Health Service Needs from a Household Perspective: An Empirical Study in Rural Empty Nest Families in Sinan and Dangyang, China
Abstract
:1. Introduction
2. Methods
2.1. Setting
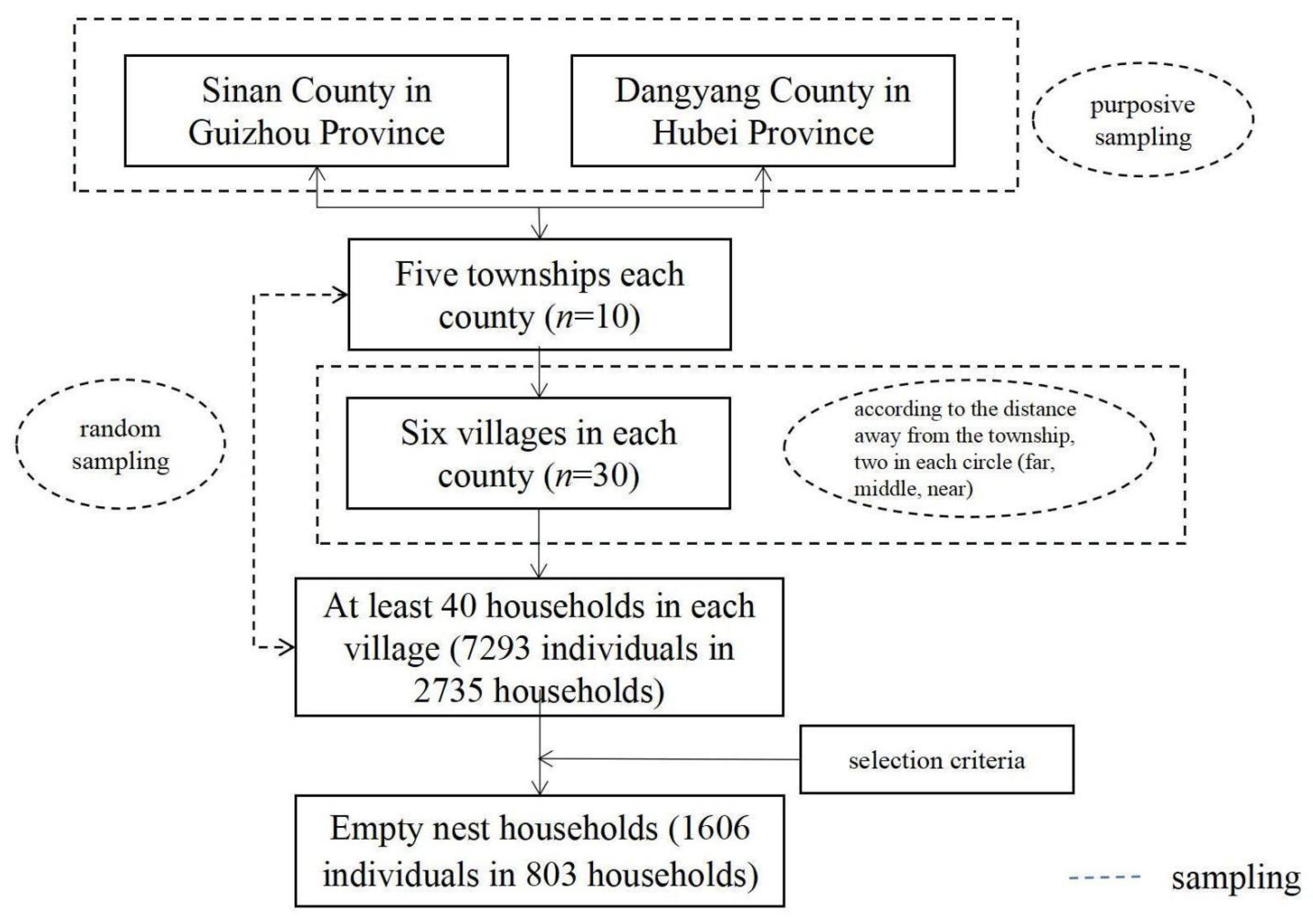
2.2. Study Design and Data Collection
2.3. Health Service Needs
2.4. Health Service Needs Consistency Rates
2.5. Health Service Needs from a Household Perspective
Collective Household Model
3. Results
3.1. Consistency Rates of Different Health Service Needs in Empty Nest Households
3.2. Correlations between Individual’s Health Service Need in Empty Nest Households
3.3. Health Service Needs from a Household Perspective in Empty Nest Households
3.4. Characteristics for Health Service Needs in a Household Unit
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benzein, E.; Johansson, P.; Arestedt, K.F.; Berg, A.; Saveman, B.I. Families’ importance in nursing care: Nurses’ attitudes—An instrument development. J. Fam. Nurs. 2008, 14, 97–117. [Google Scholar] [CrossRef]
- Allred, R.H. Nurses and Families: A Guide to Family Assessment and Intervention. J. Community Health Nurs. 1984, 1, 69–71. [Google Scholar] [CrossRef]
- Epstein, N.B.; Bishop, D.S.; Levin, S. The McMaster model of family functioning. J. Marital Fam. Ther. 1978, 4, 19–31. [Google Scholar] [CrossRef]
- McGoldrick, M.; Carter, E.A.; Garcia-Preto, N. The Expanded Family Life Cycle: Individual, Family, and Social Perspectives; Pearson Allyn & Bacon: Boston, MA, USA, 2013. [Google Scholar]
- The Joint Commission. Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for Hospitals; The Joint Commission: Oakbrook Terrace, IL, USA, 2010. [Google Scholar]
- Leahey, M.; Wright, L.M. Application of the Calgary Family Assessment and Intervention Models: Reflections on the Reciprocity between the Personal and the Professional. J. Fam. Nurs. 2016, 22, 450–459. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.T.; Neves, É.T.B.; Dutra, L.D.C.; Gomes, M.C.; Paiva, S.M.; Abreu, M.H.N.G.; Ferreira, F.M.; Granville-Garcia, A.F. Socioeconomic status and family functioning influence oral health literacy among adolescents. Rev. Saude Publica 2020, 54, 30. [Google Scholar] [CrossRef] [Green Version]
- Çuhadar, D.; Savaş, H.A.; Ünal, A.; Gökpınar, F. Family Functionality and Coping Attitudes of Patients with Bipolar Disorder. J. Relig. Health 2015, 54, 1731–1746. [Google Scholar] [CrossRef]
- Astedt-Kurki, P.; Tarkka, M.T.; Rikala, M.R.; Lehti, K.; Paavilainen, E. Further testing of a family nursing instrument (FAFHES). Int. J. Nurs. Stud. 2009, 46, 350–359. [Google Scholar] [CrossRef]
- Montoro-Gurich, C.; Garcia-Vivar, C. The Family in Europe: Structure, Intergenerational Solidarity, and New Challenges to Family Health. J. Fam. Nurs. 2019, 25, 170–189. [Google Scholar] [CrossRef]
- Prime, H.; Wade, M.; Browne, D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020, 75, 631–643. [Google Scholar] [CrossRef]
