The Economic Burden Associated with Depressive Symptoms among Middle-Aged and Elderly People with Chronic Diseases in China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Sample
2.3. Criteria for Depressive Symptoms
2.4. Health Care Costs
2.5. Productivity Loss
2.6. Variables
2.7. Statistical Analysis
3. Results
3.1. Prevalence of Depressive Symptoms and Demographic Characteristics
3.2. Health Care Cost Estimation of Depressive Symptoms
3.3. Productivity Loss Estimation of Depressive Symptoms
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Conditions a | Chronic Patients n (%) b | Present Depressive Symptoms n (%) c |
|---|---|---|
| Model 1: conditions | ||
| Hypertension | 5773 (46.3) | 2294 (39.7) |
| Dyslipidemia | 3276 (26.3) | 1303 (39.8) |
| Diabetes | 1901 (15.3) | 789 (41.5) |
| Cancer or malignant tumor | 297 (2.4) | 137 (46.1) |
| Chronic lung disease | 2220 (17.8) | 1054 (47.5) |
| Liver disease | 982 (7.9) | 440 (44.8) |
| Heart attack | 2831 (22.7) | 1289 (45.5) |
| Stroke | 885 (7.1) | 431 (48.7) |
| Kidney disease | 1383 (11.1) | 683 (49.4) |
| Stomach or other digestive disease | 4553 (36.6) | 2177 (47.8) |
| Arthritis or rheumatism | 5790 (46.5) | 2779 (48.0) |
| Asthma | 801 (6.4) | 416 (51.9) |
| Model 2: No. of conditions d | ||
| 1 | 4173 (33.5) | 1295 (31.0) |
| 2 | 3346 (26.9) | 1277 (38.2) |
| 3 | 2258 (18.1) | 980 (43.4) |
| ≥4 | 2681 (21.5) | 1407 (52.5) |
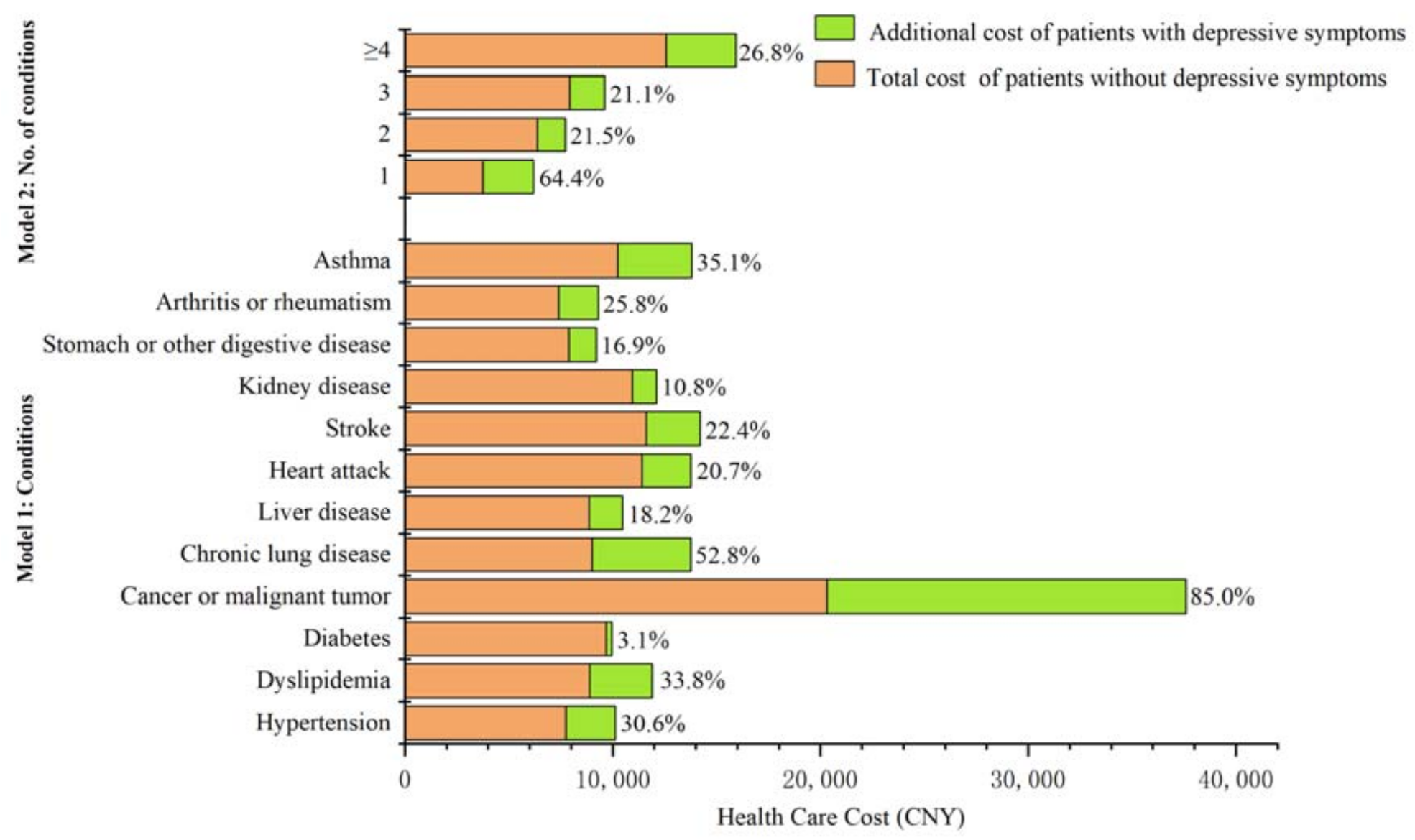
| Conditions | Without Depressive Symptoms | With Depressive Symptoms | % |
|---|---|---|---|
| Total Cost (95% CI) | Additional Cost (95% CI) | ||
| Model 1: conditions | |||
| Hypertension | 7750.5 (6762.4–8738.5) | 2371.8 (933.8–3809.9) | 30.6 |
| Dyslipidemia | 8898.1 (7612.8–10,183.4) | 3009.9 (1134.4–4885.3) | 33.8 |
| Diabetes | 9674.5 (8115.1–11,234.0) | 2,95.1 (−1653.9–2244.1) | 3.1 |
| Cancer or malignant tumor | 20,318.6 (13,443.5–27,193.8) | 17,273.7 (6164.7–28,382.6) | 85.0 |
| Chronic lung disease | 9010.2 (7283.6–10,736.8) | 4759.4 (2321.8–7197.0) | 52.8 |
| Liver disease | 8870.5 (7067.5–10,673.4) | 1611.2 (−1017.6–4234.0) | 18.2 |
| Heart attack | 11,413.0 (9657.6–13,168.5) | 2359.5 (234.4–4484.6) | 20.7 |
| Stroke | 11,609.6 (8357.6–14,861.6) | 2595.0 (−488.7–5678.7) | 22.4 |
| Kidney disease | 10,937.1 (8925.5–12,948.7) | 1178.4 (−1423.5–3780.3) | 10.8 |
| Stomach or other digestive disease | 7893.1 (6567.2–9219.0) | 1334.4 (−61.5–2730.4) | 16.9 |
| Arthritis or rheumatism | 7399.1 (6382.3–8415.9) | 1909.3 (429.8–3388.9) | 25.8 |
| Asthma | 10,232.4 (7709.6–12,755.2) | 3589.0 (640.5–6537.4) | 35.1 |
| Model 2: No. of conditions | |||
| 1 | 3764.9 (3152.3–4377.4) | 2422.7 (756.6–4088.8) | 64.4 |
| 2 | 6363.7 (5405.7–7321.6) | 1365.7 (3.8–2727.5) | 21.5 |
| 3 | 7932.1 (6315.6–9550.1) | 1674.4 (−4.4–3353.3) | 21.1 |
| ≥4 | 12,570.8 (10,594.1–14,547.5) | 3369.9 (924.3–5815.5) | 26.8 |
| Conditions | Without Depressive Symptoms | With Depressive Symptoms | % |
|---|---|---|---|
| Total Loss (95% CI) | Additional Loss (95% CI) | ||
| Model 1: conditions | |||
| Hypertension | 1306.7 (1167.3–1446.1) | 273.5 (16.8–530.2) | 20.9 |
| Dyslipidemia | 1203.3 (1025.2–1381.3) | 326.8 (23.8–629.7) | 27.2 |
