Developing a Personalized Integrative Obesity-Coaching Program: A Systems Health Perspective
Abstract
1. Introduction
2. Materials and Methods
2.1. Theoretical Approach: Systems Health
2.2. Intervention Design and Participants
3. Results
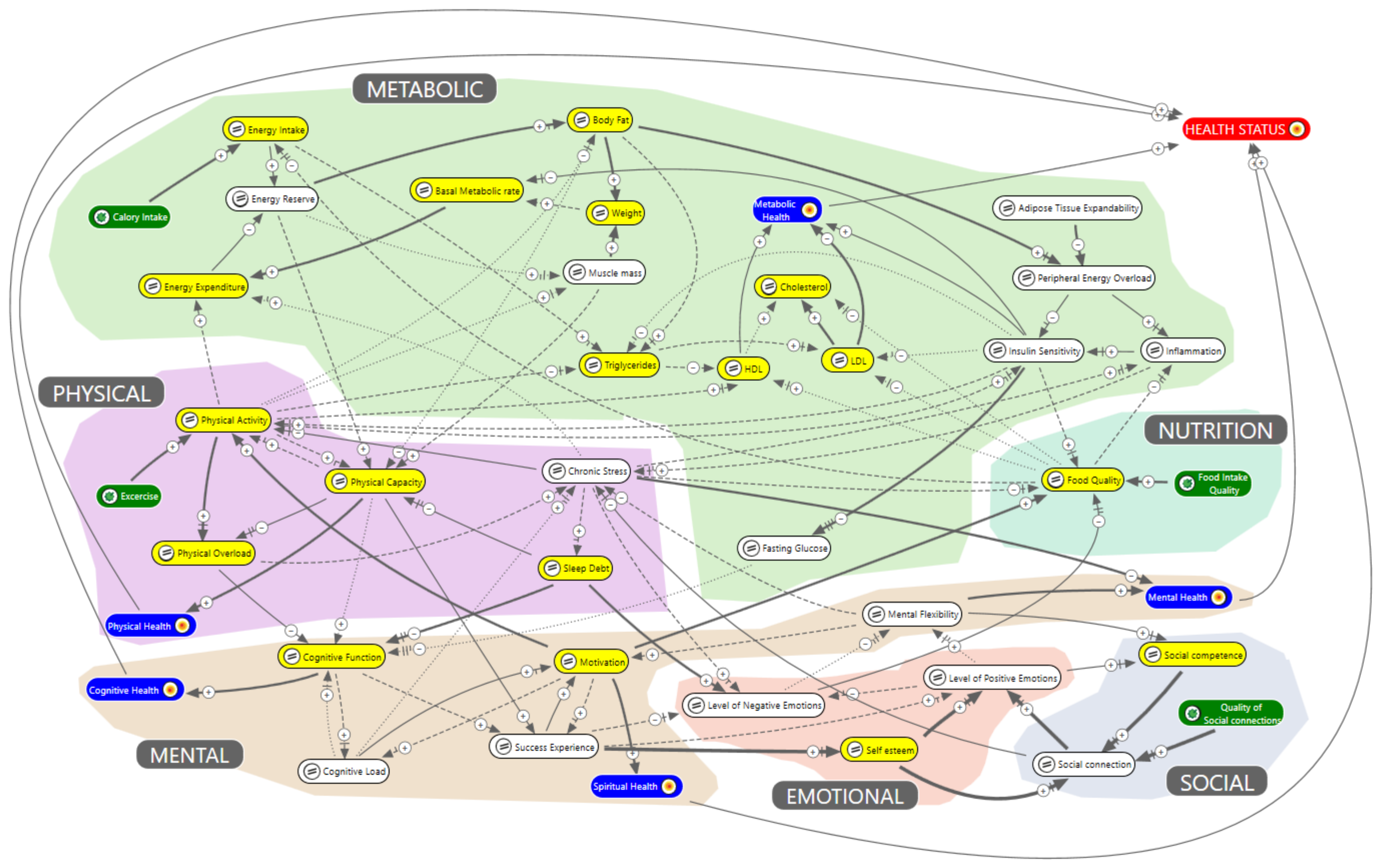
3.1. Systems Health Model of Obesity
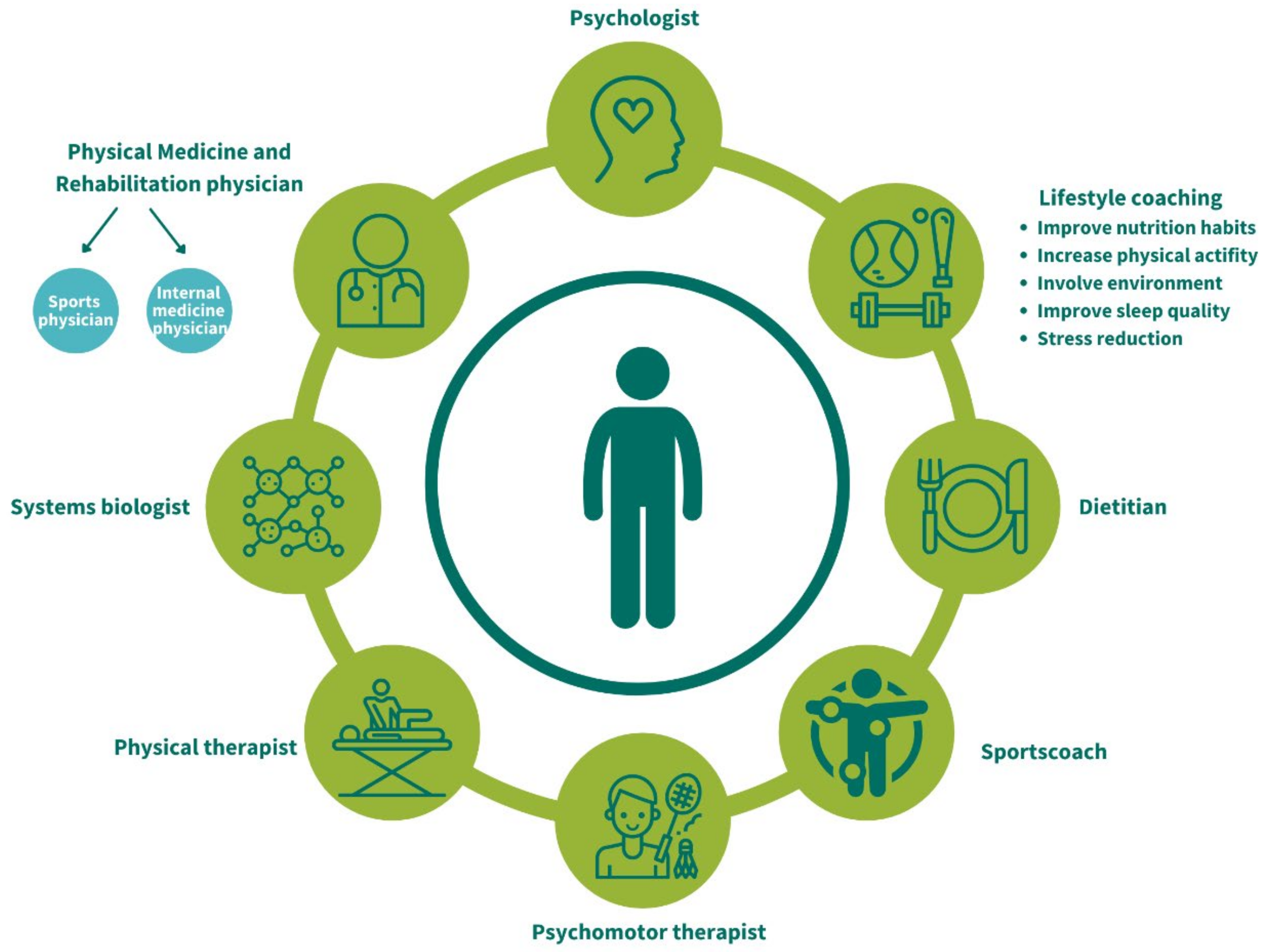