- Trougakos, J.P.; Chawla, N.; McCarthy, J.M. Working in a pandemic: Exploring the impact of COVID-19 health anxiety on work, family, and health outcomes. J. Appl. Psychol. 2020, 105, 1234–1245. [Google Scholar] [CrossRef]
- Kilic, S.T.; Oz, F. Family Caregivers’ Involvement in Caring with Cancer and their Quality of Life. Asian Pac. J. Cancer Prev. 2019, 20, 1735–1741. [Google Scholar] [CrossRef] [Green Version]
- Meng, N.; Chen, J.; Cao, B.; Wang, F.; Xie, X.; Li, X. Focusing on quality of life in the family caregivers of patients with schizophrenia from the perspective of family functioning: A cross-sectional study. Medicine 2021, 100, e24270. [Google Scholar] [CrossRef]
- Ohashi, A.; Higuchi, M.; Labeeb, S.A.; Mohamed, A.G.; Chiang, C.; Aoyama, A. Family support for women’s health-seeking behavior: A qualitative study in rural southern Egypt (Upper Egypt). Nagoya J. Med. Sci. 2014, 76, 17–25. [Google Scholar]
- Abelson, J.; Humphrey, A.; Syrowatka, A.; Bidonde, J.; Judd, M. Evaluating Patient, Family and Public Engagement in Health Services Improvement and System Redesign. Healthc. Q. 2018, 21, 61–67. [Google Scholar] [CrossRef]
- Hughes, M.E.; Waite, L.J. Health in household context: Living arrangements and health in late middle age. J. Health Soc. Behav. 2002, 43, 1–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, L.W.; Zhang, J.; Liang, J. Health among the oldest-old in China: Which living arrangements make a difference? Soc. Sci. Med. 2009, 68, 220–227. [Google Scholar] [CrossRef] [Green Version]
- Rosland, A.M.; Piette, J.D. Emerging models for mobilizing family support for chronic disease management: A structured review. Chronic Illn. 2010, 6, 7–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ris, I.; Schnepp, W.; Mahrer Imhof, R. An integrative review on family caregivers’ involvement in care of home-dwelling elderly. Health Soc. Care Community 2019, 27, e95–e111. [Google Scholar] [CrossRef] [Green Version]
- Fu, P.; Wang, Y.; Liu, S.; Li, J.; Gao, Q.; Zhou, C.; Meng, Q.; Sylvia, S. Analysing the preferences for family doctor contract services in rural China: A study using a discrete choice experiment. BMC Fam. Pract. 2020, 21, 148. [Google Scholar] [CrossRef] [PubMed]
- Shang, X.; Huang, Y.; Li, B.; Yang, Q.; Zhao, Y.; Wang, W.; Liu, Y.; Lin, J.; Hu, C.; Qiu, Y. Residents’ Awareness of Family Doctor Contract Services, Status of Contract with a Family Doctor, and Contract Service Needs in Zhejiang Province, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 3312. [Google Scholar] [CrossRef] [Green Version]
- Gu, L.; Zhu, R.; Li, Z.; Zhang, S.; Li, J.; Tian, D.; Sun, Z. Factors Associated with Rural Residents’ Contract Behavior with Village Doctors in Three Counties: A Cross-Sectional Study from China. Int. J. Environ. Res. Public Health 2020, 17, 8969. [Google Scholar] [CrossRef]
