Changes in Social and Clinical Determinants of COVID-19 Outcomes Achieved by the Vaccination Program: A Nationwide Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
Study Design and Participants
3. Statistical Analysis
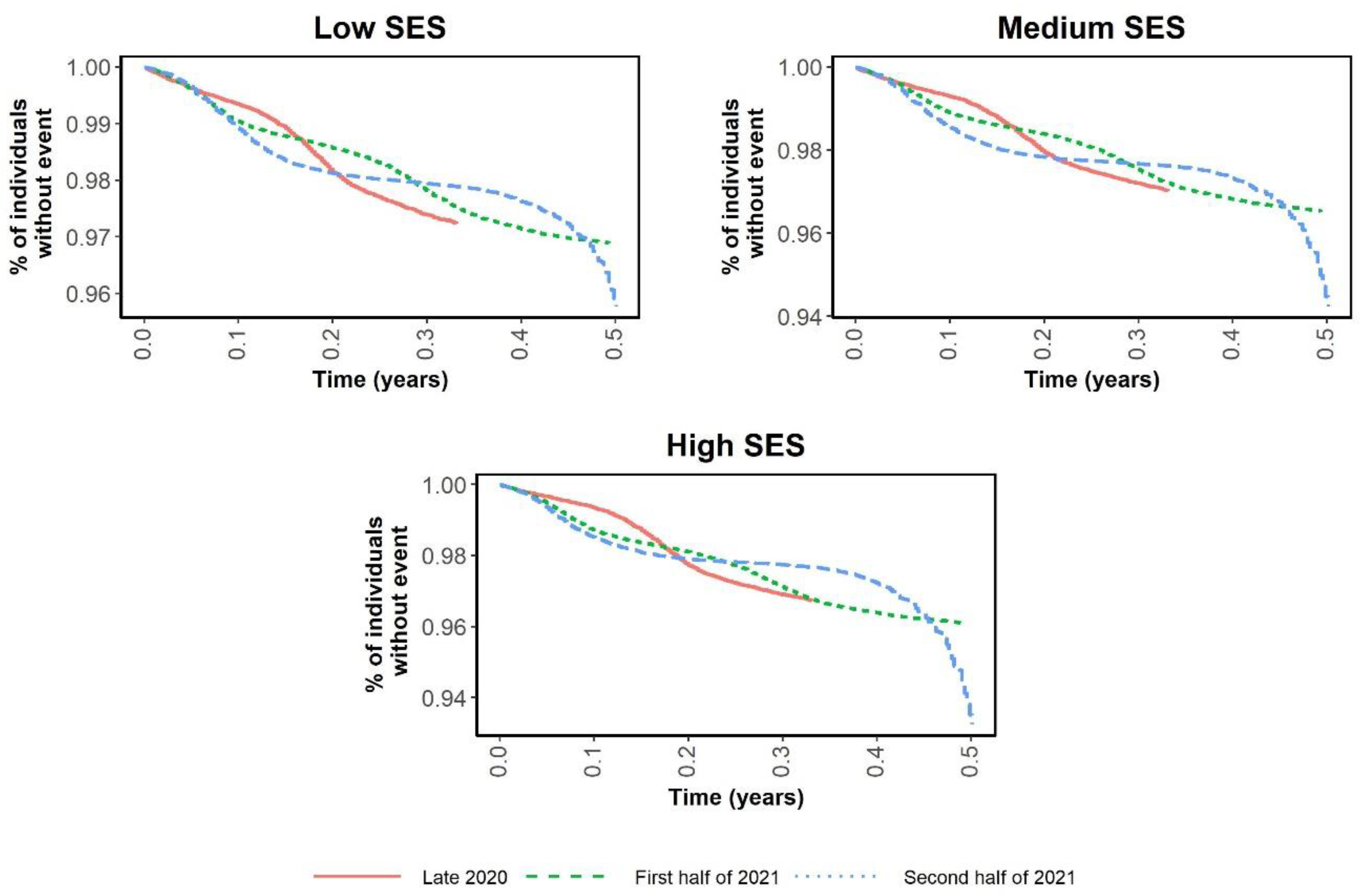
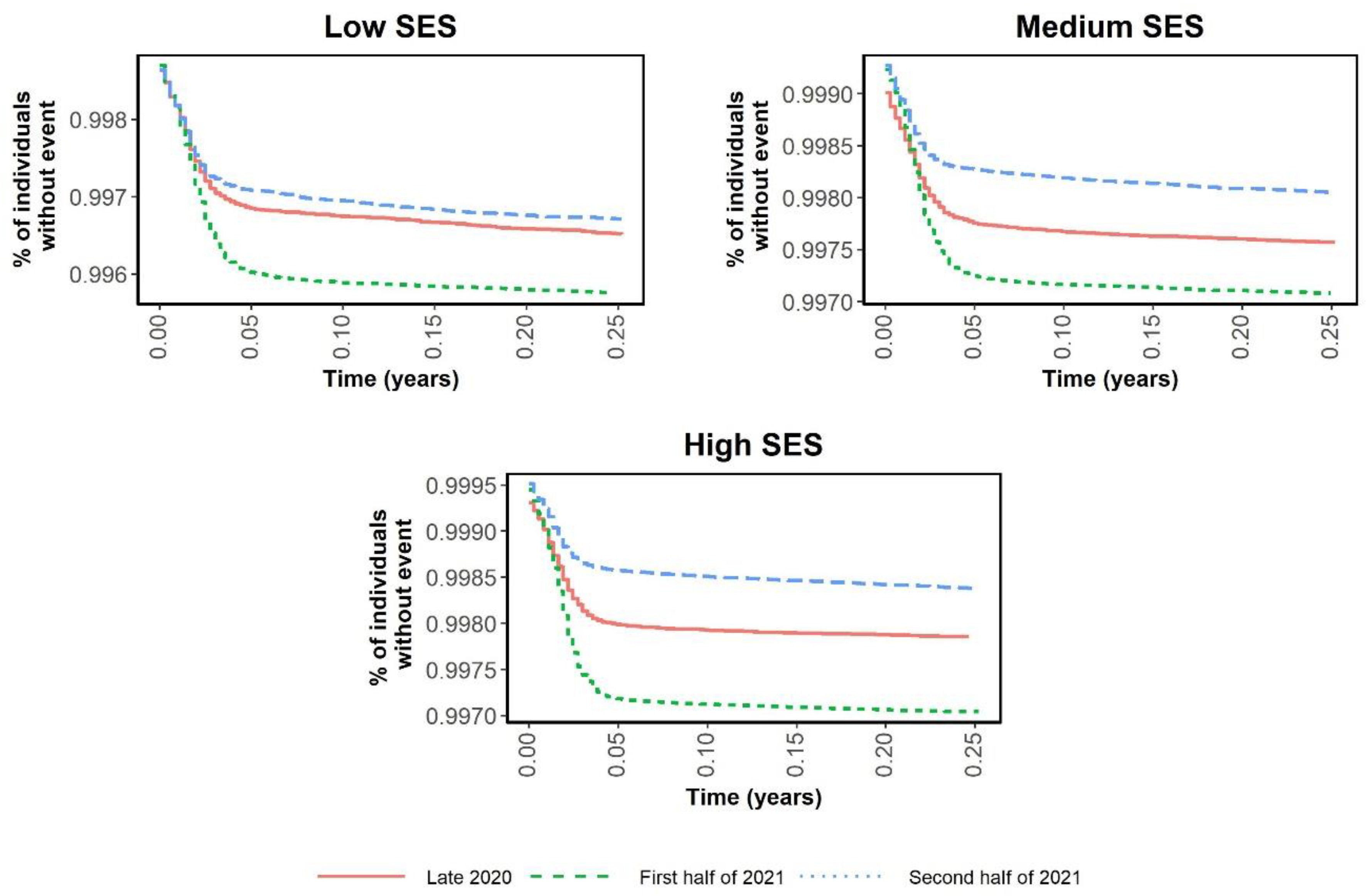
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alamilla, S.G.; Cano, M.Á. COVID-19 and Adverse Social Determinants of Health. Behav. Med. 2022, 48, 67–71. [Google Scholar] [CrossRef]
- Haas, E.J.; Angulo, F.J.; McLaughlin, J.M.; Anis, E.; Singer, S.R.; Khan, F.; Brooks, N.; Smaja, M.; Mircus, G.; Pan, K.; et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: An observational study using national surveillance data. Lancet 2021, 397, 1819–1829. [Google Scholar] [CrossRef]
- Leshem, E.; Lopman, B.A. Population immunity and vaccine protection against infection. Lancet 2021, 397, 1685–1687. [Google Scholar] [CrossRef]
- Wouters, O.J.; Shadlen, K.C.; Salcher-Konrad, M.; Pollard, A.J.; Larson, H.J.; Teerawattananon, Y.; Jit, M. Challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. Lancet 2021, 397, 1023–1034. [Google Scholar] [CrossRef]
- Acosta, A.M.; Garg, S.; Pham, H.; Whitaker, M.; Anglin, O.; O’Halloran, A.; Milucky, J.; Patel, K.; Taylor, C.; Wortham, J.; et al. Racial and Ethnic Disparities in Rates of COVID-19-Associated Hospitalization, Intensive Care Unit Admission, and In-Hospital Death in the United States From March 2020 to February 2021. JAMA Netw. Open 2021, 4, e2130479. [Google Scholar] [CrossRef]
- Khanijahani, A.; Iezadi, S.; Gholipour, K.; Azami-Aghdash, S.; Naghibi, D. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int. J. Equity Health 2021, 20, 248. [Google Scholar] [CrossRef]
