Decision Tree-Based Foot Orthosis Prescription for Patients with Pes Planus
Abstract
:1. Introduction
2. Related Study
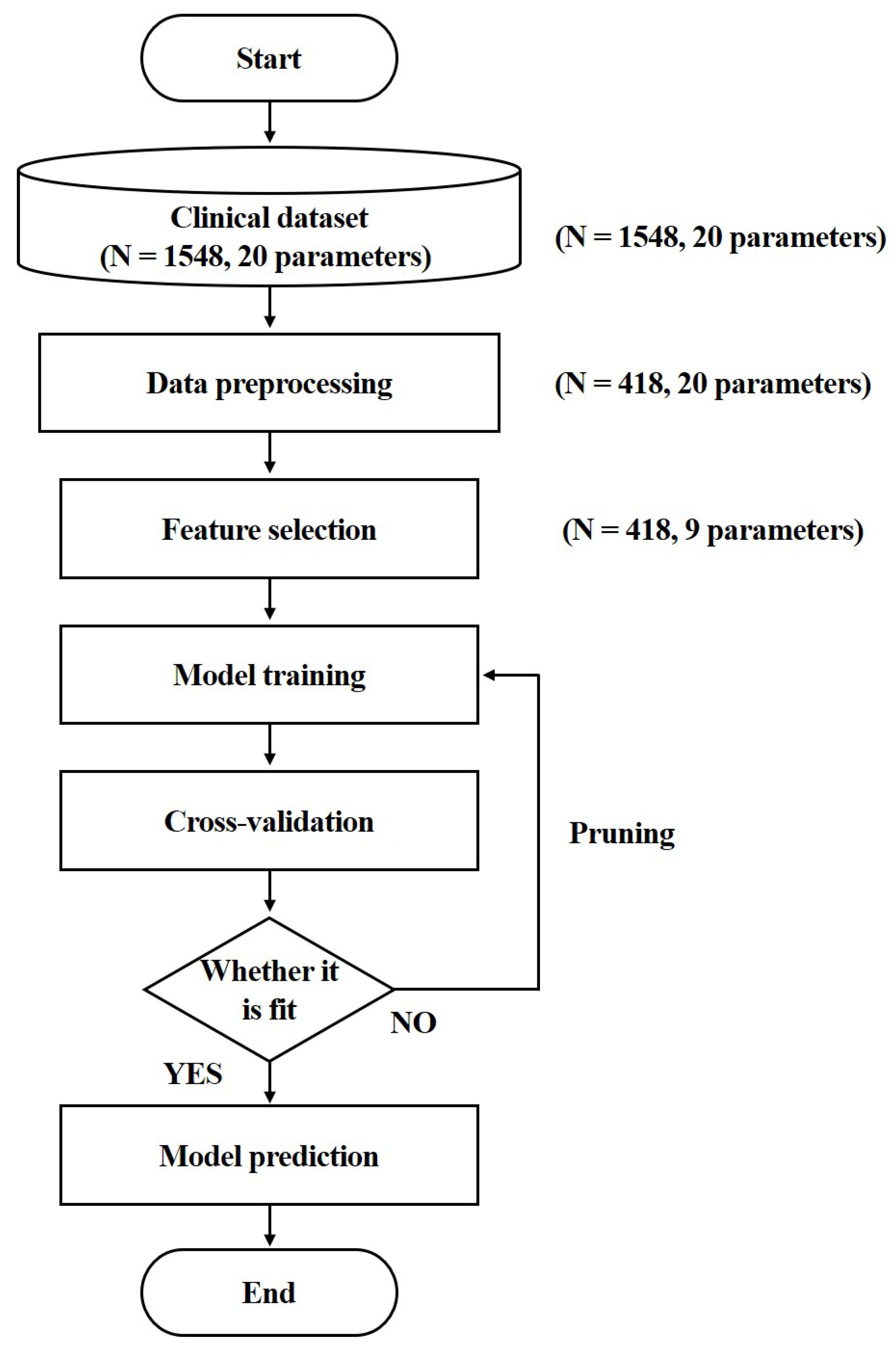
3. Methodology
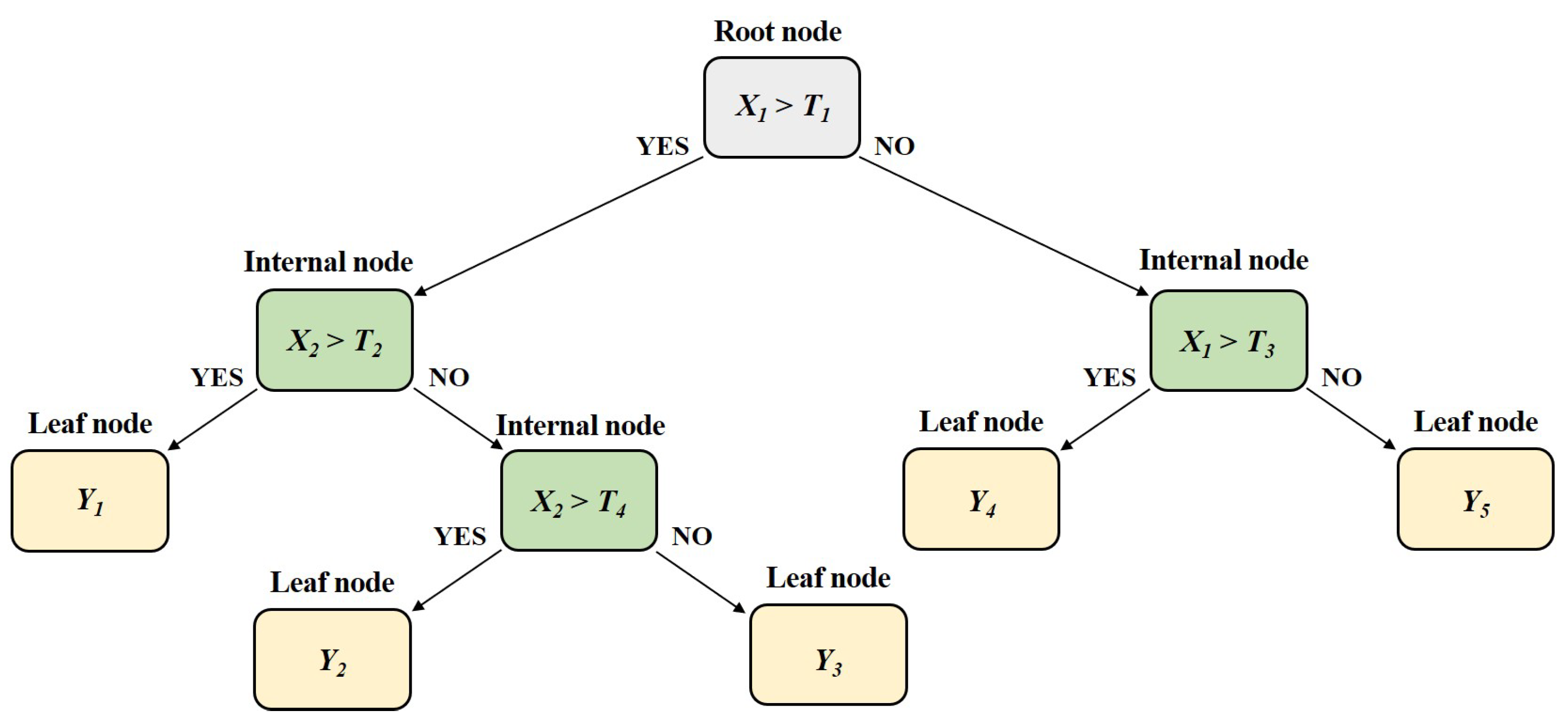
3.1. CART Algorithm
3.2. Dataset Description
3.3. Dataset Splitting
3.4. Pruning
3.5. Evaluation Metrics
4. Results
5. Discussion
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ramanathan, A.K.; Kiran, P.; Arnold, G.P.; Wang, W.; Abboud, R.J. Repeatability of the Pedar-X® in-shoe pressure measuring system. Foot Ankle Surg. 2010, 16, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Chou, M.C.; Huang, J.Y.; Hung, Y.M.; Perng, W.T.; Chang, R.; Wei, J.C.C. Flat foot and spinal degeneration: Evidence from nationwide population-based cohort study. J. Formos. Med. Assoc. 2021, 120, 1897–1906. [Google Scholar] [CrossRef] [PubMed]
- Jafarnezhadgero, A.; Shad, M.M.; Ferber, R. The effect of foot orthoses on joint moment asymmetry in male children with flexible flat feet. J. Bodyw. Mov. Ther. 2018, 22, 83–89. [Google Scholar] [CrossRef]
- Cebulski-Delebarre, A.; Boutry, N.; Szymanski, C.; Maynou, C.; Lefebvre, G.; Amzallag-Bellenger, E.; Cotten, A. Correlation between primary flat foot and lower extremity rotational misalignment in adults. J. Diagn. Interv. Imaging 2016, 97, 1151–1157. [Google Scholar] [CrossRef] [PubMed]
- Pita-Fernandez, S.; Gonzalez-Martin, C.; Alonso-Tajes, F.; Seoane-Pillado, T.; Pertega-Diaz, S.; Perez-Garcia, S.; Seijo-Bestilleiro, R.; Balboa-Barreiro, V. Flat Foot in a Random Population and its Impact on Quality of Life and Functionality. J. Clin. Diagn. Res. 2017, 11, LC22–LC27. [Google Scholar] [CrossRef]
- Ataabadi, P.A.; Abbassi, A.; Letafatkar, A.; Vanwanseele, B. The Effects of Foot Orthosis and Low-Dye Tape on Lower Limb Joint Angles and Moments During Running in Individuals with Pes Planus. Gait Posture 2017, 96, 154–159. [Google Scholar] [CrossRef]
- Demetracopoulos, C.A.; Nair, P.; Malzberg, A.; Del, J.T. Outcomes of a stepcut lengthening calcaneal osteotomy for adult-acquired flatfoot deformity. Foot Ankle Int. 2015, 36, 749–755. [Google Scholar] [CrossRef]
