Risk of Mortality in Association with Pregnancy in Women Following Motor Vehicle Crashes: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Risk of Bias Assessment
2.4. Data Extraction
2.5. Data Analysis
3. Results
3.1. Characteristics of Included Studies
3.2. Risk of Bias
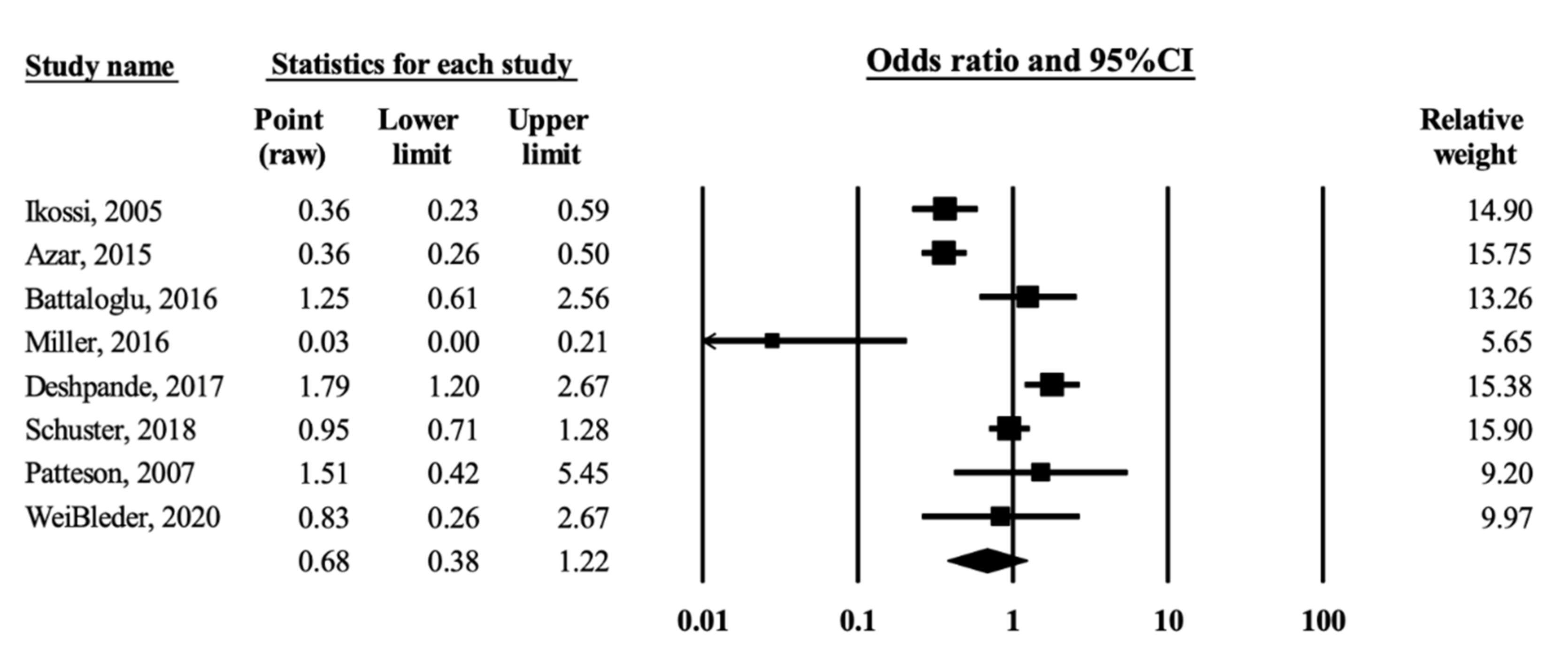
3.3. Overall Effects
3.4. Sensitivity Analysis
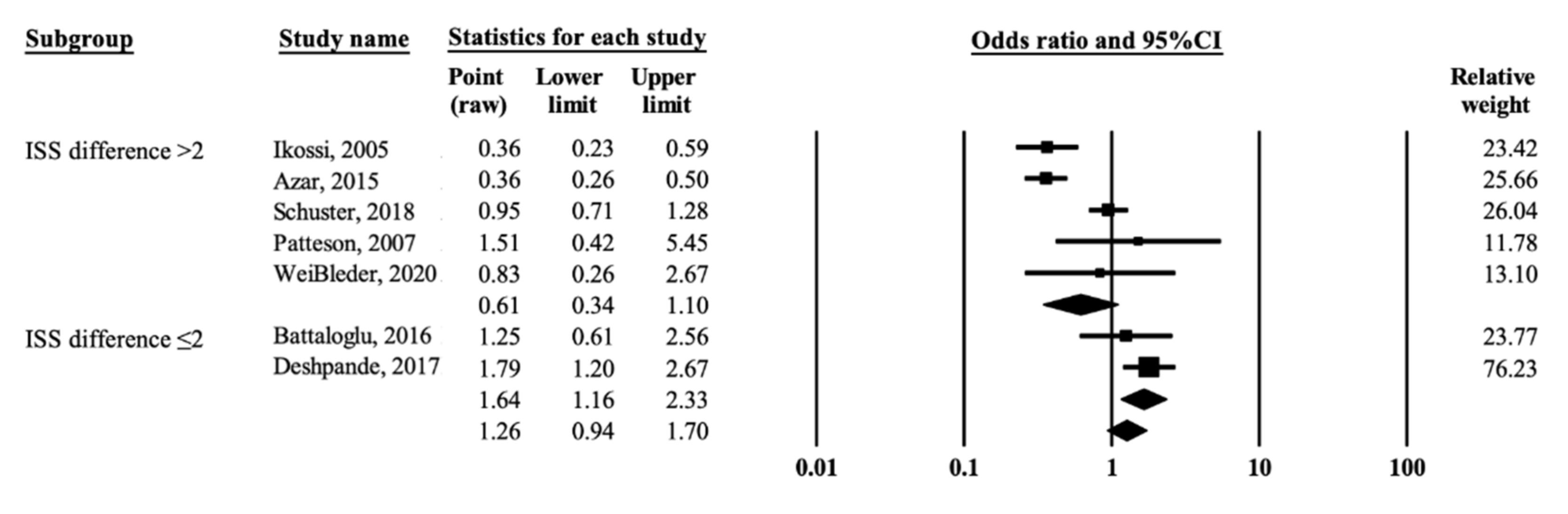
3.5. Subgroup Analysis
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Petrone, P.; Jiménez-Morillas, P.; Axelrad, A.; Marini, C.P. Traumatic injuries to the pregnant patient: A critical literature review. Eur. J. Trauma Emerg. Surg. 2019, 45, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, J.; Michels, C.; Eisfelder, B.; Joshi, N. Trauma in pregnancy. Emerg. Med. Clin. N. Am. 2019, 37, 317–338. [Google Scholar] [CrossRef] [PubMed]
- Schiff, M.A.; Holt, V.L. The injury severity score in pregnant trauma patients: Predicting placental abruption and fetal death. J. Trauma 2002, 53, 946–949. [Google Scholar] [CrossRef] [PubMed]
- Vladutiu, C.J.; Weiss, H.B. Motor vehicle safety during pregnancy. Am. J. Lifestyle Med. 2012, 6, 241–249. [Google Scholar] [CrossRef]
- Schuster, M.; Becker, N.; Young, A.; Paglia, M.J.; Mackeen, A.D. Trauma in pregnancy: A review of the Pennsylvania Trauma Systems Foundation database. Trauma 2018, 20, 30–37. [Google Scholar] [CrossRef] [Green Version]
- Deshpande, N.A.; Kucirka, L.M.; Smith, R.N.; Oxford, C.M. Pregnant trauma victims experience nearly 2-fold higher mortality compared to their nonpregnant counterparts. Am. J. Obstet. Gynecol. 2017, 217, 590.e1–590.e9. [Google Scholar] [CrossRef]
- Battaloglu, E.; McDonnell, D.; Chu, J.; Lecky, F.; Porter, K. Epidemiology and outcomes of pregnancy and obstetric complications in trauma in the United Kingdom. Injury 2016, 47, 184–187. [Google Scholar] [CrossRef]
- Miller, N.; Biron-Shental, T.; Peleg, K.; Fishman, A.; Olsha, O.; Givon, A.; Kessel, B. Are pregnant women safer in motor vehicle accidents? J. Perinat. Med. 2016, 44, 329–332. [Google Scholar] [CrossRef]
- Azar, T.; Longo, C.; Oddy, L.; Abenhaim, H.A. Motor vehicle collision-related accidents in pregnancy. J. Obstet. Gynaecol. Res. 2015, 41, 1370–1376. [Google Scholar] [CrossRef]
