Abstract
Patients on hemodialysis with multiple comorbidities have limited physical activity, resulting in poor health, low activity participation, and low quality of life. Accordingly, the nursing care provided to such patients should include regular physical activity training programs. Therefore, this cross-sectional descriptive study investigated whether patients on hemodialysis with and without comorbidities have different levels of physical activity and health-related quality of life (HRQoL); the correlations among the comorbidities, physical activity, and HRQoL of the two cohorts were also assessed. The 36-Item Short-Form Health Survey version 2 and International Physical Activity Questionnaire were employed to collect data from 120 patients on hemodialysis. An independent samples t-test and univariate and multivariate linear regression analyses were conducted. The overall HRQoL of patients with comorbidities was lower than that of patients without comorbidities (p = 0.008). Compared with patients who participated in low-intensity physical activity, the overall HRQoL of patients who participated in moderate-intensity physical activity was higher (p < 0.001). The overall HRQoL of patients with comorbidities who participated in low-intensity physical activity was lower than that of those who participated in moderate-intensity physical activity (p < 0.001). Moderate-intensity physical activity was correlated with higher HRQoL for patients with comorbidities. This finding supports the implementation of effective physical activity intervention measures. Furthermore, it supports the promotion of patient self-management and the implementation of regular exercise programs and lifestyle changes, and patients on hemodialysis can benefit from the future management of physical activities.
1. Introduction
The most common comorbidities of patients on hemodialysis are hypertension, diabetes, and cardiovascular diseases. These comorbidities can cause complications and can result in limited physical activity and low quality of life [1,2,3]. In addition, the risk of patients on hemodialysis with declining physical function and reduced muscle and bone mass is higher than that of normal people. Studies have suggested that patients should exercise at least five days a week and engage in moderate-intensity activities that last for 30 min or longer [4]. Their energy expenditure must reach at least 600 metabolic equivalents of tasks (METs). An energy expenditure of less than 600 METs among these patients indicates that their physical activity level is insufficient, and they should intensify their physical training to prevent further decline in their physical function [5,6].
In Taiwan, chronic kidney disease (CKD) is the ninth most common cause of death [7], and the incidence of hemodialysis increased from 10,668 people in 2014 to 12,346 in 2018. The prevalence of hemodialysis in Taiwan is 3587 per million people, and the number of patients on hemodialysis is increasing by 3% to 4% annually. Approximately 94,000 patients undergo hemodialysis every year. This figure is the highest globally, and hemodialysis is becoming a major public health problem in Taiwan [8]. Approximately 40% of patients on hemodialysis have two or more comorbidities [8]. The development of diseases and clinical abnormalities in these patients causes negative effects, such as the rapid reduction of muscle tension and strength, reduced physical activity, poor prognoses, and low health-related quality of life (HRQoL) [9,10].
Patients with CKD must undergo two to three sessions of hemodialysis every week, with each session lasting between 3 and 4 h. Therefore, compared with healthy people, their physical activity level is 35% lower, and their physical tolerance is also lower [11,12,13]. Approximately 47.4% of all patients have limited time for physical activity and become accustomed to a sedentary lifestyle. With time, patients on hemodialysis tend to develop symptoms, such as fatigue, muscle soreness, and cramping as well as reduced lower extremity muscle strength. The severity of these symptoms is negatively correlated with their physical activity levels and HRQoL. Relative to patients without multiple comorbidities, those with multiple comorbidities have poorer physical health and limited physical activity, resulting in lower physical activity participation [11,12,14,15,16] and a higher mortality rate [17]. Furthermore, the presence of multiple comorbidities aggravates their diseases, contributes to their medical burden, and increases their mortality risk [10]. Few studies have evaluated how the presence of comorbidities in patients on hemodialysis affects their level of physical activity and HRQoL. Therefore, the present study compared the physical activity levels of patients on hemodialysis with comorbidities and those without comorbidities and determined how their level of physical activity affects their HRQoL.
2. Materials and Methods
2.1. Design
This study is a descriptive cross-sectional study.
