PTSD and Depression Symptoms Increase Women’s Risk for Experiencing Future Intimate Partner Violence
Abstract
:1. Introduction
1.1. Women Veterans
1.2. PTSD Symptoms, Depression Symptoms, and Alcohol Use as Factors Increasing Risk for IPV
1.3. Current Study
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measures
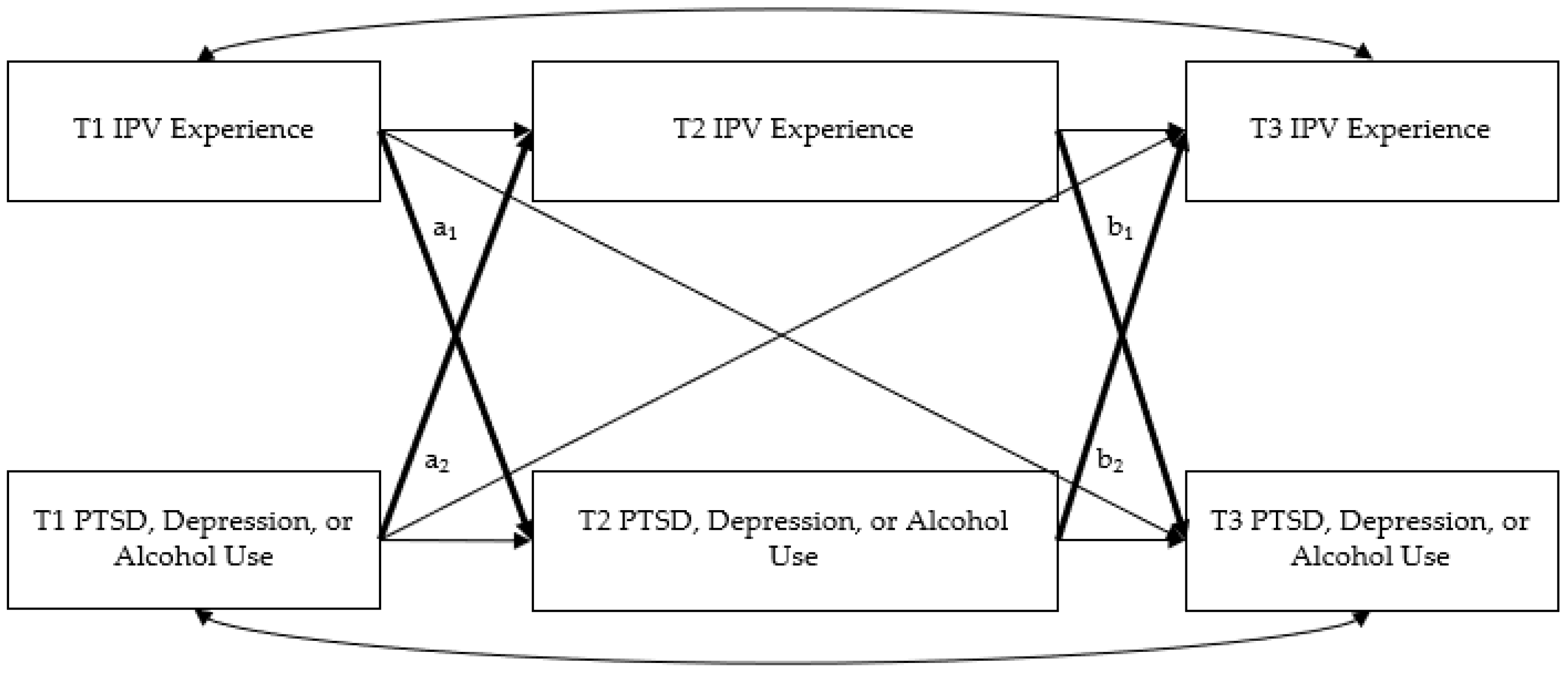
2.4. Data Analytic Plan
3. Results
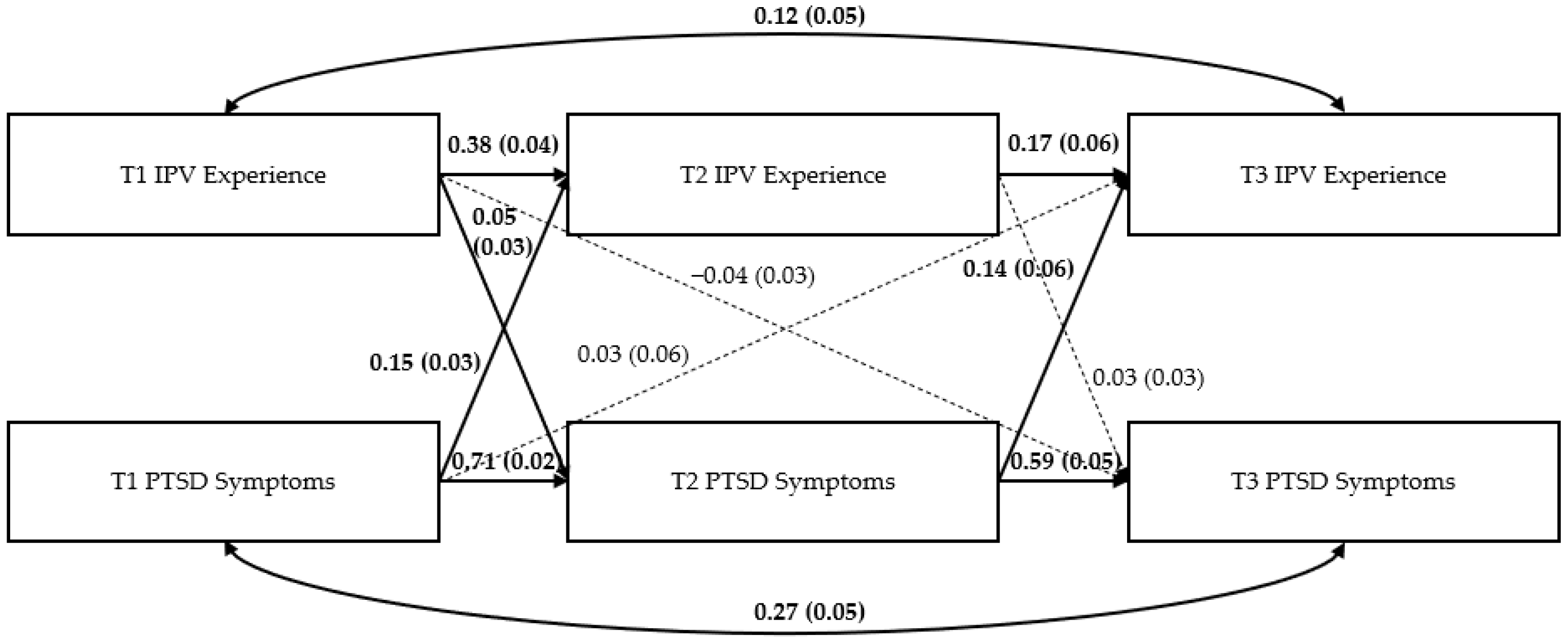
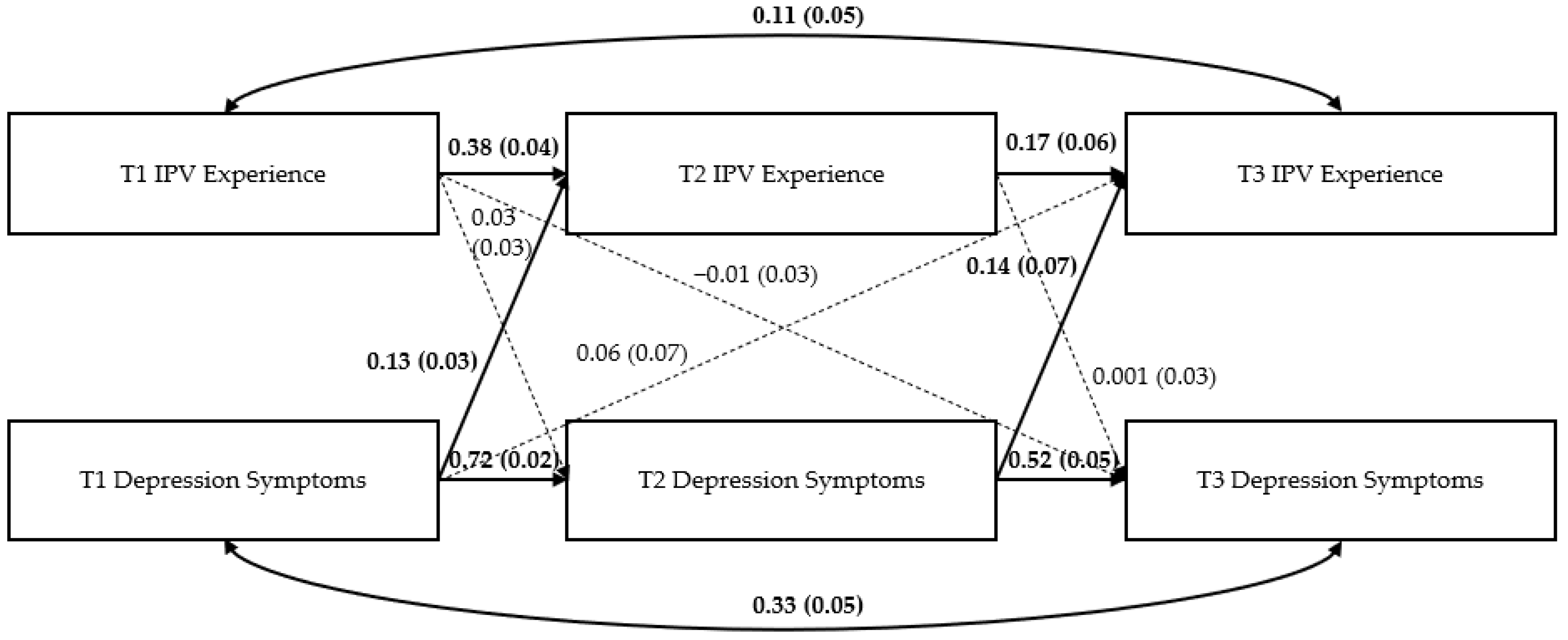
Path Models
4. Discussion
4.1. Limitations
4.2. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Violence against Women Prevalence Estimates, 2018: Global, Regional and National Prevalence Estimates for Intimate Partner Violence against Women and Global and Regional Prevalence Estimates for Non-Partner Sexual Violence against Women; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- World Health Organization. Responding to Intimate Partner Violence and Sexual Violence against Women: WHO Clinical and Policy Guidelines; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Black, M.C.; Basile, K.C.; Breiding, M.J.; Smith, S.G.; Walters, M.L.; Merrick, M.T.; Chen, J.; Stevens, M.R. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report; National Center for Injury Prevention and Control, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2011.
- Smith, S.G.; Zhang, X.; Basile, K.C.; Merrick, M.T.; Wang, J.; Kresnow, M.; Chen, J. The National Intimate Partner and Sexual Violence Survey: 2015 Data Brief—Updated Release; National Center for Injury Prevention and Control Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018.
- Smith, S.G.; Chen, J.; Basile, K.C.; Gilbert, L.K.; Merrick, M.T.; Patel, N.; Walling, M.; Jain, A. National Intimate Partner and Sexual Violence Survey (NISVS): 2010–2012 State Report. 2017. Available online: https://www.cdc.gov/violenceprevention/pdf/nisvs-statereportbook.pdf (accessed on 30 June 2022).
