Effects of Social Vulnerability and Spatial Accessibility on COVID-19 Vaccination Coverage: A Census-Tract Level Study in Milwaukee County, USA
Abstract
:1. Introduction
2. Materials and Methods
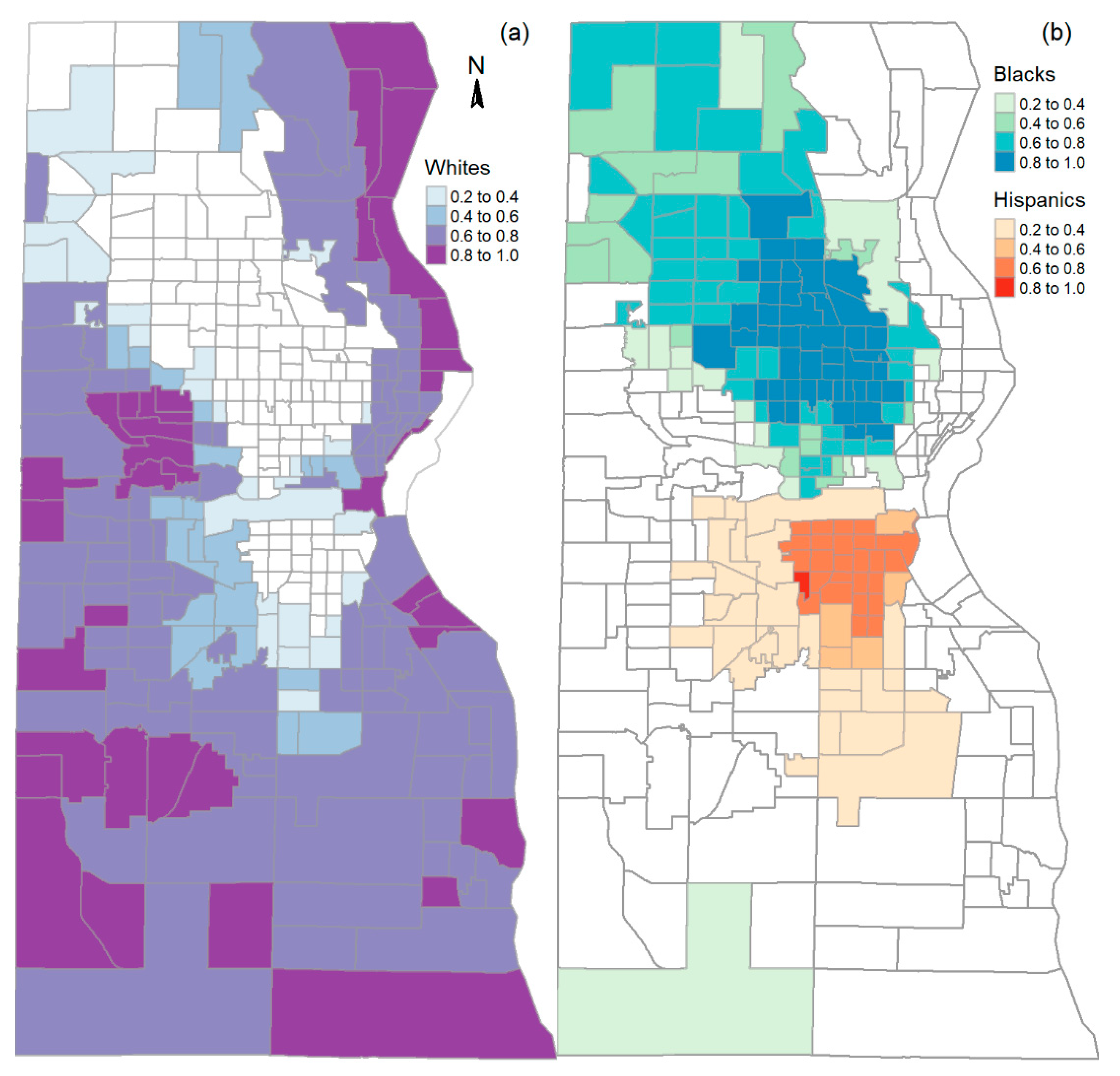
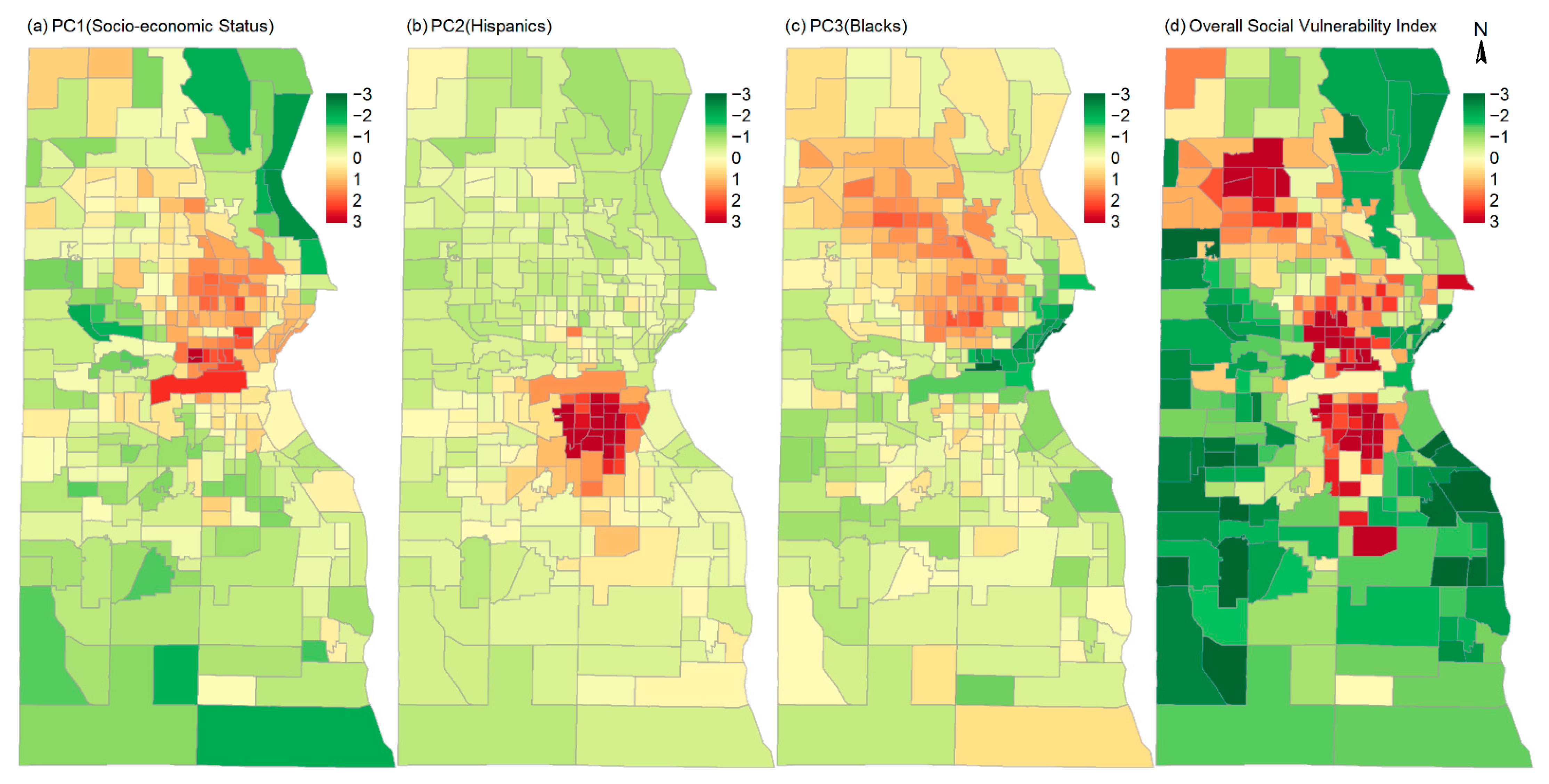
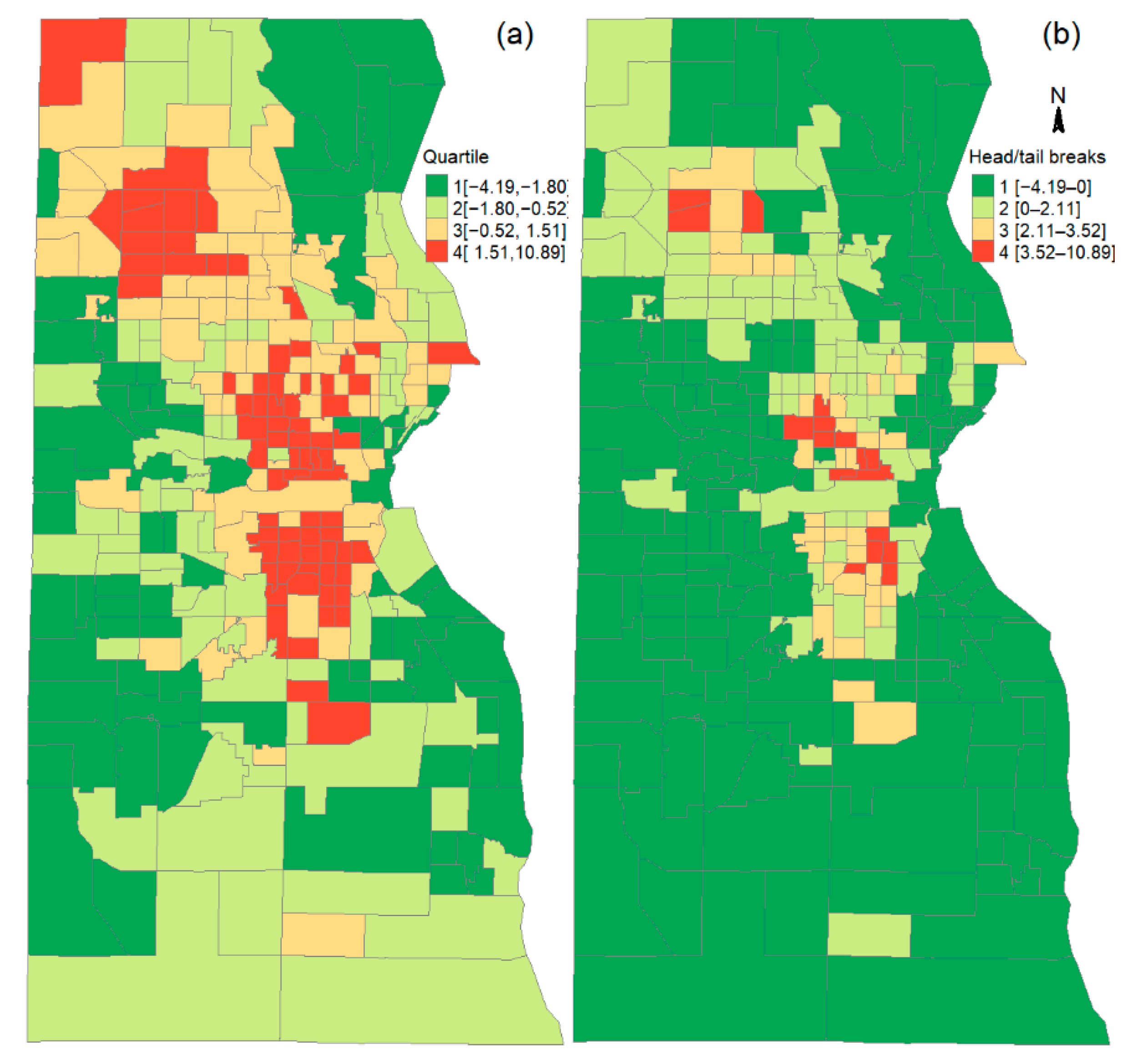
2.1. Index of Social Vulnerability
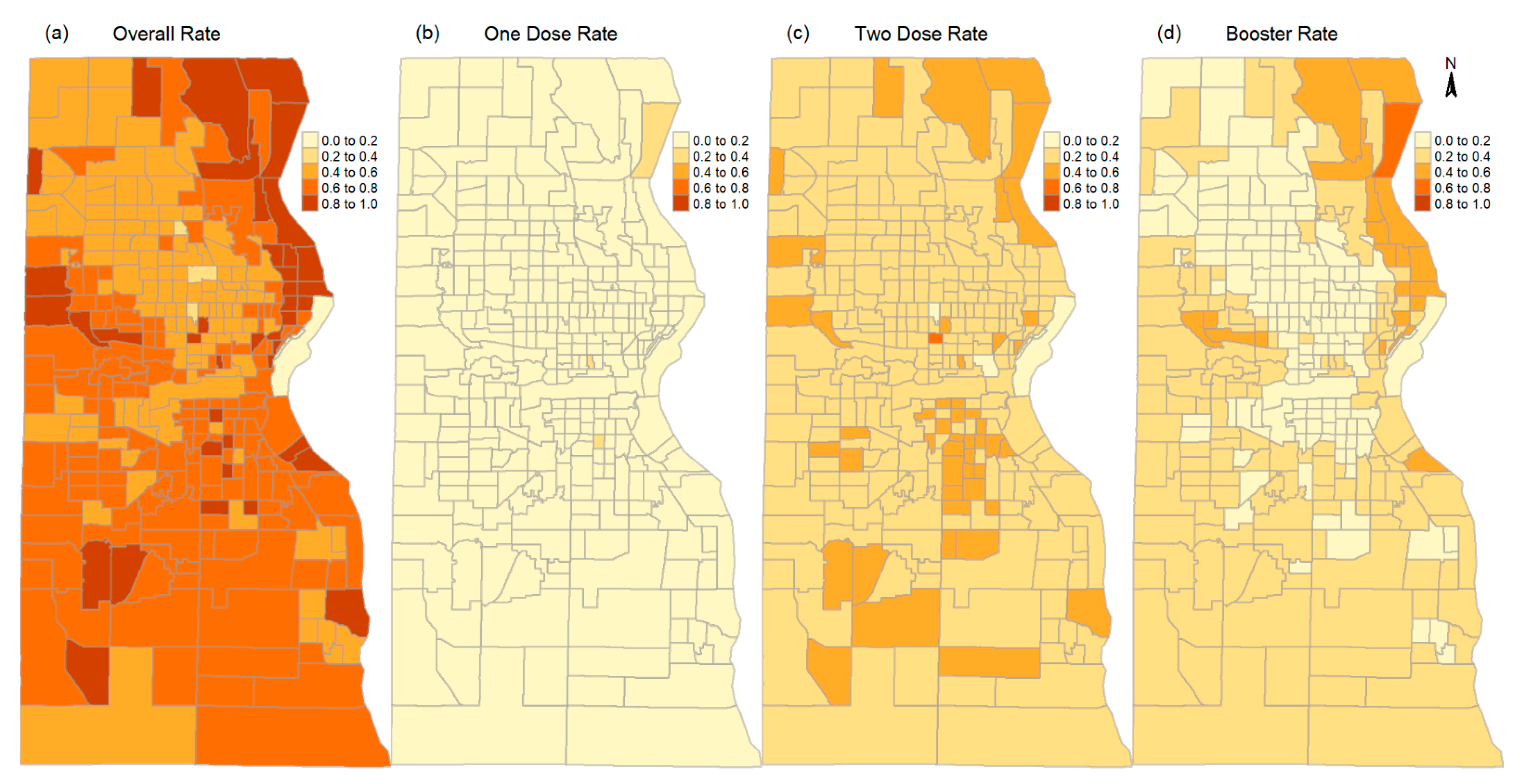
2.2. Vaccination Rates by Race/Ethnicity, Doses, and in Areas of Different Social Vulnerability
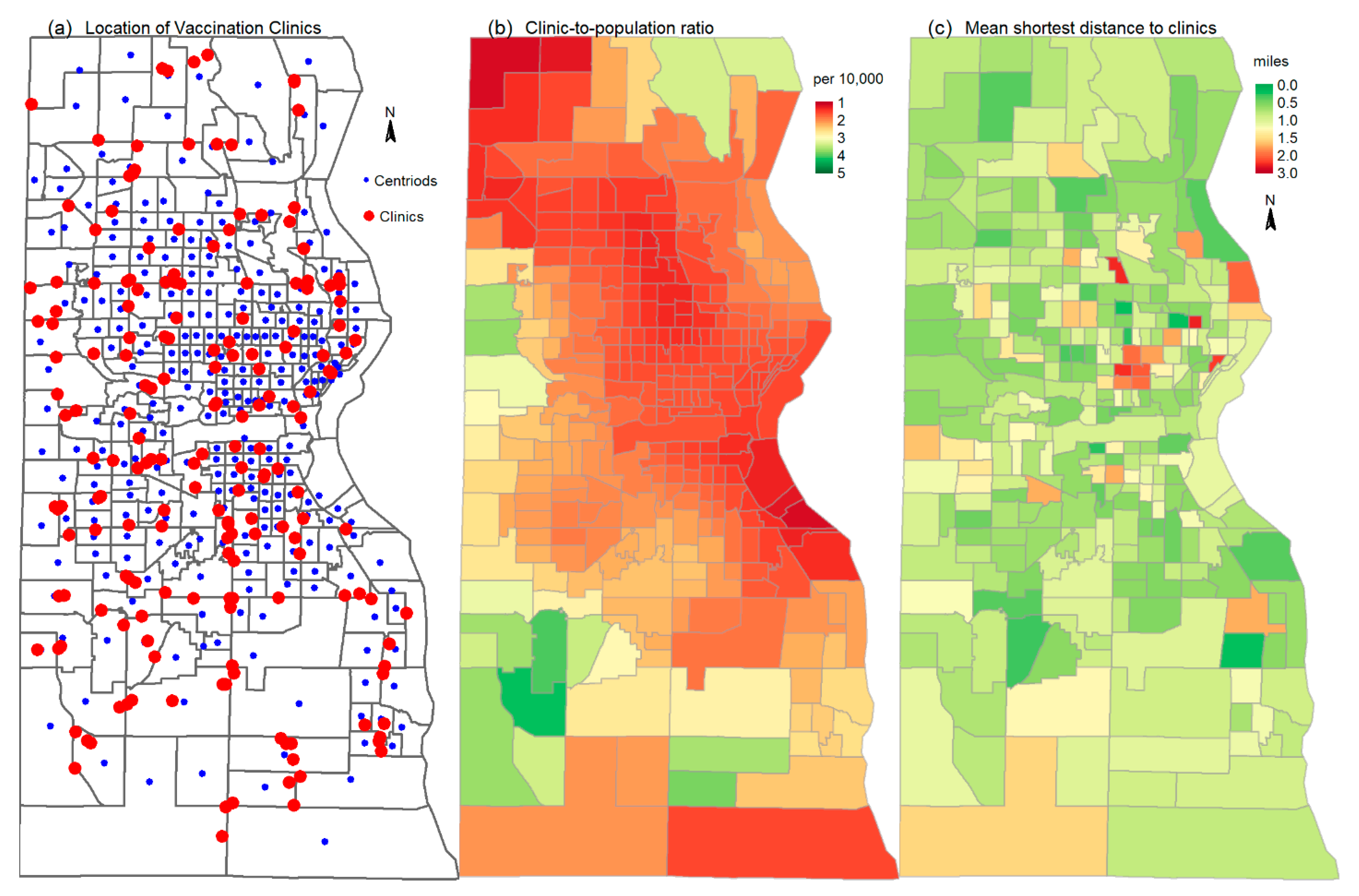
2.3. Spatial Accessibility to Vaccination Clinics
2.4. Modeling Vaccination Rates by Social Vulnerability and Spatial Accessibility
3. Results
3.1. Disparate Vaccination Rates by Race/Ethnicity, Doses, and Social Vulnerability
3.2. Effects of Social Vulnerability and Spatial Accessibility on Vaccination Rates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Y.; Li, M.; Rice, M.; Su, Y.; Yang, C. Phased implementation of COVID-19 vaccination: Rapid assessment of policy adoption, reach and effectiveness to protect the most vulnerable in the US. Int. J. Environ. Res. Public Health 2021, 18, 7665. [Google Scholar] [CrossRef]