| Diabetes | 1239.7 (991.7–1487.7) | 547.3 (112.9–981.7) | 44.2 |
| Cancer or malignant tumor | 2436.6 (1524.2–3349.0) | 2196.2 (244.0–4149.0) | 90.2 |
| Chronic lung disease | 1673.5 (1406.7–1940.2) | 813.5 (330.7–1296.3) | 48.6 |
| Liver disease | 1266.0 (932.7–1599.2) | 378.7 (−108.14–865.4) | 29.9 |
| Heart attack | 1458.8 (1236.3–1681.2) | 434.5 (11.5–857.5) | 29.8 |
| Stroke | 2009.8 (1535.6–2484.0) | −22.6 (−851.2–805.9) | 1.6 |
| Kidney disease | 1376.5 (1068.4–1684.5) | 561.7 (56.6–1066.9) | 40.8 |
| Stomach or other digestive disease | 1288.2 (1128.6–1447.8) | 278.9 (38.1–519.7) | 21.7 |
| Arthritis or rheumatism | 1507.2 (1352.6–1661.9) | 354.4 (115.1–593.6) | 23.5 |
| Asthma | 2251.8 (1717.0–2786.7) | 661.8 (−314.5–1638.2) | 29.4 |
| Model 2: No. of conditions | |||
| 1 | 742.5 (632.0–853.0) | 190.5 (17.0–364.1) | 25.7 |
| 2 | 1147.8 (983.9–1311.6) | 506.1 (193.7–818.5) | 44.1 |
| 3 | 1543.2 (1290.1–1796.3) | 54.0 (−338.2–446.2) | 3.5 |
| ≥4 | 1812.3 (1547.6–2076.9) | 363.4 (−70.6–797.4) | 20.1 |
References
- Lepine, J.P.; Brile, M. The increasing burden of depression. Neuropsychiatr. Dis. Treat. 2011, 7, 3–7. [Google Scholar] [PubMed] [Green Version]
- Marcus, M.; Yasamy, M.T.; van Ommeren, M.V.; Chisholm, D.; Saxena, S. Depression: A Global Public Health Concern; World Federation of Mental Health (WHO): Geneva, Switzerland, 2012. [Google Scholar]
- Rudisch, B.; Nemeroff, C.B. Epidemiology of comorbid coronary artery disease and depression. Biol. Psychiatry 2003, 54, 227–240. [Google Scholar] [CrossRef]
- Anderson, R.J.; Freedland, K.E.; Clouse, R.E.; Lustman, P.J. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care 2001, 24, 1069–1078. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matcham, F.; Rayner, L.; Steer, S.; Hotopf, M. The prevalence of depression in rheumatoid arthritis: A systematic review and meta-analysis. Rheumatology 2013, 52, 2136–2148. [Google Scholar] [CrossRef] [Green Version]
- Moussavi, S.; Chatterji, S.; Verdes, E.; Tandon, A.; Patel, V.; Ustun, B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet 2007, 370, 851–858. [Google Scholar] [CrossRef]
- McCarron, R.M.; Shapiro, B.; Rawles, J.; Luo, J. Depression. Ann. Intern. Med. 2021, 174, ITC65–ITC80. [Google Scholar] [CrossRef]
- Ji, H.; Du, L.; Zhu, X. Depression and its influence factors in the elderly with chronic disease in China. Mod. Prev. Med. 2020, 47, 3002–3006. [Google Scholar]
- Van den Akker, M.; Buntinx, F.; Roos, S.; Knottnerus, J.A. Problems in determining occurrence rates of multimorbidity. J. Clin. Epidemiol. 2001, 54, 675–679. [Google Scholar] [CrossRef]
- Read, J.R.; Sharpe, L.; Modini, M.; Dear, B.F. Multimorbidity and depression: A systematic review and meta-analysis. J. Affect Disord. 2017, 221, 36–46. [Google Scholar] [CrossRef]
- Katon, W.J. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol. Psychiatry 2003, 54, 216–226. [Google Scholar] [CrossRef]
- Ziarko, M.; Mojs, E.; Piasecki, B.; Samborski, W. The mediating role of dysfunctional coping in the relationship between beliefs about the disease and the level of depression in patients with rheumatoid arthritis. Sci. World J. 2014, 2014, 585063. [Google Scholar] [CrossRef]
