The Influence of Stigma Perceptions on Employees’ Claims Experiences for Psychological Injuries: Re-Examination of a Cross-Sectional Survey among Australian Police and Emergency Service Personnel
Abstract
:1. Introduction
2. Method
2.1. Overview
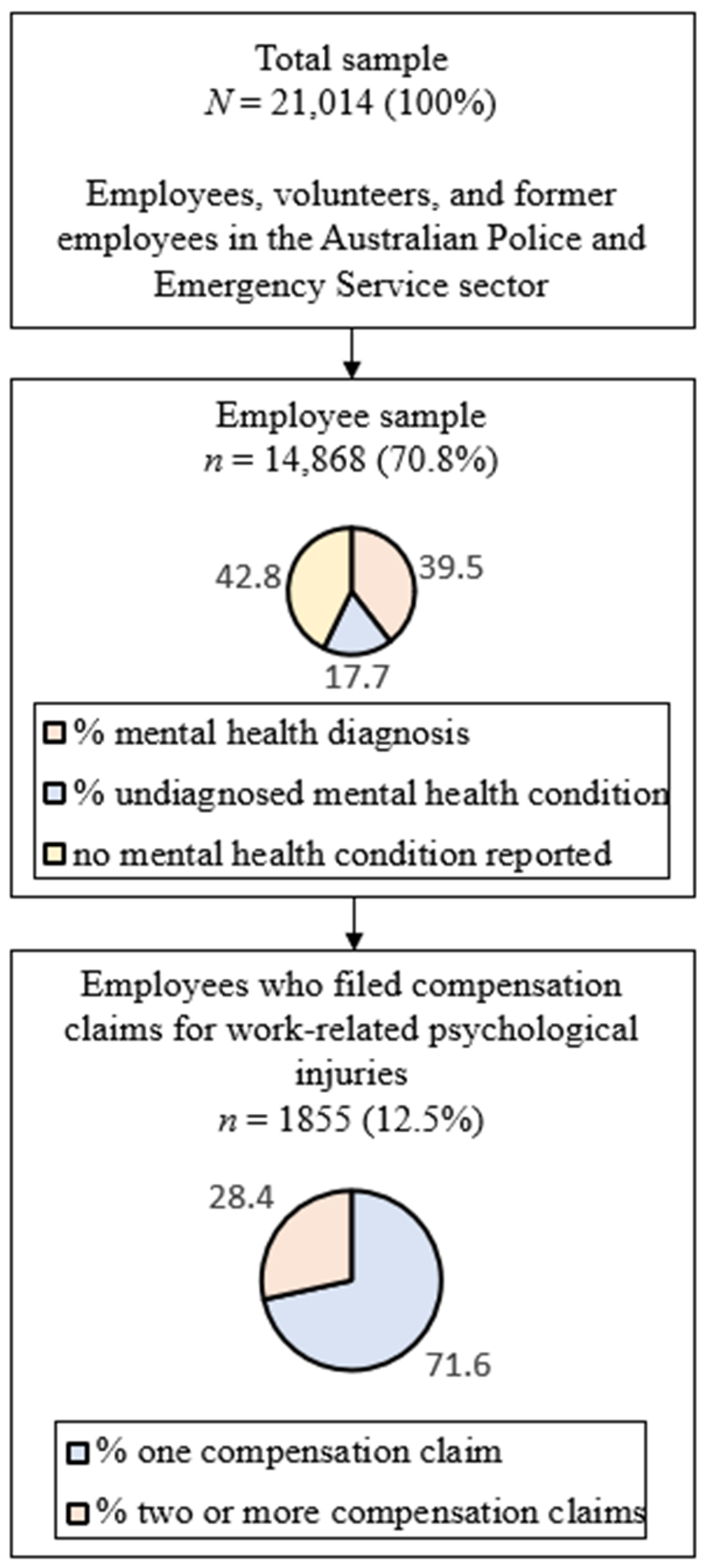
2.2. Participants and Procedures
2.3. Measures
2.3.1. Compensation Claims Experiences
2.3.2. Stigmatising Mental Health Attitudes
2.4. Analysis Plan
3. Results
3.1. Sample Characteristics
3.2. Multiple Regression Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thornicroft, G.; Rose, D.; Kassam, A.; Sartorius, N. Stigma: Ignorance, prejudice or discrimination? Br. J. Psychiatry 2007, 190, 192–193. Available online: https://www.cambridge.org/core/product/identifier/S0007125000171351/type/journal_article (accessed on 15 February 2022). [CrossRef] [PubMed]
- Link, B.G.; Phelan, J.C. Conceptualizing stigma. Annu. Rev. Sociol. 2001, 27, 363–385. Available online: https://www.annualreviews.or (accessed on 7 April 2022). [CrossRef]
- Corrigan, P.W.; Watson, A.C. Understanding the impact of stigma on people with mental illness. World Psychiatry 2002, 1, 16–20. Available online: http://www.ncbi.nlm.nih.gov/pubmed/16946807article (accessed on 17 February 2022).
