Have Deaths of Despair Risen during the COVID-19 Pandemic? A Systematic Review
Abstract
1. Introduction
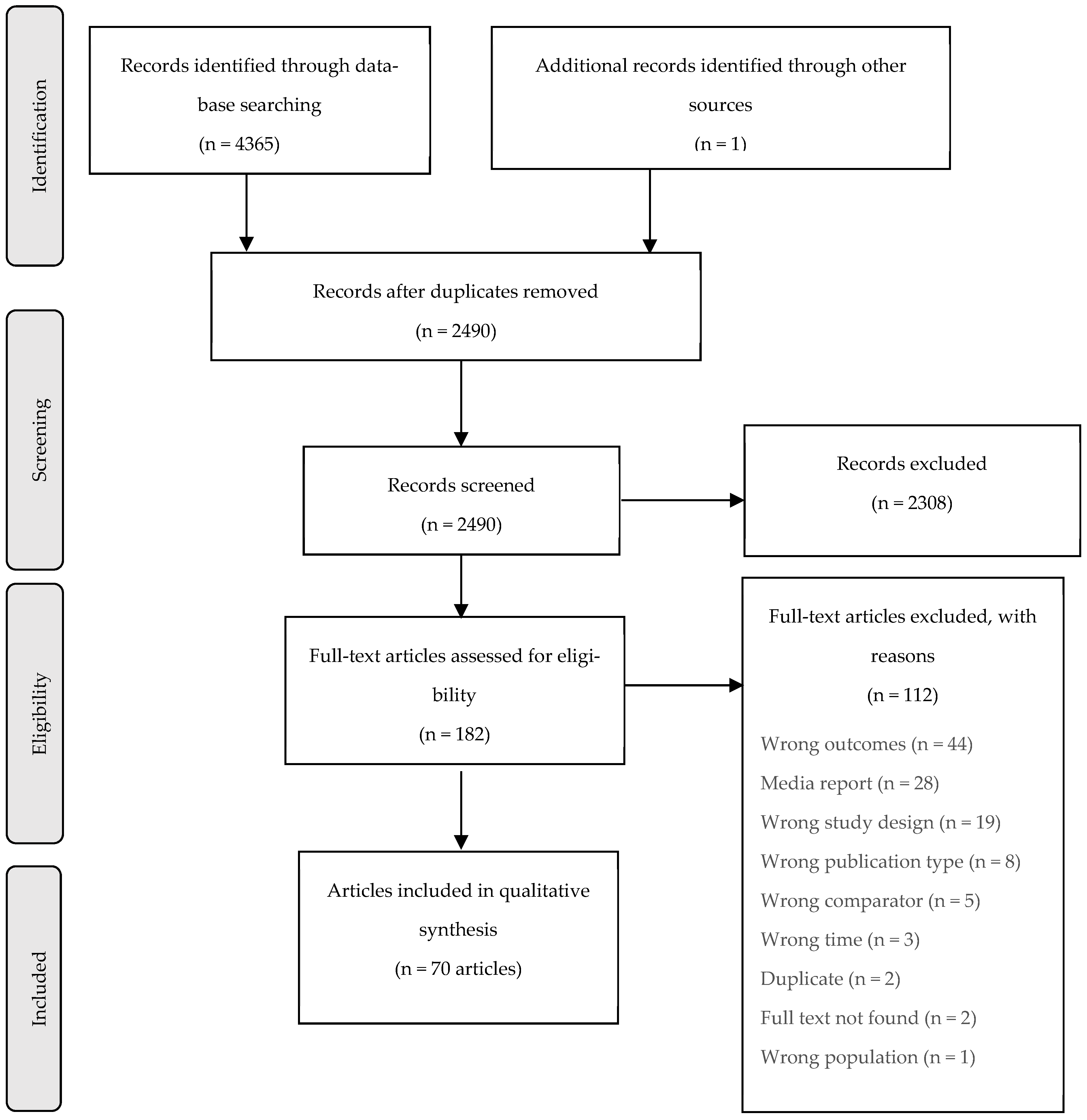
2. Materials and Methods
2.1. Study Selection
2.2. Search Strategies
2.3. Data Extraction
2.4. Quality Assessment
3. Results
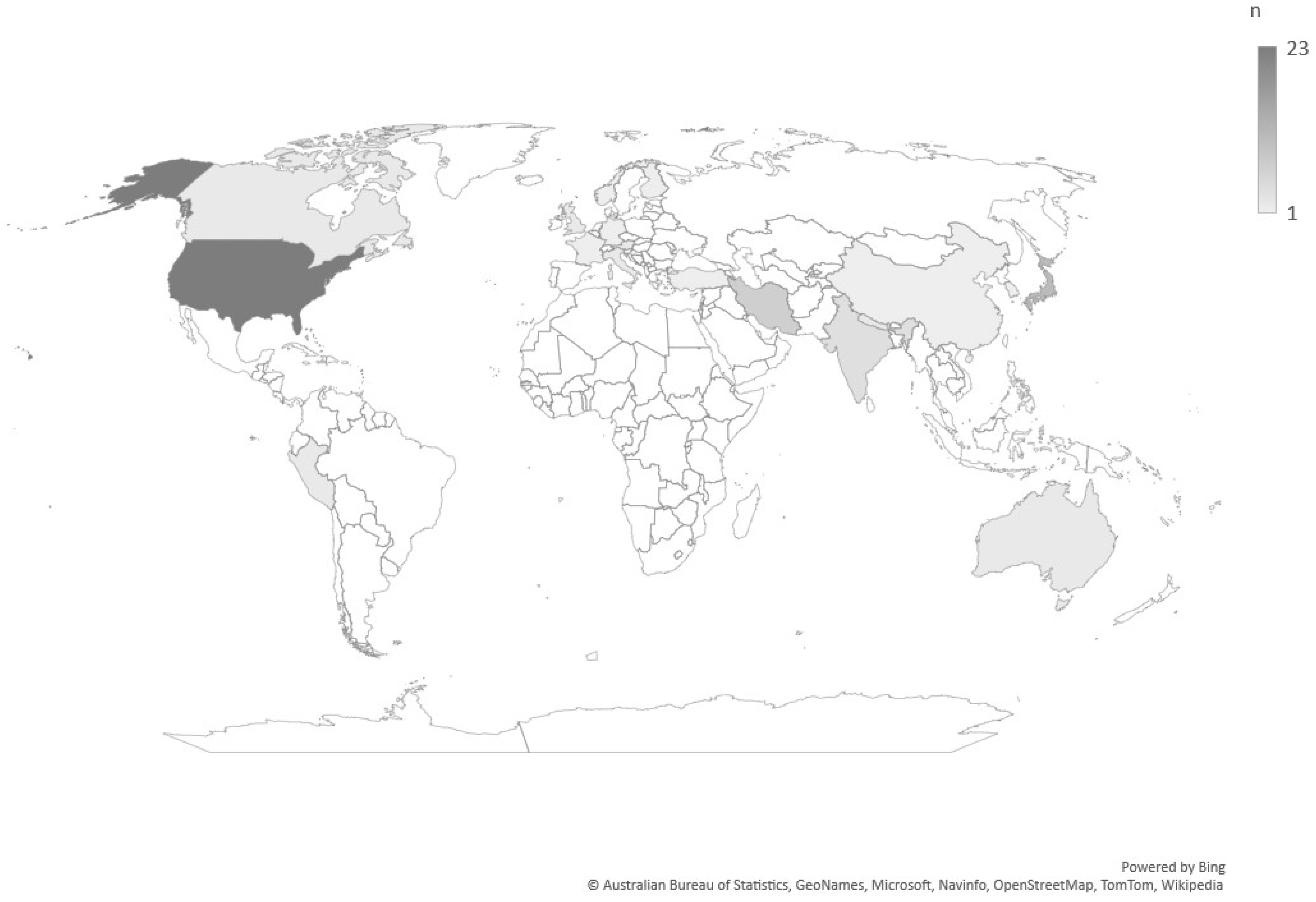
3.1. Study Characteristics
3.2. Suicide Deaths
3.3. Overdose Deaths
3.4. Liver Disease
3.5. Inequities
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Santomauro, D.F.; Mantilla Herrera, A.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Phiri, P.; Ramakrishnan, R.; Rathod, S.; Elliot, K.; Thayanandan, T.; Sandle, N.; Haque, N.; Chau, S.W.H.; Wong, O.W.H.; Chan, S.S.M.; et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: A systematic review and meta-analysis. eClinicalMedicine 2021, 34, 100806. [Google Scholar] [CrossRef] [PubMed]
- John, A.; Eyles, E.; Webb, R.T.; Okolie, C.; Schmidt, L.; Arensman, E.; Hawton, K.; O’Connor, R.C.; Kapur, N.; Moran, P.; et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: Update of living systematic review. F1000Research 2020, 9, 1097. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Begum, N.; Saini, A.; Wang, S.; McGuire, P.; Fusar-Poli, P.; Lewis, G.; David, A.S. Suicide, self-harm and thoughts of suicide or self-harm in infectious disease epidemics: A systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 2021, 30, e32. [Google Scholar] [CrossRef] [PubMed]
- Imtiaz, S.; Nafeh, F.; Russell, C.; Ali, F.; Elton-Marshall, T.; Rehm, J. The impact of the novel coronavirus disease (COVID-19) pandemic on drug overdose-related deaths in the United States and Canada: A systematic review of observational studies and analysis of public health surveillance data. Subst. Abuse Treat. Prev. Policy 2021, 16, 87. [Google Scholar] [CrossRef]
- Karanikolos, M.; Heino, P.; McKee, M.; Stuckler, D.; Legido-Quigley, H. Effects of the Global Financial Crisis on Health in High-Income Oecd Countries: A Narrative Review. Int. J. Health Serv. 2016, 46, 208–240. [Google Scholar] [CrossRef]
- Parmar, D.; Stavropoulou, C.; Ioannidis, J.P.A. Health outcomes during the 2008 financial crisis in Europe: Systematic literature review. BMJ 2016, 354, i4588. [Google Scholar] [CrossRef]
- Pirkis, J.; Shin, S.; Spittal, M.J.; John, A.; DelPozo-Banos, M.; Arya, V.; Analuisa-Aguilar, P.; Appleby, L.; Webb, R.T.; Arensman, E.; et al. Suicide trends in the early months of the COVID-19 pandemic: An interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry 2021, 8, 579–588. [Google Scholar] [CrossRef]