- Gunn, J.M.; Ayton, D.R.; Densley, K.; Pallant, J.F.; Chondros, P.; Herrman, H.E.; Dowrick, C.F. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatry Psychiatr. Epidemiol. 2012, 47, 175–184. [Google Scholar] [CrossRef]
- Zhang, Z.; Gong, G.; Mao, J.; Ye, Z. Path analysis of relationship between chronic conditions and depression in middle to older age people. J. Nurs. Sci. 2018, 33, 76–78. [Google Scholar]
- Fan, V.S.; Ramsey, S.D.; Giardino, N.D.; Make, B.J.; Emery, C.F.; Diaz, P.T.; Benditt, J.O.; Mosenifar, Z.; McKenna, R.; Curtis, J.L.; et al. Sex, depression, and risk of hospitalization and mortality in chronic obstructive pulmonary disease. Arch. Intern. Med. 2007, 167, 2345–2353. [Google Scholar] [CrossRef] [Green Version]
- Koo, J.-R.; Yoon, J.-Y.; Joo, M.-H.; Lee, H.-S.; Oh, J.-E.; Kim, S.-G.; Seo, J.-W.; Lee, Y.-K.; Kim, H.-J.; Noh, J.-W.; et al. Treatment of depression and effect of antidepression treatment on nutritional status in chronic hemodialysis patients. Am. J. Med. Sci. 2005, 329, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Su, C.-H.; Chiu, H.-C.; Hsieh, H.-M.; Yen, J.-Y.; Lee, M.-H.; Li, C.-Y.; Chang, K.-P.; Huang, C.-J. Healthcare Utilization and Expenditures for Persons with Diabetes Comorbid with Mental Illnesses. Psychiatr. Q. 2016, 87, 545–557. [Google Scholar] [CrossRef]
- Sporinova, B.; Manns, B.; Tonelli, M.; Hemmelgarn, B.; MacMaster, F.; Mitchell, N.; Au, F.; Ma, Z.; Weaver, R.; Quinn, A. Association of Mental Health Disorders With Health Care Utilization and Costs Among Adults With Chronic Disease. JAMA Netw. Open 2019, 2, e199910. [Google Scholar] [CrossRef] [Green Version]
- Dalal, A.A.; Shah, M.; Lunacsek, O.; Hanania, N.A. Clinical and economic burden of depression/anxiety in chronic obstructive pulmonary disease patients within a managed care population. COPD 2011, 8, 293–299. [Google Scholar] [CrossRef]
- Evans-Lacko, S.; Knapp, M. Global patterns of workplace productivity for people with depression: Absenteeism and presenteeism costs across eight diverse countries. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 1525–1537. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.; Mui, A.C. Factorial validity of the Center for Epidemiologic Studies Depression Scale short form in older population in China. Int. Psychogeriatr. 2014, 26, 49–57. [Google Scholar] [CrossRef]
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Lei, X.; Sun, X.; Strauss, J.; Zhang, P.; Zhao, Y. Depressive symptoms and SES among the mid-aged and elderly in China: Evidence from the China Health and Retirement Longitudinal Study national baseline. Soc. Sci. Med. 2014, 120, 224–232. [Google Scholar] [CrossRef] [Green Version]
- Qiu, Y.; Li, H.; Yang, Z.; Liu, Q.; Wang, K.; Li, R.; Xing, D.; Hou, Y.; Lin, J. The prevalence and economic burden of pain on middle-aged and elderly Chinese people: Results from the China health and retirement longitudinal study. BMC health services research 2020, 20, 600. [Google Scholar] [CrossRef]
- Jin, H.Y.; Liu, X.; Xue, Q.L.; Chen, S.; Wu, C. The Association between Frailty and Healthcare Expenditure among Chinese Older Adults. J. Am. Med. Dir. Assoc. 2020, 21, 780–785. [Google Scholar] [CrossRef]
