Retinal and Choroidal Effects of Continuous Positive Airway Pressure as Treatment for Sleep Apnea: Results at 12 Months
Abstract
:1. Introduction
2. Methods
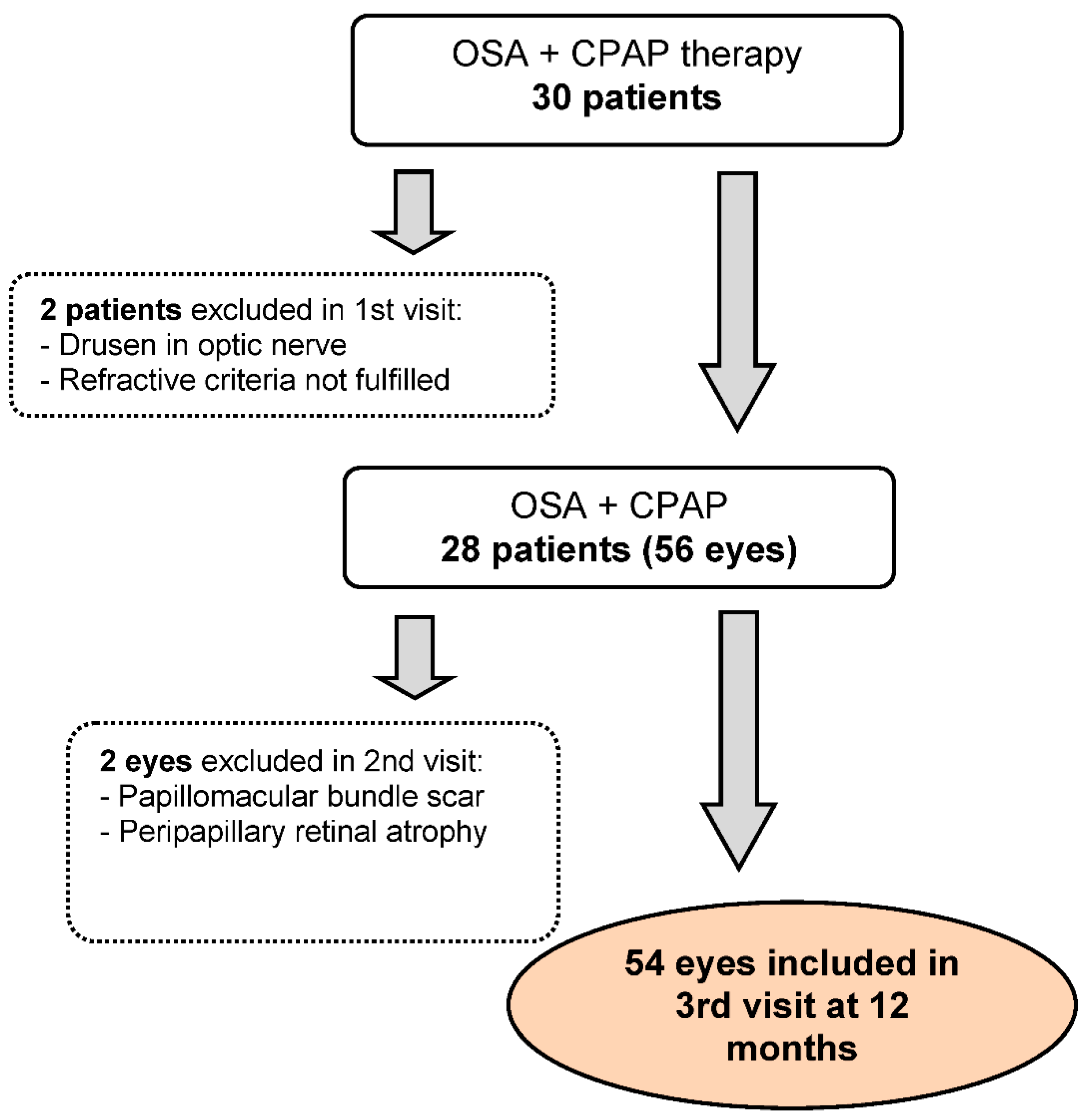
2.1. Study Participants
2.2. Polysomnography
2.3. Ophthalmologic Examination
2.4. CPAP
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHI | apnea hypopnea index |
| CPAP | continuous positive airway pressure |
| F | fovea |
| G | global |
| ICC | intraclass correlation coefficient |
| IIM | inferior inner macula |
| IN | inferonasal |
| IOM | inferior outer macula |
| IOP | intraocular pressure |
| IPL | inner plexiform layer |
| IT | inferotemporal |
| N | nasal |
| NIM | nasal inner macula |
| NOM | nasal outer macula |
| OSA | obstructive sleep apnea |
| PL | photoreceptor layer |
| RGCL | retinal ganglion cell layer |
| RNFL | retinal nerve fiber layer |
| pRNFL | peripapillary retinal nerve fiber layer |
| SAP | standard automated perimetry |
| SIM | superior inner macula |
| SN | superonasal |
| SOM | superior outer macula |
| SpO2 | peripheral oxygen saturation |
| ST | superotemporal |
| T | temporal |
| TIM | temporal inner macula |
| TOM | temporal outer macula |
| TR | total retinal |
| T90 | percentage sleep time spent at SpO2 ≤ 90% |
| VEGF | vascular endothelial growth factor |
| IOP | intraocular pressure |
| SD-OCT | spectral domain ocular coherence tomography |
| OCT-A | ocular coherence tomography angiography |
References
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef] [Green Version]
- Young, T.; Peppard, P.E.; Gottlieb, D.J. Epidemiology of obstructive sleep apnea: A population health perspective. Am. J. Respir. Crit. Care Med. 2002, 165, 1217–1239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baratta, F.; Pastori, D.; Fabiani, M.; Fabiani, V.; Ceci, F.; Lillo, R.; Lolli, V.; Brunori, M.; Pannitteri, G.; Cravotto, E.; et al. Severity of OSAS, CPAP and cardiovascular events: A follow-up study. Eur. J. Clin. Investig. 2018, 48, e12908. [Google Scholar] [CrossRef] [PubMed]
- Levy, P.; Kohler, M.; McNicholas, W.T.; Barbe, F.; McEvoy, R.D.; Somers, V.K.; Lavie, L.; Pepin, J.L. Obstructive sleep apnoea syndrome. Nat. Rev. Dis. Prim. 2015, 1, 15015. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.Y.; Riangwiwat, T.; Rattanawong, P.; Nesmith, B.L.W.; Deobhakta, A. Association of obstructive sleep apnea with central serous chorioretinopathy and choroidal thickness: A Systematic Review and Meta-Analysis. Retina 2018, 38, 1642–1651. [Google Scholar] [CrossRef]