- Agyemang, C.; Richters, A.; Jolani, S.; Hendriks, S.; Zalpuri, S.; Yu, E.; Pijls, B.; Prins, M.; Stronks, K.; Zeegers, M.P.; et al. Ethnic minority status as social determinant for COVID-19 infection, hospitalisation, severity, ICU admission and deaths in the early phase of the pandemic: A meta-analysis. BMJ Glob. Health 2021, 6, e007433. [Google Scholar] [CrossRef]
- Manohar, J.; Abedian, S.; Martini, R.; Kulm, S.; Salvatore, M.; Ho, K.; Christos, P.; Campion, T.; Imperato-McGinley, J.; Ibrahim, S.; et al. Social and Clinical Determinants of COVID-19 Outcomes: Modeling Real-World Data from a Pandemic Epicenter. medRxiv 2021. [Google Scholar] [CrossRef]
- Aguiar, M.; Ortuondo, E.M.; Bidaurrazaga Van-Dierdonck, J.; Mar, J.; Stollenwerk, N. Modelling COVID 19 in the Basque Country from introduction to control measure response. Sci. Rep. 2020, 10, 17306. [Google Scholar] [CrossRef]
- Cho, S.I.; Yoon, S.; Lee, H.J. Impact of comorbidity burden on mortality in patients with COVID-19 using the Korean health insurance database. Sci. Rep. 2021, 11, 6375. [Google Scholar] [CrossRef]
- Horton, R. Offline: COVID-19 is not a pandemic. Lancet 2020, 396, 874. [Google Scholar] [CrossRef]
- Brasso, C.; Bellino, S.; Blua, C.; Bozzatello, P.; Rocca, P. The Impact of SARS-CoV-2 Infection on Youth Mental Health: A Narrative Review. Biomedicines 2022, 10, 772. [Google Scholar] [CrossRef]
- Mendenhall, E. The COVID-19 syndemic is not global: Context matters. Lancet 2020, 396, 1731. [Google Scholar] [CrossRef]
- Tuty Kuswardhani, R.A.; Henrina, J.; Pranata, R.; Anthonius Lim, M.; Lawrensia, S.; Suastika, K. Charlson comorbidity index and a composite of poor outcomes in COVID-19 patients: A systematic review and meta-analysis. Diabetes Metab. Syndr. 2020, 14, 2103–2109. [Google Scholar] [CrossRef]
- Vrotsou, K.; Rotaeche, R.; Mateo-Abad, M.; Machón, M.; Vergara, I. Variables associated with COVID-19 severity: An observational study of non-paediatric confirmed cases from the general population of the Basque Country, Spain. BMJ Open 2021, 11, e049066. [Google Scholar] [CrossRef]