- Shi, J.; Wang, Y.; Cheng, W.; Shao, H.; Shi, L. Direct health care costs associated with obesity in Chinese population in 2011. J. Diabetes Its Complicat. 2017, 31, 523–528. [Google Scholar] [CrossRef]
- Greenberg, P.E.; Fournier, A.A.; Sisitsky, T.; Pike, C.T.; Kessler, R.C. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J. Clin. Psychiatry 2015, 76, 155–162. [Google Scholar] [CrossRef] [Green Version]
- Wu, Y.; Zhao, D.; Guo, J.; Lai, Y.; Chen, L.; Jin, S.; Huang, Y. Economic Burden of Depressive Symptoms Conditions among Middle-Aged and Elderly People with Hypertension in China. Int. J. Environ. Res. Public Health 2021, 18, 10009. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Wallace, K.; Zhao, X.; Misra, R.; Sambamoorthi, U. The Humanistic and Economic Burden Associated with Anxiety and Depression among Adults with Comorbid Diabetes and Hypertension. J. Diabetes Res. 2018, 2018, 4842520. [Google Scholar] [CrossRef]
- Lin, W.; Yin, W.; Yuan, D. Factors associated with the utilization of community-based health services among older adults in China-an empirical study based on Anderson’s health behavior model. BMC Prim. Care 2022, 23, 99. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.I.; Kim, S. The determinants of caregiver use and its costs for elderly inpatients in Korea: A study applying Andersen’s behavioral model of health care utilization and replacement cost method. BMC Health Serv. Res. 2021, 21, 631. [Google Scholar] [CrossRef] [PubMed]
- Guy, G.P.; Yabroff, K.R.; Ekwueme, D.U.; Rim, S.H.; Li, R.; Richardson, L.C. Economic Burden of Chronic Conditions Among Survivors of Cancer in the United States. J. Clin. Oncol. 2017, 35, 2053–2061. [Google Scholar] [CrossRef] [PubMed]
- Shao, H.; Mohammed, M.U.; Thomas, N.; Babazadeh, S.; Yang, S.; Shi, Q.; Shi, L. Evaluating Excessive Burden of Depression on Health Status and Health Care Utilization Among Patients With Hypertension in a Nationally Representative Sample From the Medial Expenditure Panel Survey (MEPS 2012). J. Nerv. Ment. Dis. 2017, 205, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Mihaylova, B.; Briggs, A.; O’Hagan, A.; Thompson, S.G. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011, 20, 897–916. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.Q.; Dong, B.R.; Lu, Z.C.; Yue, J.R.; Liu, Q.X. Chronic diseases and risk for depression in old age: A meta-analysis of published literature. Ageing Res. Rev. 2010, 9, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Casey, D.A. Depression in Older Adults: A Treatable Medical Condition. Prim. Care 2017, 44, 499–510. [Google Scholar] [CrossRef]
- Pálinkás, A.; Sándor, J.; Papp, M.; Kőrösi, L.; Falusi, Z.; Pál, L.; Bélteczki, Z.; Rihmer, Z.; Döme, P. Associations between untreated depression and secondary health care utilization in patients with hypertension and/or diabetes. Soc. Psychiatry Psychiatr. Epidemiol. 2019, 54, 255–276. [Google Scholar] [CrossRef]
