Longitudinal Relationship between Cognitive Function and Health-Related Quality of Life among Middle-Aged and Older Patients with Diabetes in China: Digital Usage Behavior Differences
Abstract
1. Introduction
2. Materials and Methods
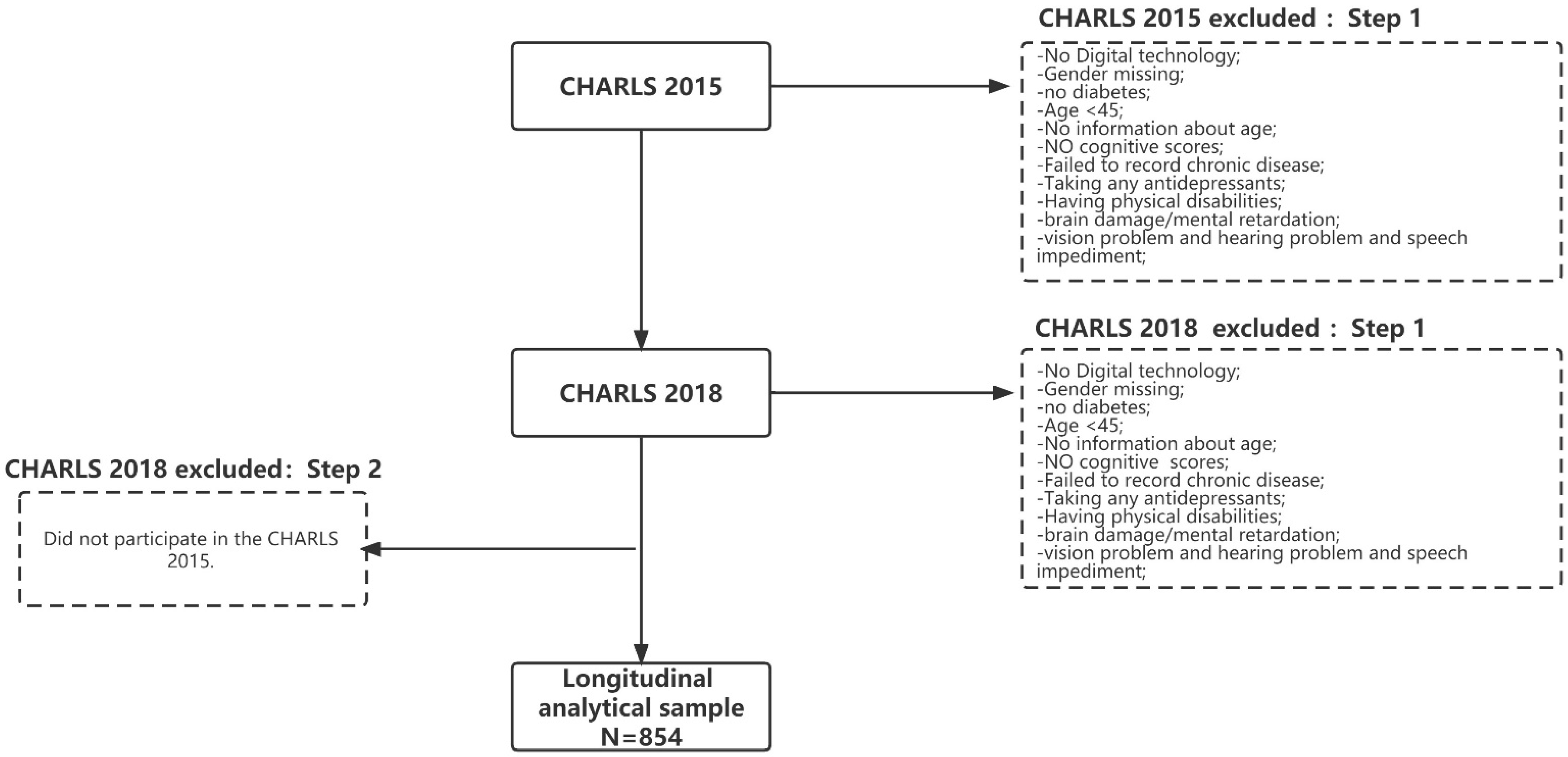
2.1. Participants
2.2. Measurements
2.2.1. Cognitive Functioning
2.2.2. HRQoL
2.2.3. Socio-Demographic Variables
2.3. Statistical Methods
3. Results
3.1. Descriptive Statistics
3.2. Stability Analysis of Cognitive Function and HRQoL
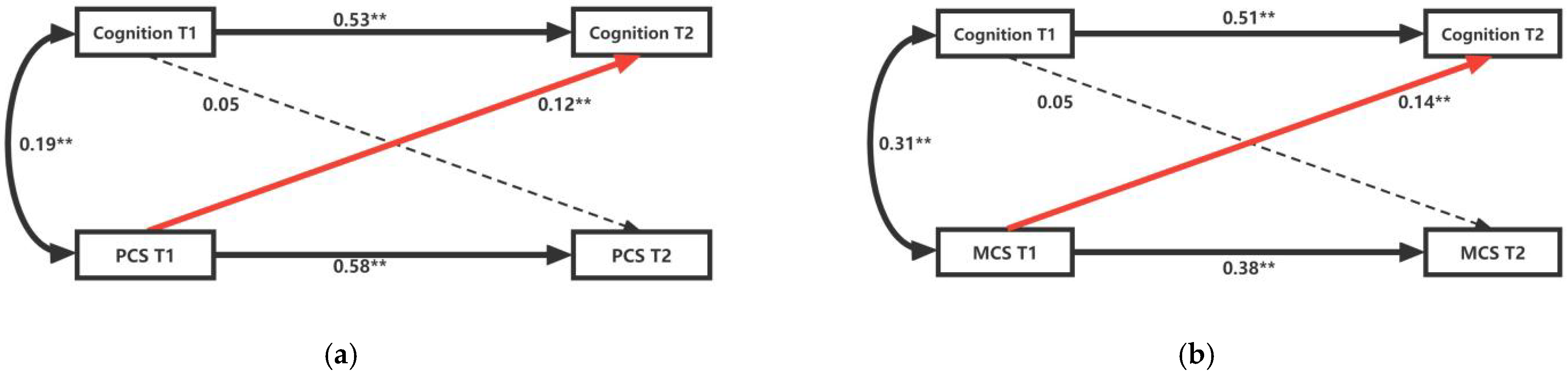
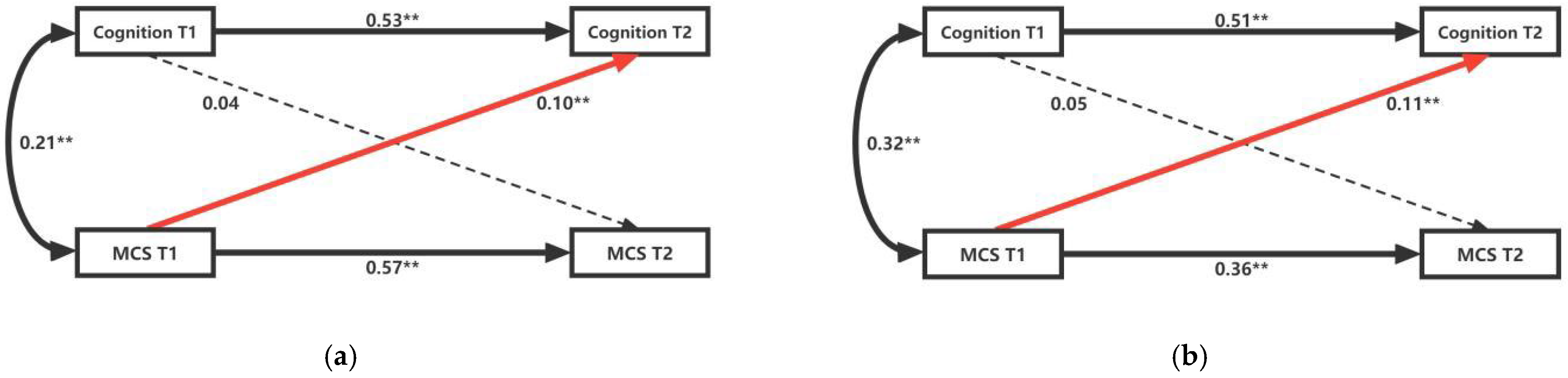
3.3. Cross-Lagged Analysis of Cognitive Function and HRQoL
3.4. Heterogeneity Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Godin, J.; Armstrong, J.J.; Wallace, L.; Rockwood, K.; Andrew, M.K. The impact of frailty and cognitive impairment on quality of life: Employment and social context matter. Int. Psychogeriatr. 2019, 31, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Zhang, Y.; Wang, Z.; Shen, H. Sleep Quality Partially Mediate the Relationship Between Depressive Symptoms and Cognitive Function in Older Chinese: A Longitudinal Study Across 10 Years. Psychol. Res. Behav. Manag. 2022, 15, 785–799. [Google Scholar] [CrossRef] [PubMed]
- IDF Diabetes Atlas. Available online: https://diabetesatlas.org/ (accessed on 20 August 2022).