- Lin, P.W.; Friedman, M.; Lin, H.C.; Chang, H.W.; Pulver, T.M.; Chin, C.H. Decreased retinal nerve fiber layer thickness in patients with obstructive sleep apnea/hypopnea syndrome. Graefe’s Arch. Clin. Exp. Ophthalmol. 2011, 249, 585–593. [Google Scholar] [CrossRef]
- Zengin, M.O.; Tuncer, I.; Karahan, E. Retinal nerve fiber layer thickness changes in obstructive sleep apnea syndrome: One year follow-up results. Int. J. Ophthalmol. 2014, 7, 704–708. [Google Scholar] [CrossRef]
- Shiba, T.; Takahashi, M.; Sato, Y.; Onoda, Y.; Hori, Y.; Sugiyama, T.; Bujo, H.; Maeno, T. Relationship between severity of obstructive sleep apnea syndrome and retinal nerve fiber layer thickness. Am. J. Ophthalmol. 2014, 157, 1202–1208. [Google Scholar] [CrossRef]
- Hashim, S.P.; Al Mansouri, F.A.; Farouk, M.; Al Hashemi, A.A.; Singh, R. Prevalence of glaucoma in patients with moderate to severe obstructive sleep apnea: Ocular morbidity and outcomes in a 3 year follow-up study. Eye 2014, 28, 1304–1309. [Google Scholar] [CrossRef] [Green Version]
- Casas, P.; Ascaso, F.J.; Vicente, E.; Tejero-Garces, G.; Adiego, M.I.; Cristobal, J.A. Retinal and optic nerve evaluation by optical coherence tomography in adults with obstructive sleep apnea-hypopnea syndrome (OSAHS). Graefe’s Arch. Clin. Exp. Ophthalmol. 2013, 251, 1625–1634. [Google Scholar] [CrossRef]
- Kur, J.; Newman, E.A.; Chan-Ling, T. Cellular and physiological mechanisms underlying blood flow regulation in the retina and choroid in health and disease. Prog. Retin. Eye Res. 2012, 31, 377–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Portmann, N.; Gugleta, K.; Kochkorov, A.; Polunina, A.; Flammer, J.; Orgul, S. Choroidal blood flow response to isometric exercise in glaucoma patients and patients with ocular hypertension. Investig. Ophthalmol. Vis. Sci. 2011, 52, 7068–7073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papst, N.; Demant, E.; Niemeyer, G. Changes in pO2 induce retinal autoregulation in vitro. Graefe’s Arch. Clin. Exp. Ophthalmol. 1982, 219, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Jelic, S.; Padeletti, M.; Kawut, S.M.; Higgins, C.; Canfield, S.M.; Onat, D.; Colombo, P.C.; Basner, R.C.; Factor, P.; LeJemtel, T.H. Inflammation, oxidative stress, and repair capacity of the vascular endothelium in obstructive sleep apnea. Circulation 2008, 117, 2270–2278. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.; Yoo, C.; Kim, S.W.; Kim, Y.Y. Retinal vessel diameter, retinal nerve fiber layer thickness, and intraocular pressure in korean patients with normal-tension glaucoma. Am. J. Ophthalmol. 2011, 151, 100–105.e1. [Google Scholar] [CrossRef]
