Randomized Controlled Trial of the Cholera-Hospital-Based-Intervention-for-7-Days (CHoBI7) Cholera Rapid Response Program to Reduce Diarrheal Diseases in Bangladesh
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Patient and Public Involvement
2.3. Ethical Approval
2.4. Participants
2.5. Randomization and Masking
2.6. Intervention Procedures
2.7. Evaluation Procedure
2.8. Outcomes
2.9. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ali, M.; Nelson, A.R.; Lopez, A.L.; Sack, D.A. Updated Global Burden of Cholera in Endemic Countries. PLoS Negl. Trop. Dis. 2015, 9, e0003832. [Google Scholar] [CrossRef] [PubMed]
- Institute, I.V. Country Investment Case Study on Cholera Vaccination: Bangladesh; International Vaccine Institute: Seoul, Korea, 2013. [Google Scholar]
- Alam, M.; Hasan, N.A.; Sadique, A.; Bhuiyan, N.A.; Ahmed, K.U.; Nusrin, S.; Nair, G.B.; Siddique, A.K.; Sack, R.B.; Sack, D.A.; et al. Seasonal cholera caused by Vibrio cholerae serogroups O1 and O139 in the coastal aquatic environment of Bangladesh. Appl. Environ. Microbiol. 2006, 72, 4096–4104. [Google Scholar] [CrossRef]
- George, C.M.; Rashid, M.; Almeida, M.; Saif-Ur-Rahman, K.M.; Monira, S.; Bhuyian, M.S.I.; Hasan, K.; Mahmud, T.T.; Li, S.; Brubaker, J.; et al. Genetic relatedness of Vibrio cholerae isolates within and between households during outbreaks in Dhaka, Bangladesh. BMC Genom. 2017, 18, 903. [Google Scholar] [CrossRef]
- Richterman, A.; Sainvilien, D.R.; Eberly, L.; Ivers, L.C. Individual and Household Risk Factors for Symptomatic Cholera Infection: A Systematic Review and Meta-analysis. J. Infect. Dis. 2018, 218 (Suppl. 3), S154–S164. [Google Scholar] [CrossRef]
- Burrowes, V.; Perin, J.; Monira, S.; Sack, D.A.; Rashid, M.U.; Mahamud, T.; Rahman, Z.; Mustafiz, M.; Bhuyian, S.I.; Begum, F.; et al. Risk Factors for Household Transmission of Vibrio cholerae in Dhaka, Bangladesh (CHoBI7 Trial). Am. J. Trop. Med. Hyg. 2017, 96, 1382–1387. [Google Scholar] [CrossRef]
- George, C.M.; Hasan, K.; Monira, S.; Rahman, Z.; Saif-Ur-Rahman, K.M.; Rashid, M.U.; Zohura, F.; Parvin, T.; Islam Bhuyian, M.S.; Mahmud, M.T.; et al. A prospective cohort study comparing household contact and water Vibrio cholerae isolates in households of cholera patients in rural Bangladesh. PLoS Negl. Trop. Dis. 2018, 12, e0006641. [Google Scholar] [CrossRef]
- Wolfe, M.; Kaur, M.; Yates, T.; Woodin, M.; Lantagne, D. A Systematic Review and Meta-Analysis of the Association between Water, Sanitation, and Hygiene Exposures and Cholera in Case-Control Studies. Am. J. Trop. Med. Hyg. 2018, 99, 534–545. [Google Scholar] [CrossRef]
- Ali, M.; Debes, A.K.; Luquero, F.J.; Kim, D.R.; Park, J.Y.; Digilio, L.; Manna, B.; Kanungo, S.; Dutta, S.; Sur, D.; et al. Potential for Controlling Cholera Using a Ring Vaccination Strategy: Re-analysis of Data from a Cluster-Randomized Clinical Trial. PLoS Med. 2016, 13, e1002120. [Google Scholar] [CrossRef]