- Yuan, S.; Wang, F.; Li, X.; Jia, M.; Tian, M. Facilitators and barriers to implement the family doctor contracting services in China: Findings from a qualitative study. BMJ Open 2019, 9, e032444. [Google Scholar] [CrossRef]
- Bamm, E.L.; Rosenbaum, P. Family-centered theory: Origins, development, barriers, and supports to implementation in rehabilitation medicine. Arch. Phys. Med. Rehabil. 2008, 89, 1618–1624. [Google Scholar] [CrossRef]
- Liu, Y.; Xiao, X.; Peng, C.; Zhao, T.; Wu, Y.; Yu, W.; Ou, L.; Chen, X.; Wu, X.; Xu, D.R.; et al. Development and Implementation of Couple-Based Collaborative Management Model of Type 2 Diabetes Mellitus for Community-Dwelling Chinese Older Adults: A Pilot Randomized Trial. Front. Public Health 2021, 9, 686282. [Google Scholar] [CrossRef] [PubMed]
- Tu, J.; Liao, J. Primary care providers’ perceptions and experiences of family-centered care for older adults: A qualitative study of community-based diabetes management in China. BMC Geriatr. 2021, 21, 438. [Google Scholar] [CrossRef] [PubMed]
- Barnes, M.D.; Hanson, C.L.; Novilla, L.B.; Magnusson, B.M.; Crandall, A.C.; Bradford, G. Family-Centered Health Promotion: Perspectives for Engaging Families and Achieving Better Health Outcomes. Inquiry 2020, 57, 46958020923537. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Li, Y.; Zhang, S.; Gu, L.; Zhang, J.; Li, Z.; Zhang, W.; Tian, D. Does an Empty Nest Affect Elders’ Health? Empirical Evidence from China. Int. J. Environ. Res. Public Health 2017, 14, 463. [Google Scholar] [CrossRef]
- Lv, X.-L.; Jiang, Y.-H.; Sun, Y.-H.; Ren, C.-Z.; Sun, C.-Y.; Sun, L.; Wu, Z.-Q.; Zhao, X. Short form 36-Item Health Survey test result on the empty nest elderly in China: A meta-analysis. Arch. Gerontol. Geriatr. 2013, 56, 291–297. [Google Scholar] [CrossRef]
- Su, D.; Wu, X.-N.; Zhang, Y.-X.; Li, H.-P.; Wang, W.-L.; Zhang, J.-P.; Zhou, L.-S. Depression and social support between China’ rural and urban empty-nest elderly. Arch. Gerontol. Geriatr. 2012, 55, 564–569. [Google Scholar] [CrossRef]
- Liang, Y.; Wu, W. Exploratory analysis of health-related quality of life among the empty-nest elderly in rural China: An empirical study in three economically developed cities in eastern China. Health Qual. Life Outcomes 2014, 12, 59. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H. Who will care for our parents? Changing boundaries of family and public roles in providing care for the aged in urban China. Care Manag. J. 2007, 8, 39–46. [Google Scholar] [CrossRef]
- Chatterji, S.; Byles, J.; Cutler, D.; Seeman, T.; Verdes, E. Health, functioning, and disability in older adults—Present status and future implications. Lancet 2015, 385, 563–575. [Google Scholar] [CrossRef] [Green Version]
