Oral Health in 12- and 15-Year-Old Children in Serbia: A National Pathfinder Study
Abstract
:1. Introduction
2. Materials and Methods
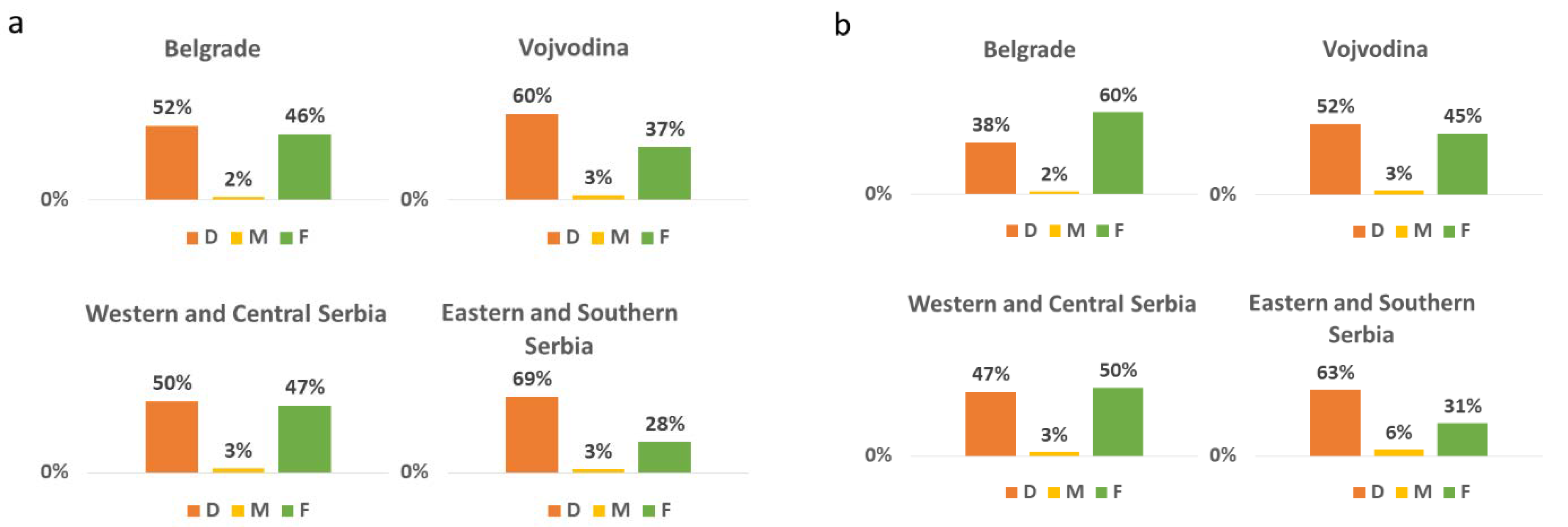
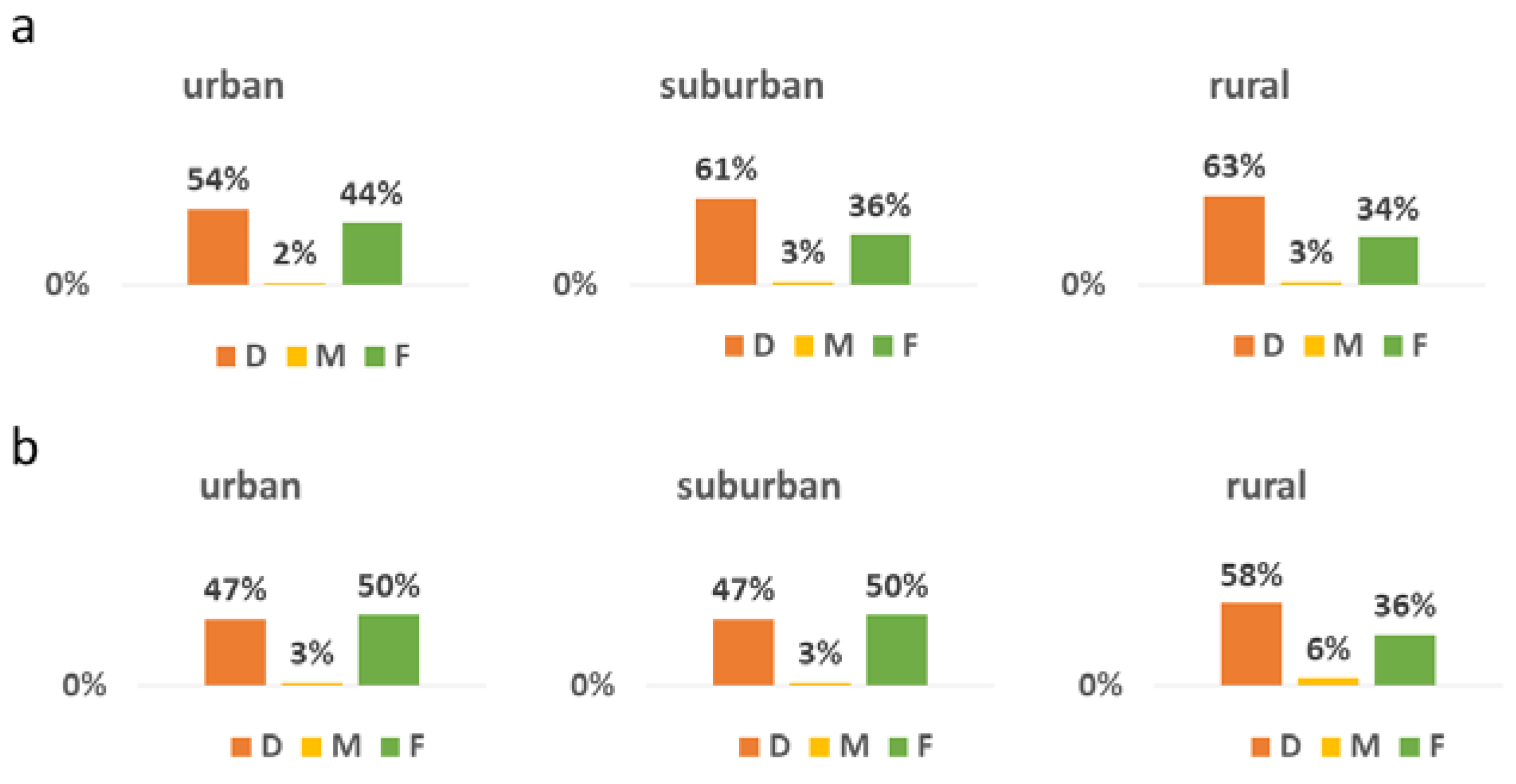
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Statistical Office of the Republic of Serbia. Municipalities and Regions of the Republic of Serbia, 2020; Statistical Office of the Republic of Serbia: Belgrade, Serbia, 2020. Available online: https://publikacije.stat.gov.rs/G2020/PdfE/G202013047.pdf (accessed on 20 July 2020).
- Carevic, M.; Vulovic, M. National program for prevention of oral diseases on caries distribution in population of Serbia 1996–2001. In Scientific Thought and Clinical Practice—10 Years of Balkan Stomatological Society; Markovic, D., Ed.; Faculty of Dentistry: Belgrade, Serbia, 2005; pp. 119–125. [Google Scholar]
- Vrbic, V.; Vulović, M.; Rajić, Z.; Topić, B.; Tatić, E.; Malić, M.; Milić, D.; Aurer-Kozelj, J.; Neceva, L.; Redzepagić, S. Oral health in SFR Yugoslavia in 1986. Community Dent. Oral. Epidemiol. 1988, 16, 286–288. [Google Scholar] [CrossRef] [PubMed]
- Government of Serbia, Ministry of Health. Policy of Healthcare Rights under Compulsory National Health Insurance Fund, Including Scope and Funding of Provision of Health Care Services for 2020. Službeni Glasnik RS 25/19. Available online: https://www.rfzo.rs/download/pravilnici/obim-sadrzaj/sadrzaj%20i%20obim%20od%2020.06.2020.godine.pdf (accessed on 10 June 2020). (In Serbian).
- Government of Serbia, Ministry of Health. National Program for Prevention of Oral Diseases in Republic of Serbia. Službeni Glasnik RS 22/2009. Available online: http://demo.paragraf.rs/demo/combined/Old/t/t2009_04/t04_0044.htm (accessed on 17 June 2017). (In Serbian).