- Doyle, K.W.; Knetig, J.A.; Iverson, K.M. Practical implications of research on intimate partner violence experiences for the mental health clinician. Curr. Treat. Options Psychiatry 2022, 9, 280–300. [Google Scholar] [CrossRef]
- Coker, A.L.; Davis, K.E.; Arias, I.; Desai, S.; Sanderson, M.; Brandt, H.M.; Smith, P.H. Physical and mental health effects of intimate partner violence for men and women. Am. J. Prev. Med. 2002, 23, 260–268. [Google Scholar] [CrossRef]
- Dutton, M.A. Pathways linking intimate partner violence and posttraumatic disorder. Trauma Violence Abus. 2009, 10, 211–224. [Google Scholar] [CrossRef] [PubMed]
- Iverson, K.M.; Dick, A.; McLaughlin, K.A.; Smith, B.N.; Bell, M.E.; Gerber, M.R.; Cook, N.; Mitchell, K.S. Exposure to interpersonal violence and its associations with psychiatric morbidity in a US national sample: A gender comparison. Psychol. Violence 2013, 3, 273–287. [Google Scholar] [CrossRef] [PubMed]
- Lagdon, S.; Armour, C.; Stringer, M. Adult experience of mental health outcomes as a result of intimate partner violence victimisation: A systematic review. Eur. J. Psychotraumatol. 2014, 5, 24794. [Google Scholar] [CrossRef]
- Maskin, R.M.; Iverson, K.M.; Vogt, D.; Smith, B.N. Associations between intimate partner violence victimization and employment outcomes among male and female post-9/11 veterans. Psychol. Trauma Theory Res. Pract. Policy 2019, 11, 406–414. [Google Scholar] [CrossRef]
- Krause, E.D.; Kaltman, S.; Goodman, L.; Dutton, M.A. Role of distinct PTSD symptoms in intimate partner reabuse: A prospective study. J. Trauma. Stress 2006, 19, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Kuijpers, K.F.; Van Der Knaap, L.M.; Winkel, F.W. Victims’ influence on intimate partner violence revictimization: An empirical test of dynamic victim-related risk factors. J. Interpers. Violence 2012, 27, 1716–1742. [Google Scholar] [CrossRef]
- Iverson, K.M.; Gradus, J.L.; Resick, P.A.; Suvak, M.K.; Smith, K.F.; Monson, C.M. Cognitive–behavioral therapy for PTSD and depression symptoms reduces risk for future intimate partner violence among interpersonal trauma survivors. J. Consult. Clin. Psychol. 2011, 79, 193–202. [Google Scholar] [CrossRef]
- Iverson, K.M.; Litwack, S.D.; Pineles, S.L.; Suvak, M.K.; Vaughn, R.A.; Resick, P.A. Predictors of intimate partner violence revictimization: The relative impact of distinct PTSD symptoms, dissociation, and coping strategies. J. Trauma. Stress 2013, 26, 102–110. [Google Scholar] [CrossRef]
- Babcock, J.C.; Green, C.E.; Robie, C. Does batterers’ treatment work? A meta-analytic review of domestic violence treatment. Clin. Psychol. Rev. 2004, 23, 1023–1053. [Google Scholar] [CrossRef] [PubMed]
- Travers, Á.; McDonagh, T.; Cunningham, T.; Armour, C.; Hansen, M. The effectiveness of interventions to prevent recidivism in perpetrators of intimate partner violence: A systematic review and meta-analysis. Clin. Psychol. Rev. 2021, 84, 101974. [Google Scholar] [CrossRef] [PubMed]
- Taft, C.T.; Creech, S.K.; Gallagher, M.W.; Macdonald, A.; Murphy, C.M.; Monson, C.M. Strength at Home Couples program to prevent military partner violence: A randomized controlled trial. J. Consult. Clin. Psychol. 2016, 84, 935–945. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, L.B.; Goodman, L.A. Risk factors for reabuse in intimate partner violence: A cross-disciplinary critical review. Trauma Violence Abus. 2005, 6, 141–175. [Google Scholar] [CrossRef] [PubMed]
- Goodman, L.; Dutton, M.A.; Vankos, N.; Weinfurt, K. Women’s resources and use of strategies as risk and protective factors for reabuse over time. Violence Against Women 2005, 11, 311–336. [Google Scholar] [CrossRef] [PubMed]
- Risser, H.J.; Hetzel-Riggin, M.D.; Thomsen, C.J.; McCanne, T.R. PTSD as a mediator of sexual revictimization: The role of reexperiencing, avoidance, and arousal symptoms. J. Trauma. Stress Off. Publ. Int. Soc. Trauma. Stress Stud. 2006, 19, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Cowlishaw, S.; Freijah, I.; Kartal, D.; Sbisa, A.; Mulligan, A.; Notarianni, M.; Couineau, A.-L.; Forbes, D.; O’Donnell, M.; Phelps, A.; et al. Intimate Partner Violence (IPV) in military and veteran populations: A systematic review of population-based surveys and population screening studies. Int. J. Environ. Res. Public Health 2022, 19, 8853. [Google Scholar] [CrossRef]
- Parr, N.J.; Young, S.; Ward, R.; Mackey, K. Evidence Brief: Prevalence of Intimate Partner Violence/Sexual Assault among Veterans; Department of Veterans Affairs (US): Washington, DC, USA, 2021.