- Hoogs, M.; Kaur, S.; Smerbeck, A.; Weinstock-Guttman, B.; Benedict, R.H.B. Cognition and physical disability in predicting health-related quality of life in multiple sclerosis. Int. J. MS Care 2011, 13, 57–63. [Google Scholar] [CrossRef] [PubMed]
- The Centers for Disease Control Prevention. Available online: https://www.cdc.gov/ (accessed on 20 August 2022).
- Wei, Y.; Speechley, K.N.; Zou, G.Y.; Campbell, C. The relationship between quality of life and health-related quality of life in young males with Duchenne muscular dystrophy. Dev. Med. Child Neurol. 2017, 59, 1152–1157. [Google Scholar] [CrossRef]
- Schmoldt, A.; Benthe, H.F.; Haberland, G. Digitoxin metabolism by rat-liver microsomes. Biochem. Pharmacol. 1975, 24, 1639–1641. [Google Scholar] [CrossRef]
- Pan, C.W.; Wang, X.Z.; Ma, Q.H.; Sun, H.P.; Xu, Y.; Wang, P. Cognitive dysfunction and health-related quality of life among older Chinese. Sci. Rep. 2015, 5, 8. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.D.; Kuhn, T.; Levine, A.; Sacktor, N.; Munro, C.A.; Teplin, L.A.; D’Souza, G.; Martin, E.M.; Becker, J.T.; Miller, E.N.; et al. Changes in Cognition Precede Changes in HRQoL Among HIV plus Males: Longitudinal Analysis of the Multicenter AIDS Cohort Study. Neuropsychology 2019, 33, 370–378. [Google Scholar] [CrossRef]
- Davis, J.C.; Marra, C.A.; Najafzadeh, M.; Liu-Ambrose, T. The independent contribution of executive functions to health related quality of life in older women. BMC Geriatr. 2010, 10, 8. [Google Scholar] [CrossRef]
- Janssen, N.; Handels, R.L.; Wimo, A.; Antikainen, R.; Laatikainen, T.; Soininen, H.; Strandberg, T.; Tuomilehto, J.; Kivipelto, M.; Evers, S.M.A.A.; et al. Association Between Cognition, Health Related Quality of Life, and Costs in a Population at Risk for Cognitive Decline. J. Alzheimer’s Dis. JAD 2022, 89, 623–632. [Google Scholar] [CrossRef]
- Ezzati, A.; Zammit, A.R.; Katz, M.J.; Derby, C.A.; Zimmerman, M.E.; Lipton, R.B. Health-related Quality of Life, Cognitive Performance, and Incident Dementia in a Community-based Elderly Cohort. Alzheimer Dis. Assoc. Dis. 2019, 33, 240–245. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, J.; Liao, Z.Y.; Zhao, X.M.; Hu, X.F.; Zhu, W.L.; Zhang, Z.F. Association between Diabetes and Cognitive Function among People over 45 Years Old in China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 12. [Google Scholar] [CrossRef] [PubMed]
- Xue, M.; Xu, W.; Ou, Y.N.; Cao, X.P.; Tan, M.S.; Tan, L.; Yu, J.T. Diabetes mellitus and risks of cognitive impairment and dementia: A systematic review and meta-analysis of 144 prospective studies. Ageing Res. Rev. 2019, 55, 9. [Google Scholar] [CrossRef] [PubMed]
- Rawlings, A.M.; Sharrett, A.R.; Schneider, A.L.C.; Coresh, J.; Albert, M.; Couper, D.; Griswold, M.; Gottesman, R.F.; Wagenknecht, L.E.; Windham, B.G.; et al. Diabetes in Midlife and Cognitive Change over 20 Years A Cohort Study. Ann. Intern. Med. 2014, 161, 785–793. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.J.; D’Alessio, D.A.; Fradkin, J.; Kernan, W.N.; Mathieu, C.; Mingrone, G.; Rossing, P.; Tsapas, A.; Wexler, D.J.; Buse, J.B. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018, 41, 2669–2701. [Google Scholar] [CrossRef] [PubMed]
- Pelimanni, E.; Jehkonen, M. Type 2 Diabetes and Cognitive Functions in Middle Age: A Meta-Analysis. J. Int. Neuropsychol. Soc. 2019, 25, 215–229. [Google Scholar] [CrossRef]