- Dars, S.; Uden, H.; Banwell, H.A.; Kumar, S. The effectiveness of non-surgical intervention (Foot Orthoses) for paediatric flexible pes planus: A systematic review: Update. PLoS ONE 2018, 13, e0193060. [Google Scholar] [CrossRef]
- Elftman, N.W. Nonsurgical treatment of adult acquired flat foot deformity. Foot Ankle Clin. 2003, 8, 473–489. [Google Scholar] [CrossRef]
- Bok, S.K.; Kim, B.O.; Lim, J.H.; Ahn, S.Y. Effects of custom-made rigid foot orthosis on pes planus in children over 6 years old. Ann. Rehabil. Med. 2014, 38, 369–375. [Google Scholar] [CrossRef]
- Akbari, M.; Mohammadi, M.; Saeedi, H. Effects of rigid and soft foot orthoses on dynamic balance in females with flatfoot. Med. J. Islam. Repub. Iran 2007, 21, 91–97. [Google Scholar]
- Xu, R.; Wang, Z.; Ren, Z.; Ma, T.; Jia, Z.; Fang, S.; Jin, H. Comparative study of the effects of customized 3D printed insole and prefabricated insole on plantar pressure and comfort in patients with symptomatic flatfoot. Med. Sci. Monit. 2019, 25, 3510. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, H.; Mousavi, M.E.; Majddoleslam, B.; Rahgozar, M.; Aminian, G.; Tabatabai; Ghomshe, F.; Movahedi; Yeganeh, M. The evaluation of modified foot orthosis on muscle activity and kinetic in a subject with flexible flat foot: Single case study. Prosthet. Orthot. Int. 2014, 38, 160–166. [Google Scholar] [CrossRef]
- Kaddi, S.S.; Patil, M.M. Forecasting the Survival Rate of Breast Cancer Patients using a Supervised Learning Method. Glob. Transit. Proc. 2022, 3, 25–30. [Google Scholar] [CrossRef]
- Chae, J.; Kang, Y.J.; Noh, Y. A deep-learning approach for foot-type classification using heterogeneous pressure data. Sensors 2020, 20, 4481. [Google Scholar] [CrossRef]
- Mei, Z.; Ivanov, K.; Zhao, G.; Wu, Y.; Liu, M.; Wang, L. Foot type classification using sensor-enabled footwear and 1D-CNN. Measurement 2020, 165, 108184. [Google Scholar] [CrossRef]
- Eksen, K.; Serif, S.; Serif, T. Remote pre-diagnosis of pes planus and pes cavus using arch index. Eur. J. Eng. Sci. Tech. 2021, 28, 1321–1329. [Google Scholar] [CrossRef]