- Eurelings, L.S.; van Dalen, J.W.; Ter Riet, G.; van Charante EP, M.; Richard, E.; van Gool, W.A.; Almeida, O.P.; Alexandre, T.S.; Baune, B.T.; Bickel, H.; et al. Apathy and depressive symptoms in older people and incident myocardial infarction, stroke, and mortality: A systematic review and meta-analysis of individual participant data. Clin. Epidemiol. 2018, 10, 363–379. [Google Scholar] [CrossRef] [Green Version]
- Palladino, R.; Tayu Lee, J.; Ashworth, M.; Triassi, M.; Millett, C. Associations between multimorbidity, healthcare utilisation and health status: Evidence from 16 European countries. Age Ageing 2016, 45, 431–435. [Google Scholar] [CrossRef] [Green Version]
- Tang, X.; Qi, S.; Zhang, H.; Wang, Z. Prevalence of depressive symptoms and its related factors among China’s older adults in 2016. J. Affect Disord. 2021, 292, 95–101. [Google Scholar] [CrossRef]
- Salive, M.E. Multimorbidity in older adults. Epidemiol. Rev. 2013, 35, 75–83. [Google Scholar] [CrossRef]
- DeJean, D.; Giacomini, M.; Vanstone, M.; Brundisini, F. Patient experiences of depression and anxiety with chronic disease: A systematic review and qualitative meta-synthesis. Ont. Health Technol. Assess. Ser. 2013, 13, 1–33. [Google Scholar]
- Hamre, H.J.; Witt, C.M.; Glockmann, A.; Ziegler, R.; Kienle, G.S.; Willich, S.N.; Kiene, H. Health costs in patients treated for depression, in patients with depressive symptoms treated for another chronic disorder and in non-depressed patients: A two-year prospective cohort study in anthroposophic outpatient settings. Eur. J. Health Econ. 2010, 11, 77–94. [Google Scholar] [CrossRef] [Green Version]
- Wan, J.; Chua, E.Y.C.; Soon, W.S.W.; Xie, Y.; Tang, W.E. The impact of a mental health service on chronic disease management in primary care. Singap. Med. J. 2021, 62, 235–239. [Google Scholar] [CrossRef]
- Thornicroft, G.; Ahuja, S.; Barber, S.; Chisholm, D.; Collins, P.Y.; Docrat, S.; Fairall, L.; Lempp, H.; Niaz, U.; Ngo, V.; et al. Integrated care for people with long-term mental and physical health conditions in low-income and middle-income countries. Lancet Psychiatry 2019, 6, 174–186. [Google Scholar] [CrossRef]
- Ali, M.K.; Chwastiak, L.; Poongothai, S.; Emmert-Fees, K.M.; Patel, S.A.; Anjana, R.M.; Sagar, R.; Shankar, R.; Sridhar, G.R.; Kosuri, M.; et al. Effect of a Collaborative Care Model on Depressive Symptoms and Glycated Hemoglobin, Blood Pressure, and Serum Cholesterol Among Patients With Depression and Diabetes in India: The INDEPENDENT Randomized Clinical Trial. JAMA 2020, 324, 651–662. [Google Scholar] [CrossRef]
- Chen, S.; Conwell, Y.; Xue, J.; Li, L.W.; Tang, W.; Bogner, H.R.; Dong, H. Protocol of an ongoing randomized controlled trial of care management for comorbid depression and hypertension: The Chinese Older Adult Collaborations in Health (COACH) study. BMC Geriatr. 2018, 18, 124. [Google Scholar] [CrossRef] [Green Version]
- Hathaway, E. Chronic Disease Prevention in Faith-Based Organizations. J. Pastor. Care Couns. 2018, 72, 159–162. [Google Scholar] [CrossRef]
- Cancelliere, C.; Cassidy, J.D.; Ammendolia, C.; Côté, P. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health 2011, 11, 395. [Google Scholar] [CrossRef] [Green Version]
- Evans-Lacko, S.; Knapp, M. Is manager support related to workplace productivity for people with depression: A secondary analysis of a cross-sectional survey from 15 countries. BMJ Open 2018, 8, e021795. [Google Scholar] [CrossRef]

