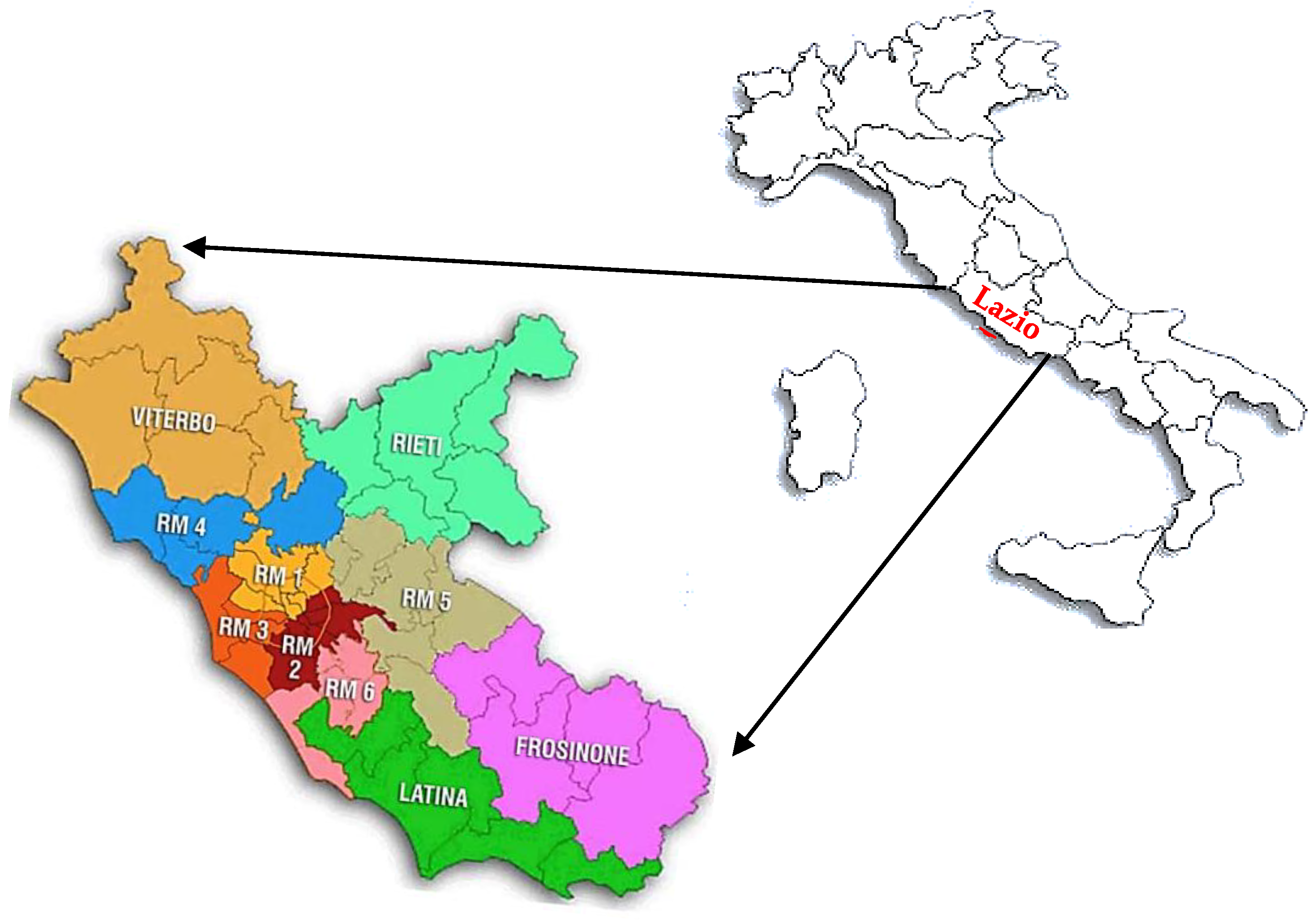
Impact of the COVID-19 Pandemic on Clinical Pathways for Non-SARS-CoV-2 Related Diseases in the Lazio Region, Italy
Abstract
:1. Introduction
2. Materials and Methods
The Survey Questionnaire
- Context analysis;
- Patients access to care pathways/Operational Unit;
- Impact on the treatment of non-COVID patients in the CPs;
- Impact on the treatment of patients also SARS-CoV-2 infected in the CPs;
- Impact of the COVID-19 pandemic on patient management;
- Structural and organizational changes of the CP/UO;
- Procedures and recommendations for healthcare professionals/users;
- Training, information, and management of health workers in the pandemic era.
3. Results
- Context analysis: only in 7 UU.OO. (29.2%) more than 75% of the patients accepted the treatment within the CP, the fear of being infected notwithstanding; compared to the same period of the previous year, during the first wave, there was a reduction in the treatment given within the CP in 91.7% of the UU.OO., as only 8.3% UU.OO. declared that the accesses remained stable (mean score 2.21 ± 1.04). By contrast, patient management stabilized in the second pandemic event according to 20 respondents (83.3%; 62.5% “yes” and 20.8% “enough”, with a mean score 3.38 ± 0.99).
- Patient access to CP/UO: The CPs have been adapted to the pandemic setting by adopting security and social distancing measures in 91.7 and in 79.2% of the UU.OO. respectively (mean score 3.92 ± 0.28 and 3.71 ± 0.68, respectively). Patients who accepted treatment within the CP filled a preliminary pre-triage form in 83.3% of the UU.OO. (mean score 3.46 ± 1.22).