- Debes, A.K.; Ali, M.; Azman, A.S.; Yunus, M.; Sack, D.A. Cholera cases cluster in time and space in Matlab, Bangladesh: Implications for targeted preventive interventions. Int. J. Epidemiol. 2016, 45, 2134–2139. [Google Scholar] [CrossRef]
- Weil, A.A.; Khan, A.I.; Chowdhury, F.; LaRocque, R.C.; Faruque, A.; Ryan, E.T.; Calderwood, S.B.; Qadri, F.; Harris, J.B. Clinical outcomes in household contacts of patients with cholera in Bangladesh. Clin. Infect. Dis. 2009, 49, 1473–1479. [Google Scholar] [CrossRef]
- Deb, B.C.; Sircar, B.K.; Sengupta, P.G.; Sen, D.; Saha, M.R.; Pal, S.C. Intra-familial transmission of Vibrio cholerae biotype El Tor in Calcutta slums. Indian J. Med. Res. 1982, 76, 814–819. [Google Scholar]
- Spira, W.; Khan, M.U.; Saeed, Y.; Sattar, M. Microbiological surveillance of intra-neighbourhood El Tor cholera transmission in rural Bangaldesh. Bull. World Health Organ. 1980, 58, 731. [Google Scholar]
- George, C.M.; Monira, S.; Sack, D.A.; Rashid, M.U.; Saif-Ur-Rahman, K.M.; Mahmud, T.; Rahman, Z.; Mustafiz, M.; Bhuyian, S.I.; Winch, P.J.; et al. Randomized Controlled Trial of Hospital-Based Hygiene and Water Treatment Intervention (CHoBI7) to Reduce Cholera. Emerg. Infect. Dis. 2016, 22, 233–241. [Google Scholar] [CrossRef]
- D’Mello-Guyett, L.; Cumming, O.; Bonneville, S.; D’Hondt, R.; Mashako, M.; Nakoka, B.; Gorski, A.; Verheyen, D.; Van den Bergh, R.; Welo, P.O.; et al. Effectiveness of hygiene kit distribution to reduce cholera transmission in Kasaï-Oriental, Democratic Republic of Congo, 2018: A prospective cohort study. BMJ Open 2021, 11, e050943. [Google Scholar] [CrossRef]
- Mosler, H.-J. A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: A conceptual model, a review, and a guideline. Int. J. Environ. Health Res. 2012, 22, 431–449. [Google Scholar] [CrossRef] [PubMed]
- Dreibelbis, R.; Winch, P.J.; Leontsini, E.; Hulland, K.R.; Ram, P.K.; Unicomb, L.; Luby, S.P. The integrated behavioural model for water, sanitation, and hygiene: A systematic review of behavioural models and a framework for designing and evaluating behaviour change interventions in infrastructure-restricted settings. BMC Public Health 2013, 13, 1015. [Google Scholar] [CrossRef]
- George, C.M.; Zohura, F.; Teman, A.; Thomas, E.; Hasan, T.; Rana, S.; Parvin, T.; Sack, D.A.; Bhuyian, S.I.; Labrique, A.; et al. Formative research for the design of a scalable water, sanitation, and hygiene mobile health program: CHoBI7 mobile health program. BMC Public Health 2019, 19, 1028. [Google Scholar]
- George, C.M.; Monira, S.; Zohura, F.; Thomas, E.D.; Hasan, M.T.; Parvin, T.; Hasan, K.; Rashid, M.U.; Papri, N.; Islam, A.; et al. Effects of a Water, Sanitation and Hygiene Mobile Health Program on Diarrhea and Child Growth in Bangladesh: A Cluster-Randomized Controlled Trial of the CHoBI7 Mobile Health Program. Clin. Infect. Dis. 2021, 73, e2560–e2568. [Google Scholar] [CrossRef]