2.2. Participants
Patients on hemodialysis were recruited from the outpatient clinic of a medical center in Northern Taiwan between January and December 2020. In total, 120 patients completed the 36-Item Short-Form Health Survey version 2 (SF-36) and the abbreviated version of the International Physical Activity Questionnaire (IPAQ) used in Taiwan (Figure 1). The Charlson comorbidity index (CCI) comprises 19 diseases that are weighted on the basis of their association with mortality [18]. The present study used the CCI to measure the comorbidity severity of patients on hemodialysis. As selected by physicians, the study population included patients who regularly received hemodialysis for ≥3 months at a frequency of three times a week, with each session lasting ≥3 h; were ≥20 years old; were conscious; were able to communicate clearly in Chinese or Taiwanese; were literate; and were willing to participate in the present study after the purpose of the study was explained to them. We excluded patients with cognitive disabilities or mental illnesses (because such patients cannot properly respond to our questionnaire), patients who could not care for themselves, and patients who were hospitalized at the time of recruitment.
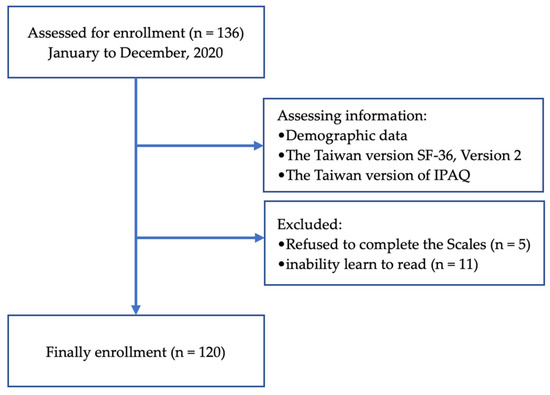
Figure 1.
Flowchart for the present cross-sectional study.
The required sample number was estimated using the G*Power version 3.1.9 [19] software. A linear multiple regression model F-test was conducted, with the effect size (f2), significance level, and power being 0.2, 0.05, and 0.80, respectively. With a projected attrition rate of 10%, the required sample size was estimated to be ≥104.
2.3. Measurement
2.3.1. Demographics
The demographic data of the participants included age, gender, education, marital status, living arrangement, current employment, monthly income, body mass index (BMI, kg/m2), comorbidities, regular physical activity (three times/week), and duration of hemodialysis (years). The biochemical data of the participants included dialysis efficiency (Kt/V), normalized protein catabolic rate (nPCR), hemoglobin level (mg/dL), blood urea nitrogen level (BUN; mg/dL), creatinine level (mg/dL), and albumin level (g/dL) [20].
2.3.2. HRQoL
HRQoL was assessed using the Medical Outcomes Study 36-Item Short-Form Health Survey version 2 (SF-36). The questionnaire contains 36 items under eight subscales as follows: physical functioning (10 items), role-physical (4 items), bodily pain (2 items), general health (5 items), vitality (4 items), social functioning (2 items), role-emotional (3 items), mental health (5 items), and health transition (1 item). The eight subscales belong to the two constructs of physical component score (PCS) and mental component score (MCS) [21]. The total score ranges from 0 to 100, with a higher score indicating better health and higher quality of life [22]. The Cronbach alpha of the questionnaire has been reported as being greater than 0.70 [22].
2.3.3. Physical Activity Measure
The present study used Taiwan’s abbreviated version of the International Physical Activity Questionnaire (IPAQ) for measuring physical activity [23]. The scale was used to examine how much time the participants spent on physical activities over the past 7 days, the types of physical activities they engaged in that lasted more than 10 min, and the duration of such activities. Physical activity intensity was measured using physical activity metabolic equivalent of task (MET; kcal/h/kg). MET is the product of the resting metabolic rate multiplied by time [6]. The activities were categorized as low-intensity (<600 MET-min/week), moderate-intensity (600–2999 MET-min/week), and vigorous-intensity (≥3000 MET-min/week) activities, and their overall physical activity score was calculated. The IPAQ has excellent stability; Spearman’s rho was used to test the IPAQ, and the results indicated that the IPAQ had a reliability of 0.8 and criterion validity of 0.30 [24]. Therefore, the IPAQ is precise and effective.
2.4. Ethical Considerations
The present study enrolled participants after obtaining approval from the relevant institutional review board (IRB number: 1-108-05-195). The participants provided oral and written consent, and they had the right to exercise their autonomy and refuse participation in or withdraw from the study at any time; the medical rights of the participants were not affected by their participation in the present study. All of the data collected in the present study were coded and used only for research purposes.