3.2. Organizational Structure of the Personalized Integrative Obesity-Coaching Program
3.3. Conditions for Participating in the Program
3.4. Ethics and Informed Consent
3.5. The Contents of the Personalized Integrative Obesity-Coaching Program
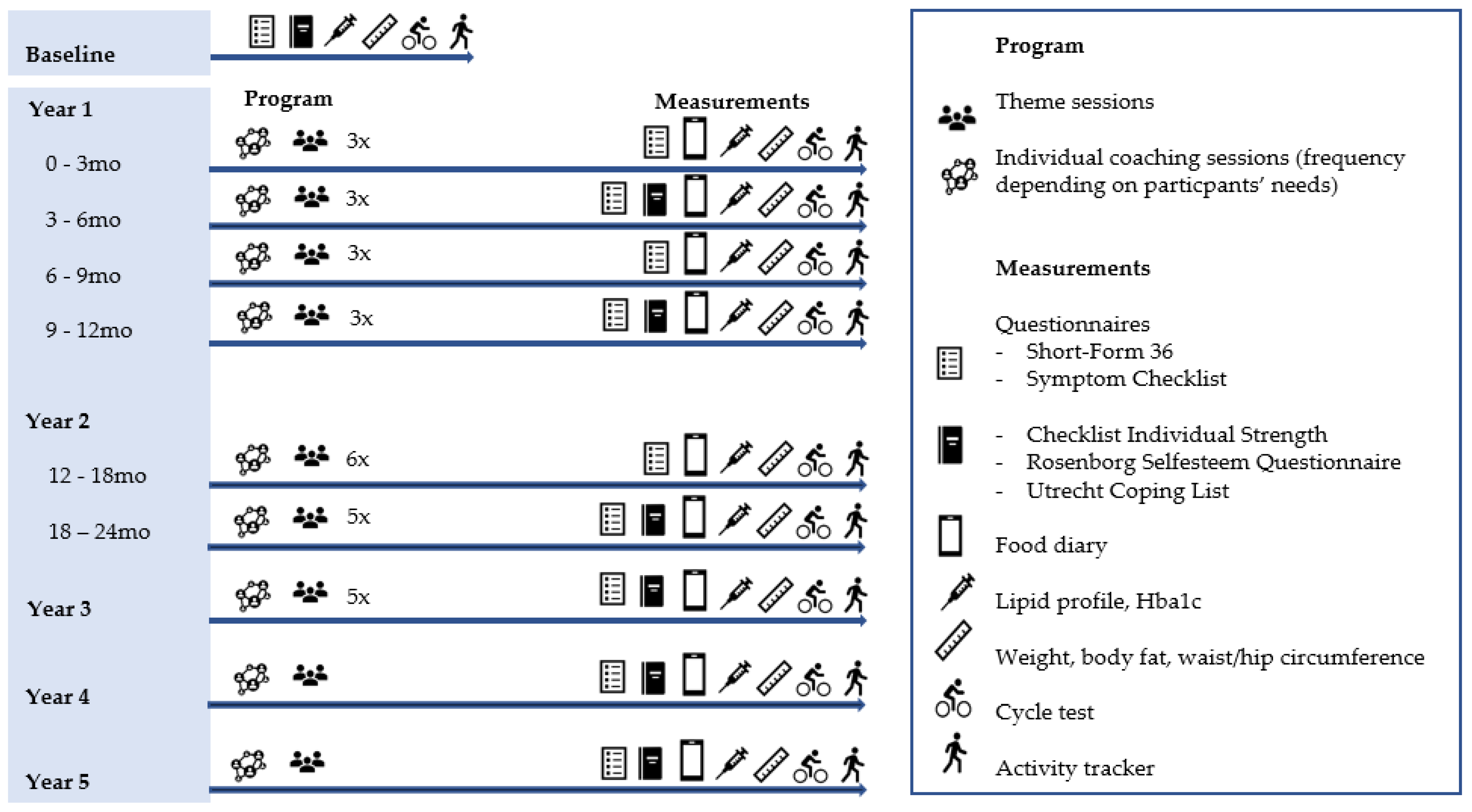
3.6. Monitoring Plan
3.7. Evaluation and Analysis
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 22 April 2021).
- Stefan, N.; Birkenfeld, A.L.; Schulze, M.B. Global pandemics interconnected—Obesity, impaired metabolic health and COVID-19. Nat. Rev. Endocrinol. 2021, 17, 135–149. [Google Scholar] [CrossRef] [PubMed]
- Volksgezondheidenzorg.info. Available online: https://www.volksgezondheidenzorg.info/onderwerp/overgewicht/cijfers-context/huidige-situatie (accessed on 21 April 2021).
