Study on the Development of a Conceptual Framework to Identify the Risk Factors of Diabetic Retinopathy among Diabetic Patients: A Concept Paper
Abstract
:1. Introduction
2. Literature Review
- Background information on DR;
- Statistics and blindness related to DR;
- The risk factors of DR.
2.1. Background Information on DR
2.2. Prevalence of DR
2.3. The Risk Factor
3. Research Gap
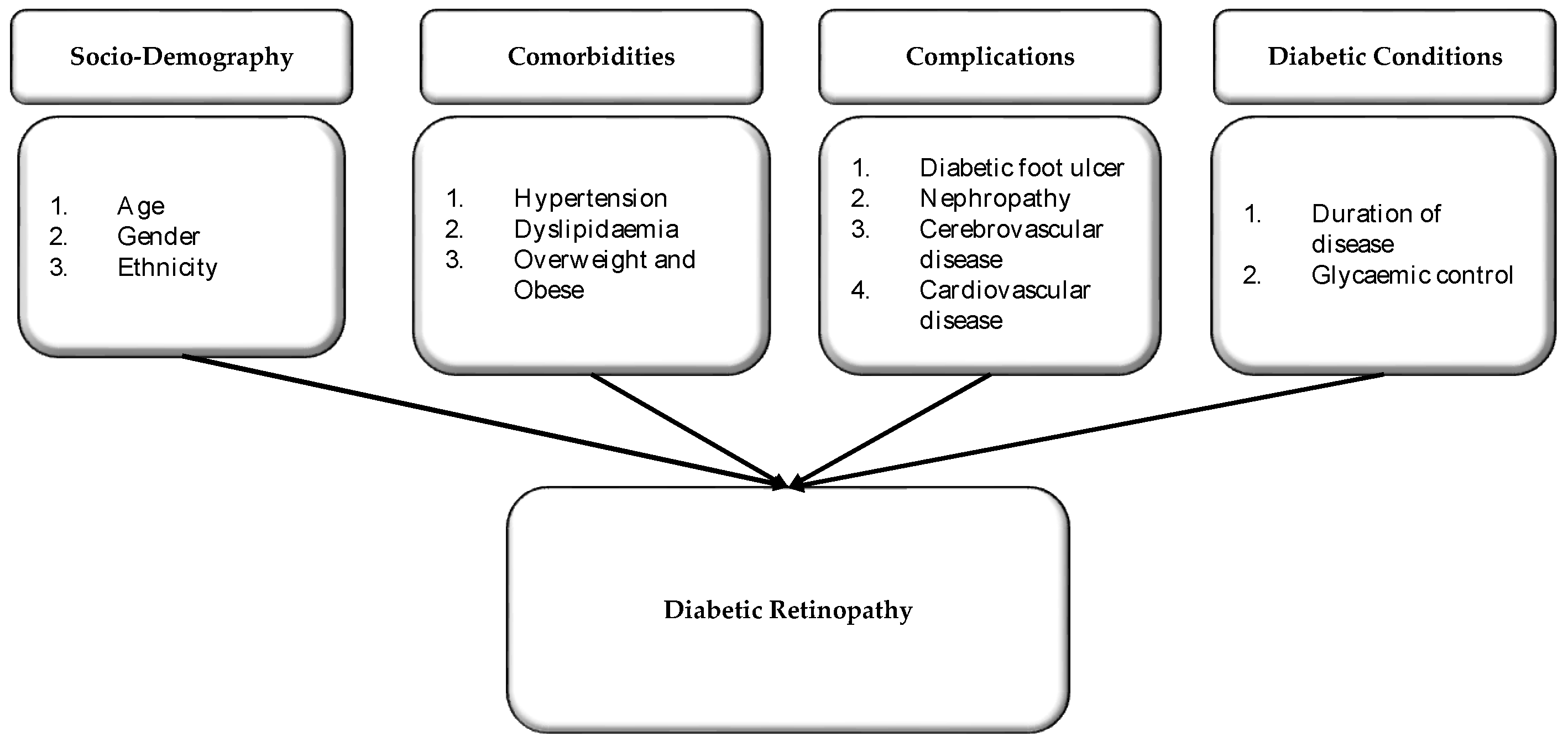
4. Suggested Conceptual Framework
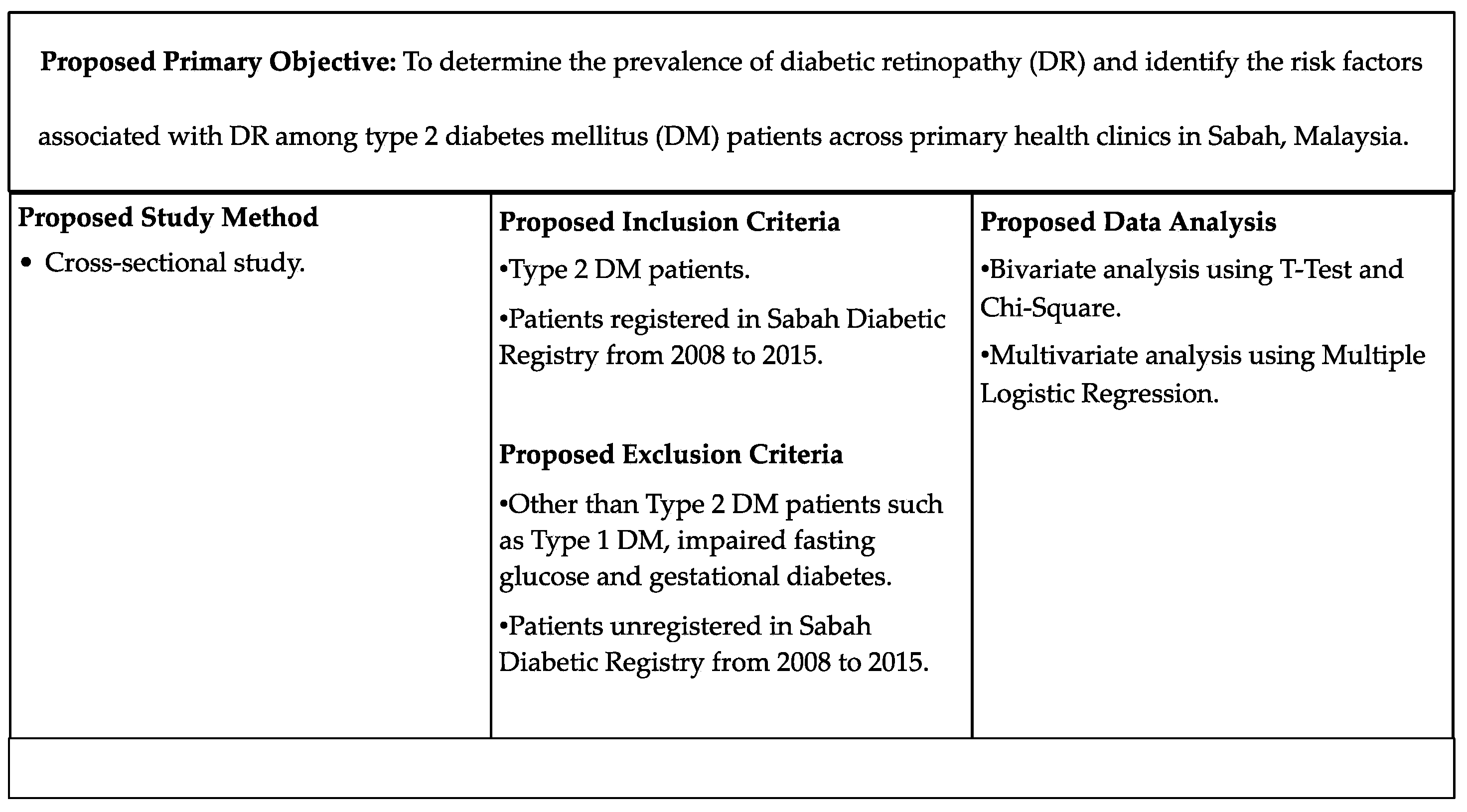
5. Proposed Study Framework According to the Proposed Conceptual Framework
- To identify the sociodemographic characteristics, comorbidities, and complications of T2DM patients in primary health clinics in Sabah;
- To identify the associated factors of DR among T2DM in Sabah primary health clinics;
- To determine the association between DR and sociodemographic data, such as age and gender;
- To determine the association between DR and comorbidities such as hypertension, dyslipidaemia, and high body mass index;
- To determine the association between DR and other diabetes complications such as nephropathy, foot ulcer, and cerebrovascular and cardiovascular disease;
- To determine the association between DR and above normal HBA1C level.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lin, X.; Xu, Y.; Pan, X.; Xu, J.; Ding, Y.; Sun, X.; Song, X.; Ren, Y.; Shan, P.F. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci. Rep. 2020, 10, 14790. [Google Scholar] [CrossRef] [PubMed]
- Cade, W.T. Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys. Ther. 2008, 11, 1322–1335. [Google Scholar] [CrossRef] [PubMed]
- Chawla, A.; Chawla, R.; Jaggi, S. Microvasular and macrovascular complications in diabetes mellitus: Distinct or continuum? Indian J. Endocrinol. Metab. 2016, 20, 546. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4911847/ (accessed on 15 January 2021). [CrossRef] [PubMed]
- Garofolo, M.; Gualdani, E.; Giannarelli, R.; Aragona, M.; Campi, F.; Lucchesi, D.; Daniele, G.; Miccoli, R.; Francesconi, P.; Del Prato, S.; et al. Microvascular complications burden (nephropathy, retinopathy and peripheral polyneuropathy) affects risk of major vascular events and all-cause mortality in type 1 diabetes: A 10-year follow-up study. Cardiovasc. Diabetol. 2019, 18, 159. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Wong, T.Y.; Sabanayagam, C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis. 2015, 2, 17. [Google Scholar] [CrossRef]
