Factors Associated with Improved Knowledge of Metabolic Syndrome in Female Market Traders
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Subject Characteristics
3.2. Presence of Cardiometabolic Disease Risk Factors
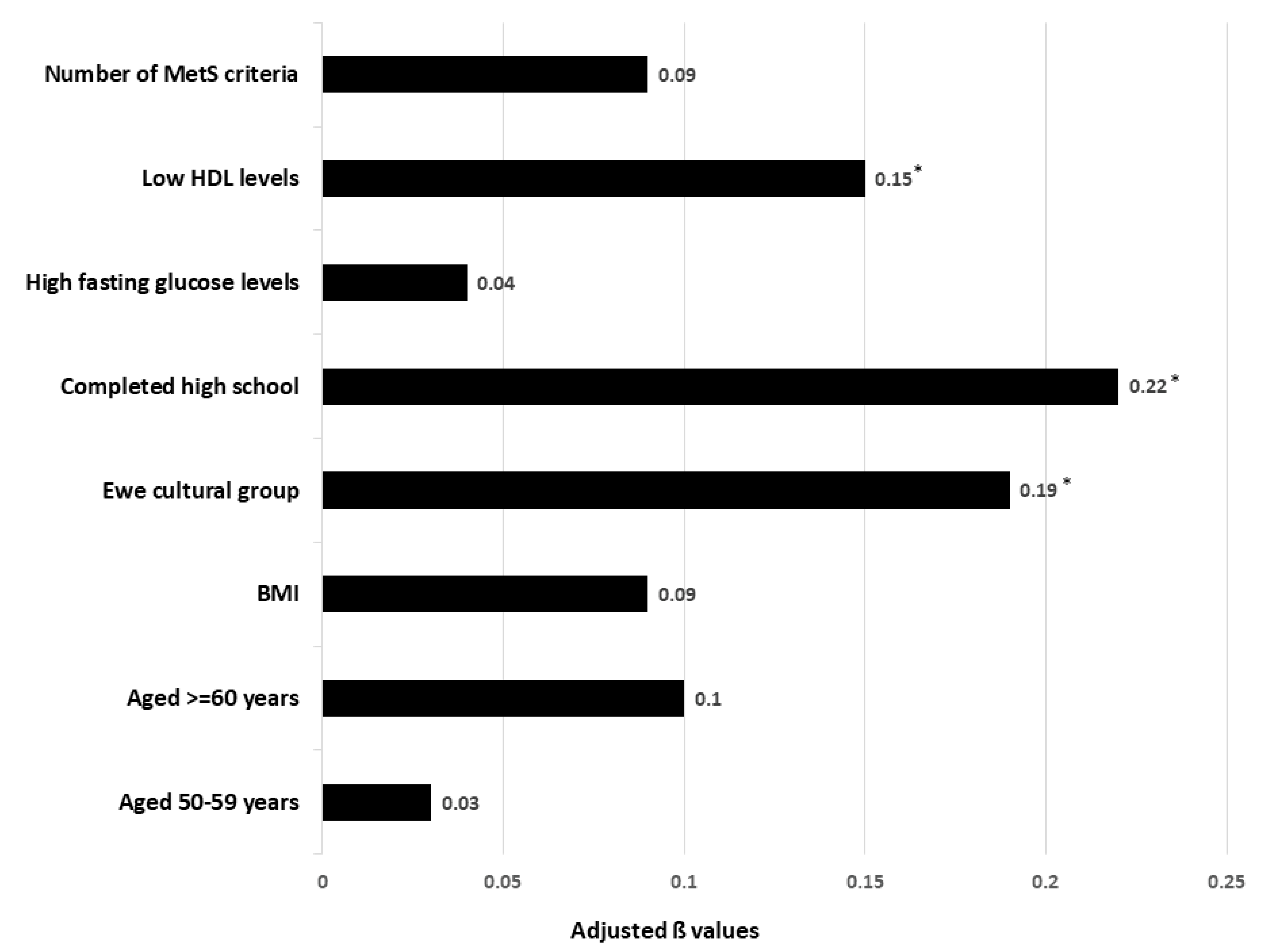
3.3. Factors Associated with Knowledge of MetS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grundy, S.M. Metabolic syndrome update. Trends Cardiovasc. Med. 2016, 26, 364–373. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.T.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Gradidge, P.J.; Crowther, N.J. Review: Metabolic Syndrome in Black South African Women. Ethn. Dis. 2017, 27, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2005, 365, 1415–1428. [Google Scholar] [CrossRef]
- Akinyemiju, T.; Do, A.N.; Patki, A.; Aslibekyan, S.; Zhi, D.; Hidalgo, B.; Tiwari, H.K.; Absher, D.; Geng, X.; Arnett, D.K.; et al. Epigenome-wide association study of metabolic syndrome in African-American adults. Clin. Epigenetics 2018, 10, 49. [Google Scholar] [CrossRef]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Christian, A.K.; Sanuade, O.A.; Kushitor, S.B.; Kushitor, M.; Kretchy, I.; Agyemang, C.; de-Graft Aikins, A. Metabolic syndrome among individuals living with hypertension in Accra, Ghana. PLoS ONE 2021, 16, e0253837. [Google Scholar] [CrossRef]
- Ofori-Asenso, R.; Agyeman, A.A.; Laar, A. Metabolic Syndrome in Apparently “Healthy” Ghanaian Adults: A Systematic Review and Meta-Analysis. Int. J. Chronic Dis. 2017, 2017, 2562374. [Google Scholar] [CrossRef]
- Arthur, F.K.; Adu-Frimpong, M.; Osei-Yeboah, J.; Mensah, F.O.; Owusu, L. The prevalence of metabolic syndrome and its predominant components among pre-and postmenopausal Ghanaian women. BMC Res. Notes 2013, 6, 446. [Google Scholar] [CrossRef]
- Afrifa-Anane, E.; Beune, E.; Addo, J.; Smeeth, L.; Bahendeka, S.; Stronks, K.; Agyemang, C. Physical Inactivity among Ghanaians in Ghana and Ghanaian Migrants in Europe. Med. Sci. Sports Exerc. 2020, 52, 2152–2161. [Google Scholar] [CrossRef]
- Abagre, T.A.; Bandoh, D.A.; Addo-Lartey, A.A. Determinants of metabolic syndrome among patients attending diabetes clinics in two sub-urban hospitals: Bono Region, Ghana. BMC Cardiovasc. Disord. 2022, 22, 366. [Google Scholar] [CrossRef]
- Ignatowicz, A.; Odland, M.L.; Bockarie, T.; Wurie, H.; Ansumana, R.; Kelly, A.H.; Willott, C.; Witham, M.; Davies, J. Knowledge and understanding of cardiovascular disease risk factors in Sierra Leone: A qualitative study of patients’ and community leaders’ perceptions. BMJ Open 2020, 10, e038523. [Google Scholar] [CrossRef]
- Annan, R.A.; Apprey, C.; Oppong, N.K.; Petty-Agamatey, V.; Mensah, L.; Thow, A.M. Public awareness and perception of Ghana’s restrictive policy on fatty meat, as well as preference and consumption of meat products among Ghanaian adults living in the Kumasi Metropolis. BMC Nutr. 2018, 4, 2. [Google Scholar] [CrossRef]