- World Health Organization. Oral Health Surveys. Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Pitts, N. “ICDAS”—An international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent. Health 2004, 21, 193–198. [Google Scholar] [PubMed]
- Monse, B.; Heinrich-Weltzien, R.; Benzian, H.; Holmgren, C.; van Palenstein Helderman, W. PUFA—An index of clinical consequences of untreated dental caries. Community Dent. Oral. Epidemiol. 2010, 38, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Vernazza, C.R.; Rolland, S.L.; Chadwick, B.; Pitts, N. Caries experience, the caries burden and associated factors in children in England, Wales and Northern Ireland 2013. Br. Dent. J. 2016, 221, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Silness, J.; Loe, H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol. Scand. 1964, 22, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, S.E.; Allison, P.J. A Canadian national oral health survey—Coming soon! Can. J. Dent. Hyg. 2022, 56, 3–6. [Google Scholar]
- Zhu, L.; Petersen, P.E.; Wang, H.Y.; Bian, J.Y.; Zhang, B.X. Oral health knowledge, attitudes and behaviour of children and adolescents in China. Int. Dent. J. 2003, 53, 289–298. [Google Scholar] [CrossRef]
- Bombert, F.; Manso, A.C.; Sousa Ferreira, C.; Nogueira, P.; Nunes, C. Sociodemographic factors associated with oral health in 12-year-old adolescents: Hygiene behaviours and health appointments. A cross-sectional national study in Portugal. Int. Dent. J. 2018, 68, 327–335. [Google Scholar] [CrossRef]
- Hall-Scullin, E.; Goldthorpe, J.; Milsom, K.; Tickle, M. A qualitative study of the views of adolescents on their caries risk and prevention behaviours. BMC Oral Health 2015, 15, 141. [Google Scholar] [CrossRef]
- Rouxel, P.; Chandola, T. Socioeconomic and ethnic inequalities in oral health among children and adolescents living in England, Wales and Northern Ireland. Community Dent. Oral Epidemiol. 2018, 46, 426–434. [Google Scholar] [CrossRef]
- Oulis, C.J.; Berdouses, E.D.; Mamai-Homata, E.; Polychronopoulou, A. Prevalence of sealants in relation to dental caries on the permanent molars of 12 and 15-year-old Greek adolescents. A national pathfinder survey. BMC Public Health 2011, 11, 100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jablonski-Momeni, A.; Winter, J.; Petrakakis, P.; Schmidt-Schäfer, S. Caries prevalence (ICDAS) in 12-year-olds from low caries prevalence areas and association with independent variables. Int. J. Paediatr. Dent. 2014, 24, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Berna, K.; Ece, E.; Nese, G. Clinical success of fluoride-releasing fissure sealant in permanent first molars: 5-year retrospective atudy. Balk. J. Dent. Med. 2022. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global burden of untreated caries: A systematic review and metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Campus, G.; Solinas, G.; Cagetti, M.G.; Senna, A.; Minelli, L.; Majori, S.; Montagna, M.T.; Reali, D.; Castiglia, P.; Strohmenger, L. National Pathfinder survey of 12-year-old Children’s Oral Health in Italy. Caries Res. 2007, 41, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Jordan, R.A.; Bodechtel, C.; Hertrampf, K.; Hoffmann, T.; Kocher, T.; Nitschke, I.; Schiffner, U.; Stark, H.; Zimmer, S.; Micheelis, W.; et al. The Fifth German Oral Health Study (Fünfte Deutsche Mundgesundheitsstudie, DMS V)—Rationale, design, and methods. BMC Oral Health 2014, 14, 161. [Google Scholar] [CrossRef] [PubMed]
- El-Nadeef, M.A.; Al Hussani, E.; Hassab, H.; Arab, I.A. National survey of the oral health of 12- and 15-year-old schoolchildren in the United Arab Emirates. East Mediterr. Health J. 2009, 15, 993–1004. [Google Scholar] [CrossRef]
- Besseling, S.; Ngonephady, S.; van Wijk, A.J. Pilot survey on dental health in 5–12-year-old school children in Laos. J. Investig. Clin. Dent. 2013, 4, 44–48. [Google Scholar] [CrossRef]
- Mafuvadze, B.T.; Mahachi, L.; Mafuvadze, B. Dental caries and oral health practice among 12 year old school children from low socio-economic status background in Zimbabwe. Pan. Afr. Med. J. 2013, 14, 164. [Google Scholar] [CrossRef]
- Monse, B.; Benzian, H.; Araojo, J.; Holmgren, C.; van Palenstein Helderman, W.; Naliponguit, E.C.; Heinrich-Weltzien, R. A silent public health crisis: Untreated caries and dental infections among 6- and 12-year-old children in the Philippine National Oral Health Survey 2006. Asia Pac. J. Public Health 2015, 27, NP2316–NP2325. [Google Scholar] [CrossRef]