- Brouwers, E.P.M. Social stigma is an underestimated contributing factor to unemployment in people with mental illness or mental health issues: Position paper and future directions. BMC Psychol. 2020, 8, 36. Available online: https://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-020-00399-0 (accessed on 15 February 2022). [CrossRef] [PubMed]
- Knaak, S.; Mantler, E.; Szeto, A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthc. Manag. Forum. 2017, 30, 111–116. Available online: http://journals.sagepub.co (accessed on 7 April 2022).
- Busby Grant, J.; Bruce, C.P.; Batterham, P.J. Predictors of personal, perceived and self-stigma towards anxiety and depression. Epidemiol. Psychiatr. Sci. 2016, 25, 247–254. Available online: https://www.cambridge.org/core/product/identifier/S2045796015000220/type/journal_article (accessed on 22 February 2022). [CrossRef]
- Beyond Blue Ltd. Beyond Blue Information Paper: Stigma and Discrimination Associated with Depression and Anxiety. 2015. Available online: https://www.beyondblue.org.au/docs/default-source/about-beyond-blue/policy-submissions/stigma-and-discrimination-associated-with-depression-and-anxiety.pdf?sfvrsn=92367eea_4 (accessed on 15 February 2022).
- Yanos, P.T.; DeLuca, J.S.; Roe, D.; Lysaker, P.H. The impact of illness identity on recovery from severe mental illness: A review of the evidence. Psychiatry Res. 2020, 288, 112950. [Google Scholar] [CrossRef]
- Clement, S.; Schauman, O.; Graham, T.; Maggioni, F.; Evans-Lacko, S.; Bezborodovs, N.; Morgan, C.; Rüsch, N.; Brown, J.S.; Thornicroft, G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 2015, 45, 11–27. [Google Scholar] [CrossRef]
- Schnyder, N.; Panczak, R.; Groth, N.; Schultze-Lutter, F. Association between mental health-related stigma and active help-seeking: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 261–268. [Google Scholar] [CrossRef]
- Oexle, N.; Müller, M.; Kawohl, W.; Xu, Z.; Viering, S.; Wyss, C.; Vetter, S.; Rüsch, N. Self-stigma as a barrier to recovery: A longitudinal study. Eur. Arch. Psychiatry Clin. Neurosci. 2018, 268, 209–212. [Google Scholar] [CrossRef]
- Jones, S. Describing the Mental Health Profile of First Responders: A Systematic Review. J. Am. Psychiatr. Nurses Assoc. 2017, 23, 200–214. [Google Scholar] [CrossRef]
- Gray, S.E.; Collie, A. The nature and burden of occupational injury among first responder occupations: A retrospective cohort study in Australian workers. Injury 2017, 48, 2470–2477. [Google Scholar] [CrossRef]
- Kyron, M.J.; Rikkers, W.; LaMontagne, A.; Bartlett, J.; Lawrence, D. Work-Related and Nonwork Stressors, PTSD, and Psychological Distress: Prevalence and Attributable Burden Among Australian Police and Emergency Services Employees. Psychol. Trauma Theory Res. Pract. Policy 2019, 14, 1124–1133. [Google Scholar] [CrossRef]
- Soomro, S.; Yanos, P.T. Predictors of Mental Health Stigma among Police Officers: The Role of Trauma and PTSD. J. Police Crim. Psychol. 2019, 34, 175–183. Available online: http://link.springer.com/10.1007/s11896-018-9285-x (accessed on 22 February 2022). [CrossRef]
- Morgan, A.J.; Reavley, N.J.; Ross, A.; Too, L.S.; Jorm, A.F. Interventions to reduce stigma towards people with severe mental illness: Systematic review and meta-analysis. J. Psychiatry Res. 2018, 103, 120–133. [Google Scholar] [CrossRef]
- Productivity Commission. National Workers’ Compensation and Occupational Health and Safety Frameworks, Report No. 27, Canberra, March 2004. Available online: https://www.pc.gov.au/inquiries/completed/workers-compensation/report/workerscomp.pdf (accessed on 22 February 2022).