- Shanahan, L.; Hill, S.N.; Gaydosh, L.M.; Steinhoff, A.; Costello, E.J.; Dodge, K.A.; Harris, K.M.; Copeland, W.E. Does Despair Really Kill? A Roadmap for an Evidence-Based Answer. Am. J. Public Health 2019, 109, 854–858. [Google Scholar] [CrossRef]
- Diez Roux, A.V. Despair as a Cause of Death: More Complex Than It First Appears. Am. J. Public Health 2017, 107, 1566–1567. [Google Scholar] [CrossRef]
- Case, A.; Deaton, A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. USA 2015, 112, 15078. [Google Scholar] [CrossRef] [PubMed]
- Muntaner, C.; Gunn, V.; Prins, S.J. On Case and Deaton’s deaths of despair: Implications for health inequalities research in the post-COVID-19 era. Gac. Sanit. 2021, 35, 409–410. [Google Scholar] [CrossRef] [PubMed]
- Allik, M.; Brown, D.; Dundas, R.; Leyland, A.H. Deaths of despair: Cause-specific mortality and socioeconomic inequalities in cause-specific mortality among young men in Scotland. Int. J. Equity Health 2020, 19, 215. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, C.B. Deaths of Despair and the Incidence of Excess Mortality in 2020; National Bureau of Economic Research: Cambridge, MA, USA, 2021. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021, 134, 103–112. [Google Scholar] [CrossRef]
- UT Health San Antonio The Libaries. 2019 Novel Coronavirus Information: COVID-19 Literature. Available online: https://libguides.uthscsa.edu/coronavirus/COVD-19_Lit (accessed on 1 August 2022).
- Canadian Agency for Drugs and Technologies in Health. CADTH COVID-19 Search Strings. Available online: https://covid.cadth.ca/literature-searching-tools/cadth-covid-19-search-strings/ (accessed on 1 August 2022).
- World Health Organization. Global Spending on Health: A World in Transition; World Health Organization: Geneva, Switzerland, 2019; pp. 47–48. [Google Scholar]
- National Institutes of Health; National Heart, Lung and Blood Institute. Quality assessment tools. In Health Professional Guidelines Cohort; Bethesda: Rockville, MD, USA, 2014. [Google Scholar]
- Dufault, B.; Klar, N. The quality of modern cross-sectional ecologic studies: A bibliometric review. Am. J. Epidemiol. 2011, 174, 1101–1107. [Google Scholar] [CrossRef]
- Moola, S.M.Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; Mu, P. Critical appraisal tools. In JBI Manual for Evidence Synthesis; Aromataris, E.M.Z., Ed.; JBI: Adelaide, Australia, 2020. [Google Scholar]
- Dzhambov, A.M.; Dimitrova, D.D.; Dimitrakova, E.D. Association between residential greenness and birth weight: Systematic review and meta-analysis. Urban For. Urban Green. 2014, 13, 621–629. [Google Scholar] [CrossRef]