2.5. Data Analysis
Statistical analysis was performed using SPSS version 22.0 (SPSS, Chicago, IL, USA), with the significance level set at 0.05. The participants’ sociodemographics, quality of life, and physical activity data are presented as means, standard deviations (SDs), and percentages (%). The associations among comorbidities, quality of life, and physical activity were evaluated using t-tests and generalized linear modeling (GLM). Multivariate analyses based on linear regression models were conducted, with adjustment for sociodemographic characteristics (age, gender, education, marital status, employment, monthly income, regular physical activity, duration of hemodialysis, and comorbidities) and physical activity.
3. Results
We enrolled 120 patients on hemodialysis who were aged between 24 and 84 years (mean age = 61.46 years) as participants in the present study. Most participants were male (77.5%), and 62.5% of the participants had a senior high school or higher level of education. Among the participants, 65.8% were married, 89.2% lived with their family, 81.7% did not have an occupation, and 90.0% had a personal income of <50,000 NTD. Their average hemodialysis time was 5.68 years (SD = 4.37). Among the participants, 49.2% had comorbidities that were common, namely congestive heart failure (34.2%), peripheral vascular disease (77.5%), and diabetes (47.5%); 50.8% performed regular physical activity; and only 45% reported sufficient energy expenditure (≥600 METs/week). Furthermore, the participants’ total mean score for HRQoL was 63.11 (SD = 16.20), their average PCS was 65.37 (SD = 17.55), and their average MCS was 60.85 (SD = 14.85; Table 1).

Table 1.
Sociodemographic characteristics of patients on hemodialysis (n = 120).
Table 2 presents the univariate linear regression analysis results. For the PCS construct, patients with >12 years of education (B = 10.58, p < 0.001, 95% confidence interval [CI]: 4.40–16.76), married (B = 6.57, p = 0.047, 95% CI: 0.08–13.06), current employment (B = 18.58, p < 0.001, 95% CI: 11.21–25.95), monthly income was >50,000 NT$ (B = 21.74, p < 0.001, 95% CI: 12.07–31.41), an increase in Kt/V (B = 10.86, p = 0.028, 95% CI: 1.16–20.56), a higher hemoglobin level (B = 2.69, p = 0.020, 95% CI: 0.42–4.95), regular weekly physical activity (B = 8.28, p = 0.008, 95% CI: 2.20–14.36), and weekly energy expenditure of ≥600 METs (B = 74.46, p < 0.001, 95% CI: 71.24–77.69) were positively correlated, and the presence of comorbidities (B = −8.30, p = 0.008, 95% CI: −14.56 to −2.15) was negatively correlated.

Table 2.
Analysis of factors associated with health-related quality of life and sociodemographic characteristics (n = 120).
For the MCS construct, patients with >12 years of education (B = 6.76, p = 0.013, 95% CI: 1.43–12.10), current employment (B = 11.87, p < 0.001, 95% CI: 5.36–18.37), monthly income was >50,000 NT$ (B = 18.10, p < 0.001, 95% CI: 9.89–26.30), an increase in Kt/V (B = 11.51, p = 0.005, 95% CI: 3.40–19.62), regular weekly physical activity (B = 5.48, p = 0.039, 95% CI: 0.28–10.69), duration of hemodialysis (B = 0.70, p = 0.020, 95% CI: 1.11–3.66), and weekly energy expenditure of ≥600 METs (B = 67.92, p < 0.001, 95% CI: 64.86–70.97) were positively correlated, and the presence of comorbidities (B = −6.46, p = 0.015, 95% CI: −11.68 to −1.23) was negatively correlated.
Table 3 presents the result of the independent samples t-test, which revealed that the patients on hemodialysis with comorbidities had lower overall HRQoL (t = 2.70, p = 0.008), PCS (t = 2.83, p = 0.005), MCS (t = 2.29, p = 0.024), and weekly energy expenditure of ≥600 METs (t = 3.35, p < 0.001) than those without comorbidities. Multivariate analysis was conducted, with adjustment for the demographic statistics and factors of physical activity. Compared with the patients on hemodialysis without comorbidities, those with comorbidities had lower HRQoL but reported a comparable level of physical activity.

Table 3.
Comparison of health-related quality of life and physical activity of patients with and without comorbidities (n = 120).