- Li, H.; Huang, Z.; Fu, J.; Li, Y.; Zeng, N.; Zhang, J.; Ye, C.; Jin, L. Modified weights-and-structure-determination neural network for pattern classification of flatfoot. IEEE Access 2019, 7, 63146–63154. [Google Scholar] [CrossRef]
- Aruntammanak, W.; Aunhathaweesup, Y.; Wongseree, W.; Leelasantitham, A.; Kiattisin, S. Diagnose flat foot from foot print image based on neural network. In Proceedings of the 6th 2013 Biomedical Engineering International Conference, Amphur Muang, Thailand, 23–25 October 2013. [Google Scholar]
- Ardhianto, P.; Subiakto, R.B.R.; Lin, C.Y.; Jan, Y.K.; Liau, B.Y.; Tsai, J.Y.; Akbari, V.B.H.; Lung, C.W. A Deep Learning Method for Foot Progression Angle Detection in Plantar Pressure Images. Sensors 2022, 22, 2786. [Google Scholar] [CrossRef]
- Ture, M.; Tokatli, F.; Kurt, I. Using Kaplan-Meier analysis together with decision tree methods (C&RT, CHAID, QUEST, C4. 5 and ID3) in determining recurrence-free survival of breast cancer patient. Expert Syst. Appl. 2009, 36, 2017–2026. [Google Scholar]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification and Regression Tree, 1st ed.; Routledge: Oxfordshire, UK, 2017; pp. 154–196. [Google Scholar]
- Tang, R.; Zhang, X. CART decision tree combined with boruta feature selection for medical data classification. In Proceedings of the 2020 5th IEEE International Conference on Big Data Analytics (ICBDA), Xiamen, China, 8–11 May 2020. [Google Scholar]
- Xie, T.; Li, R.; Zhang, X.; Zhou, B.; Wang, Z. Research on heartbeat classification algorithm based on CART decision tree. In Proceedings of the 2019 8th International Symposium on Next Generation Electronics (ISNE), Zhengzhou, China, 9–10 October 2019. [Google Scholar]
- Aziza, E.Z.; El Amine, L.M.; Mohamed, M.; Abdelhafid, B. Decision tree cart algorithm for diabetic retinopathy classification. In Proceedings of the 2019 6th International Conference on Image and Signal Processing and their Applications (ISPA), Mostaganem, Algeria, 24–25 November 2019. [Google Scholar]
- Ghiasi, M.M.; Zendehboudi, S.; Mohsenipour, A.A. Decision tree-based diagnosis of coronary artery disease: CART model. Comput. Meth. Prog. Biomed. 2020, 192, 105400. [Google Scholar] [CrossRef]