- Zhang, S.; Xu, B.; Liu, J.; Lo, E.C.; Chu, C.H. Dental and periodontal status of 12-year-old Dai school children in Yunnan Province, China: A cross-sectional study. BMC Oral Health 2015, 15, 117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elias-Boneta, A.R.; Toro, M.J.; Rivas-Tumanyan, S.; Murillo, M.; Orraca, L.; Encarnacion, A.; Cernigliaro, D.; Toro-Vizcarrondo, C.; Psoter, W.J. Persistent oral health disparity in 12-year-old Hispanics: A cross-sectional study. BMC Oral Health 2016, 16, 10. [Google Scholar] [CrossRef]
- Rybarczyk-Townsend, E.; Hilt, A.; Szczepanska, J. Dentition status in 12-year-old children in Lodzkie province in 2014. Przegl. Epidemiol. 2016, 70, 47–51. [Google Scholar] [PubMed]
- Yin, W.; Yang, Y.M.; Chen, H.; Li, X.; Wang, Z.; Cheng, L.; Yin, Q.D.; Fang, H.Z.; Fei, W.; Mi, F.L.; et al. Oral health status in Sichuan Province: Findings from the oral health survey of Sichuan, 2015–2016. Int. J. Oral Sci. 2017, 9, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Bilder, L.; Stepco, E.; Uncuta, D.; Aizenbud, D.; Machtei, E.; Bilder, A.; Sgan-Cohen, H.D. The pathfinder study among schoolchildren in the Republic of Moldova: Dental caries experience. Int. Dent. J. 2018, 68, 344–347. [Google Scholar] [CrossRef]
- Karki, S.; Laitala, M.L.; Humagain, M.; Seppänen, M.; Päkkila, J.; Anttonen, V. Oral health status associated with sociodemographic factors of Nepalese schoolchildren: A population-based study. Int. Dent. J. 2018, 68, 348–358. [Google Scholar] [CrossRef]
- Ballouk, M.A.; Dashash, M. Caries prevalence and dental health of 8-12 year-old children in Damascus city in Syria during the Syrian Crisis; a cross-sectional epidemiological oral health survey. BMC Oral Health 2019, 19, 16. [Google Scholar] [CrossRef]
- Du, A.; Zhang, H.; Chen, C.; Zhang, F.; Liu, X.; Zhang, Z.; Wang, R. Oral health of 12-year-old children in Jilin province, China: A population-based epidemiological survey. Medicine 2019, 98, e18463. [Google Scholar] [CrossRef]
- Ghotane, S.G.; Challacombe, S.J.; Don-Davis, P.; Kamara, D.; Gallagher, J.E. Unmet need in Sierra Leone: A national oral health survey of schoolchildren. BDJ Open 2022, 8, 16. [Google Scholar] [CrossRef]
- Markovic, N.; Muratbegovic, A.; Kobaslija, S.; Bajric, A.; Huseinbegovic, A.; Selimovic-Dragas, M. Caries prevalence in Bosnia and Herzegovina schoolchildren—Findings of first national survey. Stomatol. Vjesn. 2013, 2, 9–15. [Google Scholar]
- Ondine Lucaciu, P.; Mester, A.; Constantin, I.; Orban, N.; Cosma, L.; Candrea, S.; Sava-Rosianu, R.; Mesaros, A.S. A WHO pathfinder survey of dental caries in 6 and 12-year old Transylvanian children and the possible correlation with their family background, oral-health behavior, and the intake of sweets. Int. J. Environ. Res. Public Health 2020, 17, 4180. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. Inequality in oral health: The social context for oral health. In Community Oral Health; Harris, R., Pine, C., Eds.; Quintessence Publ.: Copenhagen, Danemark, 2005. [Google Scholar]
- Ha, D.H.; Crocombe, L.A.; Mejia, G.C. Clinical oral health of Australia’s rural children in a sample attending school dental services. Aust. J. Rural Health 2014, 22, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Shen, A.; Zeng, X.; Cheng, M.; Tai, B.; Huang, R.; Bernabé, E. Inequalities in dental caries among 12-year-old Chinese children. J. Public Health Dent. 2015, 75, 210–217. [Google Scholar] [CrossRef]
- Quan, J.K.; Wang, X.Z.; Sun, X.Y.; Yuan, C.; Liu, X.N.; Wang, X.; Feng, X.P.; Tai, B.J.; Hu, Y.; Lin, H.C.; et al. Permanent Teeth Caries Status of 12- to 15-year-olds in China: Findings from the 4th National Oral Health Survey. Chin. J. Dent. Res. 2018, 21, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Bonev, B.; Avramova, N.; Yaneva, K.; Filchev, D. Dental caries and associated socio-demographic factors in adult people in Bulgaria. Balk. J. Dent. Med. 2015, 19, 33–37. [Google Scholar] [CrossRef]
- Statistical Office of the Republic of Serbia. Estimates of Population by Age and Sex; Statistical Office of the Republic of Serbia: Belgrade, Serbia, 2019. Available online: https://data.stat.gov.rs/Home/Result/18010403?languageCode=en-US (accessed on 20 July 2020).
