Temporal Heterogeneity of Short-Term Effects of Particulate Matter on Stroke Outpatients in Seven Major Cities of the Republic of Korea
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
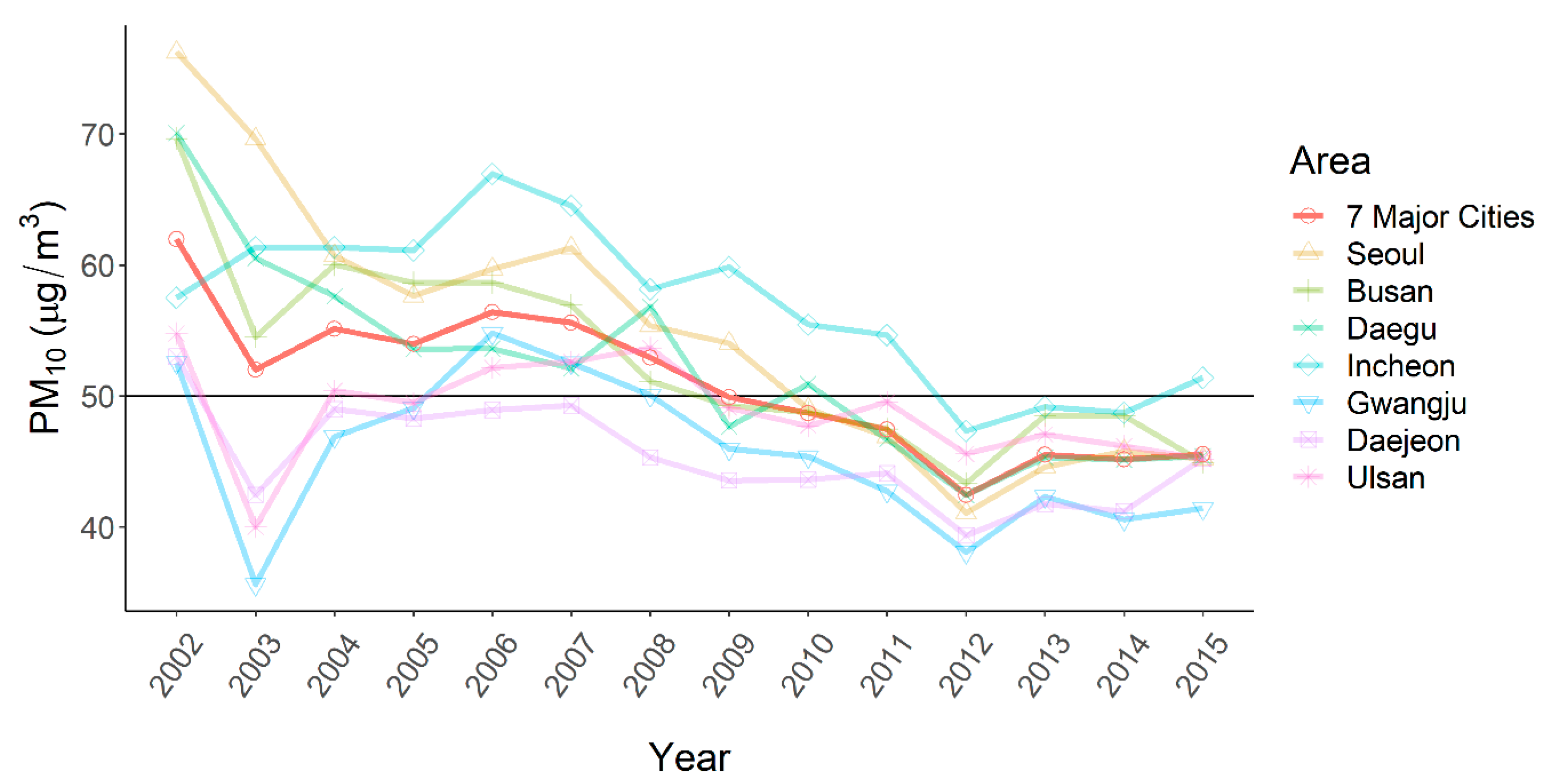