- Working group for the surveillance and control of COVID-19 in Spain. The first wave of the COVID-19 pandemic in Spain: Characterisation of cases and risk factors for severe outcomes, as at 27 April 2020. Eurosurveillance 2020, 25, 2001431. [Google Scholar]
- Upshaw, T.L.; Brown, C.; Smith, R.; Perri, M.; Ziegler, C.; Pinto, A.D. Social determinants of COVID-19 incidence and outcomes: A rapid review. PLoS ONE 2021, 16, e0248336. [Google Scholar] [CrossRef]
- White, T.M.; Cash-Gibson, L.; Martin-Moreno, J.M.; Matesanz, R.; Crespo, J.; Alfonso-Sanchez, J.L.; Villapol, S.; El-Mohandes, A.; Lazarus, J.V. COVID-SCORE Spain: Public perceptions of key government COVID-19 control measures. Eur. J. Public Health 2021, 31, 1095–1102. [Google Scholar] [CrossRef]
- Boland, M.R.; Liu, J.; Balocchi, C.; Meeker, J.; Bai, R.; Mellis, I.; Mowery, D.L.; Herman, D. Association of Neighborhood-Level Factors and COVID-19 Infection Patterns in Philadelphia Using Spatial Regression. AMIA Jt. Summits Transl. Sci. Proc. 2021, 2021, 545–554. [Google Scholar]
- Madlock-Brown, C.; Wilkens, K.; Weiskopf, N.; Cesare, N.; Bhattacharyya, S.; Riches, N.O.; Espinoza, J.; Dorr, D.; Goetz, K.; Phuong, J.; et al. Clinical, social, and policy factors in COVID-19 cases and deaths: Methodological considerations for feature selection and modeling in county-level analyses. BMC Public Health 2022, 22, 747. [Google Scholar] [CrossRef]
- Evans, S.J.W.; Jewell, N.P. Vaccine Effectiveness Studies in the Field. N. Engl. J. Med. 2021, 385, 650–651. [Google Scholar] [CrossRef] [PubMed]
- Dagan, N.; Barda, N.; Kepten, E.; Miron, O.; Perchik, S.; Katz, M.A.; Hernán, M.A.; Lipsitch, M.; Reis, B.; Balicer, R.D. BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. N. Engl. J. Med. 2021, 384, 1412–1423. [Google Scholar] [CrossRef] [PubMed]