- The impact on the treatment of NON-COVID patients in the clinical pathway: despite the COVID-19 pandemic, in the majority of the UU.OO. (66.7% “yes”, 20.8% “enough”) the access and the treatment were guaranteed in any case, and the canceled visits were rescheduled in 75.0% of the UU.OO. (58.3% “yes”, 16.7% “enough”). Overall, 58.3% (16.7% “yes”, 41.7% “enough”) of the UU.OO. used telemedicine in the form of remote monitoring to avoid the care interruption (mean score 2.25 ± 1.39) and 54.2% (20.8% “yes”, 33.3% “enough”) of the UU.OO. have adopted tele-assistance solutions for patient follow-up (mean score 2.25 ± 1.42).
- The impact on the treatment of patients also infected with SARS-CoV-2 in the CPs: the CPs have not been shown to be adequate for the management of patients affected by SARS-CoV-2. In fact, no UU.OO. declared that they treated patients affected by COVID-19 within the care pathway/hospital ward answered “yes”, and only 2 (8.3%) answered “enough” (mean score 1.04 ± 0.84). It’s the only section that registered a not acceptable level of performance, both as a whole and for the single questions. Most of the enrolled healthcare settings were not integrated into the COVID Hospitals’ net, therefore 83.3% UU.OO. found the question if they had treated COVID-19 positive patients within a COVID ward not applicable to their setting (mean score 0.21 ± 0.50).
- Impact of the COVID-19 pandemic on patient management: the SARS-CoV-2 screening test was routinely repeated during hospitalization in 45.8% of the UU OO, even if 45.8% found the question not applicable to their setting (mean score 1.96 ± 1.93), and in 91.7% of the UU.OO. the correct use of personal protective equipment (PPE) by staff and patients was monitored (mean score 3.71 ± 0.98).
- Structural and organizational changes of the CP/UO: in 20 UU.OO. (83.3%; 58.3% “yes” and 25.0% “enough”) outpatient and/or surgical activities were guaranteed anyway (mean score 3.13 ± 1.36), and in 19 (79.2%; 37.5% “yes”, 41.7% “enough”) the timing in the transition of patients from one care setting to another was respected (mean score 2.79 ± 1.41). The services related to non-deferrable diseases were maintained in 22 UU.OO. (91.7%; 83.3% “yes” and 8.3% “enough”, mean score 3.63 ± 0.99).
- Procedures and recommendations for healthcare professionals/users: In most of the UU.OO., the measures adopted were respected by both patients (100%; 54.2% “yes” and 45.8% “enough”) and relatives (95.8%; 62.5% “yes”, 33.3% “enough” and 4.2% “not enough”); as for the healthcare professionals, the recommendations were visible and clear in 91.7% of the UU.OO. (87.5% “yes” and 4.2% “enough”, with only 4.2% “not applicable”; mean score 3.67 ± 0.99) and the measures adopted were respected in 87.5% of them (83.3% “yes” and 4.2% “enough”, with 8.3% “not applicable”; mean score 3.50 ± 1.22).
- Training, information, and management of health workers in the pandemic era: In 22 UU. OO. (91.7%; 87.5% “yes” and 4.2% “enough”), specific training was carried out to ensure the correct adoption of PPE (mean score 3.63 ± 1.11), and the health personnel working within the CPs were monitored with screening tests for SARS-CoV-2 (87.5% “yes”, 8.3% “enough” and 4.2% “not applicable”; mean score 3.75 ± 0.83), and kept as safe as possible through the use of PPE modulated on the basis of the different risk exposure (79.2% “yes”, 16.7% “enough” and 4.2% “not applicable”; mean score 3.67 ± 0.85).
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vanhaecht, K.; Panella, M.; Van Zelm, R.; Sermeus, W. An overview on the history and concept of care pathways as complex interventions. Int. J. Care Pathw. 2010, 14, 117–123. [Google Scholar] [CrossRef]
- Capalbo, C.; Bertamino, E.; Zerbetto, A.; Santino, I.; Petrucca, A.; Mancini, R.; Bonfini, R.; Alfonsi, V.; Ferracuti, S.; Marchetti, P.; et al. No Evidence of SARS-CoV-2 Circulation in Rome (Italy) during the Pre-Pandemic Period: Results of a Retrospective Surveillance. Int. J. Environ. Res. Public Health 2020, 17, 8461. [Google Scholar] [CrossRef]
- Di Bidino, R.; Cicchetti, A. Impact of SARS-CoV-2 on Provided Healtcare. Evidence from the emergency phase in Italy. Front. Public Health 2020, 8, 1–8. [Google Scholar] [CrossRef]
- Napoli, C.; Dente, M.G.; Kärki, T.; Riccardo, F.; Rossi, P.; Declich, S. Screening for Infectious Diseases among Newly Arrived Migrants: Experiences and Practices in Non-EU Countries of the Mediterranean Basin and Black Sea. Int. J. Environ. Res. Public Health 2015, 12, 15550–15558. [Google Scholar] [CrossRef] [Green Version]
- Capalbo, C.; Aceti, A.; Simmaco, M.; Bonfini, R.; Rocco, M.; Ricci, A.; Napoli, C.; Rocco, M.; Alfonsi, V.; Teggi, A.; et al. The Exponential Phase of the COVID-19 Pandemic in Central Italy: An Integrated Care Pathway. Int. J. Environ. Res. Public Health 2020, 17, 3792. [Google Scholar] [CrossRef] [PubMed]