- Volksgezondheid Toekomst Verkenning. 2018. Available online: https://www.vtv2018.nl/leefstijl (accessed on 21 April 2021).
- Hruby, A.; Manson, J.E.; Qi, L.; Malik, V.S.; Rimm, E.B.; Sun, Q.; Willett, W.C.; Hu, F.B. Determinants and Consequences of Obesity. Am. J. Public Health 2016, 106, 1656–1662. [Google Scholar] [CrossRef] [PubMed]
- Tuomilehto, J.; Lindström, J.; Eriksson, J.G.; Valle, T.T.; Hämäläinen, H.; Ilanne-Parikka, P.; Keinänen-Kiukaanniemi, S.; Laakso, M.; Louheranta, A.; Rastas, M.; et al. Finnish Diabetes Prevention Study Group Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 2001, 344, 1343–1350. [Google Scholar] [CrossRef] [PubMed]
- Van der Valk, E.S.; van den Akker, E.L.T.; Savas, M.; Kleinendorst, L.; Visser, J.A.; Van Haelst, M.M.; Sharma, A.M.; van Rossum, E.F.C. A comprehensive diagnostic approach to detect underlying causes of obesity in adults. Obes. Rev. 2019, 20, 795–804. [Google Scholar] [CrossRef] [PubMed]
- Del Busto, S.; Galindo, I.; Hernandez, J.J.; Camarelles, F.; Nieto, E.; Caballero, Á; Sandín Vázquez, M. Creating a Collaborative Platform for the Development of Community Interventions to Prevent Non-Communicable Diseases. Int. J. Environ. Res. Public Health 2019, 16, 676. [Google Scholar] [CrossRef]
- Burgess, E.; Hassmén, P.; Pumpa, K.L. Determinants of adherence to lifestyle intervention in adults with obesity: A systematic review. Clin. Obes. 2017, 7, 123–135. [Google Scholar] [CrossRef]
- Collins, C.E.; Morgan, P.J.; Jones, P.; Fletcher, K.; Martin, J.; Aguiar, E.J.; Lucas, A.; Neve, M.J.; Callister, R. A 12-week commercial web-based weight-loss program for overweight and obese adults: Randomized controlled trial comparing basic versus enhanced features. J. Med. Internet Res. 2012, 14, e57. [Google Scholar] [CrossRef]
- Thomson, M.; Martin, A.; Logue, J.; Wells, V.; Simpson, S.A. Barriers and facilitators of successful weight loss during participation in behavioural weight management programmes: A protocol for a systematic review. Syst Rev. 2020, 9, 168. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O.; Wyatt, H.R.; Reed, G.W.; Peters, J.C. Obesity and the environment: Where do we go from here? Science 2003, 299, 853–855. [Google Scholar] [CrossRef]
- Hall, K.D.; Heymsfield, S.B.; Kemnitz, J.W.; Klein, S.; Schoeller, D.A.; Speakman, J.R. Energy balance and its components: Implications for body weight regulation. Am. J. Clin. Nutr. 2012, 95, 989–994. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. Lancet 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Oussaada, S.M.; van Galen, K.A.; Cooiman, M.I.; Kleinendorst, L.; Hazebroek, E.J.; van Haelst, M.M.; Ter Horst, K.W.; Serlie, M.J. The pathogenesis of obesity. Metabolism 2019, 92, 26–36. [Google Scholar] [CrossRef]
- Van Wietmarschen, H.A.; Dai, W.; van der Kooij, A.J.; Reijmers, T.H.; Schroën, Y.; Wang, M.; Xu, Z.; Wang, X.; Kong, H.; Xu, G.; et al. Characterization of rheumatoid arthritis subtypes using symptom profiles, clinical chemistry and metabolomics measurements. PLoS ONE 2012, 7, e44331. [Google Scholar] [CrossRef]
- Waterlander, W.E.; Luna Pinzon, A.; Verhoeff, A.; den Hertog, K.; Altenburg, T.; Dijkstra, C.; Halberstadt, J.; Hermans, R.; Renders, C.; Seidell, J.; et al. A System Dynamics and Participatory Action Research Approach to Promote Healthy Living and a Healthy Weight among 10–14-Year-Old Adolescents in Amsterdam: The LIKE Programme. Int. J. Environ. Res. Public Health 2020, 17, 4928. [Google Scholar] [CrossRef] [PubMed]
- Van Wietmarschen, H.A.; Wortelboer, H.M.; van der Greef, J. Grip on health: A complex systems approach to transform health care. J. Eval. Clin. Pract. 2018, 24, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Veldhuis, G.A.; Sluijs, T.; van Zwieten, M.H.J.; Bouwman, J.; Wiezer, N.M.; Wortelboer, H.M. A Proof-of-Concept System Dynamics Simulation Model of the Development of Burnout and Recovery Using Retrospective Case Data. Int. J. Environ. Res. Public Health 2020, 17, 5964. [Google Scholar] [CrossRef] [PubMed]