- Naranjo-Bonilla, P.; Munoz-Villanueva, M.C.; Gimenez-Gomez, R.; Jurado-Gamez, B. Retinal and choroidal thickness measurements in obstructive sleep apnea: Impacts of continuous positive airway pressure treatment. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 3381–3393. [Google Scholar] [CrossRef]
- Zheng, Y.; Cheung, N.; Aung, T.; Mitchell, P.; He, M.; Wong, T.Y. Relationship of retinal vascular caliber with retinal nerve fiber layer thickness: The singapore malay eye study. Investig. Ophthalmol. Vis. Sci. 2009, 50, 4091–4096. [Google Scholar] [CrossRef] [Green Version]
- Ucak, T.; Unver, E. Alterations in Parafoveal and Optic Disc Vessel Densities in Patients with Obstructive Sleep Apnea Syndrome. J. Ophthalmol. 2020, 2020, 4034382. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, F.A.; Lisboa, R.; Weinreb, R.N.; Liebmann, J.M.; Girkin, C.; Zangwill, L.M. Retinal ganglion cell count estimates associated with early development of visual field defects in glaucoma. Ophthalmology 2013, 120, 736–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jurado-Gamez, B.; Fernandez-Marin, M.C.; Gomez-Chaparro, J.L.; Munoz-Cabrera, L.; Lopez-Barea, J.; Perez-Jimenez, F.; Lopez-Miranda, J. Relationship of oxidative stress and endothelial dysfunction in sleep apnoea. Eur. Respir. J. 2011, 37, 873–879. [Google Scholar] [CrossRef]
- Lloberes, P.; Duran-Cantolla, J.; Martinez-Garcia, M.A.; Marin, J.M.; Ferrer, A.; Corral, J.; Masa, J.F.; Parra, O.; Alonso-Alvarez, M.L.; Teran-Santos, J. Diagnosis and treatment of sleep apnea-hypopnea syndrome. Spanish Society of Pulmonology and Thoracic Surgery. Arch. Bronconeumol. 2011, 47, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Jurado-Gamez, B.; Bardwell, W.A.; Cordova-Pacheco, L.J.; Garcia-Amores, M.; Feu-Collado, N.; Buela-Casal, G. A basic intervention improves CPAP adherence in sleep apnoea patients: A controlled trial. Sleep Breath. 2015, 19, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Xiao, K.; Huang, J.; Sun, X.; Jiang, C. Reduced Retinal Vessel Density in Obstructive Sleep Apnea Syndrome Patients: An Optical Coherence Tomography Angiography Study. Investig. Ophthalmol. Vis. Sci. 2017, 58, 3506–3512. [Google Scholar] [CrossRef]