- Institute of Public Health of Serbia “Dr. Milan Jovanovic Batut”. Health Statistical Yearbook of Republic of Serbia 2019; Institute of Public Health of Serbia “Dr. Milan Jovanovic Batut”: Belgrade, Serbia, 2020; Available online: http://www.batut.org.rs/download/publikacije/pub2019a.pdf (accessed on 7 December 2020).
- Vadiakas, G.; Oulis, C.J.; Tsinidou, K.; Mamai-Homata, E.; Polychronopoulou, A. Oral hygiene and periodontal status of 12 and 15-year-old Greek adolescents. A national pathfinder survey. Eur. Arch. Paediatr. Dent. 2012, 13, 11–20. [Google Scholar] [CrossRef]
- Zumpe, L.; Bensel, T.; Wienke, A.; Mtaya-Mlangwa, M.; Hey, J. The Oral Health Situation of 12-Year-Old School Children in the Rural Region of Ilembula in Southwestern Tanzania: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 12237. [Google Scholar] [CrossRef] [PubMed]
- Elias-Boneta, A.R.; Ramirez, K.; Rivas-Tumanyan, S.; Murillo, M.; Toro, M.J. Prevalence of gingivitis and calculus in 12-year-old Puerto Ricans: A cross-sectional study. BMC Oral Health 2018, 18, 13. [Google Scholar] [CrossRef]
- Leroy, R.; Eaton, K.A.; Savage, A. Methodological issues in epidemiological studies of periodontitis—How can it be improved? BMC Oral Health 2010, 10, 8. [Google Scholar] [CrossRef]
- Martignon, S.; Bartlett, D.; Manton, D.J.; Martinez-Mier, E.A.; Splieth, C.; Avila, V. Epidemiology of Erosive Tooth Wear, Dental Fluorosis and Molar Incisor Hypomineralization in the American Continent. Caries Res. 2021, 55, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Shokri, A.; Poorolajal, J.; Khajeh, S.; Faramarzi, F.; Kahnamoui, H.M. Prevalence of dental anomalies among 7- to 35-year-old people in Hamadan, Iran in 2012–2013 as observed using panoramic radiographs. Imaging Sci. Dent. 2014, 44, 7–13. [Google Scholar] [CrossRef]
- Bilge, N.H.; Yeşiltepe, S.; Törenek Ağırman, K.; Çağlayan, F.; Bilge, O.M. Investigation of prevalence of dental anomalies by using digital panoramic radiographs. Folia Morphol. 2018, 77, 323–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whelton, H.P.; Ketley, C.E.; McSweeney, F.; O’Mullane, D.M. A review of fluorosis in the European Union: Prevalence, risk factors and aesthetic issues. Community Dent. Oral Epidemiol. 2004, 32 (Suppl. 1), 9–18. [Google Scholar] [CrossRef] [PubMed]
- Bilder, L.; Margvelashvili, V.; Sgan-Cohen, H.; Kalandadze, M.; Levin, L.; Ivanishvili, R.; Machtei, E.E. Traumatic dental injuries among 12- and 15-year-old adolescents in Georgia: Results of the pathfinder study. Dent. Traumatol. 2016, 32, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Eltair, M.; Pitchika, V.; Standl, M.; Lang, T.; Krämer, N.; Hickel, R.; Kühnisch, J. Prevalence of traumatic crown injuries in German adolescents. Clin. Oral Investig. 2020, 24, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Schlueter, N.; Luka, B. Erosive tooth wear—A review on global prevalence and on its prevalence in risk groups. Br. Dent. J. 2018, 224, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Salas, M.M.; Nascimento, G.G.; Huysmans, M.C.; Demarco, F.F. Estimated prevalence of erosive tooth wear in permanent teeth of children and adolescents: An epidemiological systematic review and meta-regression analysis. J. Dent. 2015, 43, 42–50. [Google Scholar] [CrossRef]