- Pasquarella, C.; Veronesi, L.; Castiglia, P.; Liguori, G.; Montagna, M.T.; Napoli, C.; Rizzetto, R.; Torre, I.; Masia, M.D.; Di Onofrio, V.; et al. Italian multicentre study on microbial environmental contamination in dental clinics: A pilot study. Sci. Total Environ. 2010, 408, 4045–4051. [Google Scholar] [CrossRef]
- Richards, M.; Anderson, M.; Carter, P.; Ebert, B.L.; Mossialos, E. The impact of the COVID-19 pandemic on cancer care. Nat. Cancer 2020, 1, 565–567. [Google Scholar] [CrossRef] [PubMed]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 Era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef] [PubMed]
- Piccolo, R.; Bruzzese, D.; Mauro, C.; Aloia, A.; Baldi, C.; Boccalatte, M.; Bottiglieri, G.; Briguori, C.; Caiazzo, G.; Calabrò, P.; et al. Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID-19 outbreak. Circulation 2020, 141, 2035–2037. [Google Scholar] [CrossRef] [PubMed]
- Jereczek-Fossa, B.A.; Palazzi, M.F.; Soatti, C.P.; Cazzaniga, L.F.; Ivaldi, G.B.; Pepa, M.; Amadori, M.; Antognoni, P.; Arcangeli, S.; Buffoli, A.; et al. COVID-19 outbreak and cancer radiotherapy disruption in Lombardy, Northern Italy. Clin. Oncol. 2020, 32, 160–161. [Google Scholar] [CrossRef]
- Torzilli, G.; Viganò, L.; Galvanin, J.; Castoro, C.; Quagliuolo, V.; Spinelli, A.; Zerbi, A.; Donadon, M.; Montorsi, M. A snapshot of elective oncological surgery in Italy during COVID-19 emergency: Pearls, pitfalls, and perspectives. Ann. Surg. 2020, 272, 112–117. [Google Scholar] [CrossRef]
- Indini, A.; Aschele, C.; Cavanna, L.; Clerico, M.; Daniele, B.; Fiorentini, G.; Fioretto, L.; Giordano, M.; Montesarchio, V.; Ortega, C.; et al. Reorganisation of medical oncology departments during the novel coronavirus disease-19 pandemic: A nationwide Italian survey. Eur. J. Cancer 2020, 132, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Lahner, E.; Dilaghi, E.; Prestigiacomo, C.; Alessio, G.; Marcellini, L.; Simmaco, M.; Santino, I.; Orsi, G.B.; Anibaldi, P.; Marcolongo, A.; et al. Prevalence of SARS-COV-2 Infection in Health Workers (HWs) and Diagnostic Test Performance: The Experience of a Teaching Hospital in Central Italy. Int. J. Environ. Res. Public Health 2020, 17, 4417. [Google Scholar] [CrossRef] [PubMed]
- Italian Ministry of Health. “Linee di Indirizzo per la Progressiva Riattivazione delle Attività Programmate Considerate Differibili in corso di Emergenza da COVID-19.” 1 June 2020. Available online: https://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2020&codLeg=74374&parte=1%20&serie=null (accessed on 2 January 2021).
- Gola, M.; Caggiano, G.; De Giglio, O.; Napoli, C.; Diella, G.; Carlucci, M.; Carpagnano, L.F.; D’Alessandro, D.; Joppolo, C.M.; Capolongo, S.; et al. SARS-CoV-2 indoor contamination: Considerations on anti-COVID-19 management of ventilation systems, and finishing materials in healthcare facilities. Ann. Ig. 2021, 33, 381–392. [Google Scholar]
- Caggiano, G.; Napoli, C.; Coretti, C.; Lovero, G.; Scarafile, G.; De Giglio, O.; Montagna, M.T. Mold contamination in a controlled hospital environment: A 3-year surveillance in southern Italy. BMC Infect. Dis. 2014, 14, 595. [Google Scholar] [CrossRef] [Green Version]
- Presidency of the Italian Council of Ministries. Decreto del Presidente del Consiglio dei Ministri 11 marzo 2020. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19, applicabili sull’intero territorio nazionale, (20A01605); Gazzetta Ufficiale della Repubblica Italiana n.64 del 11-03-2020; Istituto Poligrafico e Zecca dello Stato: Rome, Italy, 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/03/11/20A01605/sg (accessed on 2 January 2021).
- Presidency of the Italian Council of Ministries. Decreto del Presidente del Consiglio dei Ministri, Ulteriori disposizioni attuative del decreto-legge 25 marzo 2020, n. 19, convertito, con modificazioni, dalla legge 22 maggio 2020, n. 35, recante «Misure urgenti per fronteggiare l’emergenza epidemiologica da COVID-19», del decreto-legge 16 maggio 2020, n. 33, convertito, con modificazioni, dalla legge 14 luglio 2020, n. 74, recante «Ulteriori misure urgenti per fronteggiare l’emergenza epidemiologica da COVID-19», e del decreto-legge 23 febbraio 2021, n. 15, recante «Ulteriori disposizioni urgenti in materia di spostamenti sul territorio nazionale per il contenimento dell’emergenza epidemiologica da COVID-19». (21A01331); Gazzetta Ufficiale della Repubblica Italiana n. 52 del 02-03-2021; Istituto Poligrafico e Zecca dello Stato: Rome, Italy, 2021. Available online: https://www.gazzettaufficiale.it/eli/id/2021/03/02/21A01331/sg (accessed on 2 March 2021).