- Wang, J.S.; Xie, H.T.; Jia, Y.; Zhang, M.C. Retinal nerve fiber layer thickness changes in obstructive sleep apnea syndrome: A systematic review and Meta-analysis. Int. J. Ophthalmol. 2016, 9, 1651–1656. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Liu, P.; Guan, J.; Lu, Y.; Su, K. Association between glaucoma and obstructive sleep apnea syndrome: A meta-analysis and systematic review. PLoS ONE 2015, 10, e0115625. [Google Scholar] [CrossRef]
- Kivela, T.; Hietanen, J.; Uusitalo, M. Autopsy analysis of clinically unilateral exfoliation syndrome. Investig. Ophthalmol. Vis. Sci. 1997, 38, 2008–2015. [Google Scholar]
- Lin, P.W.; Friedman, M.; Lin, H.C.; Chang, H.W.; Wilson, M.; Lin, M.C. Normal tension glaucoma in patients with obstructive sleep apnea/hypopnea syndrome. J. Glaucoma 2011, 20, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Mojon, D.S.; Hess, C.W.; Goldblum, D.; Fleischhauer, J.; Koerner, F.; Bassetti, C.; Mathis, J. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology 1999, 106, 1009–1012. [Google Scholar] [CrossRef]
- Lin, P.W.; Lin, H.C.; Friedman, M.; Chang, H.W.; Salapatas, A.M.; Lin, M.C.; Chen, Y.C. Effects of CPAP for patients with OSA on visual sensitivity and retinal thickness. Sleep Med. 2020, 67, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Antic, N.A.; Catcheside, P.; Buchan, C.; Hensley, M.; Naughton, M.T.; Rowland, S.; Williamson, B.; Windler, S.; McEvoy, R.D. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep 2011, 34, 111–119. [Google Scholar] [CrossRef] [Green Version]
- Yu, J.; Gu, R.; Zong, Y.; Xu, H.; Wang, X.; Sun, X.; Jiang, C.; Xie, B.; Jia, Y.; Huang, D. Relationship Between Retinal Perfusion and Retinal Thickness in Healthy Subjects: An Optical Coherence Tomography Angiography Study. Investig. Ophthalmol. Vis. Sci. 2016, 57, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Abdullayev, A.; Tekeli, O.; Yanik, O.; Acican, T.; Gulbay, B. Investigation of the Presence of Glaucoma in Patients with Obstructive Sleep Apnea Syndrome Using and Not Using Continuous Positive Airway Pressure Treatment. Turk. J. Ophthalmol. 2019, 49, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.K.; Ye, C.; Weinreb, R.N.; Cheung, C.Y.; Qiu, Q.; Liu, S.; Xu, G.; Lam, D.S. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography a study on diagnostic agreement with Heidelberg Retinal Tomograph. Ophthalmology 2010, 117, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Dioum, E.M.; Chen, R.; Alexander, M.S.; Zhang, Q.; Hogg, R.T.; Gerard, R.D.; Garcia, J.A. Regulation of hypoxia-inducible factor 2alpha signaling by the stress-responsive deacetylase sirtuin 1. Science 2009, 324, 1289–1293. [Google Scholar] [CrossRef]