- Shim, E. Projecting the impact of SARS-CoV-2 variants and the vaccination program on the fourth wave of the COVID-19 pandemic in South Korea. Int. J. Environ. Res. Public Health 2021, 18, 7578. [Google Scholar] [CrossRef]
- Sycinska-Dziarnowska, M.; Paradowska-Stankiewicz, I.; Woźniak, K. The global interest in vaccines and its prediction and perspectives in the era of COVID-19. Real-time surveillance using Google Trends. Int. J. Environ. Res. Public Health 2021, 18, 7841. [Google Scholar] [CrossRef]
- Lin, L.; Zhao, Y.; Chen, B.; He, D. Multiple COVID-19 waves and vaccination effectiveness in the united states. Int. J. Environ. Res. Public Health 2022, 19, 2282. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, A.; Lee, E.C.; Grigorescu, V.; Smith, S.R.; De Lew, N.; Sommers, B.D. Overview of Barriers and Facilitators in COVID-19 Vaccine Outreach; US Department of Health and Human Services: Washington, DC, USA, 2021.
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Campos-Mercade, P.; Meier, A.N.; Schneider, F.H.; Meier, S.; Pope, D.; Wengström, E. Monetary incentives increase COVID-19 vaccinations. Science 2021, 374, 879–882. [Google Scholar] [CrossRef]
