruk, S.; Yilma, T.; Andualem, M.; Tilahun, B. Health Professionals’ readiness to implement electronic medical record system at three hospitals in Ethiopia: A cross sectional study. BMC Med. Inform. Decis. Mak. 2014, 14, 115. [Google Scholar] [CrossRef]
- Yehualashet, G.; Asemahagn, M.; Tilahun, B. The Attitude towards and Use of Electronic Medical Record System by Health Professionals at a Referral Hospital in Northern Ethiopia: Cross-Sectional Study. J. Health Inform. Africa 2015, 3, 19–29. [Google Scholar] [CrossRef]
- Garavand, A.; Mohseni, M.; Asadi, H.; Etemadi, M.; Moradi-Joo, M.; Moosavi, A. Factors influencing the adoption of health information technologies: A systematic review. Electron. Physician 2016, 8, 2713. [Google Scholar] [CrossRef]
- Zhou, M.; Zhao, L.; Kong, N.; Campy, K.S.; Qu, S.; Wang, S. Factors influencing behavior intentions to telehealth by Chinese elderly: An extended TAM model. Int. J. Med. Inform. 2019, 126, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Alexandra, S.; Handayani, P.W.; Azzahro, F. Indonesian hospital telemedicine acceptance model: The influence of user behavior and technological dimensions. Heliyon 2021, 7, e08599. [Google Scholar] [CrossRef]
- Kamal, S.A.; Shafiq, M.; Kakria, P. Investigating acceptance of telemedicine services through an extended technology acceptance model (TAM). Technol. Soc. 2020, 60, 101212. [Google Scholar] [CrossRef]
- Lanseng, E.J.; Andreassen, T.W. Electronic healthcare: A study of people’s readiness and attitude toward performing self-diagnosis. Int. J. Serv. Ind. Manag. 2007, 18, 394–417. [Google Scholar] [CrossRef]
- Sandberg, J.; Trief, P.M.; Izquierdo, R.; Goland, R.; Morin, P.C.; Palmas, W.; Larson, C.D.; Strait, J.G.; Shea, S.; Weinstock, R.S. A Qualitative Study of the Experiences and Satisfaction of Direct Telemedicine Providers in Diabetes Case Management. Telemed. e-Health 2009, 15, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Olver, I.N.; Selva-Nayagam, S. Evaluation of a Telemedicine Link Between Darwin and Adelaide to Facilitate Cancer Management. Telemed. J. 2004, 6, 213–218. [Google Scholar] [CrossRef]
- Zaidi, S.T.R.; Marriott, J.L.; Nation, R.L. The role of perceptions of clinicians in their adoption of a web-based antibiotic approval system: Do perceptions translate into actions? Int. J. Med. Inform. 2008, 77, 33–40. [Google Scholar] [CrossRef]
- Taylor, P. Evaluating telemedicine systems and services. J. Telemed. Telecare 2005, 11, 167–177. [Google Scholar] [CrossRef]
- Park, H.-Y.; Kwon, Y.-M.; Jun, H.-R.; Jung, S.-E.; Kwon, S.-Y. Satisfaction Survey of Patients and Medical Staff for Telephone-Based Telemedicine during Hospital Closing Due to COVID-19 Transmission. Telemed. e-Health 2020, 27, 724–732. [Google Scholar] [CrossRef]