- Liu, J.; Narasimhan, P.; Yu, F.; Chan, P.H. Neuroprotection by hypoxic preconditioning involves oxidative stress-mediated expression of hypoxia-inducible factor and erythropoietin. Stroke 2005, 36, 1264–1269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaal, S.; Sherman, M.P.; Nesmith, B.; Barak, Y. Untreated Obstructive Sleep Apnea Hinders Response to Bevacizumab in Age-Related Macular Degeneration. Retina 2016, 36, 791–797. [Google Scholar] [CrossRef]
- Sivaprasad, S.; Arden, G. Spare the rods and spoil the retina: Revisited. Eye 2016, 30, 189–192. [Google Scholar] [CrossRef]
- Lee, A.G.; Golnik, K.; Kardon, R.; Wall, M.; Eggenberger, E.; Yedavally, S. Sleep apnea and intracranial hypertension in men. Ophthalmology 2002, 109, 482–485. [Google Scholar] [CrossRef]
- Jurado-Gamez, B.; Bujalance Cabrera, C.; Caballero Ballesteros, L.; Marin Hinojosa, C.; Munoz Cabrera, L.; Perez-Jimenez, F.; Lopez-Miranda, J. Association of cellular adhesion molecules and oxidative stress with endothelial function in obstructive sleep apnea. Intern. Med. 2012, 51, 363–368. [Google Scholar] [CrossRef]


| Patients No. (% or ± SD) n = 28 | |
|---|---|
| Sex (men) | 26 (92.9) |
| Age (years) | 57 (±9) |
| BMI (Kg/m2) | 32.1 (±4.8) |
| Glaucoma (%) | 2 (7.14) |
| AMI (%) | 1 (3.6) |
| Smoker (%) | 4 (14.3) |
| AHT (%) | 12 (42.9) |
| Hyperlipidemia (%) | 11 (39.3) |
| DMII (%) | 7 (25.0) |
| Hyperuricemia (%) | 4 (14.3) |
| CKD (%) | 1 (3.6) |
| Anemia (%) | 1 (3.6) |
| Psoriasis (%) | 1 (3.6) |
| Hypothyroidism (%) | 1 (3.6) |
| Arrhythmia (%) | 1 (3.6) |
| Severe OSA (%) | 27 (96.4) |
| AHI (events/h) | 61.8 (±21.5) |
| CPAP use (h) | 5.09 (±1.83) |
| ODI (events/h) | 66.8 (±21.6) |
| T90 (%) | 13.0 (±12.2) |
| SpO2 mean (%) | 91.2 (±3.5) |
| SpO2 minimum (%) | 77.0 (±10.7) |
| Baseline | 3 Months | 12 Months | P* Raw | P** Adjusted (1) (2) (3) | |
|---|---|---|---|---|---|
| IOP (mmHg) | 14.65 (±3.27) | 14.13 (±2.41) | 15.27 (±2.93) | 0.039 | 0.241 0.231 0.001 |
| LogMAR | −0.04 (±0.08) | −0.06 (±0.09) | −0.07 (±0.08) | 0.121 | NA |
| VFI (%) | 98.13 (±2.21) | 97.81 (±2.44) | 98.38 (±1.76) | 0.499 | NA |
| VF MD (decibels) | −2.20 (±1.24) | −2.16 (±1.23) | −2.10 (±1.04) | 0.472 | NA |
| Baseline | 3 Months | 12 Months | P* Raw | P** Adjusted (1) (2) (3) | |
|---|---|---|---|---|---|
| RNFL_G | 97.98 (±9.12) | 99.51 (±9.55) | 98.96 (±9.02) | <0.001 | <0.001 0.012 0.535 |
| RNFL_T | 72.94 (±12.67) | 74.24 (±13.60) | 73.69 (±12.61) | 0.046 | 0.003 0.364 0.999 |