2.2. Exposure: PM10
2.3. Outcomes: Stroke Outpatients
2.4. Statistical Analysis
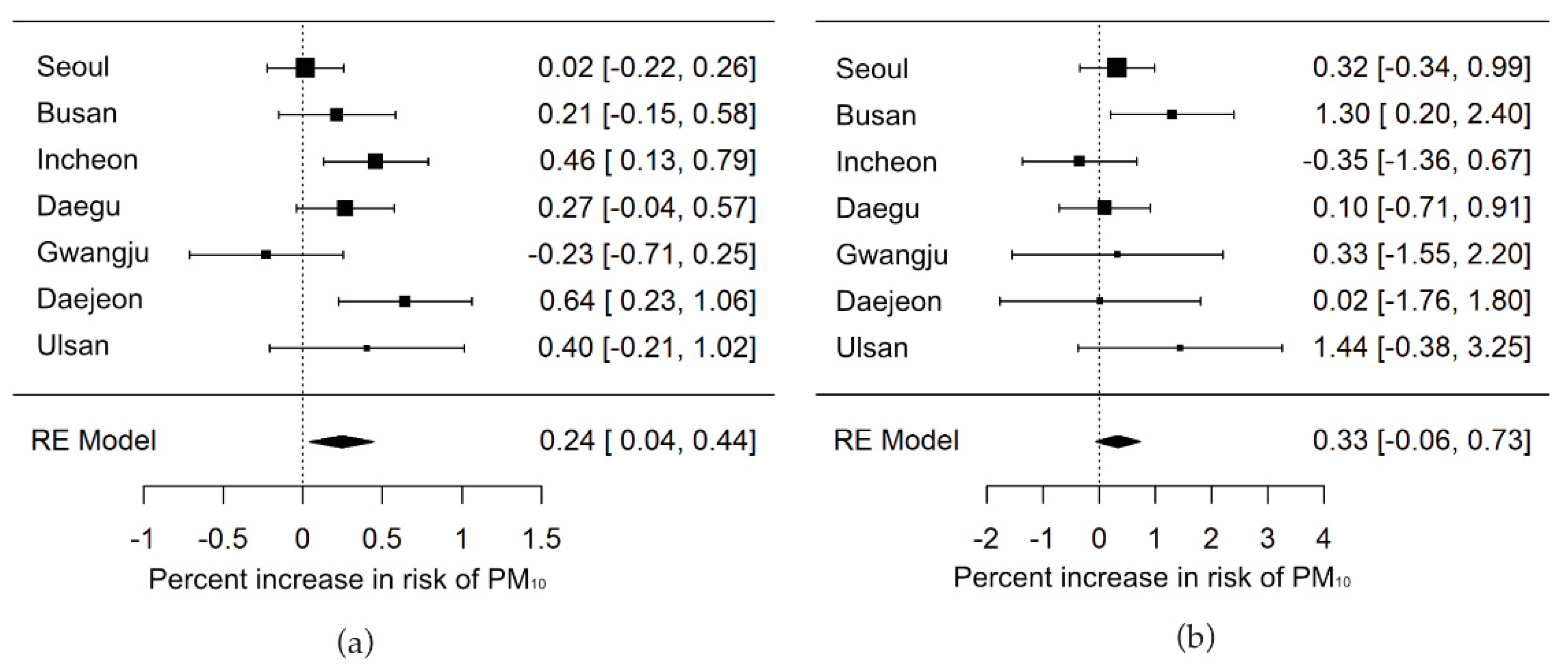
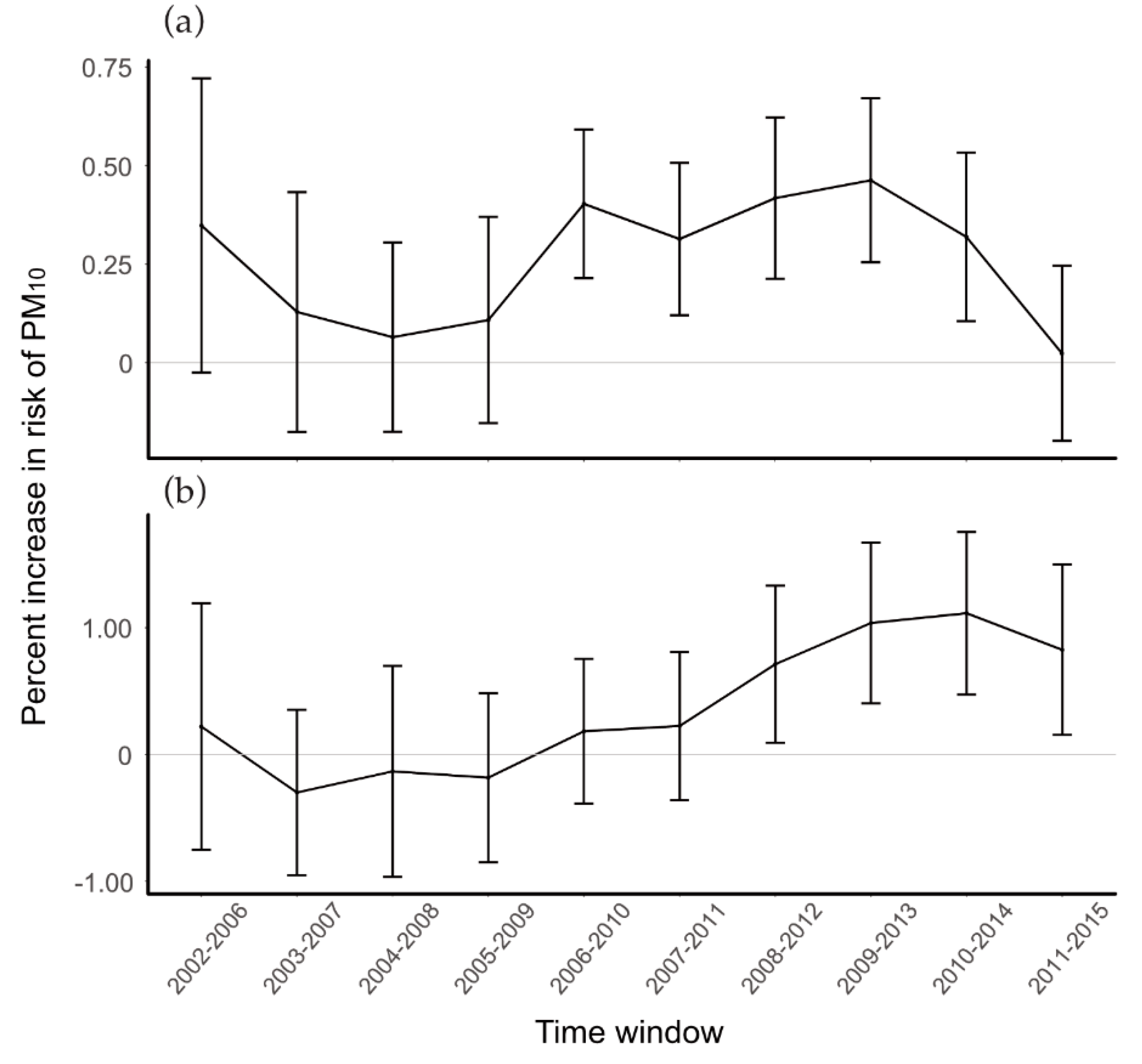
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- The Institute for Health Metrics and Evaluation. Country Profiles. Available online: http://www.healthdata.org/south-korea (accessed on 25 June 2022).
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 25 June 2022).