- Nomura, S.; Kawashima, T.; Harada, N.; Yoneoka, D.; Tanoue, Y.; Gilmour, S.; Eguchi, A.; Kawamura, Y.; Hashizume, M. Trends in suicide in Japan by gender during the COVID-19 pandemic, through December 2020. Psychiatry Res. 2021, 300, 113913. [Google Scholar] [CrossRef]
- Nomura, S.; Kawashima, T.; Yoneoka, D.; Tanoue, Y.; Eguchi, A.; Gilmour, S.; Kawamura, Y.; Harada, N.; Hashizume, M. Trends in suicide in Japan by gender during the COVID-19 pandemic, up to September 2020. Psychiatry Res. 2021, 295, 113622. [Google Scholar] [CrossRef]
- Behera, C.; Gupta, S.K.; Singh, S.; Balhara, Y.P.S. Trends in deaths attributable to suicide during COVID-19 pandemic and its association with alcohol use and mental disorders: Findings from autopsies conducted in two districts of India. Asian J. Psychiatry 2021, 58, 102597. [Google Scholar] [CrossRef]
- Bray, M.J.C.; Daneshvari, N.O.; Nestadt, P.S.; Radhakrishnan, I.; Cubbage, J.; Eagle, M.; Southall, P. Racial Differences in Statewide Suicide Mortality Trends in Maryland during the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Psychiatry 2021, 78, 444–447. [Google Scholar] [CrossRef]
- Deisenhammer, E.A.; Kemmler, G. Decreased suicide numbers during the first 6 months of the COVID-19 pandemic. Psychiatry Res. 2021, 295, 113623. [Google Scholar] [CrossRef] [PubMed]
- Faust, J.S.; Du, C.; Krumholz, H.M.; Mayes, K.D.; Li, S.-X.; Lin, Z.; Barnett, M.L. Mortality from Drug Overdoses, Homicides, Unintentional Injuries, Motor Vehicle Crashes, and Suicides during the Pandemic, March-August 2020. JAMA J. Am. Med. Assoc. 2021, 326, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Karakasi, M.-V.; Kevrekidis, D.-P.; Pavlidis, P. The Role of the SARS-CoV-2 Pandemic on Suicide Rates: Preliminary Study in a Sample of the Greek Population. Am. J. Forensic Med. Pathol. 2021, 42, 99–100. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.M. The short-term impact of the COVID-19 outbreak on suicides in Korea. Psychiatry Res. 2021, 295, 113632. [Google Scholar] [CrossRef] [PubMed]
- Marutani, T.; Fuse-Nagase, Y.; Tachikawa, H.; Iwami, T.; Yamamoto, Y.; Moriyama, T.; Yasumi, K. Has COVID-19 affected suicides among graduate students in Japan? Asian J. Psychiatry 2021, 65, 102803. [Google Scholar] [CrossRef] [PubMed]
- Messina, R.; Ciprani, F.; Garbarino, S.; Fornaro, M.; Pompili, M. Suicide mortality data from the Italian police during the COVID-19 pandemic. Ann. Gen. Psychiatry 2021, 20, 28. [Google Scholar]