Table 4 presents the results of univariate and multivariate linear regression analyses. In the analyses with adjustment for age, gender, education, marital status, employment, monthly income, Kt/V, hemoglobin level, regular physical activity, habitual physical activity, duration of hemodialysis, and comorbidities, the HRQoL of the patients on hemodialysis who engaged in moderate-intensity physical activity was significantly higher than that of the patients who engaged in low-intensity physical activity (Table 4). In addition, among the patients with comorbidities, overall HRQoL (p = 0.039), PSC (p = 0.011), physical functioning (p = 0.011), and vitality (p = 0.023) were significantly higher among the patients who engaged in moderate-intensity physical activity than among those who engaged in low-intensity physical activity (Figure 2).

Table 4.
Regression of the association between physical activity patterns and health-related quality of life of patients on hemodialysis (n = 120).
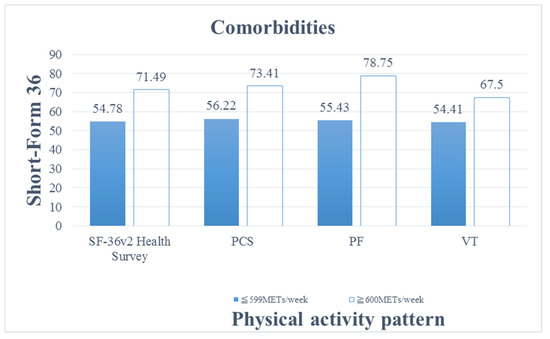
Figure 2.
Comparison of physical activity patterns and health-related quality of life of patients on hemodialysis with comorbidities. Abbreviations: Physical Component Summary, PCS; physical functioning, PF; vitality, VT.
When comparing HRQoL between the patients with comorbidities who engaged in the low-intensity physical activity and moderate-intensity physical activity, those engaging in moderate-intensity physical activity had better HRQoL; particularly, they had higher PCS, physical functioning, role-physical, MCS, vitality, and social functioning.
4. Discussion
Our results revealed that the overall quality of life of patients on hemodialysis with comorbidities was poorer than that of patients on hemodialysis without comorbidities. In addition, the patients on hemodialysis with comorbidities who exercised regularly had higher quality of life than those who did not exercise regularly. That is, engagement in physical activity improved the physical functioning and spirit of these patients. This confirmed that in patients on hemodialysis, regular exercise is a feasible and effective activity that can improve HRQoL and muscle strength and help delay their disease progression [25,26]. For these patients, the implementation of moderate-intensity exercise training programs (e.g., aerobic exercises) can effectively improve the physical role, general health, and pain management domains of their HRQoL; increase their social interactions and enhance their self-attitude [27]; alleviate their disease-related conditions and complications; and improve their physical functioning and prognosis [28,29]. A study indicated that the level of physical activity of patients on hemodialysis is correlated to their HRQoL; the study also reported that relative to healthy people, habitual exercise is a stronger predictor of HRQoL for patients on hemodialysis [30]. Therefore, exercise and physical activity are crucial for treating and preventing multiple diseases. In other words, exercise is medicine [31].
Patients on hemodialysis usually have multiple comorbidities. Compared with patients with a single disease, the HRQoL and physical functioning of patients with multiple comorbidities are more likely to be affected by various factors [32]. Studies have demonstrated that comorbidities aggravated the primary disease of patients and affected their general health and MCS [33]. The presence of multiple comorbidities is correlated with reduced PCS, MCS, and overall HRQoL [2]. Multiple studies have confirmed that comorbidities and diseases affect each other and, consequently, the physical functioning and survival of patients. Comorbidities aggravate the severity of diseases; for patients, quality of life decreases as the number of comorbidities increases, and the physical health of these patients are affected to a greater degree than their mental health [34]. Compared with patients on hemodialysis without comorbidities, the overall HRQoL of patients on hemodialysis with comorbidities is lower, and they are also more likely to experience declining health [34]. Therefore, medical personnel should focus on improving the HRQoL of patients on hemodialysis with comorbidities.