- Feigin, V.L.; Roth, G.A.; Naghavi, M.; Parmar, P.; Krishnamurthi, R.; Chugh, S.; Mensah, G.A.; Norrving, B.; Shiue, I.; Ng, M.; et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016, 15, 913–924. [Google Scholar] [CrossRef]
- Kim, K.H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [PubMed]
- Dąbrowiecki, P.; Badyda, A.; Chciałowski, A.; Czechowski, P.O.; Wrotek, A. Influence of Selected Air Pollutants on Mortality and Pneumonia Burden in Three Polish Cities over the Years 2011–2018. J. Clin. Med. 2020, 11, 3084. [Google Scholar] [CrossRef] [PubMed]
- Trnka, D. Policies, Regulatory Framework and Enforcement for Air Quality Management: The Case of Korea; Environment Working Paper No.158; OECD: Paris, France, 2020. [Google Scholar]
- Shah, A.S.; Lee, K.K.; McAllister, D.A.; Hunter, A.; Nair, H.; Whiteley, W.; Langrish, J.P.; Newby, D.E.; Mills, N.L. Short term exposure to air pollution and stroke: Systematic review and meta-analysis. BMJ 2015, 350, h1295. [Google Scholar] [CrossRef]
- Li, X.Y.; Yu, X.B.; Liang, W.W.; Yu, N.; Wang, L.; Ye, X.J.; Chen, K.; Bian, P.D. Meta-Analysis of Association between Particulate Matter and Stroke Attack. CNS Neurosci. Ther. 2012, 18, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kim, Y.; Hong, Y.C. The lag-effect pattern in the relationship of particulate air pollution to daily mortality in Seoul, Korea. Int. J. Biometeorol. 2003, 48, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.C.; Lee, J.T.; Kim, H.; Kwon, H.J. Air pollution: A new risk factor in ischemic stroke mortality. Stroke 2002, 33, 2165–2169. [Google Scholar] [CrossRef]
- Hong, Y.C.; Lee, J.T.; Kim, H.; Ha, E.H.; Schwartz, J.; Christiani, D.C. Effects of air pollutants on acute stroke mortality. Environ. Health Perspect. 2002, 110, 187–191. [Google Scholar] [CrossRef]
- Breitner, S.; Stolzel, M.; Cyrys, J.; Pitz, M.; Wolke, G.; Kreyling, W.; Kuchenhoff, H.; Heinrich, J.; Wichmann, H.E.; Peters, A. Short-term mortality rates during a decade of improved air quality in Erfurt, Germany. Environ. Health Perspect. 2009, 117, 448–454. [Google Scholar] [CrossRef]
- Chen, C.; Warrington, J.A.; Dominici, F.; Peng, R.D.; Esty, D.C.; Bobb, J.F.; Bell, M.L. Temporal variation in association between short-term exposure to fine particulate matter and hospitalisations in older adults in the USA: A long-term time-series analysis of the US Medicare dataset. Lancet Planet Health 2021, 5, E534–E541. [Google Scholar] [CrossRef]
- Choi, Y.; Kim, H.; Lee, J.T. Temporal variability of short term effects of PM10 on mortality in Seoul, Korea. Sci. Total Environ. 2018, 644, 122–128. [Google Scholar] [CrossRef]
- Dominici, F.; Peng, R.D.; Zeger, S.L.; White, R.H.; Samet, J.M. Particulate air pollution and mortality in the United States: Did the risks change from 1987 to 2000? Am. J. Epidemiol. 2007, 166, 880–888. [Google Scholar] [CrossRef]
- Kim, H.; Kim, H.; Lee, J.T. Effects of ambient air particles on mortality in Seoul: Have the effects changed over time? Environ. Res. 2015, 140, 684–690. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, K. Fine particulate matter components and mortality in Greater Houston: Did the risk reduce from 2000 to 2011? Sci. Total Environ. 2015, 538, 162–168. [Google Scholar] [CrossRef]
- Renzi, M.; Stafoggia, M.; Faustini, A.; Cesaroni, G.; Cattani, G.; Forastiere, F. Analysis of Temporal Variability in the Short-term Effects of Ambient Air Pollutants on Nonaccidental Mortality in Rome, Italy (1998–2014). Environ. Health Perspect. 2017, 125, 067019. [Google Scholar] [CrossRef]
- Tzima, K.; Analitis, A.; Katsouyanni, K.; Samoli, E. Has the risk of mortality related to short-term exposure to particles changed over the past years in Athens, Greece? Environ. Int. 2018, 113, 306–312. [Google Scholar] [CrossRef]
- Wu, R.; Zhong, L.; Huang, X.; Xu, H.; Liu, S.; Feng, B.; Wang, T.; Song, X.; Bai, Y.; Wu, F.; et al. Temporal variations in ambient particulate matter reduction associated short-term mortality risks in Guangzhou, China: A time-series analysis (2006–2016). Sci. Total Environ. 2018, 645, 491–498. [Google Scholar] [CrossRef]
- Statistics Korea Population, Households and Housing Units. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1IN1002&conn_path=I2&language=en (accessed on 24 May 2018).