- Martínez, A.; Everss, E.; Rojo-Álvarez, J.L.; Figal, D.P.; García-Alberola, A. A systematic review of the literature on home monitoring for patients with heart failure. J. Telemed. Telecare 2006, 12, 234–241. [Google Scholar] [CrossRef]
- Dünnebeil, S.; Sunyaev, A.; Blohm, I.; Leimeister, J.M.; Krcmar, H. Determinants of physicians’ technology acceptance for e-health in ambulatory care. Int. J. Med. Inform. 2012, 81, 746–760. [Google Scholar] [CrossRef] [PubMed]
- Rajan, C.A.; Baral, R. Adoption of ERP system: An empirical study of factors influencing the usage of ERP and its impact on end user. IIMB Manag. Rev. 2015, 27, 105–117. [Google Scholar] [CrossRef]
- Hung, S.Y.; Ku, Y.C.; Chien, J.C. Understanding physicians’ acceptance of the Medline system for practicing evidence-based medicine: A decomposed TPB model. Int. J. Med. Inform. 2012, 81, 130–142. [Google Scholar] [CrossRef] [PubMed]
- Thong, J.Y.L.; Hong, W.; Tam, K.Y. Understanding user acceptance of digital libraries: What are the roles of interface characteristics, organizational context, and individual differences? Int. J. Hum. Comput. Stud. 2002, 57, 215–242. [Google Scholar] [CrossRef]
- Hatz, M.H.M.; Sonnenschein, T.; Blankart, C.R. The PMA Scale: A Measure of Physicians’ Motivation to Adopt Medical Devices. Value Health 2017, 20, 533–541. [Google Scholar] [CrossRef]
- Teplensky, J.D.; Pauly, M.V.; Kimberly, J.R.; Hillman, A.L.; Schwartz, J.S. Hospital adoption of medical technology: An empirical test of alternative models. Health Serv. Res. 1995, 30, 437. [Google Scholar]
- Wu, J.H.; Shen, W.S.; Lin, L.M.; Greenes, R.A.; Bates, D.W. Testing the technology acceptance model for evaluating healthcare professionals’ intention to use an adverse event reporting system. Int. J. Qual. Health Care 2008, 20, 123–129. [Google Scholar] [CrossRef]
- Moeinedin, F. Assessing Primary Care Physicians’ Attitudes towards Adoption of an Electronic Tool to Support Cancer Diagnosis; University of Toronto: Toronto, ON, Canada, 2011. [Google Scholar]
- Abdekhoda, M.; Ahmadi, M.; Gohari, M.; Noruzi, A. The effects of organizational contextual factors on physicians’ attitude toward adoption of Electronic Medical Records. J. Biomed. Inform. 2015, 53, 174–179. [Google Scholar] [CrossRef]
- Handayani, P.W.; Hidayanto, A.N.; Pinem, A.A.; Hapsari, I.C.; Sandhyaduhita, P.I.; Budi, I. Acceptance model of a Hospital Information System. Int. J. Med. Inform. 2017, 99, 11–28. [Google Scholar] [CrossRef]
- Moore, G.C.; Benbasat, I. Development of an Instrument to Measure the Perceptions of Adopting an Information Technology Innovation. Inf. Syst. Res. 1991, 2, 192–222. [Google Scholar] [CrossRef]
- Teutsch, C. Patient–doctor communication. Med. Clin. North Am. 2003, 87, 1115–1145. [Google Scholar] [CrossRef]
- Ventres, W.; Kooienga, S.; Vuckovic, N.; Marlin, R.; Nygren, P.; Stewart, V. Physicians, Patients, and the Electronic Health Record: An Ethnographic Analysis. Ann. Fam. Med. 2006, 4, 124–131. [Google Scholar] [CrossRef]
