Diabetes Capabilities for the Healthcare Workforce Identified via a 3-Staged Modified Delphi Technique
Abstract
1. Introduction
- Identify and understand the different non-medical healthcare professional practice levels used to deliver diabetes care in Australia;
- Identify the capabilities required to deliver quality, safe diabetes education and care;
- Increase the health workforce’s capacity to manage diabetes.
2. Materials and Methods
2.1. Methodological Approach
2.2. Theoretical Framework
2.3. Research Characteristics and Reflexivity
2.4. Setting
2.5. Sampling Strategy
- A CDE for five years or more;
- In a position whose focus of employment for the past five years or more was diabetes education and care or/and research.
2.6. Ethical Considerations
2.7. Data Collection Methods
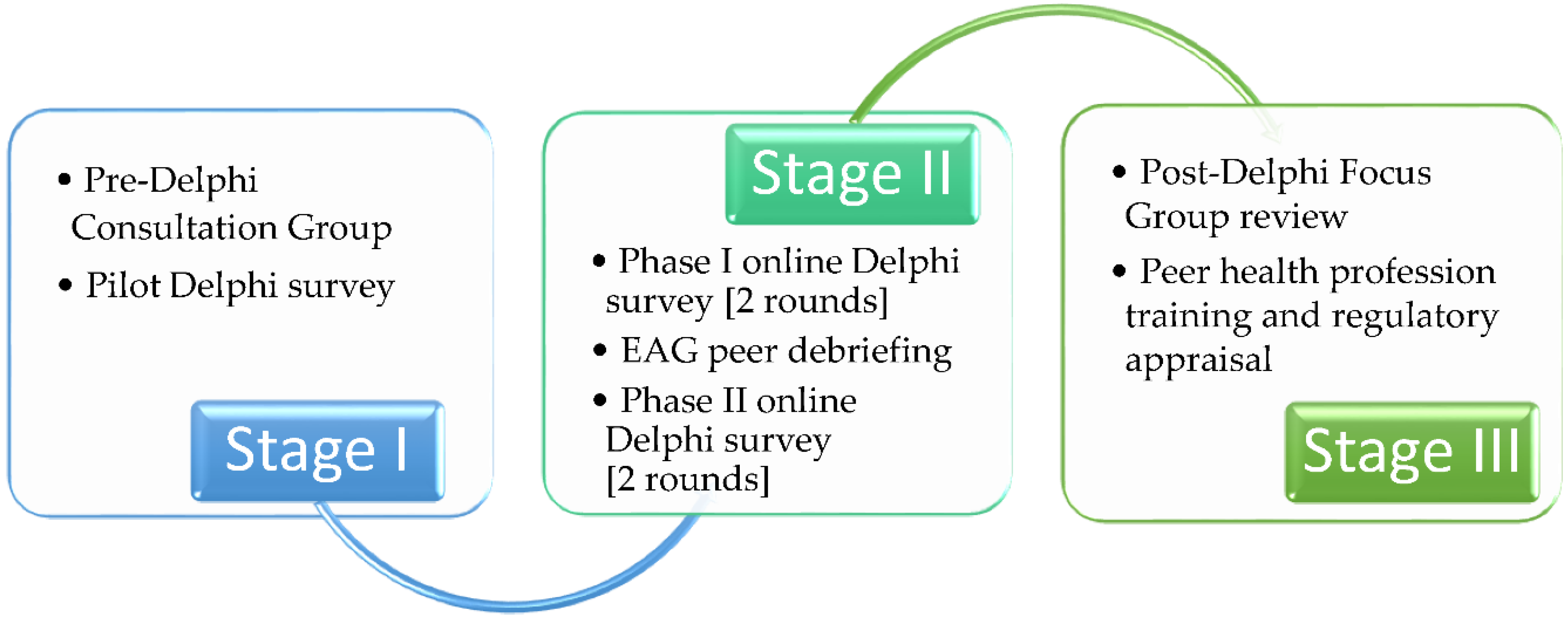
2.7.1. Stage I
2.7.2. Stage II
- No capability components were overlooked;
- Capabilities identified would allow workforce capacity growth;
- The volume of data collected during each method was managed;
- An accurate model describing practice levels was chosen.