- World Health Organization. Vision 2020 The Right to Sight. WHO Library Cataloguing. 2006. Available online: https://www.who.int/blindness/Vision2020_report.pdf (accessed on 23 January 2021).
- Diwan, V.; Purohit, M.; Chandran, S.; Parashar, V.; Shah, H.; Mahadik, V.K.; Stålsby Lundborg, C.; Tamhankar, A.J. A Three-Year Follow-Up Study of Antibiotic and Metal Residues, Antibiotic Resistance and Resistance Genes, Focusing on Kshipra—A River Associated with Holy Religious Mass-Bathing in India: Protocol Paper. Int. J. Environ. Res. Public Health 2017, 14, 574. [Google Scholar] [CrossRef]
- Cuevas-Lara, C.; Izquierdo, M.; Zambom-Ferraresi, F.; de Asteasu, M.L.S.; Marín-Epelde, I.; Chenhuichen, C.; Zambom-Ferraresi, F.; Ramírez-Vélez, R.; García-Hermoso, A.; Casas-Herrero, Á.; et al. A Feasibility Study for Implementation "Health Arcade": A Study Protocol for Prototype of Multidomain Intervention Based on Gamification Technologies in Acutely Hospitalized Older Patients. Int. J. Environ. Res. Public Health 2020, 17, 8058. [Google Scholar] [CrossRef]
- Allegri, M.D.; Srivastava, S.; Strupat, C.; Brenner, S.; Parmar, D.; Parisi, D.; Walsh, C.; Mahajan, S.; Neogi, R.; Ziegler, S.; et al. Mixed and Multi-Methods Protocol to Evaluate Implementation Processes and Early Effects of the Pradhan Mantri Jan Arogya Yojana Scheme in Seven Indian States. Int. J. Environ. Res. Public Health 2020, 17, 7812. [Google Scholar] [CrossRef]
- Marfil-Gómez, R.; Morales-Puerto, M.; León-Campos, Á.; Morales-Asencio, J.M.; Morilla-Herrera, J.C.; Timonet-Andreu, E.; Cuevas-Fernández Gallego, M.; Martí-García, C.; López-Leiva, I.; García-Mayor, S. Quality of Life, Physical and Mental Health of Family Caregivers of Dependent People with Complex Chronic Disease: Protocol of a Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 7489. [Google Scholar] [CrossRef]
- Phulkerd, S.; Rachmi, C.N.; Sameeha, M.J.; Borazon, E.Q.; Thow, A.-M.; Trevena, H.; Saptari, A.F.; Cheah, Y.K.; Wel, C.A.C.; Marquez, V.T.; et al. Identifying Opportunities for Strategic Policy Design to Address the Double Burden of Malnutrition through Healthier Retail Food: Protocol for South East Asia Obesogenic Food Environment (SEAOFE) Study. Int. J. Environ. Res. Public Health 2022, 19, 528. [Google Scholar] [CrossRef]