- Chen, M.-S.; Chiu, C.-H.; Chen, S.-H. Risk assessment of metabolic syndrome prevalence involving sedentary occupations and socioeconomic status. BMJ Open 2021, 11, e042802. [Google Scholar] [CrossRef]
- Mensah, D.; Aryeetey, R.; Oyebode, O. Evidence On Physical Activity And Sedentary Behaviour In Ghana: A Rapid Scoping Review. Afr. J. Food Agric. Nutr. Dev. 2022, 22, 19583–19601. [Google Scholar] [CrossRef]
- Boatemaa, S.; Badasu, D.M.; de-Graft Aikins, A. Food beliefs and practices in urban poor communities in Accra: Implications for health interventions. BMC Public Health 2018, 18, 434. [Google Scholar] [CrossRef]
- Jaspers Faijer-Westerink, H.; Kengne, A.P.; Meeks, K.A.C.; Agyemang, C. Prevalence of metabolic syndrome in sub-Saharan Africa: A systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 547–565. [Google Scholar] [CrossRef]
- Joshi, A.; Mehta, S.; Grover, A.; Talati, K.; Malhotra, B.; Puricelli Perin, D.M. Knowledge, Attitude, and Practices of Individuals to Prevent and Manage Metabolic Syndrome in an Indian Setting. Diabetes Technol. Ther. 2013, 15, 644–653. [Google Scholar] [CrossRef]
- Alefishat, E.A.; Abu Farha, R.K.; Al-Debei, M.M. Self-Reported Adherence among Individuals at High Risk of Metabolic Syndrome: Effect of Knowledge and Attitude. Med. Princ. Pract. 2017, 26, 157–163. [Google Scholar] [CrossRef]
- Wang, Q.; Chair, S.Y.; Wong, E.M.; Taylor-Piliae, R.E.; Qiu, X.C.H.; Li, X.M. Metabolic Syndrome Knowledge among Adults with Cardiometabolic Risk Factors: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 159. [Google Scholar] [CrossRef] [Green Version]
- Lo, S.W.S.; Chair, S.Y.; Lee, I.F.K. Knowledge of metabolic syndrome in Chinese adults: Implications for health education. Health Educ. J. 2015, 75, 589–599. [Google Scholar] [CrossRef]
- Amarasekara, P.; de Silva, A.; Swarnamali, H.; Senarath, U.; Katulanda, P. Knowledge, Attitudes, and Practices on Lifestyle and Cardiovascular Risk Factors Among Metabolic Syndrome Patients in an Urban Tertiary Care Institute in Sri Lanka. Asia Pacific J. Public Health 2015, 28, 32S–40S. [Google Scholar] [CrossRef]
- Emiral, G.O.; Tozun, M.; Atalay, B.I.; Goktas, S.; Dagtekin, G.; Aygar, H.; Arslantas, D.; Unsal, A.; Babaoglu, A.B.; Tirpan, K. Assessment of knowledge of metabolic syndrome and health literacy level among adults in Western Turkey. Niger. J. Clin. Pract. 2021, 24, 28–37. [Google Scholar] [CrossRef]
- Yahia, N.; Brown, C.; Rapley, M.; Chung, M. Assessment of college students’ awareness and knowledge about conditions relevant to metabolic syndrome. Diabetol. Metab. Syndr. 2014, 6, 111. [Google Scholar] [CrossRef]