- Dichter, M.E.; Cerulli, C.; Bossarte, R.M. Intimate partner violence victimization among women veterans and associated heart health risks. Womens Health Issues 2011, 21, S190–S194. [Google Scholar] [CrossRef]
- Iverson, K.M.; Stirman, S.W.; Street, A.E.; Gerber, M.R.; Carpenter, S.L.; Dichter, M.E.; Bair-Merritt, M.; Vogt, D. Female veterans’ preferences for counseling related to intimate partner violence: Informing patient-centered interventions. Gen. Hosp. Psychiatry 2016, 40, 33–38. [Google Scholar] [CrossRef]
- Holliday, R.; Forster, J.E.; Schneider, A.L.; Miller, C.; Monteith, L.L. Interpersonal violence throughout the lifespan: Associations with suicidal ideation and suicide attempt among a national sample of female veterans. Med. Care 2021, 59, S77–S83. [Google Scholar] [CrossRef]
- Wilson, L.C. The prevalence of military sexual trauma: A meta-analysis. Trauma Violence Abuse 2018, 19, 584–597. [Google Scholar] [CrossRef] [PubMed]
- Frayne, S.M.; Parker, V.A.; Christiansen, C.L.; Loveland, S.; Seaver, M.R.; Kazis, L.E.; Skinner, K.M. Health status among 28,000 women veterans: The VA women’s health program evaluation project. J. Gen. Intern. Med. 2006, 21, S40–S46. [Google Scholar] [CrossRef] [PubMed]
- Lehavot, K.; Hoerster, K.D.; Nelson, K.M.; Jakupcak, M.; Simpson, T.L. Health indicators for military, veteran, and civilian women. Am. J. Prev. Med. 2012, 42, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.R.; Iverson, K.M.; Dichter, M.E.; Klap, R.; Latta, R.E. Women veterans and intimate partner violence: Current state of knowledge and future directions. J. Womens Health 2014, 23, 302–309. [Google Scholar] [CrossRef]
- Portnoy, G.A.; Relyea, M.R.; Street, A.E.; Haskell, S.G.; Iverson, K.M. A longitudinal analysis of women veterans’ partner violence perpetration: The roles of interpersonal trauma and posttraumatic stress symptoms. J. Fam. Violence 2020, 35, 361–372. [Google Scholar] [CrossRef]
- Arata, C.M. Child sexual abuse and sexual revictimization. Clin. Psychol. 2002, 9, 135–164. [Google Scholar] [CrossRef]
- Fortier, M.A.; DiLillo, D.; Messman-Moore, T.L.; Peugh, J.; Denardi, K.A.; Gaffey, K.J. Severity of child sexual abuse and revictimization: The mediating role of coping and trauma symptoms. Psychol. Women Q. 2009, 33, 308–320. [Google Scholar] [CrossRef]
- Dardis, C.M.; Ullman, S.E.; Rodriguez, L.M.; Waterman, E.A.; Dworkin, E.R.; Edwards, K.M. Bidirectional associations between alcohol use and intimate partner violence and sexual assault victimization among college women. Addict. Behav. 2021, 116, 106833. [Google Scholar] [CrossRef]
- Perez, S.; Johnson, D.M. PTSD compromises battered women’s future safety. J. Interpers. Violence 2008, 23, 635–651. [Google Scholar] [CrossRef]
- Dardis, C.M.; Dichter, M.E.; Iverson, K.M. Empowerment, PTSD and revictimization among women who have experienced intimate partner violence. Psychiatry Res. 2018, 266, 103–110. [Google Scholar] [CrossRef]
- Stein, S.F.; Galano, M.M.; Grogan-Kaylor, A.C.; Clark, H.M.; Ribaudo, J.M.; Graham-Bermann, S.A. Predictors of intimate partner violence victimization by multiple partners over a period of 8 years. J. Trauma. Stress 2022, 35, 222–234. [Google Scholar] [CrossRef] [PubMed]