- Werner, P.; Karnieli, E. A model of the willingness to use telemedicine for routine and specialized care. J. Telemed. Telecare 2003, 9, 264–272. [Google Scholar] [CrossRef]
- Rimmer, M.P.; Al Wattar, B.H.; on behalf of the UKARCOG Members. Provision of obstetrics and gynaecology services during theCOVID-19 pandemic: A survey of junior doctors in the UK National Health Service. BJOG 2020, 127, 1123–1128. [Google Scholar] [CrossRef]
- Bakken, S.; Ghullo-Ficurnoa, L.; Izquierdo, R.; Lee, N.-J.; Morin, P.; Palmas, W.; Teresi, J.; Weinstock, R.; Shea, S.; Starren, J. Development, Validation, and use of English and Spanish Versions of the TElemedicine Satisfaciot and Usefulness Questionnaire. J. Am. Med. Inform. Assoc. 2006, 13, 660–667. [Google Scholar] [CrossRef]
- Whitten, P.; Doolittle, G.; Mackert, M. Providers’ Acceptance of Telehospice. J. Palliat. Med. 2005, 8, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Holden, R.J.; Karsh, B.T. The Technology Acceptance Model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Adewale, E. An Exploratory Qualitative Investigation into the Acceptance of Telemedicine Technologies in the Washington DC Metro Area. Doctoral Dissertation, Colorado Technical University, Colorado Springs, CO, USA, 2015. [Google Scholar]
- Yi, M.Y.; Jackson, J.D.; Park, J.S.; Probst, J.C. Understanding information technology acceptance by individual professionals: Toward an integrative view. Inf. Manag. 2006, 43, 350–363. [Google Scholar] [CrossRef]
- Tabachnick, B.; Fidell, L. Using Multivariate Statistics; Pearson Education: Upper Saddle River, NJ, USA, 2018; ISBN 9780134792859. [Google Scholar]
- Hair, J.F.J.; Black, W.C.; Babin, B.J.; Anderson, R.E.; Black, W.C.; Anderson, R.E. Multivariate Data Analysis; Cengage: Boston, MA, USA, 2018; ISBN 9781473756540. [Google Scholar]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A New Criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef]

| Latent Factor | Variable Name | Statement in the Questionnaire | Literature Source |
|---|---|---|---|
| Perceived Usefulness | PU1_q3s1 | My work during a pandemic would be difficult without teleconsultations | Martínez et al., 2006 [80] Rimmer et al., 2020 [95] Bakken et al, 2006 [96] Rho et al., 2014 [7] Davis, 1989 [21] |
| PU2_q3s2 | Teleconsultations meet my needs at work | ||
| PU3_q3s3 | Teleconsultations increase the efficiency of my work | ||
| PU4_q3s4 | In general I find the teleconsultations a useful system in my work | ||
| PU5_q3s5 | teleconsultations save my time | ||
| PU6_q4s1 | Teleconsultations makes my work easier | ||
| Perceived Ease of Use | PEU1_q4s2 | Using a teleconsultations system is easy | Whitten et al., 2005 [97] Martínez et al., 2006 [80] Rimmer et al., 2020 [95] Bakken et al, 2006 [96] Zaidi et al., 2008 [77] Taylor, 2005 [78] Rho et al., 2014 [7] Davis, 1989 [21] |