- Walker, P.G.T.; Whittaker, C.; Watson, O.J.; Banguelin, M.; Winskill, P.; Hamlet, A.; Djafaara, B.A.; Cucunubà, Z.; Olivera Mesa, D.; Green, W.; et al. The Impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries. Science 2020, 369, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Drinkwater, B.L. A comparison of the direction-of-perception technique with the Likert method in the measurement of attitudes. J. Soc. Psychol. 1965, 67, 189–196. [Google Scholar] [CrossRef]
- Arghittu, A.; Dettori, M.; Dempsey, E.; Deiana, G.; Angelini, C.; Bechini, A.; Bertoni, C.; Boccalini, S.; Bonanni, P.; Cinquetti, S.; et al. Health Communication in COVID-19 Era: Experiences from the Italian VaccinarSì Network Websites. Int. J. Environ. Res. Public Health 2021, 18, 5642. [Google Scholar] [CrossRef]
- Siebenhofer, A.; Huter, S.; Avian, A.; Mergenthal, K.; Schaffler Schaden, D.; Spary-Kainz, U.; Bachler, H.; Flamm, M. COVI-Prim survey: Challenges for Austrian and German general practitioners during inizial phase of COVID-19. PLoS ONE 2021, 16, 0251736. [Google Scholar] [CrossRef]
- Deiana, G.; Azara, A.; Dettori, M.; Delogu, F.; Vargiu, G.; Gessa, I.; Arghittu, A.; Tidore, M.; Steri, G.; Castiglia, P. Characteristics of SARS-CoV-2 positive cases beyond health-care professionals or social and health-care facilities. BMC Public Health 2021, 21, 83. [Google Scholar] [CrossRef]
- Bianchi, F.; Dama, E.; Di Nicolantonio, F.; Baldassarre, G.; Guerriero, I.; Torchiaro, E.; Bruno, A.; Blandino, G.; Allavena, P.; Chiarugi, P.; et al. COVID-19 epidemic strongly affected cancer research in Italy: A survey of the Italian Cancer Society (SIC). ESMO Open 2021, 6, 100165. [Google Scholar] [CrossRef] [PubMed]
- Heald, A.; Bramham-Jones, S.; Davies, M. Comparing cost of intravenous infusion and subcutaneous biologics in COVID-19 pandemic care pathways for rheumatoid arthritis and inflammatory bowel disease: A brief UK stakeholder survey. Int. J. Clin. Pract. 2021, 75, e14341. [Google Scholar] [CrossRef] [PubMed]
- Biganzoli, L.; Cardoso, F.; Beishon, M.; Cameron, D.; Cataliotti, L.; Coles, C.E.; Delgado Bolton, R.C.; Trill, M.D.; Erdem, S.; Fjell, M.; et al. The requirements of a specialist breast centre. Breast 2020, 51, 65–84. [Google Scholar] [CrossRef] [PubMed]
- Bongiovanni, A.; Mercatali, L.; Fausti, V.; Toni, I. Comment on “Reorganisation of medical oncology departments during the novel coronavirus disease-19 pandemic: A nationwide Italian survey” by Alice Indini et al. Eur. J. Cancer. 2020, 134, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Peric, S.; Stulnig, T.M. Diabetes and COVID-19: Disease-Management-People. Wien Klin Wochenschr. 2020, 132, 356–361. [Google Scholar] [CrossRef]
- Fersia, O.; Bryant, S.; Nicholson, R.; McMeeken, K.; Brown, C.; Donaldson, B.; Jardine, A.; Grierson, V.; Whalen, V.; Mackay, A. The impact of the COVID-19 pandemic on cardiology services. Open Heart 2020, 7, e001359. [Google Scholar] [CrossRef] [PubMed]
- Indini, A.; Pinotti, G.; Artioli, F.; Aschele, C.; Bernardi, D.; Butera, A.; Defraia, E.; Fasola, G.; Gamucci, T.; Giordano, M.; et al. Management of patients with cancer during the COVID-19 pandemic: The Italian perspective on the second wave. Eur. J. Cancer 2021, 148, 112–116. [Google Scholar] [CrossRef]
- Nicholas, J.; Bell, I.H.; Thompson, A.; Valentine, L.; Simsir, P.; Sheppard, H.; Adams, S. Implementation lessons from the transition to telehealth during COVID-19: A survey of clinicians and young people from youth mental health services. Psychiatry Res. 2021, 299, 113848. [Google Scholar] [CrossRef]
- Murris, F.; Huchon, C.; Zilberman, S.; Dabi, Y.; Phalippou, J.; Canlorbe, G.; Ballester, M.; Gauthier, T.; Avigdor, S.; Cirier, J.; et al. Impact of the first lockdown for coronavirus 19 on breast cancer management in France: A multicentre survey. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102166. [Google Scholar] [CrossRef]
- Lazio Region, DCA n. 81/2020 “Piano di Riorganizzazione, Riqualificazione e Sviluppo del Servizio Sanitario Regionale 2019–2021. Available online: https://www.regione.lazio.it/sites/default/files/decreti-commissario-ad-acta/SAN_DCA_U00081_25_06_2020.pdf (accessed on 2 January 2021).