- Gao, W.; Wang, J.; Zhou, L.; Luo, Q.; Lao, Y.; Lyu, H.; Guo, S. Prediction of acute kidney injury in ICU with gradient boosting decision tree algorithm. Comput. Biol. Med. 2022, 140, 105097. [Google Scholar] [CrossRef] [PubMed]
- Kuo, F.C.; Cai, D.C.; Liau, B.Y. Foot arch support effect on lumbo-pelvic kinematics and centre of pressure excursion during stand-to-sit transfer in different foot types. J. Med. Biol. Eng. 2020, 40, 169–178. [Google Scholar] [CrossRef]
- Umardani, Y.; Wibowo, D.B.; Caesarendra, W.; Suprihanto, A.; Pranoto, K.A. Calculation of the rearfoot angle representing flatfoot from comparison to the Cavanagh Arch Index. Appl. Sci. 2022, 12, 6764. [Google Scholar] [CrossRef]
- Kim, S.; Suzuki, M.; Minowa, K.; Nittono, H.; Shimizu, T. Efficacy of a tibia counter rotator system for the treatment of internal tibial torsion in children. Children 2022, 9, 970. [Google Scholar] [CrossRef] [PubMed]
- Suits, W.H. Clinical measures of pelvic tilt in physical therapy. Int. J. Sports Phys. Ther. 2021, 16, 1366–1375. [Google Scholar] [CrossRef]
- Ganjehie, S.; Saeedi, H.; Farahmand, B.; Curran, S. The efficiency of gait plate insole for children with in-toeing gait due to femoral anteversion. Prosthet. Ortho Int. 2017, 41, 51–57. [Google Scholar] [CrossRef]
- Ohuchi, H.; Chavez, J.S.; Alvarez, C.A.D. Changes in calcaneal pitch and heel fat pad thickness in static weight bearing radiographs while wearing shoes with arch support and heel cup orthotics. AP-SMART 2019, 17, 21–24. [Google Scholar] [CrossRef]
- Khandakar, A.; Chowdury, M.E.H.; Reaz, M.B.I.; Ali, S.H.M.; Hasan, M.A.; Kiranyaz, S.; Rahman, T.; Alfkey, R.; Bakar, A.A.A.; Malik, R.A. A machine learning model for early detection of diabetic foot using thermogram images. Comput. Biol. Med. 2021, 137, 104838. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, N. Deep learning-based pes planus classification model using transfer learning. JKSCI 2021, 26, 21–28. [Google Scholar]
- McCormack, A.P.; Ching, R.P.; Sangeorzan, B.J. Biomechanics of procedures used in adult flatfoot deformity. Fook Ankle Clin. 2001, 6, 15–23. [Google Scholar] [CrossRef]