| Character Variables | With Depressive Symptoms | Without Depressive Symptoms | p-Value |
|---|---|---|---|
| n = 4959 (%) | n = 7499 (%) | ||
| Gender | |||
| Male | 1896 (38.2) | 4064 (54.2) | <0.001 |
| Female | 3063 (61.8) | 3435 (45.8) | |
| Age | |||
| 45–54 | 1124 (22.7) | 1816 (24.2) | 0.175 |
| 55–64 | 1759 (35.5) | 2604 (34.7) | |
| 65–74 | 1485 (30.0) | 2241 (30.0) | |
| ≥75 | 591 (11.9) | 838 (11.2) | |
| Marital status | |||
| Married | 4116 (83.0) | 6667 (88.9) | <0.001 |
| Widowed | 104 (2.1) | 132 (1.8) | |
| Separated/Divorced/Unmarried | 739 (14.9) | 700 (9.3) | |
| Residence district | |||
| Rural | 4161 (83.91) | 5399 (72.0) | <0.001 |
| Urban | 798 (16.09) | 2100 (28.0) | |
| Education level | |||
| No formal education | 2571 (51.8) | 2678 (35.7) | <0.001 |
| Primary education | 1130 (22.8) | 1745 (23.3) | |
| Secondary education | 881 (17.8) | 1883 (25.1) | |
| High school and above | 377 (7.6) | 1193 (15.9) | |
| Occupation | |||
| Retired/Receded | 299 (6.0) | 859 (11.5) | <0.001 |
| Unemployed | 1611 (32.5) | 2042 (27.2) | |
| Agricultural work | 386 (7.8) | 916 (12.2) | |
| Employed | 2354 (47.5) | 3092 (41.2) | |
| Self-employed/Unpaid helper | 309 (6.2) | 590 (7.9) | |
| Medical insurance | |||
| Urban employee medical insurance | 420 (8.5) | 1408 (18.8) | <0.001 |
| New cooperative medical insurance | 3561 (71.8) | 4456 (58.4) | |
| Urban and rural resident medical insurance | 571 (11.5) | 949 (12.7) | |
| Urban resident medical insurance and others | 248 (5.0) | 527 (7.0) | |
| No insurance | 159 (3.2) | 159 (2.1) | |
| Household monthly expenditure | . | ||
| Lowest 25% | 1562 (31.5) | 1647 (22.0) | <0.001 |
| Lower 25% | 1573 (31.7) | 2266 (30.2) | |
| Higher 25% | 875 (17.6) | 1520 (20.3) | |
| Highest 25% | 949 (19.1) | 2066 (27.6) | |
| Perceived health status | |||
| Good | 498 (10.0) | 1944 (25.9) | <0.001 |
| Fair | 2223 (44.8) | 4183 (55.8) | |
| Poor | 2238 (45.1) | 1372 (18.3) | |
| No. of chronic disease | |||
| 1 | 1295 (26.1) | 2878 (38.4) | <0.001 |
| 2 | 1277 (25.8) | 2069 (27.6) | |
| 3 | 980 (19.7) | 1278 (17.0) | |
| ≥4 | 1407 (28.4) | 1274 (17.0) |
| Condition | Total Health Care Cost (95% CI) | Outpatient | Hospitalization | Self-Medication | |||
|---|---|---|---|---|---|---|---|
| Visit (95% CI) | Cost (95% CI) | Visit (95% CI) | Cost (95% CI) | Visit (95% CI) | Cost (95% CI) | ||
| Model 1: conditions | |||||||
| Hypertension | 2371.8 (933.8–3809.9) ** | 1.4 (0.6–2.2) ** | 872.1 (1.1–1745.2) * | 0.05 (0.02–0.1) ** | 1191.4 (440.8–1942.1) ** | 0.7 (0.4–1.1) ** | 476.7 (150.4–803.0) ** |
| Dyslipidemia | 3009.9 (1134.4–4885.3) ** | 1.8 (0.8–2.8) ** | 379.5 (−738.1–1497.1) | 0.1 (0.04–0.2) ** | 1155.7 (304.8–2006.6) ** | 0.6 (0.2–1.1) ** | 702.0 (271.6–1132.4) ** |
| Diabetes | 295.1 (−1653.9–2244.1) | 1.3 (−0.01–2.36) | −843.2 (−1916.7–230.3) | 0.05 (−0.03–0.13) | −174.0 (−1112.9–746.8) | 0.4 (−0.1–1.0) | 549.1 (48.1–1049.9) * |
| Cancer or malignant tumor | 17,273.7 (6164.7–28,382.6) ** | 2.6 (−0.1–5.3) | 1765.0 (−21,986.7–57,286.6) | 0.5 (0.21–0.84) ** | 19,158.6 (7180.2–31,136.9) ** | 2.3 (0.8–3.8) ** | 555.9 (−695.0–1806.8) |