- Wallis, K.E.; Mulé, C.; Mittal, S.; Cerda, N.; Shaffer, R.; Scott, A.; Langkamp, D.; Augustyn, M.; Perrin, E.; Soares, N.; et al. Use of Telehealth in Fellowship-Affiliated Developmental Behavioral Pediatric Practices During the COVID-19 Pandemic. J. Dev. Behav. Pediatr. 2021, 4, 314–321. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Roma, P.; De Giglio, O.; Caggiano, G.; Tafuri, S.; Da Molin, G.D.; Ferracuti, S.; Montagna, M.T.; Liguori, G.; et al. Knowledge and Acceptance of COVID-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines 2021, 9, 638. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, M.; Chakraborty, S.; Pal, R. Diabetes self-management amid COVID-19 pandemic. Diabetes Metab. Syndr. 2020, 4, 351–354. [Google Scholar] [CrossRef]
- Iatta, R.; Napoli, C.; Borghi, E.; Montagna, M.T. Rare mycoses of the oral cavity: A literature epidemiologic review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, 647–655. [Google Scholar] [CrossRef] [PubMed]
- Gallè, F.; Sabella, E.A.; Roma, P.; Ferracuti, S.; Da Molin, G.; Diella, G.; Montagna, M.T.; Orsi, G.B.; Liguori, G.; Napoli, C. Knowledge and Lifestyle Behaviors Related to COVID-19 Pandemic in People over 65 Years Old from Southern Italy. Int. J. Environ. Res. Public Health 2021, 18, 10872. [Google Scholar] [CrossRef] [PubMed]
- Bosa, I.; Castelli, A.; Castelli, M.; Ciani, O.; Compagni, A.; Galizzi, M.M.; Garofano, M.; Ghislandi, S.; Giannoni, M.; Marini, G.; et al. Corona-regionalism? Differences in regional responses to COVID-19 in Italy. Health Policy 2021, 125, 1179–1187. [Google Scholar] [CrossRef]
- Trimarchi, L.; Caruso, R.; Magon, G.; Odone, A.; Arrigoni, C. Clinical pathways and patient-related outcomes in hospital-based settings: A systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021, 92, e2021093. [Google Scholar] [CrossRef]
| Clinical Pathway | UU OO | ASL/AO |
|---|---|---|
| Heart Failure | UOC Cardiology | AO San Camillo, Rome (RM3) |
| UOD Radiologic Emergency/Urgency | ||
| UOC Emergency Medicine, Emergency Department and OBI | ||
| UOSD Cardiology Integrated Services | ||
| UOD Shock and Trauma | ||
| Hereditary breast-ovarian cancer | UOC Medical Genetics | University Hospital Sant’Andrea, Rome (RM1) |
| UOC Oncology | ||
| UOS Diagnostic and Therapeutic Breast Unit (UDTS) | ||
| UOS Breast Radiology | ||
| UOC Gynecology | ||
| UOD Breast Surgery | ||
| UOD Psychoncology | ||
| Autism Spectrum Disorders (ASD) | UOC Mental Health Center H1-H3 | ASL RM6, Department of Mental Health and Pathological Addictions (DSM-DP) |
| UOC Mental Health Center H4-H6 | ||
| UOC Protection of Mental Health and Rehabilitation of the Age of Development (TMSREE) | ||
| Psychiatric Service of Diagnosis and Cure | ||
| DH Psychiatric | ||
| PLS | ||
| Diabetes | UOC District C Management-Atina Community Health Center (Casa Della Salute) | ASL Frosinone-District C and D |
| UOS Primary Care (Assistenza Sanitaria di Base, ASB) District C and D | ||
| UOD Endocrinology and Metabolic Diseases | ||
| UOC Public Relations Office-Single Access Point (Punto Unico di Accesso, PUA) | ||
| UCP of General Practitioners—Atina Health Center | ||
| Outpatient specialistic visits in Cardiology, Diabetology, and Ophthalmology |
| COVID Survey Sections | Clinical Pathways (CPs) | Level of Performance * | |||||
|---|---|---|---|---|---|---|---|
| Overall (2.86 ± 0.08) | HF (2.54 ± 0.17) | HBOC (3.19 ± 0.12) | ASD (2.81 ± 0.14) | D 2.90 ± 0.25 | Overall: Acceptable | ||
| 1 | Context analysis | 2.63 ± 0.20 | 2.40 ± 0.34 | 3.00 ± 0.25 | 2.88 ± 0.34 | 2.25 ± 0.61 | HBOC: Good Overall, ASD, HF, D: Acceptable |
| 2 | Patients access to CP/UO | 3.68 ± 0.23 | 3.20 ± 0.33 | 3.62 ± 0.34 | 3.89 ± 0.10 | 4.00 ± 0.82 | Good |
| 3 | Impact on the treatment of NON-COVID patients in the clinical pathway | 2.80 ± 0.26 | 2.27 ± 0.59 | 3.43 ± 0.32 | 2.61 ± 0.48 | 2.89 ± 0.69 | HBOC: Good Overall, ASD, HF, D: Acceptable |
| 4 | Impact on the treatment of patients also SARS-CoV-2 infected in the Clinical Pathway | 0.79 ± 0.22 | 0.88 ± 0.63 | 0.83 ± 0.41 | 0.77 ± 0.38 | 0.67 ± 0.33 | Not Acceptable |
| 5 | Impact of the COVID-19 pandemic on patient management | 3.09 ± 0.28 | 2.84 ± 0.58 | 3.34 ± 0.49 | 3.27 ± 0.45 | 2.90 ± 0.70 | Overall, HBOC, ASD: Good HF, D: Acceptable |