- Dew, A. Protocol Paper: Conducting Life History Interviews to Explore the Journeys of People with Disability from Syrian and Iraqi Refugee Backgrounds Settling in Australia. Int. J. Environ. Res. Public Health 2021, 18, 7978. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Lo, A.C.Y. Diabetic retinopathy: Pathophysiology and treatments. Int. J. Mol. Sci. 2018, 9, 1816. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Reddy, N.; Kishan, R. Diabetic eye screening in multi-ethnic population of Malaysia: Epidemiological risk factors for the development of diabetic retinopathy. Int. J. Res. Med. Sci. 2014, 2, 1045. [Google Scholar]
- Solomon, S.D.; Chew, E.; Duh, E.J.; Sobrin, L.; Sun, J.K.; VanderBeek, B.L.; Wykoff, C.C.; Gardner, T.W. Diabetic retinopathy: A position statement by the American Diabetes Association. Diabetes Care 2017, 40, 412–418. [Google Scholar] [CrossRef]
- Yau, J.W.Y.; Rogers, S.L.; Kawasaki, R.; Lamoureux, E.L.; Kowalski, J.W.; Bek, T.; Chen, S.-J.; Dekker, J.M.; Fletcher, A.; Grauslund, J.; et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 2012, 35, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Teo, Z.L.; Tham, Y.C.; Yu, M.; Chee, M.L.; Rim, T.H.; Cheung, N.; Bikbov, M.M.; Wang, Y.X.; Tang, Y.; Lu, Y.; et al. Global Prevalence of Diabetic Retinopathy and Projection of Burden through 2045: Systematic Review and Meta-analysis. Ophthalmology 2021, 128, 1580–1591. [Google Scholar] [CrossRef]
- Cohen, S.R.; Gardner, T.W. Diabetic Retinopathy and Diabetic Macular Edema. Dev. Ophthalmol. 2016, 55, 137–146. [Google Scholar] [CrossRef]
- Shah, A. Prevalence of DR in the United States, 2011–2014. Value Health 2016, 19, A199. [Google Scholar] [CrossRef]
- Narsaiah, C.; Manoj, P.; Raju, A.G. Study on Awareness and Assessment of Diabetic Retinopathy in Diabetic Patients Attending Ophthalmology Clinic at a Tertiary Care Hospital, Telangana State. Int. J. Contemp. Med. 2019, 6, 9–13. [Google Scholar] [CrossRef]
- Sultan, S.; Fawwad, A.; Siyal, N.A.; Butt, A.; Khokar, A.R.; Basit, A. Frequency and risk factors of diabetic retinopathy in patients with type 2 diabetes presenting at a tertiary care hospital. Int. J. Diabetes Dev. Ctries 2020, 40, 87–92. [Google Scholar] [CrossRef]
- Cui, Y.; Zhang, M.; Zhang, L.; Zhang, L.; Kuang, J.; Zhang, G.; Liu, Q.; Guo, H.; Meng, Q. Prevalence and risk factors for diabetic retinopathy in a cross-sectional population-based study from rural southern China: Dongguan Eye Study. BMJ Open 2019, 9, e023586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, G.S.; Gan, A.; Sabanayagam, C.; Tham, Y.C.; Neelam, K.; Mitchell, P.; Wang, J.J.; Lamoureux, E.L.; Cheng, C.