- Knipe, D.; Silva, T.; Rajapakse, T.; Aroos, A.; Senarathna, L.; Hettiarachchi, N.M.; Galappaththi, S.R.; Spittal, M.J.; Gunnell, D.; Metcalfe, C. Hospital presentations for self-poisoning during COVID-19 in Sri Lanka: An interrupted time-series analysis. Lancet Psychiatry 2021, 8, 892–900. [Google Scholar] [CrossRef]
- Zhang, J.; Currie, J.M.; Schnell, M.K.; Schwandt, H. Trends in Drug Overdose Mortality in Ohio during the First 7 Months of the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e217112. [Google Scholar]
- Yazdi-Feyzabadi, V.; Alipouri Sakha, M.; Zandian, H.; Zahirian Moghadam, T. Alcohol-related mortality during the COVID-19 outbreak in Iran: A commentary on happening a crisis amid another crisis. J. Subst. Use 2021, 27, 435–439. [Google Scholar] [CrossRef]
- Seposo, X.T. COVID-19 threatens decade-long suicide initiatives in Japan. Asian J. Psychiatry 2021, 60, 102660. [Google Scholar] [CrossRef]
- Pokhrel, S.; Sedhai, Y.R.; Atreya, A. An increase in suicides amidst the coronavirus disease 2019 pandemic in Nepal. Med. Sci. Law 2021, 61, 161–162. [Google Scholar] [CrossRef] [PubMed]
- Qin, P.; Mehlum, L. National observation of death by suicide in the first 3 months under COVID-19 pandemic. Acta Psychiatr. Scand. 2021, 143, 92–93. [Google Scholar] [CrossRef] [PubMed]
- Yip, L.; Bixler, D.; Brooks, D.E.; Clarke, K.R.; Datta, S.D.; Dudley, S., Jr.; Komatsu, K.K.; Lind, J.N.; Mayette, A.; Melgar, M. Serious adverse health events, including death, associated with ingesting alcohol-based hand sanitizers containing methanol—Arizona and New Mexico, May–June 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1070. [Google Scholar] [CrossRef]
- Mason, M.; Welch, S.B.; Arunkumar, P.; Post, L.A.; Feinglass, J.M. Notes from the Field: Opioid Overdose Deaths Before, During, and After an 11-Week COVID-19 Stay-at-Home Order—Cook County, Illinois, 1 January 2018–6 October 2020. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 362–363. [Google Scholar] [CrossRef] [PubMed]
- Uğurlu, T.T.; Baltaci, A.S.; Akça, A.; Acar, K. A Case of Suicide Related with Covid-19. Turk Psikiyatri Derg. 2020, 31, 290–293. [Google Scholar] [CrossRef]
- Choudhury, R. An observational analysis of suicidal deaths during COVID 19 pandemic lockdown at Lucknow, India. Indian J. Forensic Med. Toxicol. 2020, 14, 445–449. [Google Scholar] [CrossRef]
- Pirnia, B.; Dezhakam, H.; Pirnia, K.; Malekanmehr, P.; Rezaeian, M. Grief of COVID-19 is a mental contagion, first family suicide in Iran. Asian J. Psychiatry 2020, 54, 102340. [Google Scholar] [CrossRef]