| PEU2_q4s3 | Using a teleconsultations system does not require too much intellectual effort | ||
| PEU3_q4s4 | Using the teleconsultations system is understandable for me | ||
| PEU4_q4s5 | Using the teleconsultations system I can do everything I want | ||
| Image | IM1_q7s1 | People who use teleconsultations are more prestigious than those who do not use it | Holden, Karsh, 2010 [98] Chau, Hu, 2002 [60] Chismar, Wiley-Patton, 2002 [58] |
| IM2_q7s2 | People who use teleconsultations get noticed | ||
| IM3_q7s3 | Using teleconsultations is a status symbol | ||
| IM4_q7s4 | I compare myself with people who use teleconsultations | ||
| Needs to implement the telehealth system | NEC1_q7s5 | Teleconsultations is an acceptable method of delivering health services | Rho et. al., 2014 [7] Holden, Karsh, 2010 [98] Adewale, 2015 [99] |
| NEC2_q8s1 | Teleconsultations are needed in new situations, such as the COVID-19 pandemic | ||
| NEC3_q8s2 | Teleconsultations are needed regardless of emerging situations, such as COVID-19 | ||
| NEC4_q8s3 | Teleconsultations can partially replace in-person patient visits | ||
| NEC5_q8s4 | By being able to use teleconsultations, patients have easier access to healthcare | ||
| Decision autonomy | AUT2_q13s1 | I can influence the number of teleconsultations I take per day | Holden, Karsh, 2010 [98] Yi et.al., 2006 [100] Chau, Hu, 2002 [60] |
| AUT3_q13s2 | I can decide in which situation to use the teleconsultation | ||
| AUT4_q13s3 | I can decide how the teleconsultations will be done | ||
| Perception of Interaction with the Patient | SIM1_q11s1 | When talking to the patient, I understand what the patient’s problem is | Rho et al., 2014 [7] Holden, Karsh, 2010 [98] |
| SIM2_q11s2 | In conversation with the patient I can easily give advice | ||
| SIM3_q11s3 | I can easily talk to the patient during the teleconsultation | ||
| SIM4_q11s4 | I can understand the patient’s problem |
| Variable Name | Mean | Std. Deviation | Variance | Skewness | Kurtosis |
|---|---|---|---|---|---|
| PU1_q3s1 | 4.36 | 0.935 | 0.875 | −1.731 | 2.773 |
| PU2_q3s2 | 4.04 | 1.031 | 1.062 | −1.247 | 1.071 |
| PU3_q3s3 | 3.85 | 1.176 | 1.383 | −0.912 | −0.136 |
| PU4_q3s4 | 4.24 | 0.867 | 0.752 | −1.342 | 1.933 |
| PU5_q3s5 | 3.89 | 1.138 | 1.295 | −0.810 | −0.378 |
| PU6_q4s1 | 4.03 | 1.006 | 1.013 | −1.163 | 0.990 |
| IM1_q7s1 | 2.70 | 1.318 | 1.738 | 0.221 | −1.077 |
| IM2_q7s2 | 3.09 | 1.243 | 1.544 | −0.148 | −0.945 |
| IM3_q7s3 | 2.64 | 1.331 | 1.771 | 0.304 | −1.062 |
| IM4_q7s4 | 2.57 | 1.367 | 1.868 | 0.310 | −1.184 |
| SIM1_q11s1 | 3.98 | 0.925 | 0.855 | −1.143 | 1.017 |
| SIM2_q11s2 | 3.91 | 1.011 | 1.022 | −0.983 | 0.293 |
| SIM3_q11s3 | 3.81 | 1.050 | 1.103 | −0.731 | −0.434 |
| SIM4_q11s4 | 3.93 | 0.992 | 0.984 | −0.954 | 0.223 |
| PEU1_q4s2 | 4.28 | 0.834 | 0.695 | −1.338 | 1.885 |