-Y.; Wong, T.Y.; et al. Ethnic Differences in the Prevalence and Risk Factors of Diabetic Retinopathy: The Singapore Epidemiology of Eye Diseases Study. Ophthalmology 2018, 125, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.Y.; Cheung, N.; Tay, W.T.; Wang, J.J.; Aung, T.; Saw, S.M.; Lim, S.C.; Tai, E.S.; Mitchell, P. Prevalence and risk factors for diabetic retinopathy. The Singapore Malay Eye Study. Ophthalmology 2008, 115, 1869–1875. [Google Scholar] [CrossRef] [PubMed]
- Mohd Aznan, M.A.; Khairidzan, M.K.; Razman, M.R.; Fa’iza, A. Prevalence of Diabetic Retinopathy and Its Associated Factors Among Diabetic Patients in Primary Care Clinics, Kuantan, Pahang. IIUM Med. J. Malay. 2020, 17. [Google Scholar] [CrossRef]
- López, M.; Cos, F.X.; Álvarez-Guisasola, F.; Fuster, E. Prevalence of diabetic retinopathy and its relationship with glomerular filtration rate and other risk factors in patients with type 2 diabetes mellitus in Spain. DM2 HOPE study. J. Clin. Transl. Endocrinol. 2017, 9, 61–65. [Google Scholar] [CrossRef]
- Chang, L.Y.; Lee, A.C.; Sue, W. Prevalence of diabetic retinopathy at first presentation to the retinal screening service in the greater Wellington region of New Zealand 2006–2015, and implications for models of retinal screening. N. Z. Med. J. 2017, 130, 78–88. [Google Scholar]
- Alharthi, A.S.; Almutairi, M.Z.K.; Alswat, A.H.K. Prevalence and Potential Risk Factors of Diabetic Retinopathy among Type 2 Diabetics Patients in Diabetic Center, Taif City. Egypt. J. Hosp. Med. 2018, 70, 455–1463. [Google Scholar] [CrossRef]
- Kohner, E.M.; Aldington, S.J.; Stratton, I.M.; Manley, S.E.; Holman, R.R.; Matthews, D.R.; Turner, R.C. United Kingdom Prospective Diabetes Study, 30: Diabetic Retinopathy at Diagnosis of Non–Insulin-Dependent Diabetes Mellitus and Associated Risk Factors. Arch. Ophthalmol. 1998, 116, 297–303. [Google Scholar] [CrossRef]
- Namperumalsamy, P.; Kim, R.; Vignesh, T.P.; Nithya, N.; Royes, J.; Gijo, T.; Thulasiraj, R.D.; Vijayakumar, V. Prevalence and risk factors for diabetic retinopathy: A population-based assessment from Theni District, South India. Br. J. Ophthalmol. 2009, 93, 429–434. [Google Scholar] [CrossRef]
- Tajunisah, I.; Nabilah, H.; Reddy, S.C. Prevalence and risk factors for DR—A study of 217 patients from University of Malaya Medical Centre. Med. J. Malays. 2006, 61, 451–456. Available online: http://eprints.um.edu.my/1799/ (accessed on 24 January 2022).