- Nádas, J.; Putz, Z.; Jermendy, G.; Hidvégi, T. Public awareness of the metabolic syndrome. Diabetes Res. Clin. Pract. 2007, 76, 155–156. [Google Scholar] [CrossRef]
- Lewis, S.J.; Rodbard, H.W.; Fox, K.M.; Grandy, S.; SHIELD Study Group. Self-reported prevalence and awareness of metabolic syndrome: Findings from SHIELD. Int. J. Clin. Pract. 2008, 62, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Ekoru, K.; Murphy, G.A.V.; Young, E.H.; Delisle, H.; Jerome, C.S.; Assah, F.; Longo-Mbenza, B.; Nzambi, J.P.D.; On’Kin, J.B.K.; Buntix, F.; et al. Deriving an optimal threshold of waist circumference for detecting cardiometabolic risk in sub-Saharan Africa. Int. J. Obes. 2017, 42, 487–494. [Google Scholar] [CrossRef]
- Amoah, P.A.; Phillips, D.R. Health literacy and health: Rethinking the strategies for universal health coverage in Ghana. Public Health 2018, 159, 40–49. [Google Scholar] [CrossRef]
- Tindana, P.; Ramsay, M.; Klipstein-Grobusch, K.; Amoakoh-Coleman, M. Advancing non-communicable diseases research in Ghana: Key stakeholders’ recommendations from a symposium. Ghana Med. J. 2020, 54, 121–125. [Google Scholar] [CrossRef]

| Variables | MetS Knowledge Score | t-Test or ANOVA p-Value for Model |
|---|---|---|
| Age categories (years) | 0.012 | |
| 25–39 (n = 98) | 42.0 ± 11.1 | |
| 40–49 (n = 96) | 42.5 ± 11.7 | |
| 50–59 (n = 103) | 43.5 ± 11.4 | |
| ≥60 (n = 41) | 39.0 ± 12.7 | |
| Marital status | 0.035 | |
| Widowed, divorced or single (n = 157) | 41.4 ± 11.7 | |
| Living together (n = 181) | 42.9 ± 11.5 | |
| Highest level of education | 0.000 | |
| None (n = 39) | 37.0 ± 10.3 | |
| Primary school (n = 52) | 40.2 ± 11.7 | |
| Middle school (n = 163) | 41.9 ± 11.2 | |
| Secondary school (n = 72) | 46.9 ± 11.5 | |
| Tertiary education (n = 12) | 44.4 ± 12.5 | |
| Cultural affiliation | 0.011 | |
| Akan (n = 200) | 42.3 ± 12.3 | |
| Ewe (n = 17) | 33.3 ± 14.2 | |
| GA (n = 91) | 43.0 ± 9.5 | |
| Other (n = 30) | 44.1 ± 9.5 | |
| Self-reported hypertension | 0.098 | |
| Yes (n = 83) | 41.6 ± 11.2 | |
| No (n = 255) | 44.0 ± 12.8 | |
| Self-reported diabetes | 0.741 | |
| Yes (n = 22) | 41.1 ± 13.8 | |
| No (n = 316) | 42.3 ± 11.5 | |
| BMI categories | 0.069 | |
| <25 kg/m2 (n = 65) | 39.5 ± 9.2 | |
| 25–29.9 kg/m2 (n = 105) | 42.0 ± 10.8 | |
| ≥30 kg/m2 (n = 168) | 43.4 ± 12.8 | |
| Central fat using waist | 0.361 | |
| ≥80 cm (n = 298) | 42.2 ± 11.8 | |
| <80 cm (n = 40) | 39.2 ± 9.7 | |
| Elevated BP | 0.956 | |
| Yes (n = 168) | 43.0 ± 11.9 | |
| No (n = 170) | 41.4 ± 11.3 | |
| Fasting glucose ≥ 5.6 mmol/L | 0.041 | |
| Yes (n = 76) | 44.9 ± 13.1 | |
| No (n = 262) | 41.4 ± 11.0 | |
| Serum triglycerides ≥ 1.7 mmol/L | 0.177 | |
| Yes (n = 10) | 46.7 ± 4.7 | |
| No (n = 328) | 42.1 ± 11.7 | |