- Jin, Y.Z.; Jing, M.X.; Ma, X.C. Effects of Digital Device Ownership on Cognitive Decline in a Chinese Middle-Aged and Elderly Population: Longitudinal Observational Study. J. Med. Internet Res. 2019, 21, 9. [Google Scholar] [CrossRef]
- Liapis, J.; Harding, K.E. Meaningful use of computers has a potential therapeutic and preventative role in dementia care: A systematic review. Australas. J. Ageing 2017, 36, 299–307. [Google Scholar] [CrossRef]
- Moreira, T.R.; Negreiros, F.D.D.; de Aquino, M.D.N.; da Silva, L.M.S.; Moreira, T.M.M.; Torres, R.A.M. Digital technology and its effects on knowledge improvement for diabetes management: An integrative review. Int. J. Nurs. Pract. 2021, 9, e13029. [Google Scholar] [CrossRef]
- Masaeli, N.; Billieux, J. Is Problematic Internet and Smartphone Use Related to Poorer Quality of Life? A Systematic Review of Available Evidence and Assessment Strategies. Curr. Addict. Rep. 2022, 9, 235–250. [Google Scholar] [CrossRef]
- Celik, B.; Ones, K.; Celik, E.C.; Bugdayci, D.S.; Paker, N.; Avci, C.; Ince, N. The effects of using the internet on the health-related quality of life in people with spinal cord injury: A controlled study. Spinal Cord 2014, 52, 388–391. [Google Scholar] [CrossRef][Green Version]
- Qian, B.; Huang, M.; Xu, M.; Hong, Y. Internet Use and Quality of Life: The Multiple Mediating Effects of Risk Perception and Internet Addiction. Int. J. Environ. Res. Public Health 2022, 19, 1795. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.D.; Fiebig, D.G. Internet use and cognition among middle-aged and older adults in China: A cross-lagged panel analysis. J. Econ. Ageing 2020, 17, 9. [Google Scholar] [CrossRef]
- Caner, N.; Evgin, D. Digital risks and adolescents: The relationships between digital game addiction, emotional eating, and aggression. Int. J. Ment. Health Nurs. 2021, 30, 1599–1609. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Wang, Q.; Li, C. The Impact of Dependency Burden on Urban Household Health Expenditure and Its Regional Heterogeneity in China: Based on Quantile Regression Method. Front. Public Health 2022, 10, 876088. [Google Scholar] [CrossRef]
- Rong, H.G.; Lai, X.Z.; Jing, R.Z.; Wang, X.; Fang, H.; Mahmoudi, E. Association of Sensory Impairments with Cognitive Decline and Depression Among Older Adults in China. JAMA Netw. Open 2020, 3, 12. [Google Scholar] [CrossRef]
- Qin, T.T.; Yan, M.M.; Fu, Z.; Song, Y.T.; Lu, W.R.; Fu, A.; Yin, P. Association between anemia and cognitive decline among Chinese middle-aged and elderly: Evidence from the China health and retirement longitudinal study. BMC Geriatr. 2019, 19, 13. [Google Scholar] [CrossRef]
- Kamin, S.T.; Lang, F.R. Internet Use and Cognitive Functioning in Late Adulthood: Longitudinal Findings from the Survey of Health, Ageing and Retirement in Europe (SHARE). J. Gerontol. Ser. B-Psychol. Sci. Soc. Sci. 2020, 75, 534–539. [Google Scholar] [CrossRef]
- Jandhyala, R. Neutral theory: Applicability and neutrality of using generic health-related quality of life tools in diseases or conditions where specific tools are available. BMC Med. Res. Methodol. 2021, 21, 8. [Google Scholar] [CrossRef]