- Khubchandani, J.; Macias, Y. COVID-19 vaccination hesitancy in Hispanics and African-Americans: A review and recommendations for practice. Brain Behav. Immun.-Health 2021, 15, 100277. [Google Scholar] [CrossRef]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J. Commun. Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Kreps, S.; Prasad, S.; Brownstein, J.S.; Hswen, Y.; Garibaldi, B.T.; Zhang, B.; Kriner, D.L. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw. Open 2020, 3, e2025594. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Dong, C.; Liang, Q.; Ji, T.; Gu, J.; Feng, J.; Shuai, M.; Zhang, X.; Zhao, R.; Gu, Z. Determinants of Vaccine Acceptance against COVID-19 in China: Perspectives on Knowledge and DrVac-COVID19S Scale. Int. J. Environ. Res. Public Health 2021, 18, 11192. [Google Scholar] [CrossRef] [PubMed]
- Barry, V.; Dasgupta, S.; Weller, D.L.; Kriss, J.L.; Cadwell, B.L.; Rose, C.; Pingali, C.; Musial, T.; Sharpe, J.D.; Flores, S.A.; et al. Patterns in COVID-19 Vaccination Coverage, by Social Vulnerability and Urbanicity—United States, December 14, 2020–May 1, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.C.; Young, S.G.; Pro, G.C. COVID-19 vaccination rates vary by community vulnerability: A county-level analysis. Vaccine 2021, 39, 4245–4249. [Google Scholar] [CrossRef] [PubMed]
- Cardona, S.; Felipe, N.; Fischer, K.; Sehgal, N.J.; Schwartz, B.E. Vaccination disparity: Quantifying racial inequity in COVID-19 vaccine administration in Maryland. J. Urban Health 2021, 98, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Murthy, B.P.; Sterrett, N.; Weller, D.; Zell, E.; Reynolds, L.; Toblin, R.L.; Murthy, N.; Kriss, J.; Rose, C.; Cadwell, B. Disparities in COVID-19 vaccination coverage between urban and rural counties—United States, December 14, 2020–April 10, 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 759. [Google Scholar] [CrossRef]
- Siegel, M.; Critchfield-Jain, I.; Boykin, M.; Owens, A.; Muratore, R.; Nunn, T.; Oh, J. Racial/ethnic disparities in state-level COVID-19 vaccination rates and their association with structural racism. J. Racial Ethn. Health Disparities 2021. [Google Scholar] [CrossRef]