- Kyron, M.J.; Rikkers, W.; O’Brien, P.; Bartlett, J.; Lawrence, D. Experiences of Police and Emergency Services Employees with Workers’ Compensation Claims for Mental Health Issues. J. Occup. Rehabil. 2021, 31, 197–206. Available online: https://link.springer.com/10.1007/s10926-020-09909-8 (accessed on 15 February 2022). [CrossRef]
- Collie, A.; Sheehan, L.; Lane, T.J.; Gray, S.; Grant, G. Injured worker experiences of insurance claim processes and return to work: A national, cross-sectional study. BMC Public Health. BMC Public Health 2019, 19, 927. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-7251-x (accessed on 17 February 2022). [CrossRef]
- Lawrence, D.; Kyron, M.; Rikkers, W.; Bartlett, J.; Hafekost, K.; Goodsell, B.; Cunneen, R. Answering the Call: National Survey of the Mental Health and Wellbeing of Police and Emergency Services-Detailed Report; Graduate School of Education, The University of Western Australia: Perth, Australia, 2018; Available online: https://api.research-repository.uwa.edu.au/ws/portalfiles/portal/36106043/Answering_the_Call.pdf (accessed on 15 February 2022).
- Answering the Call National Survey, Beyond Blue’s National Mental Health and Wellbeing Study of Police and Emergency Services-Final Report. Beyond Blue Ltd.: Hawthorn, CA, USA, 2018. Available online: https://www.beyondblue.org.au/docs/default-source/resources/bl1898-pes-full-report_final (accessed on 15 February 2022).
- Good Practice Framework for Mental Health and Wellbeing in Police and Emergency Services Organisations. Beyond Blue Ltd. 2016. Available online: https://www.afac.com.au/insight/health/articles/current/good-practice-framework-for-mental-health-and-wellbeing-for-first-responder-organisations (accessed on 7 April 2022).
- Griffiths, K.M.; Christensen, H.; Jorm, A.F.; Evans, K.; Groves, C. Effect of web-based depression literacy and cognitive-behavioural therapy interventions on stigmatising attitudes to depression: Randomised controlled trial. Br. J. Psychiatry 2004, 185, 342–349. Available online: https://www.cambridge.org/core/product/identifier/S0007125000165547/type/journal_article (accessed on 7 April 2022). [CrossRef]
- Erdfelder, E.; Faul, F.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. Available online: http://link.springer.com/10.3758/BRM.41.4.1149 (accessed on 7 April 2022).