| 6 | Structural and organizational changes of the CP/UO | 3.10 ± 0.26 | 2.37 ± 0.59 | 3.64 ± 0.26 | 3.19 ± 0.39 | 3.19 ± 0.73 | Overall, HBOC, ASD, D: Good HF: Acceptable |
| 7 | Procedures and recommendations for healthcare professionals/users | 3.63 ± 0.22 | 3.20 ± 0.24 | 3.81 ± 0.21 | 3.53 ± 0.27 | 3.97 ± 0.81 | Good |
| 8 | Training, information and management of health workers in the pandemic era | 3.19 ± 0.26 | 3.20 ± 0.47 | 3.88 ± 0.22 | 2.36 ± 0.56 | 3.31 ± 0.74 | Overall, HBOC, HF, D: Good ASD: Acceptable |
| Yes n (%) | Enough n (%) | Not Enough n (%) | Not at All n (%) | NA n (%) | Total Score | Mean Score ± DS | Level of Performance * | |
|---|---|---|---|---|---|---|---|---|
| 1. Contex Analysis | 2.63 ± 0.20 | Acceptable | ||||||
| During the COVID-19 pandemic, did patients accept treatment despite the fear of contagion? | 7 (29.2) | 8 (33.3) | 2 (8.3) | 5 (20.8) | 2 (8.3) | 61 | 2.54 ± 1.32 | Acceptable |
| Compared to the same period of the previous year, during the first wave of the pandemic, did the number of accesses remain stable? | 2 (8.3) | 10 (41.7) | 3 (12.5) | 9 (37.5) | 0 (0.0) | 53 | 2.21 ± 1.04 | Acceptable |
| Compared to the first wave of the pandemic, did the number of patients undertaking the care pathways remained stable during the second wave? | 15 (62.5) | 5 (20.8) | 3 (12.5) | 0 (0.0) | 1 (4.2) | 81 | 3.38 ± 0.99 | Good |
| Has the volume of procedures remained stable during first and second waves compared to the same period of the previous year? | 3 (12.5) | 13 (54.2) | 3 (12.5) | 3 (12.5) | 2 (8.3) | 60 | 2.50 ± 1.12 | Acceptable |
| 2. Patients access to CP/UO | 3.68 ± 0.23 | Good | ||||||
| Do you use a pre-triage module during treatment? | 20 (83.3) | 0 (0.0) | 0 (0.0) | 3 (12.5) | 1 (4.2) | 83 | 3.46 ± 1.22 | Good |
| Are security measures taken? | 22 (91.7) | 2 (8.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 94 | 3.92 ± 0.28 | Good |
| Are social distancing measures being taken? | 19 (79.2) | 4 (16.7) | 0 (0.0) | 1 (4.2) | 0 (0.0) | 89 | 3.71 ± 0.68 | Good |
| 3. Impact on the treatment of NON-COVID patients in the Clinical Pathway | 2.80 ± 0.26 | Acceptable | ||||||
| Was the start of the treatment within the care pathway guaranteed to the patients anyway? | 16 (66.7) | 5 (20.8) | 1 (4.2) | 1 (4.2) | 1 (4.2) | 82 | 3.42 ± 1.04 | Good |
| Have the cancelled visits been rescheduled and recovered? | 14 (58.3) | 4 (16.7) | 0 (0.0) | 1 (4.2) | 5 (20.8) | 69 | 2.88 ± 1.62 | Acceptable |
| Has remote monitoring been activated for patients who could not interrupt the treatment (telemedicine)? | 4 (16.7) | 10 (41.7) | 3 (12.5) | 2 (8.3) | 5 (20.8) | 54 | 2.25 ± 1.39 | Acceptable |
| 4. Impact on the treatment of patients also SARS-CoV-2 infected in the Clinical Pathway | 0.79 ± 0.22 | Not Acceptable | ||||||
| Have you treated patients affected by COVID-19 within the care pathway/hospital ward? | 0 (0.0) | 2 (8.3) | 3 (12.5) | 13 (54.2) | 6 (25.0) | 25 | 1.04 ± 0.84 | Not Acceptable |
| If yes or enough: in hospital in COVID wards? | 0 (0.0) | 0 (0.0) | 1 (4.2) | 3 (12.5) | 20 (83.3) | 5 | 0.21 ± 0.50 | Not Acceptable |
| If yes or enough: was it in COVID wards with telephone counselling? | 0 (0.0) | 0 (0.0) | 2 (8.3) | 3 (12.5) | 19 (79.2) | 7 | 0.29 ± 0.61 | Not Acceptable |
| Have the care pathways for COVID and NON_COVID patients been separated? | 12 (50.0) | 1 (4.2) | 0 (0.0) | 2 (8.3) | 9 (37.5) | 53 | 2.21 ± 1.89 | Acceptable |
| 5. Impact of the COVID-19 pandemic on patient management | 3.09 ± 0.28 | Good | ||||||
| Have ad hoc organizational solutions been implemented for patient management compared to the pre-pandemic era? | 21 (87.5) | 2 (8.3) | 0 (0.0) | 1 (4.2) | 0 (0.0) | 91 | 3.79 ± 0.64 | Good |
| Has therapeutic continuity been ensured within the pathway care? | 20 (83.3) | 4 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 92 | 3.83 ± 0.37 | Good |
| Have technological solutions, such as telemedicine, been adopted for patient follow-up? | 5 (20.8) | 8 (33.3) | 4 (16.7) | 2 (8.3) | 5 (20.8) | 54 | 2.25 ± 1.42 | Acceptable |
| Did all hospitalized patients repeat the screening test for SARS-CoV-2 several times during the hospitalization period? | 11 (45.8) | 0 (0.0) | 1 (4.2) | 1 (4.2) | 11 (45.8) | 47 | 1.96 ± 1.93 | Acceptable |