- Raman, R.; Rani, P.; Reddi Rachepalle, S.; Gnanamoorthy, P.; Uthra, S.; Kumaramanickavel, G.; Sharma, T. Prevalence of DR in India. Sankara Nethralaya DR Epidemiology and Molecular Genetics Study Report 2. Ophthalmology 2009, 116, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Cherchi, S.; Gigante, A.; Spanu, M.A.; Contini, P.; Meloni, G.; Fois, M.A.; Pistis, D.; Pilosu, R.M.; Lai, A.; Ruiu, S.; et al. Sex-Gender Differences in Diabetic Retinopathy. Diabetology 2020, 1, 1–10. [Google Scholar] [CrossRef]
- Ghaffar, Z.; Butt, Z.; Shah, S.M.A.; Tarar, S.H.; Afzal, M. Frequency of Diabetic Retinopathy among known Diabetics at District Level Teaching Hospital. J. Ophthalmol. 2022, 38, 170–174. [Google Scholar] [CrossRef]
- Li, M.; Wang, Y.; Liu, Z.; Tang, X.; Mu, P.; Tan, Y.; Wang, J.; Lin, B.; Deng, J.; Peng, R.; et al. Females with Type 2 Diabetes Mellitus Are Prone to Diabetic Retinopathy: A Twelve-Province Cross-Sectional Study in China. J. Diabetes Res. 2020, 2020, 5814296. [Google Scholar] [CrossRef] [PubMed]
- Sabanayagam, C.; Wong, T.Y. Diabetic Retinopathy and Cardiovascular Disease. Front. Diabetes Basel Karger. 2019, 27, 20–37. [Google Scholar] [CrossRef]
- Lima, V.C.; Cavalieri, G.C.; Lima, M.C.; Nazario, N.O.; Lima, G.C. Risk factors for diabetic retinopathy: A case–control study. Int. J. Retin. Vitr. 2016, 2, 21. [Google Scholar] [CrossRef]
- Gunnlaugsdottir, E.; Halldorsdottir, S.; Klein, R.; Eiriksdottir, G.; Klein, B.E.; Benediktsson, R.; Harris, T.B.; Launer, L.J.; Aspelund, T.; Gudnason, V.; et al. Retinopathy in old persons with and without diabetes mellitus: The Age, Gene/Environment Susceptibility--Reykjavik Study (AGES-R). Diabetologia 2012, 55, 671–680. [Google Scholar] [CrossRef]
- Van Leiden, H.A.; Dekker, J.M.; Moll, A.C.; Nijpels, G.; Heine, R.J.; Bouter, M.; Stehouwer, C.D.A.; Polak, B.C.P. Risk Factors for Incident Retinopathy in a Diabetic and Nondiabetic Population: The Hoorn Study. Arch. Ophthalmol. 2003, 121, 245–251. [Google Scholar] [CrossRef]
- Magliah, S.F.; Bardisi, W.; Al Attah, M.; Khorsheed, M.M. The prevalence and risk factors of diabetic retinopathy in selected primary care centers during the 3-year screening intervals. J. Family Med. Prim. Care 2018, 7, 975–981. [Google Scholar]
- Tan, F.; Chen, Q.; Zhuang, X.; Wu, C.; Qian, Y.; Wang, Y.; Wang, J.; Lu, F.; Shen, M.; Li, Y. Associated risk factors in the early stage of diabetic retinopathy. Eye Vis. 2019, 6, 23. [Google Scholar] [CrossRef]