- Barda, N.; Dagan, N.; Ben-Shlomo, Y.; Kepten, E.; Waxman, J.; Ohana, R.; Hernán, M.A.; Lipsitch, M.; Kohane, I.; Netzer, D.; et al. Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting. N. Engl. J. Med. 2021, 385, 1078–1090. [Google Scholar] [CrossRef] [PubMed]
- Mar, J.; Arrospide, A.; Soto-Gordoa, M.; Iruin, A.; Tainta, M.; Gabilondo, A.; Mar-Barrutia, L.; Calvo, M.; Mateos, M.; Ibarrondo, O. Dementia-related neuropsychiatric symptoms: Inequalities in pharmacological treatment and institutionalization. Neuropsychiatr. Dis. Treat. 2019, 15, 2027–2034. [Google Scholar] [CrossRef] [Green Version]
- Kohli, M.; Maschio, M.; Becker, D.; Weinstein, M.C. The potential public health and economic value of a hypothetical COVID-19 vaccine in the United States: Use of cost-effectiveness modeling to inform vaccination prioritization. Vaccine 2021, 39, 1157–1164. [Google Scholar] [CrossRef]
- Mar, J.; Arrospide, A.; Soto-Gordoa, M.; Machón, M.; Iruin, Á.; Martinez-Lage, P.; Gabilondo, A.; Moreno-Izco, F.; Gabilondo, A.; Arriola, L. Validity of a computerized population registry of dementia based on clinical databases. Neurologia 2021, 36, 418–425. [Google Scholar] [CrossRef]
- Mar, J.; Gorostiza, A.; Ibarrondo, O.; Cernuda, C.; Arrospide, A.; Iruin, Á.; Larrañaga, I.; Tainta, M.; Ezpeleta, E.; Alberdi, A.; et al. Validation of Random Forest Machine Learning Models to Predict Dementia-Related Neuropsychiatric Symptoms in Real-World Data. J. Alzheimers Dis. 2020, 77, 855–864. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Departamento de Salud Gobierno Vasco. DATOS GLOBALES—Vacunación en Población Adulta. 2022. Available online: https://www.euskadi.eus/estrategia-y-datos/web01-a3txerto/es/ (accessed on 18 April 2022).