- Hwang, J.; Shin, S.; Kim, J.; Oh, S.; Kang, H.; Park, S.; Jang, E.; Choi, J.; Hyun, M. Domestic Secondary Data Resources Utilization in Healthcare Research; National Evidence-Based Healthcare Collaborating Agency: Seoul, Korea, 2013. [Google Scholar]
- Bae, H.-J.; Ha, J.-S.; Lee, A.-K.; Park, J.-I. Age dependencies in air pollution-associated asthma hospitalization. J. Environ. Health Sci. 2008, 34, 124–130. [Google Scholar] [CrossRef]
- Bell, M.L.; Samet, J.M.; Dominici, F. Time-series studies of particulate matter. Annu. Rev. Public Health 2004, 25, 247–280. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Gasparrini, A.; Hajat, S.; Smeeth, L.; Armstrong, B. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 2013, 42, 1187–1195. [Google Scholar] [CrossRef]
- Byun, G.; Kim, H.; Choi, Y.; Lee, J.T. The difference in effect of ambient particles on mortality between days with and without yellow dust events: Using a larger dataset in Seoul, Korea from 1998 to 2015. Sci. Total Environ. 2019, 691, 819–826. [Google Scholar] [CrossRef]
- Lee, J.T.; Son, J.Y.; Cho, Y.S. A comparison of mortality related to urban air particles between periods with Asian dust days and without Asian dust days in Seoul, Korea, 2000–2004. Environ. Res. 2007, 105, 409–413. [Google Scholar] [CrossRef]
- Altman, D.G.; Bland, J.M. Statistics Notes—Interaction revisited: The difference between two estimates. BMJ-Brit. Med. J. 2003, 326, 219. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2013. [Google Scholar]
- Kim, H.; Bell, M.L.; Lee, J.T. Does a lag-structure of temperature confound air pollution-lag-response relation? Simulation and application in 7 major cities, Korea (1998–2013). Environ. Res. 2017, 159, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.K.; Miller, M.R.; Shah, A.S.V. Air Pollution and Stroke. J. Stroke 2018, 20, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Esmon, C.T. The impact of the inflammatory response on coagulation. Thromb. Res. 2004, 114, 321–327. [Google Scholar] [CrossRef]
- Peters, A.; Doring, A.; Wichmann, H.E.; Koenig, W. Increased plasma viscosity during an air pollution episode: A link to mortality? Lancet 1997, 349, 1582–1587. [Google Scholar] [CrossRef]
- Yorifuji, T.; Kawachi, I.; Sakamoto, T.; Doi, H. Associations of outdoor air pollution with hemorrhagic stroke mortality. J. Occup. Environ. Med. 2011, 53, 124–126. [Google Scholar] [CrossRef]
- Zhang, R.; Liu, G.; Jiang, Y.; Li, G.; Pan, Y.; Wang, Y.; Wei, Z.; Wang, J.; Wang, Y. Acute Effects of Particulate Air Pollution on Ischemic Stroke and Hemorrhagic Stroke Mortality. Front. Neurol. 2018, 9, 827. [Google Scholar] [CrossRef] [Green Version]