- Ngah, N.F.; Muhamad, N.A.; Asnir, Z.Z.; Aziz, R.A.A.; Kassim, Z.M.; Sahar, S.A.; Tarmidzi, N.A.A.; Chan, L.Y.; Uthman, R.; Satar, N.; et al. Descriptive assessment on diabetic retinopathy screening in an awareness programme in Malaysia. Int. J. Ophthalmol. 2020, 13, 1808–1813. [Google Scholar] [CrossRef] [PubMed]
- Petrie, J.R.; Guzik, T.J.; Touy, R.M. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 2018, 34, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Ting, D.S.; Cheung, G.C.; Wong, T.Y. Diabetic retinopathy: Global prevalence, major risk factors, screening practices and public health challenges: A review. Clin. Exp. Ophthalmol. 2016, 44, 260–277. [Google Scholar] [CrossRef]
- Chang, Y.C.; Wu, W.C. Dyslipidemia and diabetic retinopathy. Rev. Diabet. Stud. 2013, 10, 121–132. [Google Scholar] [CrossRef]
- Hammer, S.S.; Busik, J.V. The role of dyslipidemia in diabetic retinopathy. Vision Res. 2017, 139, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Kaštelan, S.; Tomić, M.; Gverović Antunica, A.; Ljubić, S.; Salopek Rabatić, J.; Karabatić, M. Body mass index: A risk factor for retinopathy in type 2 diabetic patients. Mediat. Inflamm. 2013, 2013, 436329. [Google Scholar] [CrossRef] [PubMed]
- Klein, R.; Knudtson, M.D.; Lee, K.E.; Gangnon, R.; Klein, B.E.K. The Wisconsin Epidemiologic Study of DR XXII the twenty-five-year progression of retinopathy in persons with type 1 diabetes. Ophthalmology 2008, 115, 1859–1868. [Google Scholar] [CrossRef]
- Dirani, M.; Xie, J.; Fenwick, E.; Benarous, R.; Rees, G.; Wong, T.Y.; Lamoureux, E.L. Are obesity and anthropometry risk factors for diabetic retinopathy?: The diabetes management project. Investig. Ophthalmol. Vis. Sci. 2011, 52, 4416–4421. [Google Scholar] [CrossRef]
- Van Leiden, H.A.; Dekker, J.M.; Moll, A.C.; Nijpels, G.; Heine, R.J.; Bouter, L.M.; Stehouwer, D.A.; Polak, B.C.P. Blood pressure, lipids, and obesity are associated with retinopathy: The Hoorn Study. Diabetes Care 2002, 25, 1320–1325. [Google Scholar] [CrossRef]
- Lee, W.J.; Sobrin, L.; Lee, M.J.; Kang, M.H.; Seong, M.; Cho, H. The relationship between DR and diabetic nephropathy in a population-based study in Korea (KNHANES V-2, 3). Investig. Ophthalmol. Vis. Sci. 2014, 55, 6547–6553. [Google Scholar] [CrossRef]
- Hwang, D.J.; Lee, K.M.; Park, M.S.; Choi, S.H.; Park, J.I.; Cho, J.H.; Park, K.H.; Woo, S.J. Association between diabetic foot ulcer and diabetic retinopathy. PLoS ONE 2017, 12, e0175270. [Google Scholar] [CrossRef] [PubMed]