- Kvarnstrand, L.; Milsom, I.; Lekander, T.; Druid, H.; Jacobsson, B. Maternal fatalities, fetal and neonatal deaths related to motor vehicle crashes during pregnancy: A national population-based study. Acta Obstet. Gynecol. Scand. 2008, 87, 946–952. [Google Scholar] [CrossRef]
- Ikossi, D.G.; Lazar, A.A.; Morabito, D.; Fildes, J.; Knudson, M.M. Profile of mothers at risk: An analysis of injury and pregnancy loss in 1,195 trauma patients. J. Am. Coll. Surg. 2005, 200, 49–56. [Google Scholar] [CrossRef]
- Aboutanos, M.B.; Aboutanos, S.Z.; Dompkowski, D.; Duane, T.M.; Malhotra, A.K.; Ivatury, R.R. Significance of motor vehicle crashes and pelvic injury on fetal mortality: A five-year insititutional review. J. Trauma 2008, 65, 616–620. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses [Article Online]. Ottawa Hospital Research Institute Web site. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 13 April 2021).
- Sobhy, S.; Babiker, Z.; Zamora, J.; Khan, K.; Kunst, H. Maternal and perinatal mortality and morbidity associated with tuberculosis during pregnancy and the postpartum period: A systematic review and meta-analysis. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 727–733. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G. Chapter 10: Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated 2021); Higgins, J.P.T., Green, S., Eds.; The Cochrane Collaboration: Chichester, UK, 2021; Available online: https://training.cochrane.org/handbook/current/chapter-10 (accessed on 13 April 2021).
- Patteson, S.K.; Snider, C.C.; Meyer, D.S.; Enderson, B.L.; Armstrong, J.E.; Whitaker, G.L.; Carroll, R.C. The consequences of high-risk behaviors: Trauma during pregnancy. J. Trauma Acute Care Surg. 2007, 62, 1015–1020. [Google Scholar] [CrossRef]
- Weißleder, A.; Kulla, M.; Annecke, T.; Beese, A.; Lang, P. Akutbehandlung schwangerer Patientinnen nach schwerem trauma—eine retrospektive multicenteranalyse. Der Unf. 2020, 123, 944–953. (In German) [Google Scholar] [CrossRef]
- Rodriguez, A.; Bohlin, G.; Lindmark, G. Symptoms across pregnancy in relation to psychosocial and biomedical factors. Acta Obstet. Gynecol. Scand. 2001, 80, 213–223. [Google Scholar] [CrossRef]
- Taylor, A.H.; Dorn, L. Stress, fatigue, health, and risk of road traffic accidents among professional drivers: The contribution of physical inactivity. Annu. Rev. Public Health 2006, 27, 371–391. [Google Scholar] [CrossRef] [Green Version]