| Chronic lung disease | 4759.4 (2321.8–7197.0) ** | 2.0 (0.8–3.3) ** | 1707.3 (295.2–3119.5) * | 0.1 (0.03–0.18) * | 1616.01 (601.9–2630.1) ** | 0.9 (0.4–1.4) ** | 637.4 (287.3–987.5) ** |
| Liver disease | 1611.2 (−1017.6–4234.0) | 1.3 (−0.5–3.1) | 65.2 (−1183.0–1313.4) | 0.04 (−0.11–0.19) | −27.7 (−1062.4–1007.1) | 0.8 (0.01–1.6) * | 519.3 (−145.7–1184.4) |
| Heart attack | 2359.5 (234.41–4484.6) * | 1.4 (0.4–2.4) ** | 425.2 (−600.5–1450.9) | 0.1 (0.02–0.16) ** | 859.0 (−265.2–1983.2) | 0.5 (0.1–0.9) * | 734.2 (239.1–1229.3) ** |
| Stroke | 2595.0 (−488.7–5678.7) | 0.2 (−2.0–2.3) | 957.3 (33.7–1880.94) * | 0.3 (−0.07–0.62) | 1631.4 (64.5–3198.2) * | 0.1 (−0.7–0.9) | 123.9 (−496.2–744.0) |
| Kidney disease | 1178.4 (−1423.5–3780.3) | 2.2 (0.6–3.7) ** | 672.3 (−410.8–1755.4) | 0.04 (−0.58–0.67) | 494.9 (−1063.6–2053.5) | 0.5 (−0.2–1.1) | −59.1 (−683.2–565.0) |
| Stomach or other digestive disease | 1334.4 (−61.5–2730.36) | 1.8 (0.9–2.7) ** | 287.2 (−631.4–1205.8) | 0.05 (0.01–0.88) * | 527.8 (−1.7–1057.4) * | 0.8 (0.4–1.1) ** | 494.6 (210.0–779.3) ** |
| Arthritis or rheumatism | 1909.3 (429.8–3388.9) * | 1.1 (0.3–1.9) ** | 764.1 (−213.4–1741.5) | 0.05 (0.01–0.09) ** | 279.5 (−171.7–730.6) | 0.6 (0.1–1.1) * | 624.0 (348.0–900.1) ** |
| Asthma | 3589.0 (640.5–6537.4) * | 1.1 (−0.7–3.0) | 2353.4 (474.3–4232.6) * | 0.1 (−0.02–0.30) | −331.4 (−1724.1–1062.4) | 0.5 (−0.3–1.2) | 740.8 (195.0–1286.6) ** |
| Model 2: No. of conditions | |||||||
| 1 | 2422.7 (756.6–4088.8) ** | 0.8 (0.1–1.4) * | 1720.8 (507.9–2933.6) ** | 0.1 (0.01–0.13) * | 373.9 (28.8–718.9) * | 0.9 (0.5–1.31) ** | 113.0 (−150.2–376.2) |
| 2 | 1365.7 (3.8–2727.5) * | 0.9 (0.03–1.7) * | 820.1 (−109.5–1749.6) | 0.01 (−0.04–0.05) | 173.7 (−319.8–667.3) | 0.7 (0.3–1.1) ** | 459.1 (134.0–784.2) ** |
| 3 | 1674.4 (−4.4–3353.3) | 2.0 (0.7–3.2) ** | 624.7 (−351.0–1600.3) | 0.1 (0.01–0.13) * | 928.1 (−3.5–1859.7) * | 0.6 (0.1–1.1) * | 395.5 (−31.8–822.9) |
| ≥4 | 3369.9 (924.3–5815.5) ** | 1.6 (0.3–2.9) * | 444.4 (−968.4–1856.9) | 0.1 (0.04–0.2) ** | 999.7 (−95.2–2094.7) | 0.5 (0.1–0.9) * | 849.6 (334.8–1364.3) ** |
| Condition | Total Productivity Loss (95% CI) | Unemployment | Agricultural | Employed | |||
|---|---|---|---|---|---|---|---|
| Missed Days (95% CI) | Economic Loss (95% CI) | Missed Days (95% CI) | Economic Loss (95% CI) | Missed Days (95% CI) | Economic Loss (95% CI) | ||
| Model 1: conditions | |||||||
| Hypertension | 273.5 (16.8–530.2) * | 1.9 (−0.9–4.6) | 22.3 (−218.5–263.1) | 3.5 (2.1–4.9) ** | 164.6 (79.7–249.5) ** | 0.01 (−0.01–0.3) | 0.03 (−0.1–0.2) |
| Dyslipidemia | 326.8 (23.8–629.7) * | 3.6 (0.4–6.9) * | 76.7 (−208.01–361.4) | 2.7 (1.2–4.2) ** | 151.8 (66.8–236.8) ** | 0.01 (−0.01–0.02) | 0.8 (0.1–1.5) * |
| Diabetes | 547.3 (112.9–981.7) * | 2.3 (−1.6–6.2) | 1.9 (−0.7–4.5) | 3.6 (1.4–5.8) ** | 100.0 (4.1–196.0) * | 0.02 (−0.01–0.04) | 0.1 (−0.4–0.6) |
| Cancer or malignant tumor | 2196.2 (244.0–4149.0) * | 4.5 (−1.2–8.0) | 1195.7 (−804.5–3195.9) | 3.8 (2.3–5.3) ** | 137.5 (3.0–171.9) * | 0.1 (−0.1–0.2) | −3.4 (−9.8–3.5) |