Physical activity is beneficial for CKD [35]. Regular physical activity can improve the physical functioning, muscle tension and strength, PCS, and MCS of patients [25,36]. In patients on hemodialysis, performing regular moderate-intensity exercises three times per week, with each exercise session lasting for more than 30 min, can improve their PCS, MCS [37], and HRQoL in terms of the pain, physical role, and general health domains [24,38]. Exercise can also improve the physical functioning of patients on hemodialysis, stabilize their cognitive function, reduce their risk of developing health conditions, and improve their quality of life [39]. Regular exercise can improve the physical functioning and HRQoL of patients [40]. Patients on hemodialysis who engage in physical activity exhibit high quality of life [13]. The quality-of-life score and daily physical activity are positively correlated [41]. Hornik et al. [13] reported that compared with patients on hemodialysis who did not exercise regularly and engaged in less physical activity, patients who exercised regularly according to physical activity plans showed a lower incidence rate of complications; in addition, regular exercise improved their hemodialysis, physical functioning, role limitations of physical problems, social function, and PCS. The results of the present study revealed that the patients who engaged in moderate-intensity physical activity every week had higher HRQoL than the patients who did not engage in moderate-intensity physical activity every week. That is, patients on hemodialysis with low physical activity had low quality of life. Therefore, engaging in regular physical activity and increasing the level of physical activity can improve the HRQoL of patients on hemodialysis.
A recent study in Taiwan reported a correlation between comorbidities and the loss of HRQoL in analyses with adjustment for sociodemographic factors and medical comorbidities; this discovery is consistent with the results of the present study [42]. Complications and the physical activity level affect HRQoL, possibly because an increase in the number of comorbidities result in deteriorating health, limited physical activity, and reduced activity participation among patients on hemodialysis [34], thereby affecting their HRQoL. When patients engaged in more physical activity, their muscle strength and physical functioning improved; this also improved the waste removal ability of their kidneys and the efficiency of their hemodialysis. Consequently, their HRQoL improved [28,41]. Patients on hemodialysis with comorbidities can exercise regularly to improve their muscle strength and cardiovascular function, prevent cardiovascular diseases, and increase their survival rate, and benefits can also be gained from social interactions. In addition, regular exercise can improve their quality of life and physical functioning and can reduce the negative effects of complications [36,42]. Our results revealed the HRQoL of the patients on hemodialysis who engaged in moderate-intensity physical activity was lower than those without comorbidities. Therefore, we can actively encourage patients on hemodialysis with comorbidities to follow regular moderate-intensity physical activity training programs to improve their HRQoL, reduce the negative effects caused by their comorbidities, and enhance their overall health.
We also observed that regular physical activity and increased levels of physical activity are correlated with HRQoL. Moreover, the educational level, marital status, occupation, income, comorbidity, and regular hemodialysis of patients are associated with their HRQoL. However, similar to other studies, sufficient evidence was not provided in the present study to support the correlation of age and gender with HRQoL [43].
Studies have indicated that patients who have a lower educational level or no education, patients who are not married or widowed, patients who are unemployed, patients who have a low monthly income, and patients who have multiple comorbidities usually have poorer mental health, which directly affects their HRQoL and is negatively correlated with their quality of life. In addition, the quality of life of patients is negatively affected by a hemodialysis history of <2 years, lack of regular exercise, and lack of moderate-intensity exercise [29,43,44]. Therefore, regular physical activity is positively correlated with improvements in quality of life, PCS, and MCS. Physical activity is a predictor of quality of life [45]. Daily moderate-intensity physical activity is correlated with improved SF-36 scores (physical functioning, freedom from pain, vitality, and mental health) [46], and it reduces complications and improves physical functioning, HRQoL, and prognoses [27,28].
The present study has several limitations. First, the study participants were patients from a single hemodialysis center in Northern Taiwan. Therefore, our results may have limited generalizability. Second, the cross-sectional design precluded the determination of long-term changes in physical activity and HRQoL. Finally, the IPAQ used in the present study is a review scale and does not consider objective data. The other data in the scale were self-reported by the patients, who could have underestimated or overestimated their conditions; hence, the reliability and authenticity of the results are lower.
Our findings indicate that the HRQoL of patients on hemodialysis, particularly those with comorbidities, can be improved by providing early intervention involving regular moderate-intensity physical activity. Healthcare professionals should implement effective physical activity interventions to improve the physical activity level of these patients and encourage them perform regular physical activity and adopt a more active lifestyle; these changes will improve their quality of life.