- McCall, S.J.; Bhattacharya, S. High risk of traffic crashes in pregnancy: Are there any explanations? Can. Med Assoc. J. 2014, 186, 733–734. [Google Scholar] [CrossRef] [Green Version]
- Esposito, T.J. Trauma during pregnancy. Emerg. Med. Clin. N. Am. 1994, 12, 167–199. [Google Scholar] [CrossRef]
- Shah, K.H.; Simons, R.K.; Holbrook, T.; Fortlage, D.; Winchell, R.J.; Hoyt, D.B. Trauma in pregnancy: Maternal and fetal outcomes. J. Trauma 1998, 45, 83–86. [Google Scholar] [CrossRef]
- Haut, E.R.; Pronovost, P.J. Surveillance bias in outcomes reporting. JAMA 2011, 305, 2462–2463. [Google Scholar] [CrossRef]
- Weiss, H.B.; Strotmeyer, S. Characteristics of pregnant women in motor vehicle crashes. Inj. Prev. 2002, 8, 207–210. [Google Scholar] [CrossRef]
- Baker, S.P.; O’Neill, B.; Haddon, W.; Long, W.B. The injury severity score: A method for describing patients with multiple injures and evaluating emergency care. J. Trauma 1974, 14, 187–196. [Google Scholar] [CrossRef]
- Baerga-Varela, Y.; Zietlow, S.P.; Bannon, M.P.; Harmsen, W.S.; Ilstrup, D.M. Trauma in pregnancy. Mayo Clin. Proc. 2000, 75, 1243–1248. [Google Scholar] [CrossRef]
- Schiff, M.A.; Holt, V.L. Pregnancy outcomes following hospitalization for motor vehicle crashes in Washington state from 1989 to 2001. Am. J. Epidemiol. 2005, 161, 503–510. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, W65–W94. [Google Scholar] [CrossRef] [Green Version]
- Wolf, M.E.; Alexander, B.H.; Rivara, F.P.; Hickok, D.E.; Maier, R.V.; Starzyk, P.M. A retrospective cohort study of seatbelt use and pregnancy outcome after a motor vehicle crash. J. Trauma 1993, 34, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Xiong, L.; Li, L. Single-vehicle and multi-vehicle accidents involving motorcycles in a small city in China: Characteristics and injury patterns. AIMS Public Health 2015, 2, 75–85. [Google Scholar] [CrossRef]
- Distelhorst, J.T.; Krishnamoorthy, V.; Schiff, M.A. Association between hospital trauma designation and maternal and neonatal outcomes after injury among pregnant women in Washington State. J. Am. Coll. Surg. 2016, 222, 296–302. [Google Scholar] [CrossRef]

| Author, Year of Publication, Country | Study Design | Study Duration | Data Source | Study Participants Injured in MVCs (%) | Age Range (Years) | Potential Confounders Considered | |
|---|---|---|---|---|---|---|---|
| Pregnant | Nonpregnant | ||||||