2.7.3. Stage III
2.8. Data Analysis
2.8.1. Qualitative Data Analysis
- The level of analysis used was word sense, phrase, or sentences of similar meanings;
- Flexibility in the coding process with no predefined number or list of concepts;
- Concepts would be coded for their content, not frequency;
- Concepts would be developed to align with study questions and aims as they emerged into categories.
2.8.2. Quantitative Data Analyses
2.8.3. Techniques to Enhance Trustworthiness
3. Results
3.1. STAGE I: Pre-Delphi Consultation
3.1.1. Findings to Inform the Framework
- Difficulties in identifying role boundary delineation between disciplines;
- Potential unsafe practices in diabetes care.
3.1.2. Findings to Inform the Delphi Survey
3.1.3. Findings for Policy Advice
3.2. STAGE 2: Delphi Survey
3.2.1. Delphi Survey Phase I Findings
3.2.2. Delphi Survey Phase 2 Findings
3.3. STAGE III: Post-Delphi External Appraisal
4. Discussion
4.1. Workforce Implications
4.1.1. Workforce Diabetes Health Literacy and Preparedness for Diabetes Care
4.1.2. Capability Framework for Diabetes Education and Care
4.1.3. Mentoring and Practice
4.2. Policy Implications
4.2.1. Medicine Management in Diabetes Care
4.2.2. Promoting Viability of Private Practice Workforce for Diabetes
4.2.3. Orientating Healthcare Organisations for Capability-Based Learning
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bach, L.; Ekinci, E.; Engler, D.; Gilfillan, C.; Hamblin, S.; Maclsaac, R.; Soldatos, G.; Steele, C.; Ward, G.; Wyatt, S. The high burden of inpatient diabetes mellitus: The Melbourne public hospitals diabetes inpatient audit. MJA 2014, 201, 334–338. [Google Scholar] [CrossRef] [PubMed]
- National Health Performance Authority. Healthy Communities: Frequent GP Attenders and Their Use of Health Services in 2012–2013 (Technical Supplement). 2015. Available online: https://apo.org.au/node/53739 (accessed on 1 June 2020).
- Hendrieckx, C.; Halliday, J.; Beeney, L.; Speight, J. Diabetes and Emotional Health: A Practical Guide for Health Professionals Supporting Adults with Type 1 Diabetes or Type 2 Diabetes, 2nd ed.; National Diabetes Services Scheme (NDSS): Canberra, Australia, 2020; Available online: https://www.ndss.com.au/health-professionals/resources/ (accessed on 10 November 2021).
- Ng, A.; Crowe, T.; Ball, K.; Rasmussen, B. Transitional needs of Australian young adults with type 1 diabetes: Mixed methods study. JMIR Diabetes 2017, 2, e29. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Australian Burden of Disease Study: Impact and Causes of Illness and Death in Australia 2015 and Disease Expenditure in Australia. 2019. Available online: https://www.aihw.gov.au/reports/health-welfare-expenditure/disease-expenditure-australia/contents/summary (accessed on 1 June 2020).
- Lee, C.; Colagiuri, R.; Magliano, D.; Cameron, A.; Shaw, J.; Zimmet, P.; Colagiuri, S. The cost of diabetes in adults in Australia. Diabetes Res. Clin. Pract. 2013, 99, 385–390. [Google Scholar] [CrossRef]
- Callander, E.J.; Corscadden, L.; Levesque, J.F. Out-of-pocket healthcare expenditure and chronic disease—do Australians forgo care because of the cost? Aust. J. Prim. Health 2017, 23, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Australian Diabetes Educators Association. Workforce in Diabetes Education. 2017. Available online: https://members.adea.com.au/resources-2/workforce-in-diabetes-education/ (accessed on 1 June 2020).