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed; Allyn and Bacon: New York, NY, USA, 2007. [Google Scholar]
- Johnston, R.; Jones, K.; Manley, D. Confounding and collinearity in regression analysis: A cautionary tale and an alternative procedure, illustrated by studies of British voting behaviour. Qual. Quant. 2018, 52, 1957–1976. Available online: http://link.springer.com/10.1007/s11135-017-0584-6 (accessed on 31 August 2022). [CrossRef]
- Stoffel, M.A.; Nakagawa, S.; Schielzeth, H. partR2: Partitioning R2 in generalized linear mixed models. PeerJ 2021, 9, e11414. Available online: https://peerj.com/articles/11414 (accessed on 4 August 2022). [CrossRef]
- Chan, K.K.S.; Mak, W.W.S. The content and process of self-stigma in people with mental illness. Am. J. Orthopsychiatry 2017, 87, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Lasalvia, A.; Zoppei, S.; van Bortel, T.; Bonetto, C.; Cristofalo, D.; Wahlbeck, K.; Bacle, S.V.; Van Audenhove, C.; Van Weeghel, J.; Reneses, B.; et al. Global pattern of experienced and anticipated discrimination reported by people with major depressive disorder: A cross-sectional survey. Lancet 2013, 381, 55–62. [Google Scholar] [CrossRef]
- Mckenzie, D. The Impact of Mediation on Workplace Relationship Conflict and Return to Work Outcomes: A Snapshot Review. 2012. Available online: http://www.iscrr.com.au/__data/assets/pdf_file/0010/297757/Mediation-Interventions-and-RTW_Full-Report_0512.pdf (accessed on 22 August 2022).
- White, C.; Green, R.A.; Ferguson, S.; Anderson, S.L.; Howe, C.; Sun, J.; Buys, N. The Influence of Social Support and Social Integration Factors on Return to Work Outcomes for Individuals with Work-Related Injuries: A Systematic Review. J. Occup. Rehabil. 2019, 29, 636–659. [Google Scholar] [CrossRef] [PubMed]
- Al-Shurafat, M.S.; Binti Abdul Halim, D.; Co-Supervisor, H.; Zainudin Awang, S. A Review of Organisational Culture and Organizational Commitment. IOSR J. Bus. Manag. 2018, 20, 21–26. Available online: www.iosrjournals.org (accessed on 14 April 2022).
- Behavioural Economics Team of the Australian Government. Returning to Work after Illness or Injury; Commonwealth of Australia, Department of the Prime Minister and Cabinet: Barton, Australia, 2020. Available online: https://behaviouraleconomics.pmc.gov.au/sites/default/files/projects/return-work-report-2.pdf (accessed on 11 April 2022).
- Vaa Stelling, B.E.; West, C.P. Faculty Disclosure of Personal Mental Health History and Resident Physician Perceptions of Stigma Surrounding Mental Illness. Acad. Med. 2021, 96, 682–685. Available online: https://journals.lww.com/10.1097/ACM.0000000000003941 (accessed on 11 April 2022). [CrossRef]
- Rao, D.; Elshafei, A.; Nguyen, M.; Hatzenbuehler, M.L.; Frey, S.; Go, V.F. A systematic review of multi-level stigma interventions: State of the science and future directions. BMC Med. 2019, 17, 41. Available online: https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-018-1244-y (accessed on 15 February 2022). [CrossRef]
- Barnes, C.M.; Dang, C.T.; Leavitt, K.; Guarana, C.L.; Uhlmann, E.L. Archival Data in Micro-Organizational Research: A Toolkit for Moving to a Broader Set of Topics. J. Manag. 2018, 44, 1453–1478. Available online: http://journals.sagepub.co (accessed on 7 April 2022).