| HDL < 1.3 mmol/L | 0.202 | |
| Yes (n = 233) | 41.1 ± 11.3 | |
| No (n = 105) | 44.8 ± 12.0 | |
| Number of MetS risk factors | 0.529 | |
| 0 (n = 1) | 44.4 ± 0 | |
| 1 (n = 50) | 39.6 ± 10.3 | |
| 2 (n = 145) | 42.5 ± 11.2 | |
| 3 (n = 123) | 42.9 ± 12.8 | |
| 4 (n = 19) | 42.7 ± 10.0 | |
| Presence of MetS | 0.615 | |
| Yes (n = 142) | 42.9 ± 12.4 | |
| No (n = 196) | 41.7 ± 11.0 |
| Risk Factors | Mean ± SD |
|---|---|
| BMI (kg/m2) | 30.7 ± 6.5 |
| WC (cm) | 95.3 ± 12.9 |
| Total cholesterol (mmol/L) | 5.5 ± 1.1 |
| Triglycerides (mmol/L) | 1.0 ± 0.3 |
| HDL (mmol/L) | 1.2 ± 0.3 |
| Systolic BP (mm Hg) | 128.2 ± 22.1 |
| Diastolic BP (mm Hg) | 77.1 ± 12.8 |
| Blood glucose (mmol/L) | 5.4 ± 2.4 |
| Item Number | Knowledge Criteria | Mean ± SD | Correct Answer n (%) | Do Not Know n (%) |
|---|---|---|---|---|
| 1 | Definition of MetS? | 0.13 ± 0.34 | 44 (13) | 294 (87) |
| 2 | Waist circumference (≥80 cm) | 0.03 ± 0.16 | 9 (2.7) | 329 (97.3) |
| 3 | Elevated blood pressure (Systolic ≥130 and/or diastolic ≥ 85 mm Hg) | 0.17 ± 0.38 | 57 (16.9) | 281 (83.1) |
| 4 | Fasting glucose (≥5.6 mmol/L) | 0.06 ± 0.24 | 21 (6.2) | 317 (93.8) |
| 5 | Complications of MetS | 0.01 ± 0.1 | 3 (0.9) | 335 (99.1) |
| 6 | Consequences of waist ≥ 80 cm | 0.66 ± 0.47 | 224 (66.3) | 114 (33.7) |
| 7 | Behaviours associated with MetS | 0.94 ± 0.23 | 319 (94.4) | 19 (5.6) |
| 8 | Self-care once diagnosed with MetS | 0.83 ± 0.37 | 281 (83.1) | 57 (16.9) |
| 9 | Medical treatment of MetS | 0.96 ± 0.19 | 326 (96.4) | 12 (3.6) |
| Total questionnaire score range (0–90) | 42.2 ± 11.6 | 1284 (37.9) | 1785 (52.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Achempim-Ansong, G.; Tshabalala, A.M.; Gradidge, P.J. Factors Associated with Improved Knowledge of Metabolic Syndrome in Female Market Traders. Int. J. Environ. Res. Public Health 2022, 19, 12256. https://doi.org/10.3390/ijerph191912256
Achempim-Ansong G, Tshabalala AM, Gradidge PJ. Factors Associated with Improved Knowledge of Metabolic Syndrome in Female Market Traders. International Journal of Environmental Research and Public Health. 2022; 19(19):12256. https://doi.org/10.3390/ijerph191912256
Chicago/Turabian StyleAchempim-Ansong, Gloria, Amme M. Tshabalala, and Philippe J. Gradidge. 2022. "Factors Associated with Improved Knowledge of Metabolic Syndrome in Female Market Traders" International Journal of Environmental Research and Public Health 19, no. 19: 12256. https://doi.org/10.3390/ijerph191912256
APA StyleAchempim-Ansong, G., Tshabalala, A. M., & Gradidge, P. J. (2022). Factors Associated with Improved Knowledge of Metabolic Syndrome in Female Market Traders. International Journal of Environmental Research and Public Health, 19(19), 12256. https://doi.org/10.3390/ijerph191912256