- Hao, X.Q.; Yang, Y.H.; Gao, X.T.; Dai, T. Evaluating the Effectiveness of the Health Management Program for the Elderly on Health-Related Quality of Life among Elderly People in China: Findings from the China Health and Retirement Longitudinal Study. Int. J. Environ. Res. Public Health 2019, 16, 9. [Google Scholar] [CrossRef]
- Wright, S.P.; Doughty, R.N. Measuring health-related quality of life. N. Z. Med. J. 1999, 112, 366. [Google Scholar]
- Palarino, J.V.; Boardman, J.D.; Rogers, R.G. Cognition and Diabetes: Examining Sex Differences Using a Longitudinal Sample of Older Adults. Res. Aging 2022, 12, 01640275221084282. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, E.R.Q.; Gouveia, B.R.; Ihle, A.; Kliegel, M.; Maia, J.A.; Badia, S.B.I.; Freitas, D.L. Correlates of health-related quality of life in young-old and old-old community-dwelling older adults. Qual. Life Res. 2017, 26, 1561–1569. [Google Scholar] [CrossRef]
- Langa, K.M.; Levine, D.A. The Diagnosis and Management of Mild Cognitive Impairment A Clinical Review. JAMA-J. Am. Med. Assoc. 2014, 312, 2551–2561. [Google Scholar] [CrossRef] [PubMed]
- Zaninotto, P.; Falaschetti, E.; Sacker, A. Age trajectories of quality of life among older adults: Results from the English Longitudinal Study of Ageing. Qual. Life Res. 2009, 18, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Musen, G.; Tinsley, L.J.; Marcinkowski, K.A.; Pober, D.; Sun, J.K.; Khatri, M.; Huynh, R.; Lu, A.; King, G.L.; Keenan, H.A. Cognitive Function Deficits Associated with Long-Duration Type 1 Diabetes and Vascular Complications. Diabetes Care 2018, 41, 1749–1756. [Google Scholar] [CrossRef]
- Wang, G.; Li, W. Diabetes as a Risk Factor for Abnormal Cognition Development. J. Alzheimers Dis. Rep. 2020, 4, 237–242. [Google Scholar] [CrossRef]
- Liu, X.J.; Chen, S.N.; Tan, A.R.; Zhou, J.Y.; Liu, W.B. Stay Slim or Get Fat?: An Examination of the “Jolly Fat” Effect in Chinese Older Adults. Risk Manag. Healthc. Policy 2021, 14, 1271–1279. [Google Scholar] [CrossRef]
- Janssen, I. Morbidity and mortality risk associated with an overweight BMI in older men and women. Obesity 2007, 15, 1827–1840. [Google Scholar] [CrossRef]
- Verghese, J.; Lipton, R.B.; Katz, M.J.; Hall, C.B.; Derby, C.A.; Kuslansky, G.; Ambrose, A.F.; Sliwinski, M.; Buschke, H. Leisure activities and the risk of dementia in the elderly. N. Engl. J. Med. 2003, 348, 2508–2516. [Google Scholar] [CrossRef]
- Daviglus, M.L.; Plassman, B.L.; Pirzada, A.; Bell, C.C.; Bowen, P.E.; Burke, J.R.; Connolly, E.S.; Dunbar-Jacob, J.M.; Granieri, E.C.; McCarty, K.; et al. Risk Factors and Preventive Interventions for Alzheimer Disease State of the Science. Arch. Neurol. 2011, 68, 1185–1190. [Google Scholar] [CrossRef]
- Yu, F.; Chen, Y.; Mathiason, M.A.; Wan, Q.Q.; Lin, F.V. Cognitive and physical factors affecting daily function in Alzheimer’s disease: A cross-sectional analysis. Nurs. Health Sci. 2019, 21, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Uchino, T.; Okubo, R.; Takubo, Y.; Aoki, A.; Wada, I.; Hashimoto, N.; Ikezawa, S.; Nemoto, T. Perceptions of and subjective difficulties with social cognition in schizophrenia from an internet survey: Knowledge, clinical experiences, and awareness of association with social functioning. Psychiatry Clin. Neurosci. 2022, 76, 429–436. [Google Scholar] [CrossRef]