- Yang, T.; Chu, J.; Zhou, C.; Medina, A.; Li, C.; Jiang, S.; Zheng, W.; Sun, L.; Liu, J. Catastrophic health expenditure: A comparative analysis of empty-nest and non-empty-nest households with seniors in Shandong, China. BMJ Open 2016, 6, e010992. [Google Scholar] [CrossRef] [PubMed]
- Jing, Z.; Li, J.; Fu, P.P.; Wang, Y.; Yuan, Y.; Zhao, D.; Hao, W.; Yu, C.; Zhou, C. Catastrophic health expenditure among single empty-nest elderly with multimorbidity in rural Shandong, China: The effect of co-occurrence of frailty. Int. J. Equity Health 2021, 20, 23. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Guo, X.; Guo, L.; Li, Z.; Yang, H.; Yu, S.; Sun, G.; Sun, Y. Comprehensive Comparison between Empty Nest and Non-Empty Nest Elderly: A Cross-Sectional Study among Rural Populations in Northeast China. Int. J. Environ. Res. Public Health 2016, 13, 857. [Google Scholar] [CrossRef] [Green Version]
- Fahrenberg, B. Coping with the empty nest situation as a developmental task for the aging female—An analysis of the literature. Z. Gerontol. 1986, 19, 323–335. [Google Scholar] [PubMed]
- Pillay, A.L. Midlife depression and the “empty nest” syndrome in Indian women. Psychol. Rep. 1988, 63, 591–594. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Shu, D.; Dong, B.; Luo, L.; Hao, Q. Anxiety disorders and its risk factors among the Sichuan empty-nest older adults: A cross-sectional study. Arch. Gerontol. Geriatr. 2013, 56, 298–302. [Google Scholar] [CrossRef]
- Cheng, P.; Jin, Y.; Sun, H.; Tang, Z.; Zhang, C.; Chen, Y.; Zhang, Q.; Zhang, Q.; Huang, F. Disparities in prevalence and risk indicators of loneliness between rural empty nest and non-empty nest older adults in Chizhou, China. Geriatr. Gerontol. Int. 2015, 15, 356–364. [Google Scholar] [CrossRef]
- Pressman, S.D.; Gallagher, M.W.; Lopez, S.J. Is the emotion-health connection a “first-world problem”? Psychol. Sci. 2013, 24, 544–549. [Google Scholar] [CrossRef]
- Geisser, M.E.; Roth, R.S.; Theisen, M.E.; Robinson, M.E.; Riley, J.R. Negative affect, self-report of depressive symptoms, and clinical depression: Relation to the experience of chronic pain. Clin. J. Pain 2000, 16, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Tian, J.; Yue, P.; Wang, Y.; Du, X.; Chen, S. Living experience and care needs of Chinese empty-nest elderly people in urban communities in Beijing, China: A qualitative study. Int. J. Nurs. Sci. 2015, 2, 15–22. [Google Scholar] [CrossRef] [Green Version]
- Yuan, Y.; Liu, Y.; Gong, L.; Chen, H.; Zhang, S.; Kitayama, A.; Takashi, E.; Liang, J. Demand Analysis of Telenursing for Community-Dwelling Empty-Nest Elderly Based on the Kano Model. Telemed. E-Health 2021, 27, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Liu, Y.; Su, Z.; Sun, S.; Liu, C.; Ding, W.; Gao, Y. Demands for Telenursing-Based Long-Term Care Among Disabled Older Adults in Qingdao, China: A Cross-Sectional Study. Patient Prefer. Adherence 2021, 15, 1981–1990. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Li, Z.; Pan, Z.; He, R.; Zhang, L. Prevalence and associated factors of self-treatment behaviour among different elder subgroups in rural China: A cross-sectional study. Int. J. Equity Health 2020, 19, 32. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, R.; Woodruff, B.A.; Bilukha, O.; Spiegel, P.B.; Salama, P. Using design effects from previous cluster surveys to guide sample size calculation in emergency settings. Disasters 2006, 30, 199–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, J.; Zhang, G. Research on the application of design effect in complex sampling-taking China’s household survey as an example. J. Appl. Stat. Manag. 2015, 34, 628–635. [Google Scholar]
- Center for Health Statistics and Information, NHFPC. The Fifth National Health Service Survey and Analysis Report; Chinese Union Medical University Press: Beijing, China, 2015.
- Nobile, M. The WHO Definition of health: A critical reading. Med. Law 2014, 33, 33–40. [Google Scholar]
- Meng, Q.; Mills, A.; Wang, L.; Han, Q. What can we learn from China’s health system reform? BMJ 2019, 365, l2349. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y. China’s public health-care system: Facing the challenges. Bull. World Health Organ. 2004, 82, 532–538. [Google Scholar] [PubMed]
- Beaglehole, R.; Bonita, R.; Horton, R.; Adams, O.; McKee, M. Public health in the new era: Improving health through collective action. Lancet 2004, 363, 2084–2086. [Google Scholar] [CrossRef]
- Cui, F.; He, X.; Zhai, Y.; Lyu, M.; Shi, J.; Sun, D.; Jiang, S.; Li, C.; Zhao, J. Application of Telemedicine Services Based on a Regional Telemedicine Platform in China from 2014 to 2020, Longitudinal Trend Analysis. J. Med. Internet Res. 2021, 23, e28009. [Google Scholar] [CrossRef] [PubMed]
- Becker, G.S. Altruism in the Family and Selfishness in the Market Place. Economica 1981, 48, 1–15. [Google Scholar] [CrossRef]
- Cherchye, L.; De Rock, B.; Lewbel, A.; Vermeulen, F. Sharing Rule Identification for General Collective Consumption Models. Econometrica 2015, 83, 2001–2041. [Google Scholar] [CrossRef]
- Wong, J.Y.H.; Wai, A.K.C.; Zhao, S.; Yip, F.; Lee, J.J.; Wong, C.K.H.; Wang, M.P.; Lam, T.H. Association of Individual Health Literacy with Preventive Behaviours and Family Well-Being during COVID-19 Pandemic: Mediating Role of Family Information Sharing. Int. J. Environ. Res. Public Health 2020, 17, 8838. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Kiuchi, T. Association of Health Literacy Levels between Family Members. Front. Public Health 2019, 7, 169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaprio, H.; Suominen, A.L.; Lahti, S. Association between subjective oral health and regularity of service use. Eur. J. Oral Sci. 2012, 120, 212–217. [Google Scholar] [CrossRef]