- Gould, N.; Morel, M.; Alvarez, R.; Trevino, S.; Fenwick, J.A. Development of the child’s arch. Foot Ankle 1989, 9, 241–245. [Google Scholar] [CrossRef]
- Turner, C.; Gardiner, M.D.; Midgley, A.; Stefanis, A. A guide to the management of paediatric pes planus. Aust. J. Gen. Pract. 2020, 49, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Zafiropoulos, G.; Prasad, K.S.R.K.; Midgley, A.; Kouboura, T.; Danis, G. Flat foot and femoral anteversion in children—A prospective study. Foot 2009, 19, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Redmond, A. The effectiveness of gait plates in controlling in-toeing symptoms in young children. J. Am. Podiatr. Med. Assoc. 2000, 90, 70–76. [Google Scholar] [CrossRef]



| Characteristics | Training Dataset (n = 292) | Test Dataset (n = 126) | |||
| Name | Description | GP (n = 146) | ASOHC (n = 146) | GP (n = 71) | ASOHC (n = 55) |
| Age (year) | Age | 6.52 ± 4.01 | 8.24 ± 3.85 | 6.38 ± 3.31 | 7.41 ± 4.37 |
| HIR (0 or 1) | Hip internal rotation angle (>: abnormal (0), ≤: normal (1)) | 0 (n = 110) 1 (n = 36) | 0 (n = 144) 1 (n = 2) | 0 (n = 55) 1 (n = 16) | 0 (n = 52) 1 (n = 3) |
| TMA-L (degree) | Transmalleolar angle on the left side | −1.93 ± 5.46 | −0.78 ± 2.92 | −2.03 ± 5.12 | −0.22 ± 2.23 |
| IASTJ-L (degree) | Inversion angle of the subtalar joint on the left side | 37.82 ± 7.88 | 38.64 ± 7.02 | 38.09 ± 7.62 | 38.45 ± 8.10 |
| EASTJ-L (degree) | Eversion angle of the subtalar joint on the left side | 16.21 ± 3.91 | 18.29 ± 4.26 | 15.63 ± 3.92 | 17.45 ± 3.51 |
| EASTJ-R (degree) | Eversion angle of the subtalar joint on the right side | 14.49 ± 4.21 | 16.86 ± 4.42 | 14.82 ± 4.55 | 15.95 ± 4.52 |
| FFRF-R (degree) | forefoot to rearfoot angle on the right side | 0.02 ± 0.26 | 0.12 ± 0.58 | 0.07 ± 0.59 | 0.27 ± 0.89 |
| RCSPA-L (degree) | RCSP angle on the left side | −5.08 ± 2.45 | −9.19 ± 3.75 | −5.29 ± 2.95 | −9.30 ± 3.33 |
| RCSPA-R (degree) | RCSP angle on the right side | −4.58 ± 2.00 | −8.12 ± 3.39 | −4.62 ± 2.51 | −8.18 ± 3.38 |
| Rules | |||
|---|---|---|---|
| GP | 1 | RCSPA-L ≤ , Age ≤ 12 years | |
| 2 | RCSPA-L ≤ , Age ≤ 12 years, RCSPA-L ≤ , FFRF-R ≤ | ||