| Has the correct use of PPE (personal protective equipment) by healthcare professionals and patients been monitored? | 22 (91.7) | 0 (0.0) | 0 (0.0) | 1 (4.2) | 1 (4.2) | 89 | 3.71 ± 0.98 | Good |
| 6. Structural and organizational changes of the CP/UO | 3.10 ± 0.26 | Good | ||||||
| Has the care pathway/hospital ward remained unchanged from an organizational point of view? | 10 (41.7) | 9 (37.5) | 2 (8.3) | 1 (4.2) | 2 (8.3) | 72 | 2.77 ± 1.40 | Acceptable |
| Were outpatient and/or surgical activities guaranteed? | 14 (58.3) | 6 (25.0) | 0 (0.0) | 1 (4.2) | 3 (12.5) | 75 | 3.13 ± 1.36 | Good |
| Has the timing of the transition of a patient from one care setting to another within the care pathway/hospital ward been respected? | 9 (37.5) | 10 (41.7) | 0 (0.0) | 1 (4.2) | 4 (16.7) | 67 | 2.79 ± 1.41 | Acceptable |
| Have there been multidisciplinary discussions about the patients’ health conditions? | 12 (50.0) | 6 (25.5) | 2 (8.3) | 0 (0.0) | 4 (16.7) | 70 | 2.92 ± 1.44 | Acceptable |
| Have structural changes been made to encourage social distancing? | 17 (70.8) | 4 (16.7) | 1 (4.2) | 1 (4.2) | 1 (4.2) | 83 | 3.46 ± 1.04 | Good |
| Have the services relating to non-deferrable diseases been guaranteed? | 20 (83.3) | 2 (8.3) | 0 (0.0) | 1 (4.2) | 1 (4.2) | 87 | 3.63 ± 0.99 | Good |
| 7. Procedures and recommendations for healthcare professionals/users | 3.63 ± 0.22 | Good | ||||||
| Have recommendations for the patients been made clear and visible? | 21 (87.5) | 2 (8.3) | 0 (0.0) | 1 (4.2) | 0 (0.0) | 91 | 3.79 ± 0.64 | Good |
| If yes, or enough, have they been respected? | 13 (54.2) | 11 (45.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 85 | 3.54 ± 0.50 | Good |
| Have recommendations for relatives been made clear and visible? | 22 (91.7) | 1 (4.2) | 0 (0.0) | 1 (4.2) | 0 (0.0) | 92 | 3.83 ± 0.62 | Good |
| If yes, or enough, have they been respected? | 15 (62.5) | 8 (33.3) | 1 (4.2) | 0 (0.0) | 0 (0.0) | 86 | 3.58 ± 0.57 | Good |
| Have recommendations for healthcare professionals been made clear and visible? | 21 (87.5) | 1 (4.2) | 0 (0.0) | 1 (4.2) | 1 (4.2) | 88 | 3.67 ± 0.99 | Good |
| If yes, or enough, have they been respected? | 20 (83.3) | 1 (4.2) | 0 (0.0) | 1 (4.2) | 2 (8.3) | 84 | 3.50 ± 1.22 | Good |
| 8. Training, information and management of health workers in the pandemic era | 3.19 ± 0.26 | Good | ||||||
| Have health care workers involved in care pathways/hospital wards been trained on the dressing-doffing PPE procedures? | 21 (87.5) | 1 (4.2) | 0 (0.0) | 0 (0.0) | 2 (8.3) | 87 | 3.63 ± 1.11 | Good |
| Has the exposed health care personnel been periodically subjected to rhino-pharyngeal swabs to evaluate the possible positivity for SARS-CoV-2? | 21 (87.5) | 2 (8.3) | 0 (0.0) | 0 (0.0) | 1 (4.2) | 90 | 3.75 ± 0.83 | Good |
| Has the staff been equipped with PPE of modulated efficiency with respect to the professional risk to which they have been exposed? | 19 (79.2) | 4 (16.7) | 0 (0.0) | 0 (0.0) | 1 (4.2) | 88 | 3.67 ± 0.85 | Good |
| Have dirty paths and clean access paths to clinical departments been organized? | 10 (41.7) | 3 (12.5) | 0 (0.0) | 0 (0.0) | 11 (45.8) | 49 | 2.04 ± 1.90 | Acceptable |
| Has the corporate anti-COVID vaccination program been performed using the employee booking portal? | 16 (66.7) | 0 (0.0) | 0 (0.0) | 3 (12.5) | 5 (20.8) | 67 | 2.79 ± 1.73 | Acceptable |
| In the company/facility, was the anti-COVID19 vaccination campaign preceded by an information campaign on the technical characteristics, methods of setting up and administering the vaccine? | 20 (83.3) | 0 (0.0) | 0 (0.0) | 2 (8.3) | 2 (8.3) | 82 | 3.42 ± 1.32 | Good |
| Clinical Pathway | COVID Survey Section | Total Score | Mean Score ± DS | Level of Performance * |
|---|---|---|---|---|
| Heart Failure | 486 | 2.54 ± 0.17 | Acceptable | |
| Context analysis | 48 | 2.40 ± 0.34 | Acceptable | |
| Patients access to CP/UO | 48 | 3.20 ± 0.33 | Good | |
| Impact on the treatment of non-COVID patients in the clinical pathway | 34 | 2.27 ± 0.59 | Acceptable | |
| Impact on the treatment of patients also SARS-CoV-2 infected in the Clinical Pathway | 22 | 0.88 ± 0.63 | Not Acceptable | |
| Impact of the COVID-19 pandemic on patient management | 71 | 2.84 ± 0.58 | Acceptable | |