- Australian Diabetes Educators Association. Credentialling Process. 2021. Available online: https://www.adea.com.au/Credentialling/Initial_Credentialling (accessed on 10 December 2021).
- Fountaine, T.; Bennett, C. Health Care Homes: Lessons from the Diabetes Care Project. MJA 2016, 205, 389–391. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Queensland Health-Clinical Excellence Division. Allied Health Expanded Scope Strategy 2016–2021, Report. 2016. Available online: https://clinicalexcellence.qld.gov.au/priority-areas/service-improvement/allied-health-expanded-scope-practice (accessed on 1 June 2020).
- Department of Health. Best-Practice Examples of Chronic Disease Management in Australia. 2017. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/health-care-homes-best-practice (accessed on 10 November 2021).
- Australia Government-Department of Health. Australian National Diabetes Strategy 2021–2030, Technical Report. 2021. Available online: https://www.health.gov.au/resources/publications/australian-national-diabetes-strategy-2021–2030 (accessed on 12 December 2021).
- Rushforth, B.; McCrorie, C.; Glidewell, L.; Midgley, E.; Foy, R. Barriers to effective management of type 2 diabetes in primary care: Qualitative systematic review. Br. J. Gen. Pract. 2016, 66, e114–e127. [Google Scholar] [CrossRef] [PubMed]
- Furler, J.; O’Neal, D.; Speight, J.; Manski-Nankervis, J.; Gorelik, A.; Holmes-Truscott, E.; Ginnivan, L.; Young, D.; Best, J.; Patterson, E.; et al. Supporting Insulin Initiation in Type 2 Diabetes in Primary Care: Results of the Stepping Up Pragmatic Cluster RCT. BMJ 2017, 356, j783. [Google Scholar] [CrossRef]
- Hollis, M.; Glaister, K.; Lapsley, J. Do practice nurses have the knowledge to provide diabetes self-management education? Contemp. Nurse 2014, 46, 234–241. [Google Scholar] [CrossRef]
- Ashton, H.; Wynen, M. Enhancing primary healthcare nurses’ diabetes care. Nurs. N. Z. 2016, 22, 25–51. [Google Scholar]
- Phillips, A. Practice nurses need better diabetes education to meet service and individual needs. Pract. Nurs. 2019, 30, 555–557. [Google Scholar] [CrossRef]
- Lin, S.; Ayre, J.; Muscat, D.M. How readable are Australian multilingual diabetes patient education materials? An evaluation of national English-language source texts. Pub. Health Res. Prac. 2020, 30, 3012002. [Google Scholar] [CrossRef]
- Australian Institute of Health Welfare. Aboriginal and Torres Strait Islander Health Performance Framework 2017 Report: Northern Territory, Cat. No. IHW 186. 2017. Available online: https://www.aihw.gov.au/reports/indigenous-health-welfare/health-performance-framework-2017-nt/contents/table-of-contents (accessed on 3 August 2020).
- Handtke, O.; Schilgen, B.; Mösko, M. Culturally Competent Healthcare—A Scoping Review of Strategies Implemented in Healthcare Organizations and a Model of Culturally Competent Healthcare Provision. PLoS ONE 2019, 14, e0219971. [Google Scholar] [CrossRef]
- Caballero, A. The “A to Z” of Managing Type 2 Diabetes in Culturally Diverse Populations. Front. Endocrinol. 2018, 9, 479. [Google Scholar] [CrossRef]
- Burrow, S.; Ride, K. Review of diabetes among Aboriginal and Torres Strait Islander people. Aust. Indig. HealthInfoNet 2016. Available online: https://healthinfonet.ecu.edu.au/healthinfonet/getContent.php?linkid=590810&title=Review+of+diabetes+among+Aboriginal+and+Torres+Strait+Islander+people (accessed on 1 June 2020).