| PEU2_q4s3 | 3.81 | 1.420 | 2.016 | −0.988 | −0.467 |
| PEU3_q4s4 | 4.51 | 0.671 | 0.451 | −1.819 | 5.271 |
| PEU4_q4s5 | 4.06 | 1.039 | 1.080 | −1.273 | 1.138 |
| AUT2_q13s1 | 4.05 | 1.009 | 1.017 | −1.189 | 0.907 |
| AUT3_q13s2 | 4.29 | 0.818 | 0.669 | −1.660 | 3.857 |
| AUT4_q13s3 | 4.35 | 0.756 | 0.572 | −1.646 | 4.272 |
| NEC1_q7s5 | 4.05 | 0.866 | 0.750 | −1.134 | 1.725 |
| NEC2_q8s1 | 4.59 | 0.631 | 0.399 | −1.864 | 5.056 |
| NEC3_q8s2 | 4.30 | 0.853 | 0.727 | −1.751 | 3.985 |
| NEC4_q8s3 | 4.11 | 0.925 | 0.857 | −1.454 | 2.321 |
| NEC5_q8s4 | 4.11 | 0.872 | 0.760 | −1.279 | 2.063 |
| Variable | Initial | Extraction |
|---|---|---|
| PU1_q3s1 | 1.000 | 0.546 |
| PU2_q3s2 | 1.000 | 0.721 |
| PU3_q3s3 | 1.000 | 0.809 |
| PU4_q3s4 | 1.000 | 0.789 |
| PU5_q3s5 | 1.000 | 0.707 |
| PU6_q4s1 | 1.000 | 0.638 |
| PEU1_q4s2 | 1.000 | 0.702 |
| PEU2_q4s3 | 1.000 | 0.604 |
| PEU3_q4s4 | 1.000 | 0.440 |
| PEU4_q4s5 | 1.000 | 0.664 |
| NEC1_q7s5 | 1.000 | 0.469 |
| NEC2_q8s1 | 1.000 | 0.643 |
| NEC3_q8s2 | 1.000 | 0.647 |
| NEC4_q8s3 | 1.000 | 0.674 |
| NEC5_q8s4 | 1.000 | 0.644 |
| IM1_q7s1 | 1.000 | 0.835 |
| IM2_q7s2 | 1.000 | 0.671 |
| IM3_q7s3 | 1.000 | 0.838 |
| IM4_q7s4 | 1.000 | 0.817 |
| AUT2_q13s1 | 1.000 | 0.755 |
| AUT3_q13s2 | 1.000 | 0.810 |
| AUT4_q13s3 | 1.000 | 0.760 |
| SIM1_q11s1 | 1.000 | 0.774 |
| SIM2_q11s2 | 1.000 | 0.757 |
| SIM3_q11s3 | 1.000 | 0.728 |
| SIM4_q11s4 | 1.000 | 0.755 |
| Component | Initial Eigenvalues | Extraction Sums of Squared Loadings | Rotation Sums of Squared Loadings | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | % of Variance | % Cumulative | Total | % of Variance | % Cumulative | Total | % of Variance | % Cumulative | |
| 1 | 8.887 | 34.181 | 34.181 | 8.887 | 34.181 | 34.181 | 3.707 | 14.257 | 14.257 |
| 2 | 2.506 | 9.639 | 43.820 | 2.506 | 9.639 | 43.820 | 3.451 | 13.272 | 27.529 |
| 3 | 2.224 | 8.555 | 52.374 | 2.224 | 8.555 | 52.374 | 3.297 | 12.681 | 40.210 |
| 4 | 1.871 | 7.196 | 59.570 | 1.871 | 7.196 | 59.570 | 3.099 | 11.917 | 52.127 |
| 5 | 1.583 | 6.088 | 65.658 | 1.583 | 6.088 | 65.658 | 2.323 | 8.933 | 61.060 |
| 6 | 1.125 | 4.327 | 69.985 | 1.125 | 4.327 | 69.985 | 2.320 | 8.925 | 69.985 |
| 7 | 0.804 | 3.092 | 73.078 | ||||||
| Variable | Component | |||||
|---|---|---|---|---|---|---|
| 1. PU | 2. SIM | 3. IM | 4. NEC | 5. AUT | 6. PEU | |
| Cronbach’s Alpha | 0.894 | 0.902 | 0.908 | 0.815 | 0.83 | 0.676 |
| PU1_q3s1 | 0.623 | |||||
| PU2_q3s2 | 0.720 | |||||
| PU3_q3s3 | 0.811 | |||||
| PU4_q3s4 | 0.733 | |||||
| PU5_q3s5 | 0.752 | |||||
| PU6_q4s1 | 0.628 | |||||
| PEU1_q4s2 | 0.807 | |||||
| PEU2_q4s3 | 0.670 | |||||
| PEU3_q4s4 | 0.592 | |||||
| PEU4_q4s5 | 0.696 | |||||
| NEC1_q7s5 | 0.545 | |||||
| NEC2_q8s1 | 0.760 | |||||
| NEC3_q8s2 | 0.727 | |||||
| NEC4_q8s3 | 0.765 | |||||
| NEC5_q8s4 | 0.659 | |||||
| IM1_q7s1 | 0.874 | |||||
| IM2_q7s2 | 0.757 | |||||
| IM3_q7s3 | 0.897 | |||||