- Figueroa, M.E.; Kincaid, D.L. Social, Cultural and Behavioral Correlates of Household Water Treatment and Storage; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Dunston, C.; McAfee, D.; Kaiser, R.; Rakotoarison, D.; Rambeloson, L.; Hoang, A.T.; Quick, R.E. Collaboration, cholera, and cyclones: A project to improve point-of-use water quality in Madagascar. Am. J. Public Health 2001, 91, 1574–1576. [Google Scholar] [CrossRef]
- Quick, R.E.; Kimura, A.; Thevos, A.; Tembo, M.; Shamputa, I.; Hutwagner, L.; Mintz, E. Diarrhea prevention through household-level water disinfection and safe storage in Zambia. Am. J. Trop. Med. Hyg. 2002, 66, 584–589. [Google Scholar] [CrossRef]
- Michel, E.; Gaudart, J.; Beaulieu, S.; Bulit, G.; Piarroux, M.; Boncy, J.; Dely, P.; Piarroux, R.; Rebaudet, S. Estimating effectiveness of case-area targeted response interventions against cholera in Haiti. Elife 2019, 8, e50243. [Google Scholar] [CrossRef]
- Sikder, M.; Altare, C.; Doocy, S.; Trowbridge, D.; Kaur, G.; Kaushal, N.; Lyles, E.; Lantagne, D.; Azman, A.S.; Spiegel, P. Case-area targeted preventive interventions to interrupt cholera transmission: Current implementation practices and lessons learned. PLoS Negl. Trop. Dis. 2021, 15, e0010042. [Google Scholar] [CrossRef]
- Bompangue, D.; Moore, S.; Taty, N.; Impouma, B.; Sudre, B.; Manda, R.; Balde, T.; Mboussou, F.; Vandevelde, T. Description of the targeted water supply and hygiene response strategy implemented during the cholera outbreak of 2017-2018 in Kinshasa, DRC. BMC Infect. Dis. 2020, 20, 226. [Google Scholar] [CrossRef]

| Standard Message Arm | CHoBI7 Cholera Rapid Response Program Arm | p-Value | |||||
|---|---|---|---|---|---|---|---|
| % or N | n | N | % or N | n | N | ||
| Number of Cholera Hotspots | 8 | 7 | |||||
| Study Households | 39 | 34 | |||||
| All Study Participants | 138 | 146 | |||||
| Baseline Household Member Age (Years) | |||||||
| Median ± SD (Min − Max) | 21.0 ± 15.3 (0.3–65) | 23.7 ± 17.5 (0.2–70) | 0.17 | ||||
| 0–5 Years | 27% | 37 | 138 | 26% | 38 | 146 | |
| 5–17 Years | 19% | 26 | 138 | 14% | 20 | 146 | |
| 18 Years or Greater | 54% | 75 | 138 | 60% | 88 | 146 | |
| Gender | |||||||
| Female | 52% | 72 | 138 | 53% | 77 | 146 | 0.83 |
| Household Roof Type | |||||||
| Tin | 72% | 28 | 39 | 68% | 23 | 34 | 0.15 |
| Concrete | 28% | 11 | 39 | 32% | 11 | 34 | |
| Other | 0% | 0 | 39 | 0% | 0 | 34 | |
| Household Wall Type | |||||||
| Concrete | 97% | 38 | 39 | 97% | 33 | 34 | 0.92 |
| Mud | 0% | 0 | 39 | 0% | 0 | 34 | |
| Tin | 3% | 1 | 39 | 3% | 1 | 34 | |
| Other | 0% | 0 | 39 | 0% | 0 | 34 | |
| Household Floor Type | |||||||
| Concrete | 100% | 39 | 39 | 100% | 34 | 34 | 1.00 |
| Other | 0% | 0 | 39 | 0% | 0 | 34 | |
| Electricity | 97% | 38 | 39 | 97% | 33 | 34 | 0.92 |
| Refrigerator Ownership | 46% | 18 | 39 | 62% | 21 | 34 | 0.18 |
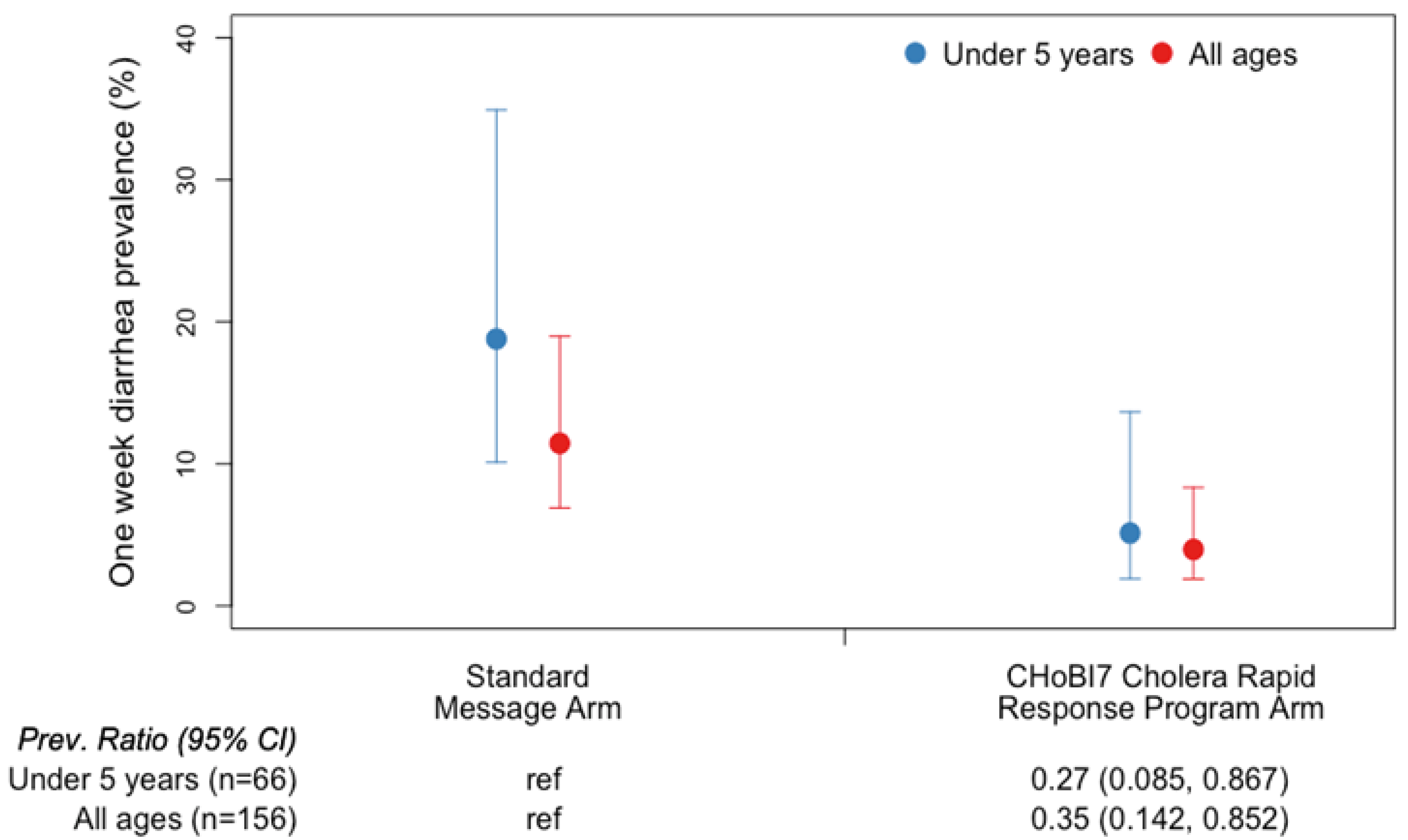