- Greenwood, M.; de Leeuw, S.; Lindsay, N. Challenges in health equity for Indigenous peoples in Canada. Lancet 2018, 391, 1645–1648. [Google Scholar] [CrossRef]
- Department of Health. Health Workforce: The Government is Committed to Ensuring Australia has a World Class Health System, Supported by a Highly Trained, Qualified and Well Distributed Health Workforce. 2019. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/Health%20Workforce-2 (accessed on 3 August 2021).
- National Rural Health Commissioner. National Rural Health Commissioner-Final Report, Technical Report. 2020. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/National-Rural-Health-Commissioner-publications (accessed on 5 May 2021).
- Gunton, J.; Cheung, N.W.; Davis, T.; Colagiuri, S.; Zoungas, S. A New Blood Glucose Management Algorithm for Type 2 Diabetes: A Position Statement of the Australian Diabetes Society. 2016. Available online: https://www.mja.com.au/journal/2014/201/11/new-blood-glucose-management-algorithm-type-2-diabetes-position-statement (accessed on 1 June 2020).
- Pease, A.J.; Andrikopoulos, S.; Abraham, M.B.; Craig, M.E.; Fenton, B.; Overland, J.; Price, S.; Simmons, D.; Ross, G.P. Utilisation, access and recommendations regarding technologies for people living with type 1 diabetes. Med. J. Aust. 2021, 215, 473–478. [Google Scholar] [CrossRef]
- Department of Health. National Medical Workforce Strategy: Scoping Framework, Report. 2019. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/Health%20Workforce-nat-med-strategy (accessed on 1 June 2020).
- Diabetes Australia. Australian Diabetes Map. 2021. Available online: https://www.ndss.com.au/about-the-ndss/diabetes-facts-and-figures/australian-diabetes-map/ (accessed on 10 November 2021).
- Australian Institute of Health and Welfare. Insulin Pump Use in Australia, Diabetes Series No.18. Cat. No. CVD 58. 2012. Available online: https://www.aihw.gov.au/getmedia/983a6c0e-55f2-465f-8bdb-d211704523a4/14454.pdf.aspx?inline=true (accessed on 1 June 2020).
- Bhogal, H. Insulin Pump Usage—Type 1 Diabetes: 31/12/2019 and 31/12/2012, Report. 2020. Available online: https://www.ndss.com.au (accessed on 8 October 2020).
- Simmons, D.; Deakin, T.; Walsh, N.; Turner, B.; Lawrence, S.; Priest, L.; George, S.; Vanerpool, G.; McArdle, J.; Rylance, A.; et al. Competency frameworks in diabetes. Diab. Med. 2015, 32, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Murfet, G. A Consensus Approach to Building Diabetes Capabilities in the Healthcare Workforce. Ph.D. Thesis, Deakin University, Burwood, Australia, 2 November 2021. Available online: https://dro.deakin.edu.au/view/DU:30159402 (accessed on 2 November 2021).
- Australian Public Service Commission. Building Capability: A Framework for Managing Learning and Development in the APS. Available online: https://www.apsc.gov.au/building-capability-framework-managing-learning-and-development-aps (accessed on 10 November 2021).