- Clare, L.; Gamble, L.D.; Martyr, A.; Sabatini, S.; Nelis, S.M.; Quinn, C.; Pentecost, C.; Victor, C.; Jones, R.W.; Jones, I.R.; et al. Longitudinal Trajectories of Quality of Life Among People with Mild-to-Moderate Dementia: A Latent Growth Model Approach with IDEAL Cohort Study Data. J. Gerontol. Ser. B-Psychol. Sci. Soc. Sci. 2022, 77, 1037–1050. [Google Scholar] [CrossRef] [PubMed]
- Langlois, F.; Thien, T.M.V.; Kergoat, M.J.; Chasse, K.; Dupuis, G.; Bherer, L. The multiple dimensions of frailty: Physical capacity, cognition, and quality of life. Int. Psychogeriatr. 2012, 24, 1429–1436. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.S.; Barnes, L.L.; Krueger, K.R.; Hoganson, G.; Bienias, J.L.; Bennett, D.A. Early and late life cognitive activity and cognitive systems in old age. J. Int. Neuropsychol. Soc. 2005, 11, 400–407. [Google Scholar] [CrossRef]
- Chan, M.Y.; Haber, S.; Drew, L.M.; Park, D.C. Training Older Adults to Use Tablet Computers: Does It Enhance Cognitive Function? Gerontologist 2016, 56, 475–484. [Google Scholar] [CrossRef]
- Cecutti, L.; Chemero, A.; Lee, S.W.S. Technology may change cognition without necessarily harming it. Nat. Hum. Behav. 2021, 5, 973–975. [Google Scholar] [CrossRef]
- Berner, J.; Comijs, H.; Elmstahl, S.; Welmer, A.K.; Berglund, J.S.; Anderberg, P.; Deeg, D. Maintaining cognitive function with internet use: A two-country, six-year longitudinal study. Int. Psychogeriatr. 2019, 31, 929–936. [Google Scholar] [CrossRef]
- Jia, S.Q.; Zhang, L.H. Health Education Based on Internet Platform for Improving Cognitive Function of Patients with Type 2 Diabetes. J. Med. Imaging Health Inform. 2020, 10, 2920–2924. [Google Scholar] [CrossRef]
- Ganju, K.K.; Pavlou, P.A.; Banker, R.D. Does information and communication technology lead to the well-being of nations? A country-level empirical investigation. MIS Q. 2016, 40, 417–430. [Google Scholar] [CrossRef]
- Jahangiry, L.; Montazeri, A.; Najafi, M.; Yaseri, M.; Farhangi, M.A. An interactive web-based intervention on nutritional status, physical activity and health-related quality of life in patient with metabolic syndrome: A randomized-controlled trial (The Red Ruby Study). Nutr. Diabetes 2017, 7, 8. [Google Scholar] [CrossRef] [PubMed]
- Binder, M.; Buenstorf, G. Smile or die: Can subjective well-being increase survival in the face of substantive health impairments? Econ. Hum. Biol. 2018, 31, 209–227. [Google Scholar] [CrossRef] [PubMed]
- Rotondi, V.; Stanca, L.; Tomasuolo, M. Connecting alone: Smartphone use, quality of social interactions and well-being. J. Econ. Psychol. 2017, 63, 17–26. [Google Scholar] [CrossRef]
- Aalbers, T.; Baars, M.A.E.; Rikkert, M. Characteristics of effective Internet-mediated interventions to change lifestyle in people aged 50 and older: A systematic review. Ageing Res. Rev. 2011, 10, 487–497. [Google Scholar] [CrossRef]
- Guo, Z.M.; Xu, Y.T.; Li, S.M.; Qi, C.Z. Association between Urban Built Environments and Moderate-to-Vigorous Physical Activity of Adolescents: A Cross-Lagged Study in Shanghai, China. Int. J. Environ. Res. Public Health 2022, 19, 10. [Google Scholar] [CrossRef]

| Variable | Abbreviations |
|---|---|
| The China Health and Retirement Longitudinal Survey | CHARLS |
| the Short Form 36 | SF-36 |
| health-related quality of life | HRQoL |
| physical component summary | PCS |
| mental component summary | MCS |
| physical function | PF |
| role-body | RP |
| body pain | BP |