| Employees Who Did Not Indicate Previous Claim (N = 13,013) | Employees with Claim History (1 or More) (N = 1855) | ||||||
|---|---|---|---|---|---|---|---|
| Variable | M/n | SD/% | M/n | SD/% | F/χ2 | p | w/g |
| Age group (years, n, %) | 196.16 | <0.001 | 0.81 | ||||
| <35 | 2883 | 22.2 | 176 | 9.5 | - | - | - |
| 35–44 | 3590 | 27.6 | 475 | 25.6 | - | - | - |
| 45–54 | 4369 | 33.6 | 795 | 42.9 | - | - | - |
| ≥55 | 2171 | 16.7 | 409 | 22.0 | - | - | - |
| Gender (n, %) | 34.14 | <0.001 | 0.58 | ||||
| Female | 5294 | 40.7 | 623 | 33.6 | - | - | - |
| Male | 7719 | 59.3 | 1232 | 66.4 | - | - | - |
| Sector (n, %) | 100.99 | <0.001 | 0.58 | ||||
| Ambulance | 3050 | 23.4 | 423 | 22.8 | - | - | - |
| Fire and Rescue | 2745 | 21.1 | 230 | 12.4 | - | - | - |
| Police | 6911 | 53.1 | 1177 | 63.5 | - | - | - |
| State Emergency Services | 307 | 2.4 | 25 | 1.3 | - | - | - |
| Mental Health History (n, %) | |||||||
| Previous diagnosis | 4496 | 34.6 | 1369 | 73.8 | 338.96 | <0.001 | 1.84 |
| Condition currently present | 2412 | 18.5 | 941 | 50.7 | 103.80 | <0.001 | 0.72 |
| Ever taken work stress leave | 3593 | 27.6 | 1410 | 76.0 | 1703.48 | <0.001 | 4.13 |
| Self-stigma ◌ | |||||||
| Shame | 0.27 | 1.05 | 0.29 | 1.07 | 0.32 | 0.571 | 0.02 |
| Burden | 0.01 | 1.08 | 0.24 | 1.08 | 50.78 | <0.001 | 0.21 |
| Experiences with others | −0.58 | 1.07 | −0.25 | 1.12 | 106.54 | <0.001 | 0.31 |
| Personal Stigma | |||||||
| Ignorance | −1.26 | 0.67 | −1.36 | 0.67 | 32.30 | <0.001 | 0.14 |
| Perceived burden | −0.81 | 0.84 | −0.88 | 0.88 | 12.58 | <0.001 | 0.09 |
| Workplace Stigma | |||||||
| Perceived stigma | 0.25 | 0.79 | 0.54 | 0.82 | 223.23 | <0.001 | 0.37 |
| Structural stigma | −1.39 | 0.88 | −1.46 | 0.91 | 10.74 | 0.001 | 0.08 |
| Organisational commitment | 0.24 | 0.73 | −0.06 | 0.80 | 278.80 | <0.001 | 0.41 |
| Employees with a Mental Health Condition (N = 4496) | Employees with Claim History (1 or More) (N = 1855) | ||||||
|---|---|---|---|---|---|---|---|
| Variable | M/n | SD/% | M/n | SD/% | F/χ2 | p | w/g |
| Age group (years, n, %) | 140.40 | <0.001 | 0.68 | ||||
| <35 | 894 | 19.9 | 176 | 9.5 | - | - | - |
| 35–44 | 1308 | 29.1 | 475 | 25.6 | - | - | - |
| 45–54 | 1592 | 35.4 | 795 | 42.9 | - | - | - |
| ≥55 | 702 | 15.6 | 409 | 22.0 | - | - | - |
| Gender (n, %) | 121.40 | <0.001 | 1.10 | ||||
| Female | 2189 | 48.7 | 623 | 33.6 | - | - | - |
| Male | 2307 | 51.3 | 1232 | 66.4 | - | - | - |
| Sector (n, %) | 99.42 | <0.001 | 0.58 | ||||
| Ambulance | 1073 | 23.9 | 423 | 22.8 | - | - | - |
| Fire and Rescue | 958 | 21.3 | 230 | 12.4 | - | - | - |
| Police | 2338 | 52.0 | 1177 | 63.5 | - | - | - |
| State Emergency Services | 127 | 2.8 | 25 | 1.3 | - | - | - |
| Mental Health History (n, %) | |||||||
| Previous diagnosis | 4496 | 100 | 1369 | 73.8 | 527.54 | <0.001 | 2.30 |