- Serban, D.; Papanas, N.; Dascalu, A.M.; Stana, D.; Nicolae, V.A.; Vancea, G.; Badiu, C.D.; Tanasescu, D.; Tudor, C.; Balasescu, S.A.; et al. Diabetic Retinopathy in Patients With Diabetic Foot Ulcer: A Systematic Review. Int. J. Low Extrem. Wounds 2021, 20, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Muhamad, N.A.; Mutalip, M.H.A.; Mustapha, N.; Dali, N.S.M.; Aris, T.; Ismail, T.F.; Murad, S.; Sulaiman, L.H. Association between Comorbidities and Selected Sociodemographic Factors with Complications of Diabetes: Results from the National Diabetic Registry Malaysia. J. Diabetes Mellit. 2018, 8, 84–97. [Google Scholar] [CrossRef] [Green Version]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Study was written in English language | Study was written in other than English language |
| Study conducted among type 2 diabetes patients | Study conducted among other than type 2 diabetes patients |
| Study conducted among diabetic retinopathy patients | Study on other diabetic complications |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naserrudin, N.A.; Jeffree, M.S.; Kaur, N.; Rahim, S.S.S.A.; Ibrahim, M.Y. Study on the Development of a Conceptual Framework to Identify the Risk Factors of Diabetic Retinopathy among Diabetic Patients: A Concept Paper. Int. J. Environ. Res. Public Health 2022, 19, 12426. https://doi.org/10.3390/ijerph191912426
Naserrudin NA, Jeffree MS, Kaur N, Rahim SSSA, Ibrahim MY. Study on the Development of a Conceptual Framework to Identify the Risk Factors of Diabetic Retinopathy among Diabetic Patients: A Concept Paper. International Journal of Environmental Research and Public Health. 2022; 19(19):12426. https://doi.org/10.3390/ijerph191912426
Chicago/Turabian StyleNaserrudin, Nurul Athirah, Mohammad Saffree Jeffree, Nirmal Kaur, Syed Sharizman Syed Abdul Rahim, and Mohd Yusof Ibrahim. 2022. "Study on the Development of a Conceptual Framework to Identify the Risk Factors of Diabetic Retinopathy among Diabetic Patients: A Concept Paper" International Journal of Environmental Research and Public Health 19, no. 19: 12426. https://doi.org/10.3390/ijerph191912426
APA StyleNaserrudin, N. A., Jeffree, M. S., Kaur, N., Rahim, S. S. S. A., & Ibrahim, M. Y. (2022). Study on the Development of a Conceptual Framework to Identify the Risk Factors of Diabetic Retinopathy among Diabetic Patients: A Concept Paper. International Journal of Environmental Research and Public Health, 19(19), 12426. https://doi.org/10.3390/ijerph191912426