- Burcharth, A.; Præst Knudsen, M.; Søndergaard, H. The role of employee autonomy for open innovation performance. Bus. Proc. Mg. J. 2017, 23, 1245–1269. [Google Scholar] [CrossRef]
- Brunner, M.; McGregor, D.; Keep, M.; Janssen, A.; Spallek, H.; Quinn, D.; Jones, A.; Tseris, E.; Yeung, W.; Togher, L.; et al. An eHealth capabilities framework for graduates and health professionals: Mixed-methods study. J. Med. Internet Res. 2018, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Diamond, I.; Grant, R.; Feldman, B.; Pencharz, P.; Ling, S.; Moore, A.; Wales, P. Defining consensus: A systematic review recommends methodologic criteria for reporting of Delphi studies. J. Clin. Epid. 2014, 67, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Courtenay, M.; Deslandes, R.; Harries-Huntley, G.; Hodson, K.; Morris, G. Classic e-Delphi survey to provide national consensus and establish priorities with regards to the factors that promote the implementation and continued development of non-medical prescribing within health services in Wales. BMJ 2018, 8, e024161. [Google Scholar] [CrossRef] [PubMed]
- Waggoner, J.; Carline, J.; Durning, S. Is there a consensus-on-consensus methodology? Descriptions and recommendations for future consensus research. Acad. Med. 2016, 91, 663–668. [Google Scholar] [CrossRef] [PubMed]
- King, O.; Nancarrow, S.; Grace, S.; Borthwick, A. Diabetes educator role boundaries in Australia: A documentary analysis. J. Foot Ank. Res. 2017, 10, 28. [Google Scholar] [CrossRef]
- Benner, P. Using the Dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. Bull. Sci. Technol. Soc. 2004, 24, 188–199. [Google Scholar] [CrossRef]
- Ericsson, K.A.; Harwell, K. Deliberate practice and proposed limits on the effects of practice on the acquisition of expert performance: Why the original definition matters and recommendations for future research. Front. Psychol. 2019, 10, 1–18. [Google Scholar] [CrossRef]
- Robertson, P. Towards a capability approach to careers: Applying Amartya Sen’s thinking to career guidance and development. Int J. Educ. Vocat. Guid. 2015, 15, 75–88. [Google Scholar] [CrossRef]
- Kayrooz, C.; Trevitt, C. Research in Organisations and Communities: Tales from the Real World; Allen & Unwin: Sydney, Australia, 2005. [Google Scholar]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quan. 2018, 52, 1893–1907. [Google Scholar] [CrossRef] [PubMed]
- Webb, C.; Kevern, J. Focus groups as a research method: A critique of some aspects of their use in nursing research. J. Adv. Nurs. 2001, 33, 798–805. [Google Scholar] [CrossRef]
- Lowry, P.; Roberts, T.; Romano, N.; Cheney, P.; Hightower, R. The impact of group size and social presence on small-group communication: Does computer-mediated communication make a difference? Small Group Res. 2006, 37, 631–661. [Google Scholar] [CrossRef]
- Erlingsson, C.; Brysiewicz, P. A hands-on guide to doing content analysis. Afr. J. Emerg. Med. 2017, 7, 93–99. [Google Scholar] [CrossRef]
- Blair, E. A reflexive exploration of two qualitative data coding techniques. J. Methods Meas. Soc. Sci. 2015, 6, 14–29. [Google Scholar] [CrossRef]
- Hutchings, A.; Raine, R.; Sanderson, C.; Black, N. An experimental study of determinants of the extent of disagreement within clinical guideline development groups. Qual. Saf. Health Care 2005, 14, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Noble, H.; Smith, J. Issues of validity and reliability in qualitative research. Evid.-Based Nurs. 2015, 18. [Google Scholar] [CrossRef] [PubMed]
- Levitt, H.; Motulsky, S.; Wertz, F.; Morrow, S.; Ponterotto, J. Recommendations for designing and reviewing qualitative research in psychology: Promoting methodological integrity. Qual. Psychol. 2017, 4, 2–22. [Google Scholar] [CrossRef]
- Naccarella, L.; Wraight, B.; Gorman, D. Is health workforce planning recognising the dynamic interplay between health literacy at an individual, organisation and system level? Aust. Health Rev. 2016, 40, 33–35. [Google Scholar] [CrossRef]
- Australian Commission on Safety and Quality Health Care. Health Literacy. 2019. Available online: https://www.safetyandquality.gov.au/our-work/patient-and-consumer-centred-care/health-literacy (accessed on 3 August 2021).