| Chronic lung disease | 813.5 (330.7–1296.3) ** | 2.1 (−3.0–7.2) | 451.2 (4.0–898.4) * | 5.3 (2.8–7.8) ** | 286.8 (135.2–438.3) ** | 0.01 (−0.01–0.03) | −0.01 (−0.1–0.5) |
| Liver disease | 378.7 (−108.14–865.4) | 1.8 (−4.7–9.1) | 6.2 (−9.0–14.5) | 4.4 (1.4–7.5) ** | 93.5 (−35.3–222.2) | 0.03 (−0.03–0.1) | 0.3 (0.03–0.6) * |
| Heart attack | 434.5 (11.5–857.5) * | 2.5 (−1.6–6.7) | 49.2 (−304.1–402.4) | 4.0 (2.1–5.9) ** | 224.2 (114.1-−334.4) ** | 0.04 (−0.5–0.6) | 0.02 (−0.05–0.1) |
| Stroke | 32.6 (−351.2–405.9) | 3.2 (−6.4–12.9) | 63.5 (−514.3–767.3) | 5.3 (2.7–7.9) ** | 129.0 (57.2–200.9) ** | 0.4 (−0.3–1.1) | 0.03 (0.01–0.15) * |
| Kidney disease | 561.7 (56.6–1066.9) * | 1.8 (−2.1–7.3) | 279.4 (−169.4–728.1) | 6.1 (3.1–9.1) ** | 163.0 (24.5–301.6) * | 0.3 (−0.01–0.5) | 33.8 (11.6–55.9) ** |
| Stomach or other digestive disease | 278.9 (38.1–519.7) * | 1.5 (0.29–3.3) * | 168.4 (−61.6–398.3) | 3.7 (2.1–5.3) ** | 167.5 (77.6–257.4) ** | 0.2 (−0.1–0.5) | 35.4 (2.79–68.1) * |
| Arthritis or rheumatism | 354.4 (115.1–593.6) ** | 1.1 (−1.8–3.9) | −44.1 (−276.4–188.1) | 6.0 (4.3–7.7) ** | 306.7 (211.5–402.0) ** | 0.2 (−0.04–0.3) | 17.1 (−4.0–38.2) |
| Asthma | 661.8 (−314.5–1638.2) | 1.3 (−1.1–4.5) | −56.1 (−290.4–178.2) | 2.6 (−2.3–7.4) | 139.8 (−60.4–339.9) | −0.1 (−0.9–0.7) | −0.02 (−0.05–0.03) |
| Model 2: No. of conditions | |||||||
| 1 | 190.5 (17.0–364.1) * | 1.0 (−0.7–2.7) | 128.6 (−9.0–266.3) | 0.8 (0.07–1.45) * | 118.7 (46.7–190.7) ** | 0.1 (−0.2–0.4) | 24.1 (−9.4–57.5) |
| 2 | 506.1 (193.7–818.5) ** | 2.8 (−0.7–6.3) | 110.7 (−162.0–383.3) | 0.9 (0.03–1.70) * | 118.4 (48.0–188.9) ** | 0.01 (−0.3–0.4) | 13.2 (−10.2–36.6) |
| 3 | 54.0 (−338.2–446.2) | 0.5 (−3.6–4.7) | −166.9 (−561.4–227.6) | 2.0 (0.67–3.21) ** | 249.2 (125.2–373.3) ** | 0.05 (−0.2–0.3) | −0.01 (−0.03–0.02) |
| ≥4 | 363.4 (−70.6–797.4) | 3.0 (−1.8–7.9) | 47.7 (−357.7–453.1) | 1.6 (0.30–2.85) * | 119.9 (49.3–350.6) ** | 0.05 (−0.2–0.3) | 0.3 (−0.2–0.8) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Y.; Jin, S.; Guo, J.; Zhu, Y.; Chen, L.; Huang, Y. The Economic Burden Associated with Depressive Symptoms among Middle-Aged and Elderly People with Chronic Diseases in China. Int. J. Environ. Res. Public Health 2022, 19, 12958. https://doi.org/10.3390/ijerph191912958
Wu Y, Jin S, Guo J, Zhu Y, Chen L, Huang Y. The Economic Burden Associated with Depressive Symptoms among Middle-Aged and Elderly People with Chronic Diseases in China. International Journal of Environmental Research and Public Health. 2022; 19(19):12958. https://doi.org/10.3390/ijerph191912958
Chicago/Turabian StyleWu, Yun, Sihui Jin, Jianwei Guo, Yi Zhu, Lijin Chen, and Yixiang Huang. 2022. "The Economic Burden Associated with Depressive Symptoms among Middle-Aged and Elderly People with Chronic Diseases in China" International Journal of Environmental Research and Public Health 19, no. 19: 12958. https://doi.org/10.3390/ijerph191912958
APA StyleWu, Y., Jin, S., Guo, J., Zhu, Y., Chen, L., & Huang, Y. (2022). The Economic Burden Associated with Depressive Symptoms among Middle-Aged and Elderly People with Chronic Diseases in China. International Journal of Environmental Research and Public Health, 19(19), 12958. https://doi.org/10.3390/ijerph191912958