- Forouzanfar, M.M.; Shahini, Z.; Hashemi, B.; Mirbaha, S. Mass Suicide of COVID-19 Patient’s Survivors; a Clinical Experience. Arch. Acad. Emerg. Med. 2021, 9, e13. [Google Scholar] [CrossRef]
- Sakelliadis, E.I.; Katsos, K.D.; Zouzia, E.I.; Spiliopoulou, C.A.; Tsiodras, S. Impact of COVID-19 lockdown on characteristics of autopsy cases in Greece. Comparison between 2019 and 2020. Forensic Sci. Int. 2020, 313, 110365. [Google Scholar] [CrossRef]
- Calati, R.; Gentile, G.; Tambuzzi, S.; Zoja, R.; Fornaro, M. Preliminary suicide trends during the COVID-19 pandemic in Milan, Italy. J. Psychiatr. Res. 2021, 143, 21–22. [Google Scholar] [CrossRef]
- Habu, H.; Takao, S.; Yorifuji, T.; Fujimoto, R.; Naito, H.; Nakao, A. Emergency dispatches for suicide attempts during the COVID-19 outbreak in Okayama, Japan: A descriptive epidemiological study. J. Epidemiol. 2021, 31, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, D.; Saha, S.; Bharatee, P.; Prasad, R. Pattern of suicidal deaths in the first month of lockdown at a tertiary care hospital: A time trend analysis. Indian J. Forensic Med. Toxicol. 2020, 14, 167–172. [Google Scholar] [CrossRef]
- Anzai, T.; Fukui, K.; Ito, T.; Ito, Y.; Takahashi, K. Excess mortality from suicide during the early covid-19 pandemic period in Japan: A time-series modeling before the pandemic. J. Epidemiol. 2021, 31, 152–156. [Google Scholar] [CrossRef]
- Isumi, A.; Doi, S.; Yamaoka, Y.; Takahashi, K.; Fujiwara, T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020, 110, 104680. [Google Scholar] [CrossRef]
- Sakamoto, H.; Ishikane, M.; Ghaznavi, C.; Ueda, P. Assessment of Suicide in Japan During the COVID-19 Pandemic vs. Previous Years. JAMA Netw. Open 2021, 4, e2037378. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021, 5, 229–238. [Google Scholar] [CrossRef]
- Ueda, M.; Nordstrom, R.; Matsubayashi, T. Suicide and mental health during the COVID-19 pandemic in Japan. J. Public Health 2021, 41, 541–548. [Google Scholar] [CrossRef]
- Dwyer, J.; Millar, C.; Lamb, A.; Dwyer, J.; Hiscock, R.; O’Callaghan, C.; Taylor, K.; Bugeja, L. COVID-19 as a context in suicide: Early insights from Victoria, Australia. Aust. N. Z. J. Public Health 2021, 45, 517–522. [Google Scholar] [CrossRef]
- Leske, S.; Kõlves, K.; Crompton, D.; Arensman, E.; de Leo, D. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: An interrupted time-series analysis. Lancet Psychiatry 2021, 8, 58–63. [Google Scholar] [CrossRef]
- COVID-19 Disaster Payment. 2021. Available online: https://www.servicesaustralia.gov.au/covid-19-disaster-payment (accessed on 1 August 2022).