- Nathan, D.; Bayless, M.; Cleary, P.; Genuth, S.; Gubitosi-Klug, R.; Lachin, J.M.; Lorenzi, G.; Zinman, B.; DCCT/EDIC Research Group. Diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: Advances and contributions. Diabetes 2013, 62, 3976–3986. [Google Scholar] [CrossRef]
- Allied Health Specialist Consultants. National Diabetes Education Review, Report. 2018. Available online: https://www.adea.com.au/contact-us/ (accessed on 1 June 2020).
- Wheelahan, L. Rethinking skills development: Moving beyond competency-based training. In The Oxford Handbook of Skills and Training; Buchanan, J., Finegold, D., Mayhew, K., Warhurst, C., Eds.; Oxford University Press: Oxford, UK, 2017; pp. 636–651. Available online: https://www-oxfordhandbooks-com.ezproxyf.deakin.edu.au/view/10.1093/oxfordhb/9780199655366.001.0001/oxfordhb-9780199655366-e-30 (accessed on 3 March 2021).
- Robeyns, I.; Morten, F. The Capability Approach. In The Stanford Encyclopedia of Philosophy; Zalta, E., Ed.; 2020; Available online: https://plato.stanford.edu/archives/win2020/entries/capability-approach/ (accessed on 3 August 2021).
- Litchman, M.; Ryan, D.; Yehl, K.; Rinker, J.; Burke, S. Developing the 2020 Diabetes Care & Education Specialist Competencies: A Modified Delphi Study. Diabetes Educ. 2020, 46, 378–383. [Google Scholar] [CrossRef]
- Australian Diabetes Educators Association. The National Diabetes Nursing Education Framework. 2020. Available online: https://www.adea.com.au/ndss/the-national-diabetes-nursing-education-framework/ (accessed on 3 August 2021).
- TREND-UK. Integrated Career and Competency Framework for Adult Diabetes Nursing, 5th ed.; 2019; Available online: https://www.knowdiabetes.org.uk/professional/trend-uk/ (accessed on 1 June 2020).
- United Kingdom Clinical Pharmacy Association. An Integrated Career and Competency Framework for Pharmacists in Diabetes. 2018. Available online: https://www.diabetes.org.uk/professionals/training--competencies/competencies (accessed on 1 June 2020).
- McCardle, J.; Atkin, L.; Bowen, G.; Chadwick, P.; Game, F.; Fox, M.; Pankhurst, C.; Sharman, D.; Stang, D.; Wylie, D. Capability Framework for Integrated Diabetic Lower Limb Care: A User’s Guide; OmniaMed Communications Ltd.: London, UK, 2019; Available online: www.diabetesonthenet.com (accessed on 1 June 2020).
- Aotearoa College of Diabetes Nurses. National Diabetes Nursing Knowledge and Skills Framework. 2018. Available online: https://www.nzno.org.nz/groups/colleges_sections/colleges/aotearoa_college_of_diabetes_nurses/education#Framework (accessed on 1 June 2020).