- Oliver-Parra, A.; Dalmau-Bueno, A.; Ruiz-Muñoz, D.; García-Altés, A. Relationship between parents’ mental disorders and socioeconomic status and offspring’s psychopathology: A cross-sectional study. PLoS ONE 2020, 15, e0240681. [Google Scholar] [CrossRef]
- Lin, D.Y.; Gu, Y.; Wheeler, B.; Young, H.; Holloway, S.; Sunny, S.-K.; Moore, Z.; Zeng, D. Effectiveness of Covid-19 Vaccines over a 9-Month Period in North Carolina. N. Engl. J. Med. 2022, 386, 933–941. [Google Scholar] [CrossRef]
- Cox, D. Regression models and lifetables. R. Stat. Soc. Ser. B Methodol. 1972, 34, 187–202. [Google Scholar]
- Rothman, K.J.; Greenland, S. Modern Epidemiology, 2nd ed.; LWW: Philadelphia, PA, USA, 1998. [Google Scholar]
- Aguiar, M.; Van-Dierdonck, J.B.; Mar, J.; Stollenwerk, N. The role of mild and asymptomatic infections on COVID-19 vaccines performance: A modeling study. J. Adv. Res. 2022, 39, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Gertz, A.; Rader, B.; Sewalk, K.; Brownstein, J.S. Emerging Socioeconomic Disparities in COVID-19 Vaccine Second-Dose Completion Rates in the United States. Vaccines 2022, 10, 121. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, K.H.; Anneser, E.; Toppo, A.; Allen, J.D.; Scott Parott, J.; Corlin, L. Disparities in national and state estimates of COVID-19 vaccination receipt and intent to vaccinate by race/ethnicity, income, and age group among adults ≥ 18 years, United States. Vaccine 2022, 40, 107–113. [Google Scholar] [CrossRef]
- Solís Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Patwary, M.M.; Alam, M.A.; Bardhan, M.; Disha, A.S.; Haque, Z.; Billah, S.M.; Kabir, P.; Browning, M.H.E.M.; Rahman, M.; Parsa, A.D.; et al. COVID-19 Vaccine Acceptance among Low- and Lower-Middle-Income Countries: A Rapid Systematic Review and Meta-Analysis. Vaccines 2022, 10, 427. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, S.F.; Laursen, T.M.; Osler, M.; Hjorthøj, C.; Benros, M.E.; Ethelberg, S.; Mølbak, K.; Nordentoft, M. Vaccination against SARS-CoV-2 infection among vulnerable and marginalised population groups in Denmark: A nationwide population-based study. Lancet Reg Health Eur. 2022, 16, 100355. [Google Scholar] [CrossRef]
- Cantarero-Prieto, D.; Pascual-Sáez, M.; Gonzalez-Prieto, N. Effect of having private health insurance on the use of health care services: The case of Spain. BMC Health Serv. Res. 2017, 17, 716. [Google Scholar] [CrossRef]


| September 2020 to December 2020 | January 2021 to June 2021 | July 2021 to December 2021 | ||||
|---|---|---|---|---|---|---|