| RNFL_ST | 135.80 (±21.44) | 136.04 (±21.83) | 136.57 (±21.26) | 0.581 | NA |
| RNFL_SN | 111.94 (±24.92) | 114.37 (±25.12) | 113.06 (±24.36) | 0.014 | 0.004 0.170 0.215 |
| RNFL_N | 72.43 (±11.45) | 74.43 (±11.63) | 73.24 (±10.81) | 0.001 | 0.001 0.392 0.137 |
| RNFL_IN | 101.94 (±20.31) | 103.82 (±20.38) | 103.94 (±20.25) | 0.030 | 0.001 0.050 0.237 |
| RNFL_IT | 143.49 (±18.88) | 144.82 (±20.31) | 143.61 (±18.25) | 0.135 | NA |
| Baseline | 3 Months | 12 Months | P* Raw | P** Adjusted (1) (2) (3) | |
|---|---|---|---|---|---|
| TR | |||||
| F | 284.82 (±20.93) | 286.61 (±21.51) | 286.37 (±20.96) | 0.035 | 0.010 0.134 0.999 |
| IIM | 342.90 (±17.56) | 345.10 (±18.46) | 344.75 (±18.05) | <0.001 | <0.001 <0.001 0.999 |
| IOM | 289.10 (±16.79) | 290.55 (±17.42) | 290.06 (±17.37) | 0.003 | 0.007 0.081 0.659 |
| TIM | 332.82 (±16.20) | 333.53 (±20.05) | 335.29 (±16.09) | 0.091 | 0.999 <0.001 0.496 |
| TOM | 285.57 (±21.00) | 286.94 (±17.27) | 284.80 (±15.97) | 0.003 | <0.001 0.108 0.120 |
| SIM | 346.51 (±17.68) | 348.25 (±18.53) | 347.47 (±18.08) | 0.001 | 0.001 0.139 0.245 |
| SOM | 297.71 (±17.20) | 299.04 (±18.53) | 298.06 (±17.41) | 0.018 | 0.057 0.999 0.079 |
| NIM | 348.31 (±16.48) | 350.92 (±18.33) | 350.98 (±17.66) | 0.016 | 0.056 0.062 0.999 |
| NOM | 316.53 (±20.07) | 317.55 (±18.80) | 315.94 (±18.75) | 0.199 | NA |
| RGCL | |||||
| F | 18.85 (±6.22) | 18.60 (±6.04) | 18.40 (±6.05) | 0.232 | NA |
| IIM | 53.35 (±5.35) | 53.54 (±5.99) | 53.40 (±5.77) | 0.787 | NA |
| IOM | 33.44 (±4.43) | 33.31 (±4.31) | 33.58 (±3.89) | 0.107 | NA |
| TIM | 49.48 (±5.91) | 49.29 (±6.46) | 49.52 (±6.04) | 0.650 | NA |
| TOM | 36.17 (±4,74) | 36.23 (±5.07) | 36.06 (±4.75) | 0.796 | NA |
| SIM | 53.79 (±5.26) | 54.12 (±5.61) | 54.63 (±5.86) | <0.001 | 0.312 <0.001 0.048 |
| SOM | 34.98 (±3.98) | 35.10 (±4.02) | 35.15 (±4.07) | 0.623 | NA |
| NIM | 52.75 (±6.12) | 52.40 (±6.87) | 52.71 (±6.61) | 0.712 | NA |
| NOM | 38.13 (±4.58) | 38.46 (±5.09) | 38.62 (±5.41) | 0.173 | NA |
| IPL | |||||
| F | 23.77 (±4.36) | 23.79 (±4.46) | 23.75 (±4.15) | 0.988 | NA |
| IIM | 41.92 (±4.06) | 42.29 (±4.04) | 42.37 (±4.30) | 0.161 | NA |
| IOM | 27.02 (±3.24) | 27.23 (±3.40) | 27.04 (±3.15) | 0.375 | NA |
| TIM | 42.40 (±3.99) | 43.25 (±4.03) | 43.10 (±4.04) | 0.004 | 0.002 0.056 0.999 |
| TOM | 32.67 (±3.44) | 33.02 (±3.34) | 32.81 (±3.38) | 0.107 | NA |
| SIM | 42.48 (±3.76) | 42.85 (±3.56) | 42.52 (±4.27) | 0.261 | NA |
| SOM | 28.58 (±3.24) | 28.77 (±3.42) | 28.77 (±3.31) | 0.281 | NA |