- Sun, Y.; Monnat, S.M. Rural-urban and within-rural differences in COVID-19 vaccination rates. J. Rural. Health 2021, 38, 916–922. [Google Scholar] [CrossRef]
- Williams, N.; Tutrow, H.; Pina, P.; Belli, H.M.; Ogedegbe, G.; Schoenthaler, A. Assessment of racial and ethnic disparities in access to COVID-19 vaccination sites in Brooklyn, New York. JAMA Network Open 2021, 4, e2113937. [Google Scholar] [CrossRef]
- Bruckhaus, A.A.; Abedi, A.; Salehi, S.; Pickering, T.A.; Zhang, Y.; Martinez, A.; Lai, M.; Garner, R.; Duncan, D. COVID-19 Vaccination Dynamics in the US: Coverage Velocity and Carrying Capacity Based on Socio-demographic Vulnerability Indices in California. J. Immigr. Minor. Health 2022, 24, 18–30. [Google Scholar] [CrossRef]
- Hughes, M.M.; Wang, A.; Grossman, M.K.; Pun, E.; Whiteman, A.; Deng, L.; Hallisey, E.; Sharpe, J.D.; Ussery, E.N.; Stokley, S. County-level COVID-19 vaccination coverage and social vulnerability—United States, December 14, 2020–March 1, 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 431. [Google Scholar] [CrossRef]
- Cutter, S.L.; Boruff, B.J.; Shirley, W.L. Social vulnerability to environmental hazards. Soc. Sci. Q. 2003, 84, 242–261. [Google Scholar] [CrossRef]
- Flanagan, B.E.; Hallisey, E.J.; Adams, E.; Lavery, A. Measuring community vulnerability to natural and anthropogenic hazards: The Centers for Disease Control and Prevention’s Social Vulnerability Index. J. Environ. Health 2018, 80, 34. [Google Scholar] [PubMed]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Bartsch, S.M.; Taitel, M.S.; DePasse, J.V.; Cox, S.N.; Smith-Ray, R.L.; Wedlock, P.; Singh, T.G.; Carr, S.; Siegmund, S.S.; Lee, B.Y. Epidemiologic and economic impact of pharmacies as vaccination locations during an influenza epidemic. Vaccine 2018, 36, 7054–7063. [Google Scholar] [CrossRef]
- Kim, N.; Mountain, T.P. Role of non-traditional locations for seasonal flu vaccination: Empirical evidence and evaluation. Vaccine 2017, 35, 2943–2948. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.V. The State of Black Milwaukee in National Perspective: Racial Inequality in the Nation’s 50 Largest Metropolitan Areas. In 65 Charts and Tables. Center for Economic Development Publications. 2020. Available online: https://dc.uwm.edu/ced_pubs/56 (accessed on 18 August 2022).