| general health | GH |
| vitality | VT |
| social functioning | SF |
| role-emotion | RE |
| mental health | MH |
| HRQoL (SF-36) | CHARLS Validity |
|---|---|
| PF | db001 db002 db003 db004 db005 db006 db007 db008 db009 |
| RP | db016 db017 db018 db019 db020 |
| BP | da041 da042s1 da042s2 da042s3 da042s4 da042s5 da042s6 da042s7 da042s8 da042s9 da042s10 da042s11 da042s12 da042s13 da042s14 da042s15 |
| GH | da001 da002 |
| VT | dc015 dc018 |
| SF | da056s1 da056s2 da056s3 da056s4 da056s5 da056s6 da056s7 da056s8 da056s9 da056s10 da056s11 da056s12 |
| RE | dc010 dc012 |
| MH | dc009 dc011 dc014 dc016 dc017 |
| Variables | All Participants | Digital Usage Behavior | |
|---|---|---|---|
| Yes | No | ||
| Cognition (Mean ± SD) | 15.73 ± 5.02 | 18.83 ± 4.09 | 14.62 ± 5.41 |
| PCS (Mean ± SD) | 71.82 ± 14.31 | 82.03 ± 8.97 | 70.71 ± 14.34 |
| MCS (Mean ± SD) | 56.48 ± 19.41 | 72.05 ± 11.92 | 66.30 ± 17.32 |
| Sex (male, n, %) | 467(54.71) | 120 (70.03) | 347 (50.87) |
| Age (Mean ± SD, years) | 63.09 ± 8.73 | 59.61 ± 8.12 | 63.47 ± 8.72 |
| Physical Activity (Mean ± SD) | 1.44 ± 1.27 | 0.57 ± 0.91 | 1.54 ± 1.27 |
| Depression (Mean ± SD) | 18.70 ± 6.79 | 14.95 ± 0.44 | 19.10 ± 6.99 |
| Marital status (Mean ± SD) | 0.86 ± 0.34 | 0.93 ± 0.26 | 0.85 ± 0.35 |
| Educational level (Mean ± SD) | 2.41 ± 1.29 | 3.87 ± 0.97 | 2.26 ± 1.22 |
| Smoking status (Mean ± SD) | 0.22 ± 0.41 | 0.45 ± 0.50 | 0.19 ± 0.39 |
| Drinking status (Mean ± SD) | 0.39 ± 0.64 | 0.73 ± 0.67 | 0.35 ± 0.62 |
| Variables | Cognition T1 | Cognition T2 | PCS T1 | PCS T2 | MCS T1 | MCS T2 |
|---|---|---|---|---|---|---|
| Cognition T1 | 1.00 | |||||
| Cognition T2 | 0.60 ** | 1.00 | ||||
| PCS T1 | 0.28 ** | 0.32 ** | 1.00 | |||
| PCS T2 | 0.25 ** | 0.32 ** | 0.63 ** | 1.00 | ||
| MCS T1 | 0.37 ** | 0.36 ** | 0.59 ** | 0.50 ** | 1.00 | |
| MCS T2 | 0.22 ** | 0.30 ** | 0.44 ** | 0.55 ** | 0.48 ** | 1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jia, Z.; Gao, Y.; Zhao, L.; Han, S. Longitudinal Relationship between Cognitive Function and Health-Related Quality of Life among Middle-Aged and Older Patients with Diabetes in China: Digital Usage Behavior Differences. Int. J. Environ. Res. Public Health 2022, 19, 12400. https://doi.org/10.3390/ijerph191912400
Jia Z, Gao Y, Zhao L, Han S. Longitudinal Relationship between Cognitive Function and Health-Related Quality of Life among Middle-Aged and Older Patients with Diabetes in China: Digital Usage Behavior Differences. International Journal of Environmental Research and Public Health. 2022; 19(19):12400. https://doi.org/10.3390/ijerph191912400
Chicago/Turabian StyleJia, Zhihao, Yan Gao, Liangyu Zhao, and Suyue Han. 2022. "Longitudinal Relationship between Cognitive Function and Health-Related Quality of Life among Middle-Aged and Older Patients with Diabetes in China: Digital Usage Behavior Differences" International Journal of Environmental Research and Public Health 19, no. 19: 12400. https://doi.org/10.3390/ijerph191912400
APA StyleJia, Z., Gao, Y., Zhao, L., & Han, S. (2022). Longitudinal Relationship between Cognitive Function and Health-Related Quality of Life among Middle-Aged and Older Patients with Diabetes in China: Digital Usage Behavior Differences. International Journal of Environmental Research and Public Health, 19(19), 12400. https://doi.org/10.3390/ijerph191912400