- Huang, F.; Luo, Y.; Guo, Y.; Tao, L.; Xu, Q.; Wang, C.; Wang, A.; Li, X.; Guo, J.; Yan, A.; et al. Particulate Matter and Hospital Admissions for Stroke in Beijing, China: Modification Effects by Ambient Temperature. J. Am. Heart. Assoc. 2016, 5, e003437. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kim, H.; Lee, J.T. Spatial variation in lag structure in the short-term effects of air pollution on mortality in seven major South Korean cities, 2006–2013. Environ. Int. 2019, 125, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-W.; Lee, H.S.; Jang, Y.J.; Lee, H.J. How does media construct particulate matter risks?: A news frame and source analysis on particulate matter risks. Korean J. Journal. Commun. Stud. 2015, 59, 121–154. [Google Scholar]
- El-Sayed, A.M.; Galea, S. Systems Science and Population Health; Oxford University Press: Oxford, UK, 2017. [Google Scholar]
| City | Population (Count) | Area (km2) | Number of Air Pollution Monitoring Stations |
|---|---|---|---|
| Seoul | 9,794,304 | 605 | 25 |
| Busan | 3,414,950 | 767 | 17 |
| Daegu | 2,446,418 | 884 | 11 |
| Incheon | 2,662,509 | 1029 | 15 |
| Gwangju | 1,475,745 | 501 | 7 |
| Daejeon | 1,501,859 | 540 | 7 |
| Ulsan | 1,082,567 | 1059 | 13 |
| Ischemic Stroke Outpatients | Hemorrhagic Stroke Outpatients | PM10 (µg/m3) | Temperature (°C) | Relative Humidity (%) | |
|---|---|---|---|---|---|
| Mean | 30.9 (30.4) | 2.5 (3.2) | 50.9 (33.2) | 13.8 (9.4) | 63.9 (16.3) |
| Seoul | 56.2 (36.9) | 4.3 (3.7) | 54.8 (41.2) | 12.8 (10.4) | 61.0 (14.9) |
| Busan | 36.3 (23.5) | 2.7 (2.5) | 52.9 (31.0) | 14.9 (8.1) | 62.0 (18.4) |
| Incheon | 23.5 (16.6) | 2.2 (2.4) | 57.0 (33.6) | 12.6 (9.8) | 69.5 (15.5) |
| Daegu | 58.1 (41.1) | 5.6 (4.5) | 52.0 (31.7) | 14.6 (9.5) | 57.6 (16.7) |
| Gwangju | 14.6 (9.6) | 0.9 (1.1) | 45.6 (30.0) | 14.2 (9.4) | 67.2 (13.2) |
| Daejeon | 17.2 (10.7) | 0.8 (1.1) | 45.4 (30.5) | 13.1 (9.9) | 67.0 (14.2) |
| Ulsan | 10.7 (8.5) | 0.8 (1.1) | 48.8 (30.8) | 14.5 (8.7) | 62.7 (17.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, Y.; Byun, G.; Lee, J.-T. Temporal Heterogeneity of Short-Term Effects of Particulate Matter on Stroke Outpatients in Seven Major Cities of the Republic of Korea. Int. J. Environ. Res. Public Health 2022, 19, 12316. https://doi.org/10.3390/ijerph191912316
Choi Y, Byun G, Lee J-T. Temporal Heterogeneity of Short-Term Effects of Particulate Matter on Stroke Outpatients in Seven Major Cities of the Republic of Korea. International Journal of Environmental Research and Public Health. 2022; 19(19):12316. https://doi.org/10.3390/ijerph191912316
Chicago/Turabian StyleChoi, Yongsoo, Garam Byun, and Jong-Tae Lee. 2022. "Temporal Heterogeneity of Short-Term Effects of Particulate Matter on Stroke Outpatients in Seven Major Cities of the Republic of Korea" International Journal of Environmental Research and Public Health 19, no. 19: 12316. https://doi.org/10.3390/ijerph191912316