- Jiang, B. Head/tail breaks: A new classification scheme for data with a heavy-tailed distribution. Prof. Geogr. 2013, 65, 482–494. [Google Scholar] [CrossRef]
- Jiang, B. A recursive definition of goodness of space for bridging the concepts of space and place for sustainability. Sustainability 2019, 11, 4091. [Google Scholar] [CrossRef]
- Jiang, B. Geospatial analysis requires a different way of thinking: The problem of spatial heterogeneity. GeoJournal 2015, 80, 1–13. [Google Scholar] [CrossRef]
- Ahmad, O.B.; Boschi-Pinto, C.; Lopez, A.D.; Murray, C.J.; Lozano, R.; Inoue, M. Age Standardization of Rates: A New WHO Standard; World Health Organization: Geneva, Switzerland, 2001; Volume 9, pp. 1–14. [Google Scholar]
- Kaissi, A.; Charland, T. The evolution of retail clinics in the United States, 2006–2012. Health Care Manag. 2013, 32, 336–342. [Google Scholar] [CrossRef]
- Duffy, C.; Newing, A.; Górska, J. Evaluating the geographical accessibility and equity of COVID-19 vaccination sites in england. Vaccines 2021, 10, 50. [Google Scholar] [CrossRef] [PubMed]
- Wan, N.; Zhan, F.B.; Zou, B.; Wilson, J.G. Spatial access to health care services and disparities in colorectal cancer stage at diagnosis in Texas. Prof. Geogr. 2013, 65, 527–541. [Google Scholar] [CrossRef]
- Chi, G.; Zhu, J. Spatial regression models for demographic analysis. Popul. Res. Policy Rev. 2008, 27, 17–42. [Google Scholar] [CrossRef]
- Elhorst, J.P. Applied spatial econometrics: Raising the bar. Spat. Econ. Anal. 2010, 5, 9–28. [Google Scholar] [CrossRef]
- Anselin, L. Spatial Econometrics: Methods and Models; Springer Science & Business Media: Cham, Switzerland, 1988; Volume 4. [Google Scholar]
- Berenbrok, L.A.; Tang, S.; Coley, K.C.; Boccuti, C.; Guo, J.; Essien, U.R.; Dickson, S.; Hernandez, I. Access to Potential COVID-19 Vaccine Administration Facilities: A Geographic Information Systems Analysis. Report. University of Pittsburgh School of Pharmacy. 2021. Available online: https://s8637.pcdn.co/wp-content/uploads/2021/02/Access-to-Potential-COVID-19-Vaccine-Administration-Facilities-2-2-2021.pdf (accessed on 18 August 2022).
| Eigen Value & Variance of the Principal Components | |||||
|---|---|---|---|---|---|
| Principal Components | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Eigen Value | 6.48 | 4.47 | 3.79 | 2.26 | 2.04 |
| Proportion Var | 0.26 | 0.18 | 0.15 | 0.09 | 0.08 |
| Cumulative Var | 0.26 | 0.44 | 0.59 | 0.68 | 0.76 |
| Variables and Their Loadings to the Principal Components | |||||
| people whose income is below poverty in the past 12 months (%) | 0.80 | 0.27 | 0.25 | 0.08 | 0.28 |
| 5+ years who speak English less than well (%) | 0.02 | 0.90 | 0.04 | 0.24 | −0.01 |
| 25+ years with less than high school education (%) | 0.40 | 0.77 | 0.34 | 0.05 | −0.04 |
| civilian noninstitutionalized population with disability (%) | 0.54 | 0.04 | 0.20 | −0.08 | −0.63 |
| median household income in past 12 months in 2019 ($) | 0.80 | 0.30 | 0.21 | 0.01 | −0.04 |
| unemployed civilian labor force (%) | 0.54 | 0.05 | 0.62 | −0.03 | −0.03 |
| renter occupied units (%) | 0.88 | 0.20 | −0.10 | 0.01 | 0.15 |
| multi-unit housing units (%) | 0.73 | 0.23 | −0.46 | 0.04 | 0.11 |
| mobile homes (%) | −0.02 | 0.04 | 0.01 | 0.16 | −0.24 |
| 16+ years workers without vehicle (%) | 0.80 | 0.03 | 0.14 | −0.06 | 0.20 |
| 16+ years workers who take public transit (%) | 0.74 | −0.04 | 0.30 | −0.07 | 0.10 |
| single parent households (%) | 0.42 | 0.20 | 0.82 | −0.02 | 0.05 |
| 3+ years enrolled in schools (%) | 0.30 | 0.10 | 0.20 | 0.17 | 0.78 |
| occupied housing units with more than one person per room (%) | 0.21 | 0.59 | 0.37 | 0.35 | 0.14 |
| population with no health insurance coverage (%) | 0.25 | 0.87 | 0.10 | −0.12 | 0.06 |
| households with no internet access (%) | 0.68 | 0.45 | 0.31 | −0.04 | −0.18 |