| NIM | 43.46 (±3.88) | 43.77 (±4.00) | 44.02 (±3.81) | 0.079 | 0.061 0.046 0.999 |
| NOM | 29.33 (±3.27) | 29.54 (±3.23) | 29.31 (±3.31) | 0.226 | NA |
| PL | |||||
| F | 87.85 (±4.33) | 87.71 (±4.92) | 87.50 (±3.80) | 0.650 | NA |
| IIM | 79.08 (±2.70) | 79.52 (±3.05) | 78.60 (±4.90) | 0.146 | NA |
| IOM | 76.81 (±2.23) | 77.08 (±2.19) | 75.92 (±5.09) | 0.166 | NA |
| TIM | 80.08 (±2.91) | 80.33 (±2.87) | 79.69 (±3.03) | 0.105 | NA |
| TOM | 77.15 (±2.38) | 77.37 (±2.43) | 76.60 (±4.12) | 0.466 | NA |
| SIM | 80.25 (±2.81) | 80.17 (±2.86) | 79.88 (±2.72) | 0.847 | NA |
| SOM | 78.52 (±2.81) | 78.65 (±2.56) | 78.06 (±3.23) | 0.178 | NA |
| NIM | 80.98 (±3.03) | 81.62 (±3.19) | 80.98 (±3.37) | 0.130 | NA |
| NOM | 77.94 (±2.51) | 78.31 (±2.38) | 77.65 (±4.41) | 0.318 | NA |
| Baseline | 3 Months | 12 Months | P* Raw | P** Adjusted (1) (2) (3) | |
|---|---|---|---|---|---|
| Fovea | 268.84 (±61.66) | 257.68 (±61.16) | 262.36 (±59.63) | 0.079 | 0.116 0.456 0.999 |
| Temporal | 259.75 (±65.06) | 247.52 (±59.33) | 250.73 (±60.19) | 0.007 | 0.014 0.038 0.999 |
| Nasal | 249.70 (±66.64) | 246.52 (±66.57) | 244.86 (±64.61) | 0.517 | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naranjo-Bonilla, P.; Giménez-Gómez, R.; Muñoz-Villanueva, M.d.C.; Jurado-Gámez, B. Retinal and Choroidal Effects of Continuous Positive Airway Pressure as Treatment for Sleep Apnea: Results at 12 Months. Int. J. Environ. Res. Public Health 2022, 19, 12637. https://doi.org/10.3390/ijerph191912637
Naranjo-Bonilla P, Giménez-Gómez R, Muñoz-Villanueva MdC, Jurado-Gámez B. Retinal and Choroidal Effects of Continuous Positive Airway Pressure as Treatment for Sleep Apnea: Results at 12 Months. International Journal of Environmental Research and Public Health. 2022; 19(19):12637. https://doi.org/10.3390/ijerph191912637
Chicago/Turabian StyleNaranjo-Bonilla, Pedro, Rafael Giménez-Gómez, María del Carmen Muñoz-Villanueva, and Bernabé Jurado-Gámez. 2022. "Retinal and Choroidal Effects of Continuous Positive Airway Pressure as Treatment for Sleep Apnea: Results at 12 Months" International Journal of Environmental Research and Public Health 19, no. 19: 12637. https://doi.org/10.3390/ijerph191912637
APA StyleNaranjo-Bonilla, P., Giménez-Gómez, R., Muñoz-Villanueva, M. d. C., & Jurado-Gámez, B. (2022). Retinal and Choroidal Effects of Continuous Positive Airway Pressure as Treatment for Sleep Apnea: Results at 12 Months. International Journal of Environmental Research and Public Health, 19(19), 12637. https://doi.org/10.3390/ijerph191912637