- National Medical Reform Office Notice on Promoting Guidance for Family Doctor Contract Services. Available online: http://www.mohrss.gov.cn/SYrlzyhshbzb/shehuibaozhang/zcwj/yiliao/201606/t20160615_241854.html (accessed on 20 December 2021). (In Chinese)
- Luttik, M.L. Family Nursing: The family as the unit of research and care. Eur. J. Cardiovasc. Nurs. 2020, 19, 660–662. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Y.; Hu, M. Association of empty nest with depressive symptom in a Chinese elderly population: A cross-sectional study. J. Affect. Disord. 2015, 187, 218–223. [Google Scholar] [CrossRef]
- Ge, D.; Chu, J.; Zhou, C.; Qian, Y.; Zhang, L.; Sun, L. Rural-urban difference in the use of annual physical examination among seniors in Shandong, China: A cross-sectional study. Int. J. Equity Health 2017, 16, 86. [Google Scholar] [CrossRef] [Green Version]
- Sun, X.; Chen, Y.; Tong, X.; Feng, Z.; Wei, L.; Zhou, D.; Tian, M.; Lv, B.; Feng, D. The use of annual physical examinations among the elderly in rural China: A cross-sectional study. BMC Health Serv. Res. 2014, 14, 16. [Google Scholar] [CrossRef] [Green Version]
- Xu, L.J.; Meng, Q.; He, S.W.; Yin, X.L.; Tang, Z.L.; Bo, H.Y.; Lan, X.Y. The effects of health education on patients with hypertension in China: A meta-analysis. Health Educ. J. 2014, 73, 137–149. [Google Scholar] [CrossRef]
- Liu, S.; Liu, Y.; Zhang, T.; Wang, L.; Huang, J.; Liang, H.; Chen, G.; Liu, C.; Zhang, Y. The developing family doctor system: Evidence from the progress of the family doctor signing service from a longitudinal survey (2013–2016) in Pudong New Area, Shanghai. BMC Fam. Pract. 2021, 22, 11. [Google Scholar] [CrossRef] [PubMed]
- Meydanlioglu, A.; Akcan, A.; Oncel, S.; Adibelli, D.; Cicek Gumus, E.; Sarvan, S.; Kavla, I. Prevalence of obesity and hypertension in children and determination of associated factors by CHAID analysis. Arch. Pediatr. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Dongn, S.; Dong, Q.; Chen, H. Mothers’ Parenting Stress, Depression, Marital Conflict, and Marital Satisfaction: The Moderating Effect of Fathers’ Empathy Tendency. J. Affect. Disord. 2022, 299, 682–690. [Google Scholar] [CrossRef]
- Crandall, A.; Novilla, L.K.B.; Hanson, C.L.; Barnes, M.D.; Novilla, M.L.B. The Public Health Family Impact Checklist: A Tool to Help Practitioners Think Family. Front. Public Health 2019, 7, 331. [Google Scholar] [CrossRef]
- Woodman, J.; Simon, A.; Hauari, H.; Gilbert, R. A scoping review of ‘think-family’ approaches in healthcare settings. J. Public Health 2020, 42, 21–37. [Google Scholar] [CrossRef]
- Samanta, T.; Chen, F.; Vanneman, R. Living Arrangements and Health of Older Adults in India. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2014, 70, 937–947. [Google Scholar] [CrossRef]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. 2015. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication (accessed on 20 December 2021).