- Lozano, J.; Boni, A.; Peris, J.; Hueso, A. Competencies in Higher Education. J. Philos. Educ. 2012, 46, 132–147. [Google Scholar] [CrossRef]
- Browne, J.; Thorpe, S.; Tunny, N.; Adams, K.; Palermo, C. A qualitative evaluation of a mentoring program for Aboriginal health workers and allied health professionals. Aust. N. Z. J. Public Health 2013, 37, 457–462. [Google Scholar] [CrossRef]
- Langloh de Dassel, J.; Ralph, A.; Cass, A. A systematic review of adherence in Indigenous Australians: An opportunity to improve chronic condition management. Health Serv. Res. 2017, 17, 845. [Google Scholar] [CrossRef]
- Krass, I.; Schieback, P.; Dhippayom, T. Adherence to diabetes medication: A systematic review. Diabet. Med. 2015, 32, 725–737. [Google Scholar] [CrossRef]
- Morton, J.; Ilomäki, J.; Magliano, D.; Shaw, J. The association of socioeconomic disadvantage and remoteness with receipt of T2D medications in Australia: A nationwide registry study. Diabetologia 2020. [Google Scholar] [CrossRef]
- Carranza, A.; Munoz, P.; Nash, A. Comparing quality of care in medical specialties between nurse practitioners and physicians. J. Am. Assoc. Nurse Pract. 2020, 33, 184–193. [Google Scholar] [CrossRef]
- Currie, J.; Chiarella, M.; Buckley, T. Privately practising nurse practitioners’ provision of care subsidised through the Medicare Benefits Schedule and the Pharmaceutical Benefits Scheme in Australia: Results from a national survey. Aust. Health Rev. 2019, 43, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Rinker, J.; Dickinson, J.; Litchman, M.; Williams, A.; Kolb, L.; Cox, C.; Lipman, R. The 2017 diabetes educator and the diabetes self-management education national practice survey. Diabetes Educ. 2018, 44, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Hicks, D.; James, J. A diabetes specialist nurse audit within NHS England. Pract. Diabetes 2020, 37, 173–176. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Private Health Insurance. 2020. Available online: https://www.aihw.gov.au/reports/australia-health/private-health-insurance (accessed on 10 November 2021).
- Rybnicek, R.; Bergner, S.; Gutschelhofer, A. How individual needs influence motivation effects: A neuroscientific study on McClelland’s need theory. Rev. Manag. Sci 2019, 13, 443–482. [Google Scholar] [CrossRef]
- Australian Diabetes Educators Association. Annual Report 2014–2015. 2015. Available online: https://www.adea.com.au/wp-content/uploads/2016/09/Annual-Report-2015-final-web12082015.pdf (accessed on 1 June 2020).
- Australian Diabetes Educators Association. National Core Competencies for Aboriginal and/or Torres Strait Islander Diabetes Health Workers and Diabetes Health Practitioners. 2018. Available online: https://www.adea.com.au/resources/standards-position-statements-and-other-resources/standards/ (accessed on 1 June 2020).
- Flanagan, T.; Ashmore, R.; Banks, D.; MacInnes, D. The Delphi method: Methodological issues arising from a study examining factors influencing the publication or non-publication of mental health nursing research. Ment. Health Rev. J. 2016, 21, 85–94. [Google Scholar] [CrossRef]

| Diabetes capabilities for practice levels one to three. The capabilities focus on awareness or promotion and are defined as: |
| Displays clinical assessment capacities: demonstrates foundational skills and is developing clinical assessment skills relevant to diabetes to assist with diagnosis and care and identify health status changes. |
| Supports diabetes self-management education: promotes, assists, and encourages self-management considering the needs, goals, and life experiences of the person with diabetes using teaching skills and a structured decision-making process guided by evidence and an understanding of health literacy. |
| Builds therapeutic relationships: develops intentional connections focused on person-centeredness and shared decision-making between a healthcare professional and an individual requiring diabetes support; the positive relationship engaged for effecting a beneficial change towards an individual’s goal. |
| Communicates with influence: informs with the intention to affect behaviour change; to inspire, motivate, encourage, guide, and advocate for people living with diabetes or prediabetes. |
| Supports counselling to achieve the best outcomes: uses supportive counselling techniques within an empowerment framework when guidance on actions is required and identifies mental health issues in people living with diabetes, such as diabetes-related distress or burnout and depression. |
| Supports quality use of medicines (QUM): demonstrates QUMs in a supportive role and identifies potential medicine-related risks and benefits. |