| Infected | Not Infected | Infected | Not Infected | Infected | Not Infected | |
| Men | 34,210 (2.98%) | 1,112,476 (97.02%) | 41,959 (3.67%) | 1,100,499 (96.33%) | 68,148 (6.00%) | 1,068,389 (94.00%) |
| Women | 38,244 (3.19%) | 1,158,928 (96.81%) | 43,155 (3.62%) | 1,149,882 (96.38%) | 72,195 (6.08%) | 1,114,933 (93.92%) |
| Age <18 years | 7932 (4.14%) | 183,797 (95.86%) | 10,546 (5.73%) | 173,353 (94.27%) | 13,586 (7.90%) | 158,459 (92.10%) |
| Age 18–50 years | 33,916 (3.29%) | 998,477 (96.71%) | 42,056 (4.10%) | 984,330 (95.90%) | 83,488 (8.22%) | 932,597 (91.78%) |
| Age 50–65 years | 16,912 (3.01%) | 544,245 (96.99%) | 19,330 (3.43%) | 545,017 (96.57%) | 27,610 (4.85%) | 541,683 (95.15%) |
| Age ≥65 years | 13,694 (2.45%) | 544,885 (97.55%) | 13,182 (2.35%) | 547,681 (97.65%) | 15,659 (2.77%) | 550,583 (97.23%) |
| Low income | 6679 (2.77%) | 234,797 (97.23%) | 7501 (3.11%) | 233,506 (96.89%) | 10,116 (4.23%) | 229,011 (95.77%) |
| Medium income | 32,128 (2.99%) | 1,043,585 (97.01%) | 37,325 (3.49%) | 1,033,278 (96.51%) | 61,386 (5.77%) | 1,003,396 (94.23%) |
| High income | 33,647 (3.28%) | 993,022 (96.72%) | 40,288 (3.93%) | 983,597 (96.07%) | 68,841 (6.75%) | 950,915 (93.25%) |
| Charlson 0 | 49,275 (3.04%) | 1,572,181 (96.96%) | 59,542 (3.81%) | 1,503,142 (96.19%) | 100,376 (6.49%) | 1,447,323 (93.51%) |
| Charlson 1–2 | 17,834 (3.17%) | 543,993 (96.83%) | 20,627 (3.78%) | 525,009 (96.22%) | 33,799 (6.17%) | 513,829 (93.83%) |
| Charlson 3–4 | 3187 (3.18%) | 96,929 (96.82%) | 30,490 (3.13%) | 94,462 (96.87%) | 3890 (3.94%) | 94,915 (96.06%) |
| Charlson >4 | 2158 (3.57%) | 58,301 (96.43%) | 18,950 (3.20%) | 57,266 (96.80%) | 2277 (3.77%) | 58,093 (96.23%) |
| Total | 72,454 (3.1%) | 2,271,404 (96.9%) | 85,114 (3.6%) | 2,250,381 (96.4%) | 140,343 (6.0%) | 2,183,322 (94.0%) |
| Full Vaccination as of 1 July 2021 | ||||
|---|---|---|---|---|
| Unvaccinated | Vaccinated | |||
| Low income | 69,089 | 29.6% | 164,355 | 70.4% |
| Medium income | 375,741 | 35.9% | 671,005 | 64.1% |
| High income | 273,287 | 27.6% | 717,964 | 72.4% |
| Total | 718,117 | 31.6% | 1,553,324 | 68.4% |
| 2020-09 to 2020-12 | 2021-01 to 2021-06 | 2021-07 to 2021-12 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Infection | HR | Lower CI | Upper CI | HR | Lower CI | Upper CI | HR | Lower CI | Upper CI |
| Man | Ref. | Ref. | Ref. | ||||||
| Woman | 1.114 *** | 1.098 | 1.13 | 1.022 ** | 1.009 | 1.036 | 1.073 *** | 1.061 | 1.084 |
| Age | 0.991 *** | 0.99 | 0.991 | 0.986 *** | 0.986 | 0.987 | 0.978 *** | 0.977 | 0.978 |