- Sterling, P. Allostasis: A model of predictive regulation. Physiol. Behav. 2012, 106, 5–15. [Google Scholar] [CrossRef]
- Pincus, D.G.S. Complexity science in the future of behavioural medicine. In Handbook of Systems and Complexity in Health; Sturmberg, J.P., Martin, C.M., Eds.; Springer: New York, NY, USA, 2013; pp. 889–909. [Google Scholar]
- Coyle, G. Qualitative and quantitative modelling in system dynamics: Some research questions. Syst. Dyn. Rev. 2000, 16, 225–244. [Google Scholar] [CrossRef]
- Van der Greef, J.; van Wietmarschen, H.; Schroën, J.; Wang, M.; Hankemeier, T.; Xu, G. Systems biology-based diagnostic principles as pillars of the bridge between Chinese and Western medicine. Planta Med. 2010, 76, 2036–2047. [Google Scholar] [CrossRef]
- Van Wietmarschen, H.; Yuan, K.; Lu, C.; Gao, P.; Wang, J.; Xiao, C.; Yan, X.; Wang, M.; Schroën, J.; Lu, A.; et al. Systems biology guided by Chinese medicine reveals new markers for sub-typing rheumatoid arthritis patients. J. Clin. Rheumatol 2009, 15, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.; Pasman, W.; Rubingh, C.; Wopereis, S.; Tienstra, M.; Schroen, J.; Wang, M.; Verheij, E.; van der Greef, J. Urine metabolomics combined with the personalized diagnosis guided by Chinese medicine reveals subtypes of pre-diabetes. Mol. Biosyst. 2012, 8, 1482–1491. [Google Scholar] [CrossRef]
- Maciocia, G. The Foundations of Chinese Medicine: A Comprehensive Text for Acupuncturists and Herbalists, 2nd ed.; Elsevier Churchill Livingstone: Philadelphia, PA, USA, 2005. [Google Scholar]
- Kastner, J. Chinese Nutrition Therapy. Dietetics in Traditional Chinese Medicine (TCM), 2nd ed.; Thieme: Zutphen, The Netherlands, 2011. [Google Scholar]
- Sterman, J.D. Business Dynamics: Systems Thinking and Modeling for a Complex World; Mcgraw-Hill Education: New York, NY, USA, 2000. [Google Scholar]
- Wang, J.Y.; Glover, W.J.; Rhodes, A.M.; Nightingale, D. A conceptual model of the psychological health system for U.S. active duty service members: An approach to inform leadership and policy decision making. Mil. Med. 2013, 178, 596–606. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.; Ross, W.; Ulieru, M. A System Dynamics View of Stress: Towards Human-Factor Modeling with Computer Agents. In Proceedings of the IEEE International Conference on Systems, Man and Cybernetics, Istanbul, Turkey, 10–13 October 2010; pp. 4369–4374. [Google Scholar]
- Veldhuis, G.A.; van Scheepstal, P.; Rouwette, E.; Logtens, T. Collaborative problem structuring using MARVEL. EURO J. Decis. Processes 2015, 3, 249–273. [Google Scholar] [CrossRef]
- Kwaliteitsinstituut voor de Gezondheidszorg CBO. Diagnostiek en Behandeling van Obesitas Bij Volwassenen en Kinderen; Van Zuiden Communications BV: Utrecht, The Netherlands, 2008. [Google Scholar]
- Partnerschap Overgewicht Nederland. Zorgstandaard Obesitas; Partnerschap Overgewicht Nederland: Amsterdam, The Netherlands, 2010. [Google Scholar]
- Winzer, E.; Dorner, T.E.; Grabovac, I.; Haider, S.; Kapan, A.; Lackinger, C.; Schindler, K. Behavior changes by a buddy-style intervention including physical training, and nutritional and social support. Geriatr. Gerontol. Int. 2019, 19, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Golay, A.; Brock, E.; Gabriel, R.; Konrad, T.; Lalic, N.; Laville, M.; Mingrone, G.; Petrie, J.; Phan, T.M.; Pietiläinen, K.H.; et al. Taking small steps towards targets—Perspectives for clinical practice in diabetes, cardiometabolic disorders and beyond. Int. J. Clin. Pract. 2013, 67, 322–332. [Google Scholar] [CrossRef]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation. Available online: https://www.who.int/publications/i/item/9789241501491 (accessed on 29 April 2021).