- Faust, J.S.; Shah, S.B.; Du, C.; Li, S.X.; Lin, Z.; Krumholz, H.M. Suicide Deaths during the COVID-19 Stay-at-Home Advisory in Massachusetts, March to May 2020. JAMA Netw. Open 2021, 4, e2034273. [Google Scholar] [CrossRef]
- Barbic, D.; Scheuermeyer, F.X.; Barbic, S.P.; Honer, W.G. Suicide Deaths in British Columbia during the First Wave of the COVID-19 Pandemic. Can. J. Psychiatry 2021, 66, 830–831. [Google Scholar] [CrossRef] [PubMed]
- Radeloff, D.; Papsdorf, R.; Uhlig, K.; Vasilache, A.; Putnam, K.; Von Klitzing, K. Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. Epidemiol. Psychiatr. Sci. 2021, 30, 1–19. [Google Scholar] [CrossRef]
- Calderon-Anyosa, R.J.C.; Bilal, U.; Kaufman, J.S. Variation in non-external and external causes of death in Peru in relation to the COVID-19 lockdown. Yale J. Biol. Med. 2021, 94, 23–40. [Google Scholar] [PubMed]
- Calderon-Anyosa, R.J.C.; Kaufman, J.S. Impact of COVID-19 lockdown policy on homicide, suicide, and motor vehicle deaths in Peru. Prev. Med. 2021, 143, 106331. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, R.; Siwakoti, S.; Singh, S.; Shrestha, A.P. Impact of the COVID-19 pandemic on suicide and self-harm among patients presenting to the emergency department of a teaching hospital in Nepal. PLoS ONE 2021, 16, e0250706. [Google Scholar] [CrossRef]
- Zheng, X.Y.; Tang, S.L.; Ma, S.L.; Guan, W.J.; Xu, X.; Xu, H.; Xu, Y.S.; Xu, Y.J.; Lin, L.F. Trends of injury mortality during the COVID-19 period in Guangdong, China: A population-based retrospective analysis. BMJ Open 2021, 11, e045317. [Google Scholar] [CrossRef]
- Kumar, V.; Biswas, J.; Bhutia, T.Z.; Chhetri, D.; Maitra, R.; Deb, P.K. Demographic studies of autopsied cases at north Bengal medical college hospital during the national lockdown period due to covid 19 pandemic. Indian J. Forensic Med. Toxicol. 2021, 15, 599–603. [Google Scholar]
- Vieson, J.; Yeh, A.B.; Lan, Q.; Sprague, J.E. During the COVID-19 Pandemic, Opioid Overdose Deaths Revert to Previous Record Levels in Ohio. J. Addict. Med. 2021, 16, e118–e122. [Google Scholar] [CrossRef]
- Glober, N.; Mohler, G.; Arkins, T.; O’Donnell, D.; Carter, J.; Huynh, P.; Ray, B. Impact of COVID-19 Pandemic on Drug Overdoses in Indianapolis. J. Urban Health Bull. N.Y. Acad. Med. 2020, 97, 802–807. [Google Scholar] [CrossRef]
- Dumollard, C.; Wiart, J.-F.; Hakim, F.; Demarly, C.; Morbidelli, P.; Allorge, D.; Gaulier, J.-M. Putatively lethal ingestion of isopropyl alcohol-related case: Interpretation of post mortem isopropyl alcohol and acetone concentrations remains challenging. Int. J. Leg. Med. 2020, 135, 175–182. [Google Scholar] [CrossRef]
- Aghababaeian, H.; Hamdanieh, L.; Ostadtaghizadeh, A. Alcohol intake in an attempt to fight COVID-19: A medical myth in Iran. Alcohol 2020, 88, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Shokoohi, M.; Nasiri, N.; Sharifi, H.; Baral, S.; Stranges, S. A syndemic of COVID-19 and methanol poisoning in Iran: Time for Iran to consider alcohol use as a public health challenge? Alcohol 2020, 87, 25–27. [Google Scholar] [CrossRef] [PubMed]
- Hassanian-Moghaddam, H.; Zamani, N.; Kolahi, A.-A.; McDonald, R.; Hovda, K.E. Double trouble: Methanol outbreak in the wake of the COVID-19 pandemic in Iran—A cross-sectional assessment. Crit. Care 2020, 24, 402. [Google Scholar] [CrossRef] [PubMed]
- Simani, L.; Ramezani, M.; Roozbeh, M.; Shadnia, S.; Pakdaman, H. The outbreak of methanol intoxication during COVID-19 pandemic: Prevalence of brain lesions and its predisposing factors. Drug. Chem. Toxicol. 2020, 45, 1500–1503. [Google Scholar] [CrossRef] [PubMed]
- Appa, A.; Gandhi, M.; Imbert, E.; Rodda, L.N.; Cawley, C.; Zevin, B.; Coffin, P.O. Drug Overdose Deaths before and after Shelter-in-Place Orders during the COVID-19 Pandemic in San Francisco. JAMA Netw. Open 2021, 4, e2110452. [Google Scholar] [CrossRef]
- Kitchen, S.A.; Gomes, T.; Murray, R. Measuring the Burden of Opioid-Related Mortality in Ontario, Canada, during the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, 12865. [Google Scholar]