| Structural and organizational changes of the CP/UO | 71 | 2.37 ± 0.59 | Acceptable | |
| Procedures and recommendations for healthcare professionals/users | 96 | 3.20 ± 0.24 | Good | |
| Training, information, and management of health workers in the pandemic era | 96 | 3.20 ± 0.47 | Good | |
| Hereditary Breast-ovarian Cancer | 852 | 3.19 ± 0.12 | Good | |
| Context analysis | 84 | 3.00 ± 0.25 | Good | |
| Patients access to CP/UO | 76 | 3.62 ± 0.34 | Good | |
| Impact on the treatment of non-COVID patients in the clinical pathway | 72 | 3.43 ± 0.32 | Good | |
| Impact on the treatment of patients also SARS-CoV-2 infected in the Clinical Pathway | 29 | 0.83 ± 0.41 | Not Acceptable | |
| Impact of the COVID-19 pandemic on patient management | 117 | 3.34 ± 0.49 | Good | |
| Structural and organizational changes of the CP/UO | 153 | 3.64 ± 0.26 | Good | |
| Procedures and recommendations for healthcare professionals/users | 160 | 3.81 ± 0.21 | Good | |
| Training, information, and management of health workers in the pandemic era | 163 | 3.88 ± 0.22 | Good | |
| Diabetes | 660 | 2.90 ± 0.25 | Acceptable | |
| Context analysis | 54 | 2.25 ± 0.61 | Acceptable | |
| Patients access to CP/UO | 72 | 4.00 ± 0.82 | Good | |
| Impact on the treatment of non-COVID patients in the clinical pathway | 52 | 2.89 ± 0.69 | Acceptable | |
| Impact on the treatment of patients also SARS-CoV-2 infected in the Clinical Pathway | 20 | 0.67 ± 0.33 | Not Acceptable | |
| Impact of the COVID-19 pandemic on patient management | 87 | 2.90 ± 0.70 | Acceptable | |
| Structural and organizational changes of the CP/UO | 115 | 3.19 ± 0.73 | Good | |
| Procedures and recommendations for healthcare professionals/users | 143 | 3.97 ± 0.81 | Good | |
| Training, information and management of health workers in the pandemic era | 119 | 3.31 ± 0.74 | Good | |
| Autism Spectrum Disorders | 634 | 2.81 ± 0.14 | Acceptable | |
| Context analysis | 69 | 2.88 ± 0.34 | Acceptable | |
| Patients access to CP/UO | 70 | 3.89 ± 0.10 | Good | |
| Impact on the treatment of non-COVID patients in the clinical pathway | 47 | 2.61 ± 0.48 | Acceptable | |
| Impact on the treatment of patients also SARS-CoV-2 infected in the Clinical Pathway | 23 | 0.77 ± 0.38 | Not Acceptable | |
| Impact of the COVID-19 pandemic on patient management | 98 | 3.27 ± 0.45 | Good | |
| Structural and organizational changes of the CP/UO | 115 | 3.19 ± 0.39 | Good | |
| Procedures and recommendations for healthcare professionals/users | 127 | 3.53 ± 0.27 | Good | |
| Training, information, and management of health workers in the pandemic era | 85 | 2.36 ± 0.56 | Acceptable |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piane, M.; Bianco, L.; Mancini, R.; Fornelli, P.; Gabriele, A.; Medici, F.; Battista, C.; Greco, S.; Croce, G.; Franceschetti, L.; et al. Impact of the COVID-19 Pandemic on Clinical Pathways for Non-SARS-CoV-2 Related Diseases in the Lazio Region, Italy. Int. J. Environ. Res. Public Health 2022, 19, 635. https://doi.org/10.3390/ijerph19020635
Piane M, Bianco L, Mancini R, Fornelli P, Gabriele A, Medici F, Battista C, Greco S, Croce G, Franceschetti L, et al. Impact of the COVID-19 Pandemic on Clinical Pathways for Non-SARS-CoV-2 Related Diseases in the Lazio Region, Italy. International Journal of Environmental Research and Public Health. 2022; 19(2):635. https://doi.org/10.3390/ijerph19020635
Chicago/Turabian StylePiane, Maria, Lavinia Bianco, Rita Mancini, Paolo Fornelli, Angela Gabriele, Francesco Medici, Claudia Battista, Stefania Greco, Giuseppe Croce, Laura Franceschetti, and et al. 2022. "Impact of the COVID-19 Pandemic on Clinical Pathways for Non-SARS-CoV-2 Related Diseases in the Lazio Region, Italy" International Journal of Environmental Research and Public Health 19, no. 2: 635. https://doi.org/10.3390/ijerph19020635
APA StylePiane, M., Bianco, L., Mancini, R., Fornelli, P., Gabriele, A., Medici, F., Battista, C., Greco, S., Croce, G., Franceschetti, L., Napoli, C., Ronchetti, M., Anibaldi, P., & Banchieri, G. (2022). Impact of the COVID-19 Pandemic on Clinical Pathways for Non-SARS-CoV-2 Related Diseases in the Lazio Region, Italy. International Journal of Environmental Research and Public Health, 19(2), 635. https://doi.org/10.3390/ijerph19020635