| people in female householder families with no health insurance (%) | 0.24 | 0.49 | 0.47 | −0.21 | −0.02 |
| population 65 years and older (%) | −0.33 | −0.34 | −0.29 | −0.01 | −0.62 |
| population 17 years and younger (%) | 0.03 | 0.32 | 0.87 | 0.06 | 0.02 |
| Hispanic population * (%) | −0.07 | 0.95 | −0.09 | −0.09 | 0.01 |
| non-Hispanic black population * (%) | 0.58 | −0.26 | 0.69 | −0.05 | 0.04 |
| Asian population * (%) | −0.02 | 0.01 | 0.02 | 0.98 | 0.02 |
| population of non-Hispanic other race * (%) | −0.08 | 0.00 | −0.09 | 0.97 | 0.02 |
| group quarter population * (%) | 0.23 | −0.14 | −0.43 | 0.06 | 0.59 |
| vacant housing units * (%) | 0.75 | −0.02 | 0.36 | −0.09 | 0.11 |
| Vaccination Rates (%) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Doses | One or More Doses | One Dose | Two Doses | Three or More Doses | |||||||||
| Areas | Whole County | High SVI Areas | Low SVI Areas | Whole County | High SVI Areas | Low SVI Areas | Whole County | High SVI Areas | Low SVI Areas | Whole County | High SVI Areas | Low SVI Areas | |
| Race | Blacks | 37 | 34 (29) | 43 (41) | 6 | 6 (6) | 6 (6) | 22 | 21 (18) | 25 (24) | 9 | 7 (5) | 12 (11) |
| Hispanics | 49 | 51 (47) | 47 (47) | 7 | 8 (8) | 6 (7) | 32 | 34 (32) | 28 (29) | 10 | 8 (7) | 13 (12) | |
| Other | 77 | 65 (53) | 82 (82) | 8 | 9 (7) | 7 (8) | 44 | 45 (39) | 40 (43) | 25 | 11 (7) | 36 (32) | |
| Whites | 60 | 50 (37) | 61 (61) | 5 | 6 (4) | 5 (5) | 26 | 26 (22) | 26 (26) | 29 | 18 (10) | 30 (30) | |
| Total population | 53 | 45 (40) | 60 (58) | 6 | 7 (6) | 5 (5) | 27 | 28 (26) | 27 (27) | 20 | 10 (7) | 28 (25) | |
| Dependent Variables | ||||||||
|---|---|---|---|---|---|---|---|---|
| OLS | Lag | OLS | Lag | OLS | Lag | OLS | Lag | |
| Overall social vulnerability index | −0.007 | −0.001 | 0.059 *** | 0.046 *** | 0.025 *** | 0.020 *** | −0.085 *** | −0.024 *** |
| Clinic-to-population ratio | 0.134 *** | 0.088 *** | 0.038 | 0.041 | 0.142 *** | 0.110 *** | 0.189 *** | 0.073 ** |
| Shortest travel distance | −0.021 | −0.024 | −0.050 | −0.050 | −0.038 | −0.035 | 0.015 | −0.009 |
| Adjusted/pseudo R2 | 0.093 | 0.254 | 0.126 | 0.178 | 0.096 | 0.175 | 0.295 | 0.623 |
| ρ | 0.489 *** | 0.291 *** | 0.344 *** | 0.745 *** | ||||
| PC1 (SES) | −0.106 *** | −0.089 *** | 0.076 *** | 0.061 *** | −0.038 *** | −0.035 *** | −0.287 *** | −0.213 *** |
| PC2 (Hispanics) | 0.022 * | 0.016 | 0.105 *** | 0.081 *** | 0.085 *** | 0.078 *** | −0.117 *** | −0.080 *** |
| PC3 (Blacks) | −0.073 *** | −0.055 *** | 0.067 *** | 0.059 *** | −0.007 | −0.006 | −0.225 *** | −0.147 *** |
| Clinic-to-population ratio | 0.020 | 0.016 | 0.052 | 0.052 | 0.076 *** | 0.072 *** | −0.048 | −0.053 |
| Shortest travel distance | −0.004 | −0.009 | −0.034 | −0.038 | −0.017 | −0.018 | 0.023 | 0.010 |
| Adjusted/pseudo R2 | 0.295 | 0.328 | 0.145 | 0.187 | 0.212 | 0.228 | 0.667 | 0.714 |
| ρ | 0.228 *** | 0.246 *** | 0.082 | 0.384 *** | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, Z.; Jiang, B. Effects of Social Vulnerability and Spatial Accessibility on COVID-19 Vaccination Coverage: A Census-Tract Level Study in Milwaukee County, USA. Int. J. Environ. Res. Public Health 2022, 19, 12304. https://doi.org/10.3390/ijerph191912304
Xu Z, Jiang B. Effects of Social Vulnerability and Spatial Accessibility on COVID-19 Vaccination Coverage: A Census-Tract Level Study in Milwaukee County, USA. International Journal of Environmental Research and Public Health. 2022; 19(19):12304. https://doi.org/10.3390/ijerph191912304
Chicago/Turabian StyleXu, Zengwang, and Bin Jiang. 2022. "Effects of Social Vulnerability and Spatial Accessibility on COVID-19 Vaccination Coverage: A Census-Tract Level Study in Milwaukee County, USA" International Journal of Environmental Research and Public Health 19, no. 19: 12304. https://doi.org/10.3390/ijerph191912304