| Study Arm | N | Mean Diarrhea Prevalence † | Prevalence Ratio (95% CI) * |
|---|---|---|---|
| Standard Message Arm | |||
| 0–5 Years | 30 | 19% | (reference) |
| All Age Groups | 76 | 11% | (reference) |
| CHoBI7 Cholera Rapid Response Program Arm | |||
| 0–5 Years | 36 | 5% | 0.27 (0.09–0.87) |
| All Age Groups | 80 | 4% | 0.35 (0.14–0.85) |
| % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | |
|---|---|---|---|---|---|---|
| Individuals Handwashing with Soap at Stool/Toilet or Food Related Events During 5-Hour Structured Observation * | ||||||
| Standard Message Arm | 28% | - | 12% | - | 22% | - |
| CHoBI7 Cholera Rapid Response Program Arm | 60% | 3.94 (2.12, 7.30) | 56% | 9.57 (3.03, 30.25) | 44% | 2.78 (1.17, 6.58) |
| Presence of Soapy Water in Household | ||||||
| Standard Message Arm | 0% | - | 0% | - | 0% | - |
| CHoBI7 Cholera Rapid Response Program Arm | 97% | ‡ | 92% | ‡ | 91% | ‡ |
| Chlorine in Stored Household Drinking Water > 0.2 mg/L | ||||||
| Standard Message Arm | 0% | - | 0% | - | 0% | - |
| CHoBI7 Cholera Rapid Response Program Arm | 59% | ‡ | 35% | ‡ | 0% | ‡ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
George, C.M.; Parvin, T.; Bhuyian, M.S.I.; Uddin, I.M.; Zohura, F.; Masud, J.; Monira, S.; Sack, D.A.; Perin, J.; Alam, M.; et al. Randomized Controlled Trial of the Cholera-Hospital-Based-Intervention-for-7-Days (CHoBI7) Cholera Rapid Response Program to Reduce Diarrheal Diseases in Bangladesh. Int. J. Environ. Res. Public Health 2022, 19, 12905. https://doi.org/10.3390/ijerph191912905
George CM, Parvin T, Bhuyian MSI, Uddin IM, Zohura F, Masud J, Monira S, Sack DA, Perin J, Alam M, et al. Randomized Controlled Trial of the Cholera-Hospital-Based-Intervention-for-7-Days (CHoBI7) Cholera Rapid Response Program to Reduce Diarrheal Diseases in Bangladesh. International Journal of Environmental Research and Public Health. 2022; 19(19):12905. https://doi.org/10.3390/ijerph191912905
Chicago/Turabian StyleGeorge, Christine Marie, Tahmina Parvin, Md. Sazzadul Islam Bhuyian, Ismat Minhaj Uddin, Fatema Zohura, Jahed Masud, Shirajum Monira, David A. Sack, Jamie Perin, Munirul Alam, and et al. 2022. "Randomized Controlled Trial of the Cholera-Hospital-Based-Intervention-for-7-Days (CHoBI7) Cholera Rapid Response Program to Reduce Diarrheal Diseases in Bangladesh" International Journal of Environmental Research and Public Health 19, no. 19: 12905. https://doi.org/10.3390/ijerph191912905
APA StyleGeorge, C. M., Parvin, T., Bhuyian, M. S. I., Uddin, I. M., Zohura, F., Masud, J., Monira, S., Sack, D. A., Perin, J., Alam, M., & Faruque, A. S. G. (2022). Randomized Controlled Trial of the Cholera-Hospital-Based-Intervention-for-7-Days (CHoBI7) Cholera Rapid Response Program to Reduce Diarrheal Diseases in Bangladesh. International Journal of Environmental Research and Public Health, 19(19), 12905. https://doi.org/10.3390/ijerph191912905