- Levin, L.; Day, P.F.; Hicks, L.; O’Connell, A.; Fouad, A.F.; Bourguignon, C.; Abbott, P.V. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: General introduction. Dent. Traumatol. 2020, 36, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Enzo, B. Malocclusion in orthodontics and oral health: Adopted by the General Assembly: September 2019, San Francisco, United States of America. Int. Dent. J. 2020, 70, 11–12. [Google Scholar] [CrossRef] [PubMed]
- Adanero, A.; Baquero, L.; Berasategui, M.; Velayos, L.; Espí, M.; Piñeiro, M.; Miegimolle, M. Oral health status of 6- to 12-year-old children in Madrid, Spain: A cross-sectional study. Heliyon 2022, 8, e09557. [Google Scholar] [CrossRef] [PubMed]
- Markovic, E.; Vukovic, A.; Peric, T.; Kuzmanovic-Pficer, J.; Petrovic, B. Prevalence of developmental dental anomalies in Serbian orthodontic patients. Srp. Arh. Celok. Lek. 2020, 148, 17–23. [Google Scholar] [CrossRef]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dental. Press. J. Orthod. 2018, 23, 40.e1–40.e10. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; Vena, F.; Negri, P.; Pagano, S.; Barilotti, C.; Paglia, L.; Colombo, S.; Orso, M.; Cianetti, S. Worldwide prevalence of malocclusion in the different stages of dentition: A systematic review and meta-analysis. Eur. J. Paediatr. Dent. 2020, 21, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Mylonopoulou, I.-M.; Sifakakis, I.; Berdouses, E.; Kavvadia, K.; Arapostathis, K.; Oulis, C.J. Orthodontic Status and Orthodontic Treatment Need of 12- and 15-Year-Old Greek Adolescents: A National Pathfinder Survey. Int. J. Environ. Res. Public Health 2021, 18, 11790. [Google Scholar] [CrossRef] [PubMed]
- De Ridder, L.; Aleksieva, A.; Willems, G.; Declerck, D.; Cadenas de Llano-Pérula, M. Prevalence of Orthodontic Malocclusions in Healthy Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7446. [Google Scholar] [CrossRef]
| No. of Healthy Teeth | D | M | F | DMFT | Gingival Bleeding | PI | ||
|---|---|---|---|---|---|---|---|---|
| LEVEL 1 | ||||||||
| Principal investigator 1–3 | median | 21 | 4 | 0 | 3 | 7 | 0.96 | 1.25 |
| min | 20 | 4 | 0 | 3 | 7 | 0.93 | 1.21 | |
| max | 21 | 5 | 0 | 3 | 8 | 1.00 | 1.25 | |
| LEVEL 2 | ||||||||
| Principal investigator 1 with examiners 4–14 | median | 14 | 14 | 0 | 0 | 14 | 0.64 | 1.39 |
| min | 13 | 14 | 0 | 0 | 14 | 0.57 | 1.21 | |
| max | 14 | 15 | 0 | 0 | 15 | 0.71 | 1.46 | |
| Principal investigator 2 with examiners 15–25 | median | 17.5 | 9.5 | 0 | 1 | 10.5 | 0.96 | 1.93 |
| min | 17 | 8 | 0 | 1 | 9 | 0.93 | 1.86 | |
| max | 19 | 10 | 0 | 1 | 11 | 0.96 | 2.00 | |
| Principal investigator 3 with examiners 26–36 | median | 17 | 9 | 0 | 2 | 11 | 0.64 | 1.18 |
| min | 17 | 9 | 0 | 2 | 11 | 0.43 | 1.14 | |