- Mariottini, C.; Ojanperä, I.; Kriikku, P. Increase in drugs-of-abuse findings in post-mortem toxicology due to COVID-19 restrictions—First observations in Finland. Drug Test. Anal. 2021, 13, 867–870. [Google Scholar] [CrossRef]
- Shreffler, J.; Shoff, H.; Thomas, J.J.; Huecker, M. Brief Report: The Impact of COVID-19 on Emergency Department Overdose Diagnoses and County Overdose Deaths. Am. J. Addict. 2021, 30, 330–333. [Google Scholar] [CrossRef]
- Rodda, L.N.; West, K.L.; LeSaint, K.T. Opioid Overdose-Related Emergency Department Visits and Accidental Deaths during the COVID-19 Pandemic. J. Urban Health Bull. N.Y. Acad. Med. 2020, 97, 808–813. [Google Scholar] [CrossRef]
- Slavova, S.; Rock, P.; Bush, H.M.; Quesinberry, D.; Walsh, S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020, 214, 108176. [Google Scholar] [CrossRef]
- UK National Statistical Bulletin. Quarterly Alcohol-Specific Deaths in England and Wales: 2001 to 2019 Registrations and Quarter 1 (Jan to Mar) to Quarter 4 (Oct to Dec) 2020 Provisional Registrations; UK National Statistical Bulletin: Newport, UK, 2021.
- Pines, J.M.; Zocchi, M.S.; Black, B.S.; Carlson, J.N.; Celedon, P.; Moghtaderi, A.; Venkat, A. How emergency department visits for substance use disorders have evolved during the early COVID-19 pandemic. J. Subst. Abuse Treat. 2021, 129, 108391. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.; Akre, S. COVID-19 and the Drug Overdose Crisis: Uncovering the Deadliest Months in the United States, January-July 2020. Am. J. Public Health 2021, 111, 1284–1291. [Google Scholar] [CrossRef] [PubMed]
- Mason, M.; Arukumar, P.; Feinglass, J. The Pandemic Stay-at-Home Order and Opioid-Involved Overdose Fatalities. JAMA J. Am. Med. Assoc. 2021, 325, 2495–2496. [Google Scholar] [CrossRef] [PubMed]
- DiGennaro, C.; Garcia, G.-G.P.; Stringfellow, E.J.; Wakeman, S.; Jalali, M.S. Changes in characteristics of drug overdose death trends during the COVID-19 pandemic. Int. J. Drug Policy 2021, 98, 103392. [Google Scholar] [CrossRef]
- Brothers, S.; Viera, A.; Heimer, R. Changes in methadone program practices and fatal methadone overdose rates in Connecticut during COVID-19. J. Subst. Abuse Treat. 2021, 131, 108449. [Google Scholar] [CrossRef]
- Congdon, L.; Sathanandan, S.; Hazan, J.; Grewal, P. An analysis of initial service transformation in response to the COVID-19 pandemic in two inner-city substance misuse services. J. Subst. Use 2021, 26, 275–279. [Google Scholar]
- Patel, I.; Li, L.; Walter, L.A. Opioid overdose crises during the COVID-19 pandemic: Implication of health disparities. Harm Reduct. J. 2021, 18, 89. [Google Scholar] [CrossRef]
- Rutledge, S.M.; Schiano, T.D.; Im, G.Y.; Florman, S. COVID-19 Aftershocks on Alcohol-Associated Liver Disease: An Early Cross-Sectional Report From the U.S. Epicenter. Hepatol. Commun. 2021, 5, 1151–1155. [Google Scholar] [CrossRef]
- Kim, D.; Ahmed, A.; Bonham, C.A.; Konyn, P.; Cholankeril, G. Mortality Trends in Chronic Liver Disease and Cirrhosis in the United States, Before and During COVID-19 Pandemic. Clin. Gastroenterol. Hepatol. 2021, 19, 2664–2666. [Google Scholar] [CrossRef]
- Osaki, Y.; Otsuki, H.; Imamoto, A.; Kinjo, A.; Fujii, M.; Kuwabara, Y.; Kondo, Y.; Suyama, Y. Suicide rates during social crises: Changes in the suicide rate in Japan after the Great East Japan earthquake and during the COVID-19 pandemic. J. Psychiatr. Res. 2021, 140, 39–44. [Google Scholar] [CrossRef]
- Mitchell, T.O.; Li, L. State-Level Data on Suicide Mortality During COVID-19 Quarantine: Early Evidence of a Disproportionate Impact on Racial Minorities. Psychiatry Res. 2021, 295, 113629. [Google Scholar] [CrossRef] [PubMed]
- Carlin, G.L.; Moftakhar, T.; Negrin, L.L.; Baumgartner, J.S.; Konig, D. Impact of COVID-19 lockdown on suicide attempts: A retrospective analysis of the springtime admissions to the trauma resuscitation room at the Medical University of Vienna from 2015–2020. Wien. Klin. Wochenschr. 2021, 133, 915–922. [Google Scholar] [CrossRef] [PubMed]