- Macsween, A. The reliability and validity of the Astrand nomogram and linear extrapolation for deriving VO2max from submaximal exercise data. J. Sports Med. Phys. Fitness 2001, 41, 312–317. [Google Scholar]
- Vercoulen, J.H.; Swanink, C.M.; Fennis, J.F.; Galama, J.M.; van der Meer, J.W.; Bleijenberg, G. Dimensional assessment of chronic fatigue syndrome. J. Psychosom. Res. 1994, 38, 383–392. [Google Scholar] [CrossRef]
- Everaert, J.; Koster, E.; Schacht, R.; De Raedt, R. Evaluatie van de psychometrische eigenschappen van de Rosenberg zelfwaardeschaal in een poliklinisch psychiatrische populatie. Gedragstherapie 2010, 43, 307–317. [Google Scholar]
- Schreurs, P.J.G.; Tellegen, B.; van de Willige, G. Gezondheid, stress en coping: De ontwikkeling van de Utrechtse Coping Lijst. Gedrag Tijdschrift voor Psychologie 1984, 12, 101–117. [Google Scholar]
- De Haes, J.C.; van Knippenberg, F.C.; Neijt, J.P. Measuring psychological and physical distress in cancer patients: Structure and application of the Rotterdam Symptom Checklist. Br. J. Cancer 1990, 62, 1034–1038. [Google Scholar] [CrossRef] [PubMed]
- VanderZee, K.I.; Sanderman, R.; Heyink, J.W.; de Haes, H. Psychometric qualities of the RAND 36-Item Health Survey 1.0: A multidimensional measure of general health status. Int. J. Behav. Med. 1996, 3, 104–122. [Google Scholar] [CrossRef] [PubMed]
- Bagnall, A.M.; Radley, D.; Jones, R.; Gately, P.; Nobles, J.; Van Dijk, M.; Blackshaw, J.; Montel, S.; Sahota, P. Whole systems approaches to obesity and other complex public health challenges: A systematic review. BMC Public Health 2019, 19, 8-z. [Google Scholar] [CrossRef]
- Van Rinsum, C.; Gerards, S.; Rutten, G.; Philippens, N.; Janssen, E.; Winkens, B.; van de Goor, I.; Kremers, S. The Coaching on Lifestyle (CooL) Intervention for Overweight and Obesity: A Longitudinal Study into Participants’ Lifestyle Changes. Int. J. Environ. Res. Public Health 2018, 15, 680. [Google Scholar] [CrossRef] [PubMed]
- Schutte, B.A.; Haveman-Nies, A.; Preller, L. One-Year Results of the BeweegKuur Lifestyle Intervention Implemented in Dutch Primary Healthcare Settings. Biomed. Res. Int. 2015, 2015, 484823. [Google Scholar] [CrossRef][Green Version]
- Duijzer, G.; Haveman-Nies, A.; Jansen, S.C.; ter Beek, J.; Hiddink, G.J.; Feskens, E.J. SLIMMER: A randomised controlled trial of diabetes prevention in Dutch primary health care: Design and methods for process, effect, and economic evaluation. BMC Public Health 2014, 14, 602. [Google Scholar] [CrossRef] [PubMed]
- Pot, G.K.; Battjes-Fries, M.C.; Patijn, O.N.; Pijl, H.; Witkamp, R.F.; de Visser, M.; van der Zijl, N.; de Vries, M.; Voshol, P.J. Nutrition and lifestyle intervention in type 2 diabetes: Pilot study in The Netherlands showing improved glucose control and reduction in glucose lowering medication. BMJ Nutr. Prev. Health 2019, 2, 43–50. [Google Scholar] [CrossRef]
| Characteristics | |||
|---|---|---|---|
| Subtype | Physical | Mental | Nutritional/Metabolism |