5. Conclusions
The present study revealed that among the patients on hemodialysis who engaged in low-intensity physical activity, those with comorbidities had lower HRQoL relative to those without comorbidities. Furthermore, among the patients on hemodialysis with comorbidities, those who engaged in moderate-intensity physical activity had higher HRQoL than those who engaged in low-intensity physical activity; this was because the latter group had a sedentary lifestyle that resulted in disabilities, and comorbidities aggravate the decrease in muscle tension, strength, and physical activities, all of which led to a poor prognosis. In our cohort, the quality of life of patients with comorbidities who exercised regularly was higher than that of patients with comorbidities who did not exercise regularly. Our findings support the promotion of moderate-intensity physical activity training programs, which can improve quality of life. These programs should play an essential role in the treatment plans and health promotion measures for patients on long-term hemodialysis with comorbidities.
Author Contributions
Conceptualization, Y.-H.W., Y.-J.H. and W.-C.T.; methodology, Y.-H.W. and W.-C.T.; software, Y.-H.W.; validation, Y.-H.W. and W.-C.T.; formal analysis, Y.-H.W. and W.-C.T.; investigation, Y.-H.W.; resources, Y.-J.H.; data curation, W.-C.T.; writing—original draft preparation, Y.-H.W.; writing—review and editing, Y.-H.W. and W.-C.T.; supervision, Y.-J.H.; project administration, Y.-H.W.; funding acquisition, Y.-H.W. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Tri-Service General Hospital (TSGH:1-108-05-195) and the Taiwan Nurses Association (TWNA-1091017), Taipei, Taiwan.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (Reference number: TSGHIRB: 1-108-05-195).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Liu, J.; Huang, Z.; Gilbertson, D.T.; Foley, R.N.; Collins, A.J. An improved comorbidity index for outcome analyses among dialysis patients. Kidney Int. 2010, 77, 141–151. [Google Scholar] [CrossRef] [Green Version]
- Cha, J.; Han, D. Health-Related Quality of Life Based on Comorbidities Among Patients with End-Stage Renal Disease. Osong Public Health Res. Perspect. 2020, 11, 194–200. [Google Scholar] [CrossRef]
- Stojanovic, M.; Stefanovic, V. Assessment of health-related quality of life in patients treated with hemodialysis in Serbia: Influence of comorbidity, age, and income. Artif. Organs 2007, 31, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Roshanravan, B.; Gamboa, J.; Wilund, K. Exercise and CKD: Skeletal Muscle Dysfunction and Practical Application of Exercise to Prevent and Treat Physical Impairments in CKD. Am. J. Kidney Dis. 2017, 69, 837–852. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Bjordal, K.; de Graeff, A.; Fayers, P.M. A 12 country field study of the EORTC QLQ-C30 (version 3.0) and the head and neck cancer specific module (EORTC QLQ-H&N35) in head and neck patients. EORTC Quality of Life Group. Eur. J. Cancer 2000, 36, 1796–1807. [Google Scholar] [PubMed]
- Health Promotion Administration, Ministry of Health and Welfare, Taiwan. 2019 Health Promotion Administration Annual Report. Available online: https://www.hpa.gov.tw/EngPages/Detail.aspx?nodeid=1070&pid=12811 (accessed on 19 October 2021).
- Kidney Disease in Taiwan Annual Report. 2020. Available online: https://www.google.com.tw/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjejszbztbzAhDAIgKHXrOB5AQFnoECAkQAQ&url=https%3A%2F%2Fwww.tsn.org.tw%2FUI%2FL%2FL002.aspx&usg=AOvVaw09xbZt9TkeB2l3rgZIPLGx (accessed on 9 January 2022).