| Condition currently present | 2412 | 53.6 | 941 | 50.7 | 97.58 | <0.001 | 0.99 |
| Ever taken work stress leave | 2132 | 47.4 | 1410 | 76.0 | 435.18 | <0.001 | 2.09 |
| Self-stigma ◌ | |||||||
| Shame | 0.19 | 1.05 | 0.29 | 1.07 | 9.19 | 0.002 | 0.09 |
| Burden | 0.04 | 1.08 | 0.24 | 1.08 | 40.12 | <0.001 | 0.19 |
| Experiences with others | −0.51 | 1.07 | −0.25 | 1.12 | 64.85 | <0.001 | 0.25 |
| Personal Stigma | |||||||
| Ignorance | −1.43 | 0.62 | −1.36 | 0.67 | 15.20 | <0.001 | 0.11 |
| Perceived burden | −1.01 | 0.82 | −0.88 | 0.88 | 29.88 | <0.001 | 0.15 |
| Workplace Stigma | |||||||
| Perceived stigma | 0.36 | 0.80 | 0.54 | 0.82 | 68.33 | <0.001 | 0.23 |
| Structural stigma | −1.46 | 0.88 | −1.46 | 0.91 | 0.02 | 0.881 | 0.00 |
| Organisational commitment | 0.14 | 0.75 | −0.06 | 0.80 | 88.18 | <0.001 | 0.26 |
| Model | b | SE-b | Beta | Pearson r | sr | rs2 | p |
|---|---|---|---|---|---|---|---|
| Constant | 3.07 | 0.09 | |||||
| Self-stigma—shame | −0.01 | 0.04 | −0.01 | 0.16 | −0.01 | 0.15 | 0.802 |
| Self-stigma—burden | 0.08 | 0.04 | 0.06 | 0.23 | 0.05 | 0.30 | 0.063 |
| Self-stigma—experiences with others ** | 0.12 | 0.04 | 0.10 | 00.28 | 0.08 | 0.45 | 0.002 |
| Personal Stigma—ignorance | −0.10 | 0.06 | −0.05 | −0.08 | −0.04 | 0.03 | 0.130 |
| Personal Stigma—perceived burden | −0.08 | 0.04 | −0.06 | −0.04 | −0.05 | 0.01 | 0.065 |
| Workplace Stigma—perceived stigma *** | 0.20 | 0.05 | 0.13 | 0.29 | 0.12 | 0.48 | <0.001 |
| Workplace Stigma—structural stigma | −0.05 | 0.04 | −0.03 | −0.09 | −0.04 | 0.04 | 0.181 |
| Organisational Commitment *** | −0.40 | 0.05 | −0.25 | −0.36 | −0.23 | 0.73 | <0.001 |
| Model | b | SE-b | Beta | Pearson r | sr | rs2 | p |
|---|---|---|---|---|---|---|---|
| Constant | 3.41 | 0.09 | |||||
| Self-stigma—shame | 0.02 | 0.04 | 0.02 | 0.17 | 0.02 | 0.17 | 0.523 |
| Self-stigma—burden | 0.05 | 0.04 | 0.04 | 0.22 | 0.03 | 0.26 | 0.226 |
| Self-stigma—experiences with others ** | 0.10 | 0.04 | 0.09 | 0.26 | 0.07 | 0.39 | 0.008 |
| Personal Stigma—ignorance * | −0.14 | 0.06 | −0.07 | −0.08 | −0.06 | 0.03 | 0.022 |
| Personal Stigma—perceived burden | −0.03 | 0.04 | −0.02 | −0.01 | −0.02 | 0.01 | 0.529 |
| Workplace Stigma—perceived stigma ** | 0.13 | 0.05 | 0.08 | 0.27 | 0.08 | 0.40 | 0.005 |
| Workplace Stigma—structural stigma | −0.04 | 0.04 | −0.02 | −0.08 | −0.03 | 0.03 | 0.333 |
| Organisational Commitment *** | −0.47 | 0.04 | −0.30 | −0.39 | −0.27 | 0.83 | <0.001 |
| Model | b | SE-b | Beta | Pearson r | sr | rs2 | p |
|---|---|---|---|---|---|---|---|
| Constant | 1.94 | 0.05 | |||||
| Self-stigma—shame | 0.01 | 0.02 | 0.02 | −0.14 | 0.01 | 0.10 | 0.619 |
| Self-stigma—burden | 0.01 | 0.02 | 0.01 | −0.17 | 0.01 | 0.14 | 0.673 |
| Self-stigma—experiences with others ** | −0.07 | 0.02 | −0.10 | −0.25 | −0.08 | 0.32 | 0.002 |