| 3 | RCSPA-L ≤ , HIR = abnormal, RCSPA-R ≤ , EASTJ-L ≤ | ||
| 4 | RCSPA-L ≤ , HIR = abnormal, RCSPA-R ≤ , EASTJ-R ≤ | ||
| 5 | RCSPA-L ≤ , HIR = abnormal, RSCPA-R ≤ , EASTJ-R ≤ , EASTJ-L ≤ | ||
| 6 | RCSPA-L ≤ , Age ≤ 12 years, RCSPA-L ≤ , TMA-L ≤ , IASTJ-L ≤ , EASTJ-L ≤ | ||
| 7 | RCSPA-L ≤ , Age ≤ 12 years, RCSPA-L ≤ , TMA-L ≤ , IASTJ-L ≤ , EASTJ-L ≤ , EASTJ-R ≤ , RCSPA-R ≤ | ||
| ASOHC | 1 | RCSPA-L ≤ , HIR = Normal | |
| 2 | RCSPA-L ≤ , Age ≤ 12 years, RCSPA-L ≤ , TMA-L ≤ | ||
| 3 | RCSPA-L ≤ , Age ≤ 12 years, RCSPA-L ≤ , FFRF-R ≤ | ||
| 4 | RCSPA-L ≤ , HIR = abnormal, RCSPA-R ≤ , EASTJ-L ≤ | ||
| 5 | RCSPA-L ≤ , HIR = abnormal, RCSPA-R ≤ , EASTJ-R ≤ , EASTJ-L ≤ | ||
| 6 | RCSPA-L ≤ , Age ≤ 12 years, RCSPA-L ≤ , TMA-L ≤ , IASTJ-L ≤ | ||
| 7 | RCSPA-L ≤ , Age ≤ 12 years, RCSPA-L ≤ , TMA-L ≤ , IASTJ-L ≤ , EASTJ-L ≤ , EASTJ-R ≤ | ||
| 8 | RCSPA-L ≤ , Age ≤ 12 years, RCSPA-L ≤ , TMA-L ≤ , IASTJ-L ≤ , EASTJ-L ≤ , EASTJ-R ≤ , RCSPA-R ≤ | ||
| Class | Accuracy (%) | Precision (%) | Sensitivity (%) | F1 Score (%) |
|---|---|---|---|---|
| GP | 80.16 | 89.66 | 73.24 | 80.62 |
| ASOHC | 80.16 | 72.06 | 89.09 | 79.67 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, J.-Y.; Yang, C.-M.; Kim, J.-J. Decision Tree-Based Foot Orthosis Prescription for Patients with Pes Planus. Int. J. Environ. Res. Public Health 2022, 19, 12484. https://doi.org/10.3390/ijerph191912484
Jung J-Y, Yang C-M, Kim J-J. Decision Tree-Based Foot Orthosis Prescription for Patients with Pes Planus. International Journal of Environmental Research and Public Health. 2022; 19(19):12484. https://doi.org/10.3390/ijerph191912484
Chicago/Turabian StyleJung, Ji-Yong, Chang-Min Yang, and Jung-Ja Kim. 2022. "Decision Tree-Based Foot Orthosis Prescription for Patients with Pes Planus" International Journal of Environmental Research and Public Health 19, no. 19: 12484. https://doi.org/10.3390/ijerph191912484
APA StyleJung, J.-Y., Yang, C.-M., & Kim, J.-J. (2022). Decision Tree-Based Foot Orthosis Prescription for Patients with Pes Planus. International Journal of Environmental Research and Public Health, 19(19), 12484. https://doi.org/10.3390/ijerph191912484