- Visser, W.J.; Egmond, A.M.E.M.; Timman, R.; Severs, D.; Hoorn, E.J. Risk Factors for Muscle Loss in Hemodialysis Patients with High Comorbidity. Nutrients 2020, 12, 2494. [Google Scholar] [CrossRef] [PubMed]
- Tonelli, M.; Wiebe, N.; Guthrie, B. Comorbidity as a driver of adverse outcomes in people with chronic kidney disease. Kidney Int. 2015, 88, 859–866. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomes, E.P.; Reboredo, M.M.; Carvalho, E.V. Physical Activity in Hemodialysis Patients Measured by Triaxial Accelerometer. BioMed Res. Int. 2015, 2015, 645645. [Google Scholar] [CrossRef]
- Johansen, K.L.; Chertow, G.M.; Ng, A.V. Physical activity levels in patients on hemodialysis and healthy sedentary controls. Kidney Int. 2000, 57, 2564–2570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hornik, B.; Duława, J. Frailty, Quality of Life, Anxiety, and Other Factors Affecting Adherence to Physical Activity Recommendations by Hemodialysis Patients. Int. J. Environ. Res. Public Health 2019, 16, 1827. [Google Scholar] [CrossRef] [Green Version]
- Cupisti, A.; D’Alessandro, C.; Bottai, A.; Fumagalli, G.; Capitanini, A. Physical activity and exercise training: A relevant aspect of the dialysis patient’s care. Intern. Emerg. Med. 2013, 8 (Suppl. 1), S31–S34. [Google Scholar] [CrossRef]
- Sheshadri, A.; Kittiskulnam, P.; Johansen, K.L. Higher Physical Activity Is Associated With Less Fatigue and Insomnia among Patients on Hemodialysis. Kidney Int. Rep. 2018, 4, 285–292. [Google Scholar] [CrossRef] [Green Version]
- Diaz, K.M.; Howard, V.J.; Hutto, B. Patterns of Sedentary Behavior and Mortality in U.S. Middle-Aged and Older Adults: A National Cohort Study. Ann. Intern. Med. 2017, 167, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Kim, J.C.; Young Do, J.; Kang, S.H. Comparisons of physical activity and understanding of the importance of exercise according to dialysis modality in maintenance dialysis patients. Sci. Rep. 2021, 11, 1–9. [Google Scholar] [CrossRef]
- Lu, J.F.; Tseng, H.T.; Tsai, Y.J. Assessment of health-related quality of life in Taiwan (I): Development and psychometric testing of SF-36 Taiwan version. Taiwan J. Public Health 2003, 22, 501–511. [Google Scholar]
- Liou, Y.M.; Jwo, C.J.; Yao, K.G.; Chiang, L.C.; Huang, L.H. Selection of appropriate Chinese terms to represent intensity and types of physical activity terms for use in the Taiwan version of IPAQ. J. Nurs. Res. 2008, 16, 252–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hallal, P.C.; Victora, C.G. Reliability and validity of the International Physical Activity Questionnaire (IPAQ). Med. Sci. Sports Exerc. 2004, 36, 556. [Google Scholar] [CrossRef]
- Ibrahim, A.A.; Althomali, O.W.; Atyia, M.R. A systematic review of trials investigating the efficacy of exercise training for functional capacity and quality of life in chronic kidney disease patients. Int. Urol. Nephrol. 2021, 10, 1–10. [Google Scholar] [CrossRef]
- Pu, J.; Jiang, Z.; Wu, W. Efficacy and safety of intradialytic exercise in haemodialysis patients: A systematic review and meta-analysis. BMJ Open 2019, 9, e020633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pei, G.; Tang, Y.; Tan, L.; Tan, J.; Ge, L.; Qin, W. Aerobic exercise in adults with chronic kidney disease (CKD): A meta-analysis. Int. Urol. Nephrol. 2019, 51, 1787–1795. [Google Scholar] [CrossRef]
- Marthoenis, M.; Syukri, M.; Abdullah, A. Quality of life, depression, and anxiety of patients undergoing hemodialysis: Significant role of acceptance of the illness. Int. J. Psychiatry Med. 2021, 56, 40–50. [Google Scholar] [CrossRef] [PubMed]
- de Lima, M.C.; Cicotoste, C.D.L.; Cardoso, K.D.S.; Forgiarini, L.A., Jr.; Monteiro, M.B.; Dias, A.S. Effect of exercise performed during hemodialysis: Strength versus aerobic. Ren. Fail. 2013, 35, 697–704. [Google Scholar] [CrossRef] [Green Version]
- Filipčič, T.; Bogataj, Š.; Pajek, J.; Pajek, M. Physical Activity and Quality of Life in Hemodialysis Patients and Healthy Controls: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 1978. [Google Scholar] [CrossRef]