| Ikossi et al. [11] 2005, US | Retrospective study | 1994–2001 | Multiple centers (130 trauma centers), National Trauma Data Bank | 70.4 | 54.7 | 12–51 | Mean age, mortality, mean ISS, mean LOS, SBP < 90, alcohol consumption, drug use, seatbelt use |
| Patteson et al. [17] 2007, US | Matched retrospective cohort study | 1996–2004 | Trauma registry at level I regional trauma center | 85.1 | NA | No restriction but age and time frame matched | Revised Trauma Score, admission to OR/ICU |
| Azar et al. [9] 2015, US | Matched retrospective cohort study | 2003–2011 | Multiple centers, national inpatient sample database | 100.0 | 100.0 | No restriction but age matched | Age, race, income, type of insurance, type of hospital, type of vehicle (motor vehicle, motorcycle, pedestrian), |
| Battaloglu et al. [7] 2016, UK | Retrospective review | 2009–2014 | National trauma registry | 55.5 | 36.4 | 15–50 (with age matched) | ISS, AIS, blood transfusion |
| Miller et al. [8] 2016, Israel | Retrospective cohort study | 2006–2013 | National trauma registry | 100.0 | 100.0 | 18–40 | ISS |
| Deshpande et al. [6] 2017, US (Pennsylvania) | Retrospective cohort study | 2005–2015 | Pennsylvania Trauma Outcome Study | 58.1 | 52.8 | 14–49 | Age, race, Hispanic ethnicity, insurance type, comorbidities, GCS score, SBP, dead on arrival, ISS, injury mechanism, transferred to OR, intubated, required ICU admission, transfused, discharge category |
| Schuster et al. [5] 2018, US(Pennsylvania) | Matched retrospective cohort study | 1999–2013 | Pennsylvania Trauma System Foundation’s (PTSF) database | 60.0 | 62.0 | No restriction but age- and injury type- matched | Race, positive for drug screening, positive for alcohol screening, SBP, pulse, respiratory rate, GCS score, ISS, protective device, intubation, number of hospital days, surgical procedure performed |
| Weißleder et al. [18] 2020, Germany, Austria, and Switzerland | Retrospective data | 2016–2018 | Multiple centers Trauma Registry TR-DGU | 60.0 | 47.0 | 16–45 | ISS, AIS, Pre-hospital measure: intubation, respiratory aids, infusion therapy, infusion volume (mL), catecholamine therapy, chest drain, analgesic sedation, tranexamic acid, imaging procedure, intensive care, invasive ventilation; ICU length of stay, ventilation duration, complications |
| Study ID | Country | Number of Participants | Number of Deaths | Odds Ratio (95% CI) | Mean ISS | Difference in Mean ISS (ISSD) between Groups | |||