- Hu, C.; Yu, W.; Lv, Y.; Chen, H.; Deng, Q.; Zhang, L. Study on the Health Status and Health Service Utilization of the Elderly of a Remote and Poor Village in a Mountainous Area in Jinzhai, Anhui. Int. J. Environ. Res. Public Health 2017, 14, 408. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Zhang, L. Poverty and health-related quality of life: A cross-sectional study in rural China. Health Qual. Life Outcomes 2020, 18, 153. [Google Scholar] [CrossRef]

| Individual 1 | H1 | H2 | H3 | H4 | H5 | H6 | H7 |
|---|---|---|---|---|---|---|---|
| Individual 2 | |||||||
| H1 | 0.404 ** | 0.049 | 0.034 | 0.063 | −0.044 | −0.086 | −0.045 |
| H2 | 0.059 | 0.003 | 0.004 | 0.026 | −0.036 | 0.006 | 0.025 |
| H3 | 0.059 | 0.005 | 0.177 ** | 0.037 | 0.002 | 0.009 | 0.039 |
| H4 | 0.003 | 0.033 | −0.004 | 0.286 ** | 0.115 ** | −0.013 | 0.015 |
| H5 | −0.032 | −0.018 | 0.037 | 0.104 ** | 0.265 ** | −0.018 | 0.051 |
| H6 | 0.005 | 0.022 | 0.026 | 0.015 | 0.024 | 0.053 | 0.036 |
| H7 | 0.007 | 0.027 | 0.031 | −0.002 | 0.085 * | −0.035 | 0.220 ** |
| Characteristics | Categories | Individual 1 | Individual 2 |
|---|---|---|---|
| Subjective health score | Mean score | 69.95 | 67.69 |
| Objective health score | Mean score | 0.887 | 0.865 |
| Educational level | Less than primary school | 50.7% | 60.0% |
| Junior and senior high school | 47.8% | 36.6% | |
| More than undergraduate | 0.3% | 0.8% | |
| Householder | Yes | 74.5% | 27.9% |
| No | 25.4% | 71.8% |
| Health Service Needs | Public Needs as Household Needs | Individual Needs as Household Needs | Total | ||
|---|---|---|---|---|---|
| Individual 1 | Individual 2 | Total | |||
| H1 | 73 (9.8) | 11 (52.4) | 15 (60.0) | 26 (56.5) | 99 (12.4) |
| H2 | 39 (5.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 39 (4.9) |
| H3 | 1 (0.1) | 1 (4.8) | 0 (0.0) | 1 (2.2) | 2 (0.3) |
| H4 | 323 (43.3) | 15 (71.4) | 15 (60.0) | 30 (65.2) | 353 (44.2) |
| H5 | 186 (24.9) | 16 (76.2) | 13 (52.0) | 29 (63.0) | 215 (26.9) |
| H6 | 29 (3.9) | 7 (33.3) | 1 (4.0) | 8 (17.4) | 37 (4.6) |
| H7 | 130 (18.1) | 11 (52.4) | 10 (40.0) | 21 (45.7) | 151 (18.9) |
| Public Needs as Household Needs | ||||||
| n | % | |||||
| Family characteristics | Householder’s gender | Male | 701 | 94.0 | ||
| Female | 45 | 6.0 | ||||
| Two-week prevalence | both | 154 | 20.7 | |||
| One individual | 335 | 47.7 | ||||
| None | 236 | 31.7 | ||||
| Chronic disease | Both | 228 | 30.7 | |||
| One individual | 384 | 51.7 | ||||
| None | 131 | 17.6 | ||||
| Individual Needs as Household Needs | ||||||
| Individual 1 | Individual 2 | |||||
| n | % | n | % | |||
| Individual characteristics | Householder | Yes | 19 | 90.5 | 0 | 0.0 |
| No | 2 | 9.5 | 25 | 100.0 | ||
| Two-week prevalence | Yes | 21 | 100.0 | 25 | 100.0 | |
| No | 0 | 0.0 | 0 | 0.0 | ||
| Chronic disease | Yes | 16 | 76.2 | 22 | 89.0 | |
| No | 5 | 23.8 | 3 | 12.0 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, X.; Zhang, L. Health Service Needs from a Household Perspective: An Empirical Study in Rural Empty Nest Families in Sinan and Dangyang, China. Int. J. Environ. Res. Public Health 2022, 19, 628. https://doi.org/10.3390/ijerph19020628
Cheng X, Zhang L. Health Service Needs from a Household Perspective: An Empirical Study in Rural Empty Nest Families in Sinan and Dangyang, China. International Journal of Environmental Research and Public Health. 2022; 19(2):628. https://doi.org/10.3390/ijerph19020628
Chicago/Turabian StyleCheng, Xueyan, and Liang Zhang. 2022. "Health Service Needs from a Household Perspective: An Empirical Study in Rural Empty Nest Families in Sinan and Dangyang, China" International Journal of Environmental Research and Public Health 19, no. 2: 628. https://doi.org/10.3390/ijerph19020628
APA StyleCheng, X., & Zhang, L. (2022). Health Service Needs from a Household Perspective: An Empirical Study in Rural Empty Nest Families in Sinan and Dangyang, China. International Journal of Environmental Research and Public Health, 19(2), 628. https://doi.org/10.3390/ijerph19020628