| Displays quality use of diabetes technology: demonstrates a supportive role with individuals using technology and identifies potential risks. |
| Supports care coordination: assists in care coordination and transition as directed or is involved in developing and implementing a care plan for the management of diabetes and facilitates appropriate services in conjunction with a medical team. |
| Achieves quality: displays a supportive role within quality and research activities and incorporates evidence in all practice elements. |
| Diabetes capabilities for practice levels four to seven. The capabilities focus on diabetes healthcare professionals who work at an advanced practice level and possess adept diabetes skills in diabetes care and education, and the capabilities are defined as: |
| Exemplifies clinical assessment capacities: advanced assessment skills and knowledge, clinical acumen, and reflection in and on practice to enable more comprehensive and individualised assessment for the person with complex diabetes issues and accumulative comorbidities. |
| Shapes diabetes self-management education (DSME), support and care: competent to design, implement, deliver, and evaluate structured DSME. Influences the continuous development of improved diabetes care skills in consumers and practices to optimise DSME, support, and care. Innovative and leads changes; promotes and develops processes to support improvement in health literacy. |
| Builds therapeutic relationships: adept at developing positive relationships between healthcare professionals and individuals requiring diabetes support through structured shared decision-making. Mentors others and incorporates evidence into local protocols, guidelines, and the organisation to better engage with people living with diabetes and their carers and effect beneficial change. |
| Communicates with influence and leadership: proficient at communicating with the intention to achieve an effect: to listen, inspire, motivate, and encourage both the consumer and other healthcare professionals. Leads with purpose and promotes wide-reaching advocacy for people living with diabetes. |
| Exemplifies counselling to achieve the best outcomes: adept at using supportive and empowering counselling techniques and implements significant evidence into guidelines, protocols, and the organisation. Proficient at detecting mental health issues early, such as diabetes-related distress, diabetes burnout, and depression. |
| Exemplifies quality use of diabetes technology: proficient or regarded as an expert at teaching, operating, and monitoring diabetes technology via different processes, i.e., providing self-management education, technology advice and care, and, in some cases, prescribing if the device administers a medicine. |
| Exemplifies QUMs: proficient or regarded as an expert at ensuring diabetes medicines are used safely when needed. Delivers comprehensive medicines management, including essential elements such as rigorous monitoring and de-prescribing when indicated. |
| Leads care coordination: adeptly coordinates relevant stakeholders involved in the consumer’s care to deliver appropriate healthcare services promptly and efficiently. Aware of the specific requirements of vulnerable groups and people with complex diabetes issues and monitors and evaluates outcomes. |
| Cultivates quality through leadership and research: identifies, engages in, mentors, and leads research and quality and safety improvement activities to identify ways to improve diabetes education and care. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murfet, G.; Ostaszkiewicz, J.; Rasmussen, B. Diabetes Capabilities for the Healthcare Workforce Identified via a 3-Staged Modified Delphi Technique. Int. J. Environ. Res. Public Health 2022, 19, 1012. https://doi.org/10.3390/ijerph19021012
Murfet G, Ostaszkiewicz J, Rasmussen B. Diabetes Capabilities for the Healthcare Workforce Identified via a 3-Staged Modified Delphi Technique. International Journal of Environmental Research and Public Health. 2022; 19(2):1012. https://doi.org/10.3390/ijerph19021012
Chicago/Turabian StyleMurfet, Giuliana, Joan Ostaszkiewicz, and Bodil Rasmussen. 2022. "Diabetes Capabilities for the Healthcare Workforce Identified via a 3-Staged Modified Delphi Technique" International Journal of Environmental Research and Public Health 19, no. 2: 1012. https://doi.org/10.3390/ijerph19021012
APA StyleMurfet, G., Ostaszkiewicz, J., & Rasmussen, B. (2022). Diabetes Capabilities for the Healthcare Workforce Identified via a 3-Staged Modified Delphi Technique. International Journal of Environmental Research and Public Health, 19(2), 1012. https://doi.org/10.3390/ijerph19021012