| Personal Stigma—ignorance | 0.04 | 0.04 | 0.03 | 0.02 | 0.03 | 0.00 | 0.294 |
| Personal Stigma—perceived burden | −0.01 | 0.03 | −0.01 | −0.04 | −0.01 | 0.01 | 0.816 |
| Workplace Stigma—perceived stigma | −0.04 | 0.03 | −0.04 | −0.25 | −0.04 | 0.30 | 0.151 |
| Workplace Stigma—structural stigma | −0.02 | 0.02 | −0.02 | 0.03 | −0.02 | 0.00 | 0.430 |
| Organisational Commitment *** | 0.36 | 0.03 | 0.39 | 0.43 | 0.35 | 0.95 | <0.001 |
| Model | b | SE-b | Beta | Pearson r | sr | rs2 | p |
|---|---|---|---|---|---|---|---|
| Constant | 2.20 | 0.08 | |||||
| Self-stigma—shame | −0.00 | 0.03 | −0.00 | −0.14 | −0.00 | 0.12 | 0.974 |
| Self-stigma—burden | −0.00 | 0.03 | −0.00 | −0.17 | −0.00 | 0.16 | 0.980 |
| Self-stigma—experiences with others * | −0.08 | 0.03 | −0.08 | −0.24 | −0.07 | 0.31 | 0.014 |
| Personal Stigma—ignorance | 0.08 | 0.05 | 0.04 | 0.02 | 0.04 | 0.00 | 0.166 |
| Personal Stigma—perceived burden | −0.05 | 0.04 | −0.04 | −0.05 | −0.03 | 0.01 | 0.206 |
| Workplace Stigma—perceived stigma | −0.03 | 0.04 | −0.02 | −0.22 | −0.02 | 0.28 | 0.413 |
| Workplace Stigma—structural stigma | 0.04 | 0.03 | 0.03 | 0.07 | 0.03 | 0.03 | 0.249 |
| Organisational Commitment *** | 0.51 | 0.04 | 0.36 | 0.41 | 0.33 | 0.94 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanatkar, S.; Bartlett, J.; Harvey, S.; Counson, I.; Lawrence, D. The Influence of Stigma Perceptions on Employees’ Claims Experiences for Psychological Injuries: Re-Examination of a Cross-Sectional Survey among Australian Police and Emergency Service Personnel. Int. J. Environ. Res. Public Health 2022, 19, 12438. https://doi.org/10.3390/ijerph191912438
Sanatkar S, Bartlett J, Harvey S, Counson I, Lawrence D. The Influence of Stigma Perceptions on Employees’ Claims Experiences for Psychological Injuries: Re-Examination of a Cross-Sectional Survey among Australian Police and Emergency Service Personnel. International Journal of Environmental Research and Public Health. 2022; 19(19):12438. https://doi.org/10.3390/ijerph191912438
Chicago/Turabian StyleSanatkar, Samineh, Jenn Bartlett, Samuel Harvey, Isabelle Counson, and David Lawrence. 2022. "The Influence of Stigma Perceptions on Employees’ Claims Experiences for Psychological Injuries: Re-Examination of a Cross-Sectional Survey among Australian Police and Emergency Service Personnel" International Journal of Environmental Research and Public Health 19, no. 19: 12438. https://doi.org/10.3390/ijerph191912438
APA StyleSanatkar, S., Bartlett, J., Harvey, S., Counson, I., & Lawrence, D. (2022). The Influence of Stigma Perceptions on Employees’ Claims Experiences for Psychological Injuries: Re-Examination of a Cross-Sectional Survey among Australian Police and Emergency Service Personnel. International Journal of Environmental Research and Public Health, 19(19), 12438. https://doi.org/10.3390/ijerph191912438