|---|---|---|---|---|---|---|---|---|---|
| Pregnant | Nonpregnant | Pregnant | Nonpregnant | Pregnant | Nonpregnant | ||||
| Ikossi et al. [11] | US | 1195 | 76,126 | 17 | 2893 | 0.37 (0.23–0.59) 1 | 6.1 | 9.7 | 3.6 |
| Patteson et al. [17] | US | 188 | 188 | 6 | 4 | 1.52 (0.42–5.46) 1 | NA | NA | >2 |
| Azar et al. [9] | US | 5936 | 59,360 | 39 | 1127 | 0.36 (0.26–0.50) 2 | NA | NA | >2 |
| Battaloglu et al. [7] | UK | 158 | 14,082 | 8 | 576 | 1.25 (0.61–2.56) 1 | 11.7 † | 11.5 † | 0.2 |
| Miller et al. [8] | Israel | 3794 | 3441 | 1 | 32 | 0.03 (0.00–0.21) 1 | 1.4 † | 6.9 † | 5.4 |
| Deshpande et al. [6] | US, Pennsylvania | 1148 | 43,608 | 22 | 790 | 1.79 (1.20–2.67) 3 | 9.0 | 10.9 | 1.9 |
| Schuster et al. [5] | US, Pennsylvania | 1599 | 7995 | 54 | 284 | 0.95 (0.71–1.28) 1 | 5 | 9 | 4 |
| Weißleder et al. [18] | Germany, Austria and Switzerland | 102 | 3135 | 3 | 110 | 0.83 (0.26–2.67) 1 | 10.7 | 14.3 | 3.6 |
| Total | 14,120 | 207,935 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.-H.; Cheng, Y.-Y.; Hou, W.-H.; Chien, Y.-W.; Chang, C.-H.; Chen, P.-L.; Lu, T.-H.; Yovita Hendrati, L.; Li, C.-Y.; Foo, N.-P. Risk of Mortality in Association with Pregnancy in Women Following Motor Vehicle Crashes: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 911. https://doi.org/10.3390/ijerph19020911
Chang Y-H, Cheng Y-Y, Hou W-H, Chien Y-W, Chang C-H, Chen P-L, Lu T-H, Yovita Hendrati L, Li C-Y, Foo N-P. Risk of Mortality in Association with Pregnancy in Women Following Motor Vehicle Crashes: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(2):911. https://doi.org/10.3390/ijerph19020911
Chicago/Turabian StyleChang, Ya-Hui, Ya-Yun Cheng, Wen-Hsuan Hou, Yu-Wen Chien, Chiung-Hsin Chang, Ping-Ling Chen, Tsung-Hsueh Lu, Lucia Yovita Hendrati, Chung-Yi Li, and Ning-Ping Foo. 2022. "Risk of Mortality in Association with Pregnancy in Women Following Motor Vehicle Crashes: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 2: 911. https://doi.org/10.3390/ijerph19020911
APA StyleChang, Y.-H., Cheng, Y.-Y., Hou, W.-H., Chien, Y.-W., Chang, C.-H., Chen, P.-L., Lu, T.-H., Yovita Hendrati, L., Li, C.-Y., & Foo, N.-P. (2022). Risk of Mortality in Association with Pregnancy in Women Following Motor Vehicle Crashes: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(2), 911. https://doi.org/10.3390/ijerph19020911