| max | 17 | 9 | 0 | 2 | 11 | 0.64 | 1.29 | |
| Overall | Dental Status | Gingival Bleeding | PI | |
|---|---|---|---|---|
| LEVEL 1 | 0.88 (0.84–0.93) | 0.74 (0.63–0.91) | No computation | 1.00 |
| LEVEL 2 | 0.91 (0.89–0.96) | 0.94 (0.91–1.00) | 0.82 (0.70–0.91) | 0.79 (0.76–0.96) |
| No. of Participants | Caries-Free | Severe Caries | DMFT | DMFS | |
|---|---|---|---|---|---|
| Gender | |||||
| Boys | 613 | 41% a | 45% | 2.14 ± 2.68 (1.00) A | 3.00 ± 4.58 (1.00) I |
| Girls | 587 | 31% a | 43% | 2.51 ± 2.69 (2.00) A | 3.34 ± 4.37 (2.00) I |
| Area | |||||
| Urban | 603 | 41% b | 39% h | 2.01 ± 2.50 (1.00) B | 2.58 ± 3.65 (1.00) J |
| Suburban | 247 | 23% b,c | 55% h | 3.06 ± 2.81 (3.00) B,C | 4.47 ± 5.04 (3.00) J,K |
| Rural | 350 | 36% c | 45% | 2.39 ± 2.39 (2.00) C | 3.42 ± 5.45 (1.00) K |
| Administrative region | |||||
| City of Belgrade | 250 | 50% d,e,f | 36% i | 1.64 ± 2.35 (0.50) D,E,F | 2.24 ± 4.04 (1.00) L,M,N |
| Vojvodina | 300 | 35% e | 46% | 2.36 ± 2.74 (2.00) D | 3.17 ± 5.01 (1.00) L,O |
| Central and Western Serbia | 338 | 36% d | 37% j | 2.26 ± 2.61 (2.00) E | 3.06 ± 3.94 (2.00) M |
| Southern and Eastern Serbia | 312 | 28% f | 52% i,j | 2.62 ± 2.86 (2.00) F | 3.68 ± 4.42 N,O |
| Parental employment | |||||
| Both parents employed | 938 | 36% g | 42% | 2.32 ± 2.67 (2.00) G | 3.17 ± 4.35 (2.00) P |
| One parent employed | 225 | 25% g | 51% | 2.85 ± 2.97 (2.00) G,H | 3.99 ± 4.62 (2.00) P,Q |
| Both parents unemployed | 37 | 40% | 28% | 1.37 ± 1.54 (1.00) H | 2.43 ± 3.84 (1.00) Q |
| No. of Participants | Caries-Free | Severe Caries | DMFT | DMFS | |
|---|---|---|---|---|---|
| Gender | |||||
| Boys | 611 | 23% | 63% | 3.95 ± 3.80 (3.00) | 5.79 ± 6.39 (4.00) |
| Girls | 609 | 20% | 59% | 4.24 ± 3.81 (4.00) | 5.87 ± 6.46 (4.00) |
| Area | |||||
| Urban | 600 | 29% a,b | 54% h,i | 3.41 ± 3.70 (2.00) A,B | 4.60 ± 5.59 (3.00) H,I |
| Suburban | 263 | 15% a | 65% h | 4.62 ± 3.58 (4.00) A | 6.36 ± 5.96 (5.00) H |
| Rural | 357 | 17% b | 65% i | 4.58 ± 4.01 (4.00) B | 7.10 ± 7.58 (5.00) I |
| Administrative region | |||||
| City of Belgrade | 250 | 38% c,d,e | 53% j | 2.95 ± 3.48 (2.00) C,D,E | 3.73 ± 4.79 (2.00) J,K,L |
| Vojvodina | 312 | 19% c | 60% | 4.35 ± 4.03 (4.00) C | 6.21 ± 6.87 (4.00) J |
| Central and Western Serbia | 358 | 18% d | 62% | 4.39 ± 3.73 (4.00) D | 6.21 ± 6.25 (4.00) K |
| Southern and Eastern Serbia | 300 | 19% e | 66% j | 4.05 ± 3.68 (3.00) E | 6.23 ± 6.88 (4.00) L |
| Parental employment | |||||
| Both parents employed | 869 | 24% f | 58% k | 3.80 ± 3.67 (3.00) F | 5.25 ± 5.92 (4.00) M |
| One parent employed | 287 | 14% f,g | 67% k | 4.67 ± 3.78 (4.00) F,G | 7.35 ± 7.25 (6.00) M,N |
| Both parents unemployed | 64 | 28% g | 57% | 3.88 ± 4.43 (3.00) G | 5.67 ± 7.39 (3.50) N |
| 12-Year-Olds | 15-Year-Olds | |||||
|---|---|---|---|---|---|---|
| Gingivitis (%) | PI | Gingivitis (%) | PI | |||
| PI = 0 (%) | Mean ± SD (Median) | PI = 0 (%) | Mean ± SD (Median) | |||
| Gender | ||||||