| IM4_q7s4 | 0.879 | |||||
| AUT2_q13s1 | 0.811 | |||||
| AUT3_q13s2 | 0.848 | |||||
| AUT4_q13s3 | 0.781 | |||||
| SIM1_q11s1 | 0.827 | |||||
| SIM2_q11s2 | 0.800 | |||||
| SIM3_q11s3 | 0.775 | |||||
| SIM4_q11s4 | 0.822 | |||||
| Variable | CR | AVE | MSV | PU | SIM | IM | NEC | AUT | PEU | |
|---|---|---|---|---|---|---|---|---|---|---|
| Correlations | ||||||||||
| PU | 0.899 | 0.602 | 0.575 | 0.776 | 1 | |||||
| SIM | 0.904 | 0.701 | 0.277 | 0.837 | 0.526 | 1 | ||||
| IM | 0.909 | 0.717 | 0.180 | 0.847 | 0.424 | 0.304 | 1 | |||
| NEC | 0.823 | 0.484 | 0.575 | 0.696 | 0.758 | 0.454 | 0.363 | 1 | ||
| AUT | 0.847 | 0.650 | 0.209 | 0.806 | 0.436 | 0.457 | 0.206 | 0.417 | 1 | |
| PEU | 0.719 | 0.407 | 0.233 | 0.638 | 0.483 | 0.479 | 0.280 | 0.347 | 0.411 | 1 |
| PU | SIM | IM | NEC | AUT | PEU | |
|---|---|---|---|---|---|---|
| PU | ||||||
| SIM | 0.551 | |||||
| IM | 0.444 | 0.335 | ||||
| NEC | 0.762 | 0.468 | 0.383 | |||
| AUT | 0.450 | 0.455 | 0.241 | 0.448 | ||
| PEU | 0.466 | 0.419 | 0.290 | 0.323 | 0.440 |
| Hypothesis | Variables | Relation | Variables | Standardized Path Estimate | p-Value | Confirmation of the Hypotheses |
|---|---|---|---|---|---|---|
| H2 | PU | ← | PEU | 0.543 | <0.0001 | Supported |
| H3a | NEC | ← | IM | 0.036 | 0.268 | Not supported |
| H3b | NEC | ← | AUT | 0.111 | 0.002 | Supported |
| H1a | NEC | ← | PU | 0.791 | <0.0001 | Supported |
| H1b | NEC | ← | PEU | −0.108 | 0.004 | Supported |
| H3c | NEC | ← | SIM | 0.049 | 0.205 | Not supported |
| H1c | PEU | → PU → | NEC | 0.464 | 0.001 | Supported |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walczak, R.; Kludacz-Alessandri, M.; Hawrysz, L. Use of Telemedicine Technology among General Practitioners during COVID-19: A Modified Technology Acceptance Model Study in Poland. Int. J. Environ. Res. Public Health 2022, 19, 10937. https://doi.org/10.3390/ijerph191710937
Walczak R, Kludacz-Alessandri M, Hawrysz L. Use of Telemedicine Technology among General Practitioners during COVID-19: A Modified Technology Acceptance Model Study in Poland. International Journal of Environmental Research and Public Health. 2022; 19(17):10937. https://doi.org/10.3390/ijerph191710937
Chicago/Turabian StyleWalczak, Renata, Magdalena Kludacz-Alessandri, and Liliana Hawrysz. 2022. "Use of Telemedicine Technology among General Practitioners during COVID-19: A Modified Technology Acceptance Model Study in Poland" International Journal of Environmental Research and Public Health 19, no. 17: 10937. https://doi.org/10.3390/ijerph191710937
APA StyleWalczak, R., Kludacz-Alessandri, M., & Hawrysz, L. (2022). Use of Telemedicine Technology among General Practitioners during COVID-19: A Modified Technology Acceptance Model Study in Poland. International Journal of Environmental Research and Public Health, 19(17), 10937. https://doi.org/10.3390/ijerph191710937