| Low income | Ref. | Ref. | Ref. | ||||||
| Medium income | 1.048 *** | 1.021 | 1.076 | 1.047 *** | 1.021 | 1.073 | 1.215 *** | 1.19 | 1.241 |
| High income | 1.179 *** | 1.148 | 1.211 | 1.203 *** | 1.174 | 1.233 | 1.472 *** | 1.441 | 1.503 |
| Charlson 0 | Ref. | Ref. | Ref. | ||||||
| Charlson 1–2 | 1.138 *** | 1.118 | 1.158 | 1.118 *** | 1.100 | 1.136 | 1.138 *** | 1.124 | 1.153 |
| Charlson 3–4 | 1.380 *** | 1.33 | 1.433 | 1.237 *** | 1.191 | 1.284 | 1.178 *** | 1.14 | 1.218 |
| Charlson >4 | 1.553 *** | 1.486 | 1.624 | 1.267 *** | 1.209 | 1.328 | 1.134 *** | 1.086 | 1.183 |
| Hospitalization | HR | Lower CI | Upper CI | HR | Lower CI | Upper CI | HR | Lower CI | Upper CI |
| Man | Ref. | Ref. | Ref. | ||||||
| Woman | 0.667 *** | 0.627 | 0.709 | 0.674 *** | 0.631 | 0.721 | 0.718 *** | 0.655 | 0.787 |
| Age | 1.044 *** | 1.042 | 1.046 | 1041 *** | 1.039 | 1.043 | 1.016 *** | 1.013 | 1.018 |
| Low income | Ref. | Ref. | Ref. | ||||||
| Medium income | 1.028 | 0.939 | 1.126 | 0.951 | 0.863 | 1.049 | 0.739 *** | 0.654 | 0.835 |
| High income | 0.978 | 0.891 | 1.074 | 0.999 | 0.904 | 1.103 | 0.507 *** | 0.444 | 0.579 |
| Charlson 0 | Ref. | Ref. | Ref. | ||||||
| Charlson 1–2 | 1.759 *** | 1.634 | 1.894 | 1.533 *** | 1.418 | 1.657 | 1.489 *** | 1.332 | 1.663 |
| Charlson 3–4 | 2.706 *** | 2.458 | 2.977 | 2.161 *** | 1.944 | 2.402 | 3.097 *** | 2.665 | 3.598 |
| Charlson >4 | 3.551 *** | 3.203 | 3.937 | 2.597 *** | 2.309 | 2.922 | 4.226 *** | 3.609 | 4.95 |
| ICU admission | HR | Lower CI | Upper CI | HR | Lower CI | Upper CI | HR | Lower CI | Upper CI |
| Man | Ref. | Ref. | Ref. | ||||||
| Woman | 0.339 *** | 0.27 | 0.424 | 0.426 *** | 0.341 | 0.531 | 0.512 *** | 0.375 | 0.7 |
| Age | 1.028 *** | 1.023 | 1.034 | 1.025 *** | 1.019 | 1.031 | 1.005 | 0.997 | 1.013 |
| Low income | Ref. | Ref. | Ref. | ||||||
| Medium income | 1.042 | 0.749 | 1.451 | 1.039 | 0.739 | 1.461 | 0.794 | 0.513 | 1.229 |
| High income | 1.059 | 0.760 | 1.476 | 1.162 | 0.828 | 1.63 | 0.550 * | 0.347 | 0.872 |
| Charlson 0 | Ref. | Ref. | Ref. | ||||||
| Charlson 1–2 | 1.735 *** | 1.376 | 2.187 | 2.120 *** | 1.676 | 2.682 | 1.545 * | 1.096 | 2.178 |
| Charlson 3–4 | 2.135 *** | 1.512 | 3.015 | 2.528 *** | 1.773 | 3.605 | 2.563 *** | 1.494 | 4.396 |
| Charlson >4 | 2.373 *** | 1.597 | 3.524 | 2.445 *** | 1.595 | 3.747 | 1.704 | 0.801 | 3.628 |
| Infection | Hospitalization | ICU Admission | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | Lower CI | Upper CI | HR | Lower CI | Upper CI | HR | Lower CI | Upper CI | |
| Period 2020 | Ref. | Ref. | Ref. | ||||||