| I Spleen Deficiency with Damp | Weak fat tissue in front of the abdominal muscles; low muscle mass, having fatigue/drowsiness; unpleasant feeling in the chest and/or stomach area; sweating easily. | Gets worried quickly; foresees a number of problems. | Likes sweet food; limited appetite; does not feel thirsty; difficult digestion. |
| II Stomach Yin Deficiency | The same as subtype 1 combined with reflux. | The same as subtype 1 combined with an increased arousal. | Having a constant need to eat; difficult digestion. |
| III Damp Heat and Qi Stagnation | Solid muscle mass; excessive weight, particularly in the abdominal area; chest breathing; often having musculoskeletal disorders. | Dreamy; irritated easily; struggles with setting personal boundaries. | Thirsty; overeating; constipation. |
| IV Yin Deficiency | Accumulation of fat in the abdominal area and buttocks; tired, edema in lower extremity; aversion to cold; sometimes thyroid disorders. | Anxious; difficulty with recognizing personal boundaries; reduced body awareness. | Often eating normal amounts; sometimes poor appetite; irregular defecation. |
| V Liver Qi Stagnation | Looking bloated; accumulation of fat in the abdominal area; has little energy; increased stress hormones; vertigo. | Having a tendency to rationalize; think and worry; likes to be in control; urge to prove. | Eating quickly; dry mouth; reduced appetite; cramping feeling in abdomen; reflux; nausea. |
| Health Domain | Measurements |
|---|---|
| Metabolic | Lipid profile, HbA1c, weight, body (visceral-) fat%, waist/hip circumference [37] |
| Physical | Maximal aerobic capacity [38], activity tracker |
| Mental | Checklist Individual Strength (CIS) [39] |
| Emotional | Rosenberg self-esteem scale (RSE) [40] |
| Social | Utrecht Coping List (UCL) [41] |
| Broad spectrum health measures | Symptom checklist (SCL-90) [42], Short Form 36 (SF-36) [43] |
| Nutrition | Food diary app ‘mijneetmeter.nl’ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brink, S.M.; Wortelboer, H.M.; Emmelot, C.H.; Visscher, T.L.S.; van Wietmarschen, H.A. Developing a Personalized Integrative Obesity-Coaching Program: A Systems Health Perspective. Int. J. Environ. Res. Public Health 2022, 19, 882. https://doi.org/10.3390/ijerph19020882
Brink SM, Wortelboer HM, Emmelot CH, Visscher TLS, van Wietmarschen HA. Developing a Personalized Integrative Obesity-Coaching Program: A Systems Health Perspective. International Journal of Environmental Research and Public Health. 2022; 19(2):882. https://doi.org/10.3390/ijerph19020882
Chicago/Turabian StyleBrink, Sander M., Heleen M. Wortelboer, Cornelis H. Emmelot, Tommy L. S. Visscher, and Herman A. van Wietmarschen. 2022. "Developing a Personalized Integrative Obesity-Coaching Program: A Systems Health Perspective" International Journal of Environmental Research and Public Health 19, no. 2: 882. https://doi.org/10.3390/ijerph19020882
APA StyleBrink, S. M., Wortelboer, H. M., Emmelot, C. H., Visscher, T. L. S., & van Wietmarschen, H. A. (2022). Developing a Personalized Integrative Obesity-Coaching Program: A Systems Health Perspective. International Journal of Environmental Research and Public Health, 19(2), 882. https://doi.org/10.3390/ijerph19020882