| Boys | 27% | 35% | 0.73 ± 0.78 (0.50) | 19% | 32% E | 0.69 ± 0.72 (0.50) H |
| Girls | 24% | 38% | 0.69 ± 0.78 (0.38) | 16% | 41% E | 0.54 ± 0.70 (0.29) H |
| Area | ||||||
| Urban | 26% | 40% d | 0.68 ± 0.78 (0.33) k | 20% A | 36% | 0.63 ± 0.71 (0.36) |
| Suburban | 24% | 36% | 0.68 ± 0.74 (0.43) | 8% A,B | 40% | 0.53 ± 0.67 (0.29) I |
| Rural | 28% | 28% d | 0.81 ± 0.83 (0.57) k | 22% B | 35% | 0.67 ± 0.76 (0.43) I |
| Administrative region | ||||||
| City of Belgrade | 29% a | 50% e,f | 0.50 ± 0.69 (0.06) l,m,n | 27% C,D | 44% F | 0.47 ± 0.63 (0.21) J,K |
| Vojvodina | 31%c | 26% e,g,h | 0.78 ± 0.82 (0.46) l,o | 17% D | 32% F | 0.68 ± 0.75 (0.43) J,L |
| Central and Western Serbia | 18% a,b,c | 41% f,g | 0.88 ± 0.87 (1.00) m,p | 13% C | 36% | 0.71 ± 0.80 (0.43) K,M |
| Southern and Eastern Serbia | 24% b | 36% h | 0.61 ± 0.64 (0.50) n,o,p | 20% | 38% | 0.47 ± 0.54 (0.29) L,M |
| Parental employment | ||||||
| Both parents employed | 24% | 43% i,j | 0.66 ± 0.77 (0.36) q,r | 17% | 37% G | 0.57 ± 0.70 (0.29) N |
| One parent employed | 25% | 26% i | 0.96 ± 0.84 (1.00) q | 21% | 29% G | 0.72 ± 0.71 (0.57) N |
| Both parents unemployed | 33% | 20% j | 1.03 ± 0.71 (1.00) r | 24% | 40% | 0.59 ± 0.68 (0.41) |
| 12-Year-Olds | 15-Year-Olds | |
|---|---|---|
| Class I molar relationship | 87% | 90% |
| Overjet > 4 mm | 7% | 5% |
| Anterior crossbite | 4% | 3% |
| Deep bite | 20% | 19% |
| Anterior open bite | 1% | 2% |
| Posterior crossbite | 10% | 9% |
| Spacing | 7% | 6% |
| Crowding | 25% | 28% |
| Mouth breathing | 6% | 4% |
| Tongue thrust and dysfunctions | 8% | 5% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peric, T.; Campus, G.; Markovic, E.; Petrovic, B.; Soldatovic, I.; Vukovic, A.; Kilibarda, B.; Vulovic, J.; Markovic, J.; Markovic, D. Oral Health in 12- and 15-Year-Old Children in Serbia: A National Pathfinder Study. Int. J. Environ. Res. Public Health 2022, 19, 12269. https://doi.org/10.3390/ijerph191912269
Peric T, Campus G, Markovic E, Petrovic B, Soldatovic I, Vukovic A, Kilibarda B, Vulovic J, Markovic J, Markovic D. Oral Health in 12- and 15-Year-Old Children in Serbia: A National Pathfinder Study. International Journal of Environmental Research and Public Health. 2022; 19(19):12269. https://doi.org/10.3390/ijerph191912269
Chicago/Turabian StylePeric, Tamara, Guglielmo Campus, Evgenija Markovic, Bojan Petrovic, Ivan Soldatovic, Ana Vukovic, Biljana Kilibarda, Jelena Vulovic, Jovan Markovic, and Dejan Markovic. 2022. "Oral Health in 12- and 15-Year-Old Children in Serbia: A National Pathfinder Study" International Journal of Environmental Research and Public Health 19, no. 19: 12269. https://doi.org/10.3390/ijerph191912269
APA StylePeric, T., Campus, G., Markovic, E., Petrovic, B., Soldatovic, I., Vukovic, A., Kilibarda, B., Vulovic, J., Markovic, J., & Markovic, D. (2022). Oral Health in 12- and 15-Year-Old Children in Serbia: A National Pathfinder Study. International Journal of Environmental Research and Public Health, 19(19), 12269. https://doi.org/10.3390/ijerph191912269