| Period 2021-1 | 0.705 *** | 0.698 | 0.713 | 0.886 *** | 0.848 | 0.925 | 0.987 | 0.857 | 1.136 |
| Period 2021-2 | 1.085 *** | 1.074 | 1.096 | 0.451 *** | 0.427 | 0.476 | 0.457 *** | 0.383 | 0.546 |
| Man | Ref. | Ref. | Ref. | ||||||
| Woman | 1.068 *** | 1.061 | 1.076 | 0.680 *** | 0.653 | 0.708 | 0.402 *** | 0.35 | 0.463 |
| Age | 0.983 *** | 0.983 | 0.984 | 1.037 *** | 1.036 | 1.038 | 1.022*** | 1.019 | 1.026 |
| Low income | Ref. | Ref. | Ref. | ||||||
| Medium income | 1.115 *** | 1.1 | 1.13 | 0.936 * | 0.883 | 0.992 | 0.988 | 0.802 | 1.217 |
| High income | 1.306 *** | 1.288 | 1.324 | 0.866 *** | 0.815 | 0.92 | 0.972 | 0.788 | 1.199 |
| Charlson 0 | Ref. | Ref. | Ref. | ||||||
| Charlson 1–2 | 1.134 *** | 1.124 | 1.144 | 1.621 *** | 1.545 | 1.702 | 1.844 *** | 1.59 | 2.139 |
| Charlson 3–4 | 1.259 *** | 1.233 | 1.286 | 2.544 *** | 2.386 | 2.713 | 2.353 *** | 1.88 | 2.946 |
| Charlson >4 | 1.297 *** | 1.264 | 1.331 | 3.264 *** | 3.045 | 3.499 | 2.297 *** | 1.754 | 3.008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibarrondo, O.; Aguiar, M.; Stollenwerk, N.; Blasco-Aguado, R.; Larrañaga, I.; Bidaurrazaga, J.; Estadilla, C.D.S.; Mar, J. Changes in Social and Clinical Determinants of COVID-19 Outcomes Achieved by the Vaccination Program: A Nationwide Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 12746. https://doi.org/10.3390/ijerph191912746
Ibarrondo O, Aguiar M, Stollenwerk N, Blasco-Aguado R, Larrañaga I, Bidaurrazaga J, Estadilla CDS, Mar J. Changes in Social and Clinical Determinants of COVID-19 Outcomes Achieved by the Vaccination Program: A Nationwide Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(19):12746. https://doi.org/10.3390/ijerph191912746
Chicago/Turabian StyleIbarrondo, Oliver, Maíra Aguiar, Nico Stollenwerk, Rubén Blasco-Aguado, Igor Larrañaga, Joseba Bidaurrazaga, Carlo Delfin S. Estadilla, and Javier Mar. 2022. "Changes in Social and Clinical Determinants of COVID-19 Outcomes Achieved by the Vaccination Program: A Nationwide Cohort Study" International Journal of Environmental Research and Public Health 19, no. 19: 12746. https://doi.org/10.3390/ijerph191912746
APA StyleIbarrondo, O., Aguiar, M., Stollenwerk, N., Blasco-Aguado, R., Larrañaga, I., Bidaurrazaga, J., Estadilla, C. D. S., & Mar, J. (2022). Changes in Social and Clinical Determinants of COVID-19 Outcomes Achieved by the Vaccination Program: A Nationwide Cohort Study. International Journal of Environmental Research and Public Health, 19(19), 12746. https://doi.org/10.3390/ijerph191912746