- Ontiveros, S.T.; Levine, M.D.; Cantrell, F.L.; Thomas, C.; Minns, A.B. Despair in the time of COVID: A look at suicidal ingestions reported to the California Poison Control System during the pandemic. Acad. Emerg. Med. 2021, 28, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Bantjes, J.; Iemmi, V.; Coast, E.; Channer, K.; Leone, T.; McDaid, D.; Palfreyman, A.; Stephens, B.; Lund, C. Poverty and suicide research in low- and middle-income countries: Systematic mapping of literature published in English and a proposed research agenda. Glob. Ment. Health 2016, 3, e32. [Google Scholar] [CrossRef]
- Kritzinger, S.; Foucault, M.; Lachat, R.; Partheymüller, J.; Plescia, C.; Brouard, S. ‘Rally round the flag’: The COVID-19 crisis and trust in the national government. West Eur. Politics 2021, 44, 1–27. [Google Scholar] [CrossRef]
- Ciccarone, D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr. Opin. Psychiatry 2021, 34, 344–350. [Google Scholar] [CrossRef]
- National Collaborating Centre for Methods and Tools. Rapid Review Update 1: What is the Effect of the COVID-19 Pandemic on Opioid and Substance Use and Related Harms? National Collaborating Centre for Methods and Tools: Hamilton, ON, Canada, 2020.
- Pouso, S.; Borja, Á.; Fleming, L.E.; Gómez-Baggethun, E.; White, M.P.; Uyarra, M.C. Contact with blue-green spaces during the COVID-19 pandemic lockdown beneficial for mental health. Sci. Total Environ. 2021, 756, 143984. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Feng, X. Time for ‘Green’ during COVID-19? Inequities in Green and Blue Space Access, Visitation and Felt Benefits. Int. J. Environ. Res. Public Health 2021, 18, 2757. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Hartig, T.; Eckermann, S.; Nieuwenhuijsen, M.; McMunn, A.; Frumkin, H.; Feng, X. More green, less lonely? A longitudinal cohort study. Int. J. Epidemiol. 2021, 51, 99–110. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Feng, X. Association of Urban Green Space With Mental Health and General Health Among Adults in Australia. JAMA Netw Open 2019, 2, e198209. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Hartig, T.; Putra, I.G.N.E.; Walsan, R.; Dendup, T.; Feng, X. Green space and loneliness: A systematic review with theoretical and methodological guidance for future research. Sci. Total Environ 2022, 847, 157521. [Google Scholar] [CrossRef] [PubMed]
- Sherif, M. Superordinate goals in the reduction of intergroup conflict. Am. J. Sociol. 1958, 63, 349–356. [Google Scholar] [CrossRef]
- Sherif, M. Experiments in group conflict. Sci. Am. 1956, 195, 54–59. [Google Scholar] [CrossRef]
| Component | Included | Excluded |
|---|---|---|
| Participants |
|
|
| Intervention/issue |
| |
| Comparator |
| |
| Outcomes |
|
|
| Study design |
|
|
| Language |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahimi-Ardabili, H.; Feng, X.; Nguyen, P.-Y.; Astell-Burt, T. Have Deaths of Despair Risen during the COVID-19 Pandemic? A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 12835. https://doi.org/10.3390/ijerph191912835
Rahimi-Ardabili H, Feng X, Nguyen P-Y, Astell-Burt T. Have Deaths of Despair Risen during the COVID-19 Pandemic? A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(19):12835. https://doi.org/10.3390/ijerph191912835
Chicago/Turabian StyleRahimi-Ardabili, Hania, Xiaoqi Feng, Phi-Yen Nguyen, and Thomas Astell-Burt. 2022. "Have Deaths of Despair Risen during the COVID-19 Pandemic? A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 19: 12835. https://doi.org/10.3390/ijerph191912835
APA StyleRahimi-Ardabili, H., Feng, X., Nguyen, P.-Y., & Astell-Burt, T. (2022). Have Deaths of Despair Risen during the COVID-19 Pandemic? A Systematic Review. International Journal of Environmental Research and Public Health, 19(19), 12835. https://doi.org/10.3390/ijerph191912835