- Wilkinson, T.J.; Shur, N.F.; Smith, A.C. “Exercise as medicine” in chronic kidney disease. Scand. J. Med. Sci. Sports 2016, 26, 985–988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fraser, S.D.; Barker, J.; Roderick, P.J. Health-related quality of life, functional impairment and comorbidity in people with mild-to-moderate chronic kidney disease: A cross-sectional study. BMJ Open 2020, 10, e040286. [Google Scholar] [CrossRef]
- Markle-Reid, M.; Ploeg, J.; Fraser, K.D. Community Program Improves Quality of Life and Self-Management in Older Adults with Diabetes Mellitus and Comorbidity. J. Am. Geriatr. Soc. 2018, 66, 263–273. [Google Scholar] [CrossRef]
- Makovski, T.T.; Schmitz, S.; Zeegers, M.P.; Stranges, S.; van den Akker, M. Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Res. Rev. 2019, 53, 100903. [Google Scholar] [CrossRef] [PubMed]
- Moisoglou, I.; Margariti, E.; Kollia, K.; Droulias, J.; Savva, L. The role of demographic characteristics and comorbidities in hemodialysis patients’ health-related quality of life. Hippokratia 2017, 21, 163–168. [Google Scholar] [PubMed]
- Wang, I.K.; Tsai, M.K.; Liang, C.C. The role of physical activity in chronic kidney disease in the presence of diabetes mellitus: A prospective cohort study. Am. J. Nephrol. 2013, 38, 509–516. [Google Scholar] [CrossRef]
- Afsar, B.; Siriopol, D.; Aslan, G. The impact of exercise on physical function, cardiovascular outcomes and quality of life in chronic kidney disease patients: A systematic review. Int. Urol. Nephrol. 2018, 50, 885–904. [Google Scholar] [CrossRef]
- Takhreem, M. The effectiveness of intradialytic exercise prescription on quality of life in patients with chronic kidney disease. Medscape J. Med. 2008, 10, 226. [Google Scholar] [PubMed]
- Lin, C.H.; Hsu, Y.J.; Hsu, P.H. Effects of Intradialytic Exercise on Dialytic Parameters, Health-Related Quality of Life, and Depression Status in Hemodialysis Patients: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 9205. [Google Scholar] [CrossRef]
- Mallamaci, F.; Pisano, A.; Tripepi, G. Physical activity in chronic kidney disease and the EXerCise Introduction To Enhance trial. Nephrol. Dial. Transplant. 2020, 35 (Suppl. 2), ii18–ii22. [Google Scholar] [CrossRef]
- Heiwe, S.; Jacobson, S.H. Exercise training for adults with chronic kidney disease. Cochrane Database Syst. Rev. 2011, 10, CD003236. [Google Scholar] [CrossRef]
- Katayama, A.; Miyatake, N.; Nishi, H. Relationship between Changes in Physical Activity and Changes in Health-related Quality of Life in Patients on Chronic Hemodialysis with 1-Year Follow-up. Acta Med. Okayama 2016, 70, 353–361. [Google Scholar] [PubMed]
- Shimoda, T.; Matsuzawa, R.; Yoneki, K. Changes in physical activity and risk of all-cause mortality in patients on maintence hemodialysis: A retrospective cohort study. BMC Nephrol. 2017, 18, 154. [Google Scholar] [CrossRef] [Green Version]
- Samoudi, A.F.; Marzouq, M.K.; Samara, A.M.; Zyoud, S.H.; Al-Jabi, S.W. The impact of pain on the quality of life of patients with end-stage renal disease undergoing hemodialysis: A multicenter cross-sectional study from Palestine. Health Qual. Life Outcomes 2021, 19, 39. [Google Scholar] [CrossRef]
- Ma, S.J.; Wang, W.J.; Tang, M.; Chen, H.; Ding, F. Mental health status and quality of life in patients with end-stage renal disease undergoing maintenance hemodialysis. Ann. Palliat. Med. 2021, 10, 6112–6121. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.C.; Chen, H.M.; Hsiao, S.M. Association of physical activity with cardiovascular and renal outcomes and quality of life in chronic kidney disease. PLoS ONE 2017, 12, e0183642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aoyagi, Y.; Park, H.; Park, S.; Shephard, R.J. Habitual physical activity and health-related quality of life in older adults: Interactions between the amount and intensity of activity (the Nakanojo Study). Qual. Life Res. 2010, 19, 333–338. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).