- Bybee, D.; Sullivan, C.M. Predicting re-victimization of battered women 3 years after exiting a shelter program. Am. J. Community Psychol. 2005, 36, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Testa, M.; Hoffman, J.H.; Livingston, J.A. Alcohol and sexual risk behaviors as mediators of the sexual victimization–revictimization relationship. J. Consult. Clin. Psychol. 2010, 78, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Wilhite, E.R.; Mallard, T.; Fromme, K. A longitudinal event-level investigation of alcohol intoxication, alcohol-related blackouts, childhood sexual abuse, and sexual victimization among college students. Psychol. Addict. Behav. 2018, 32, 289–300. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, C.T.; Iverson, K.M. The roles of alcohol use severity and posttraumatic stress disorder symptoms as risk factors for women’s intimate partner violence experiences. J. Womens Health 2020, 29, 827–836. [Google Scholar] [CrossRef] [PubMed]
- Testa, M.; Livingston, J.A.; Hoffman, J.H. Does sexual victimization predict subsequent alcohol consumption? A prospective study among a community sample of women. Addict. Behav. 2007, 32, 2926–2939. [Google Scholar] [CrossRef]
- Smith, P.H.; Homish, G.G.; Leonard, K.E.; Cornelius, J.R. Intimate partner violence and specific substance use disorders: Findings from the national epidemiologic survey on alcohol and related conditions. Psychol. Addict. Behav. 2012, 26, 236–245. [Google Scholar] [CrossRef]
- Cattaneo, L.B.; Bell, M.E.; Goodman, L.A.; Dutton, M.A. Intimate partner violence victims’ accuracy in assessing their risk of re-abuse. J. Fam. Violence 2007, 22, 429–440. [Google Scholar] [CrossRef]
- Testa, M.; Livingston, J.A.; Vanzile-Tamsen, C.; Frone, M.R. The role of women’s substance use in vulnerability to forcible and incapacitated rape. J. Stud. Alcohol Drugs 2003, 64, 756–764. [Google Scholar] [CrossRef]
- Foa, E.B.; Cascardi, M.; Zoellner, L.A.; Feeny, N.C. Psychological and environmental factors associated with partner violence. Trauma Violence Abus. 2000, 1, 67–91. [Google Scholar] [CrossRef]
- Nillni, Y.I.; Fox, A.B.; Cox, K.; Paul, E.; Vogt, D.; Galovski, T.E. The impact of military sexual trauma and warfare exposure on women veterans’ perinatal outcomes. Psychol. Trauma 2022, 14, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Dillman, D.A.; Smyth, J.D.; Christian, L.M. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method; John Wiley & Sons: Hoboken, NJ, USA, 2014. [Google Scholar]
- Vogt, D.; Smith, B.N.; King, L.A.; King, D.W.; Knight, J.; Vasterling, J.J. Deployment Risk and Resilience Inventory-2 (DRRI-2): An updated tool for assessing psychosocial risk and resilience factors among service members and veterans. J. Trauma. Stress 2013, 26, 710–717. [Google Scholar] [CrossRef] [PubMed]
- Breiding, M.J.; Basile, K.C.; Smith, S.G.; Black, M.C.; Mahendra, R.R. Intimate Partner Violence Surveillance: Uniform Definitions and Recommended Data Elements, Version 2.0.; National Center for Injury Prevention and Control, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2015.
- Galovski, T.; Iverson, K. Lifetime Trauma Interview for Intimate Partner Violence Survivors. 2019; unpublished. [Google Scholar]
- Bovin, M.J.; Marx, B.P.; Weathers, F.W.; Gallagher, M.W.; Rodriguez, P.; Schnurr, P.P.; Keane, T.M. Psychometric properties of the PTSD checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychol. Assess. 2016, 28, 1379–1391. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5). Available online: http://www.ptsd.va.gov (accessed on 10 April 2022).
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A.; Ambulatory Care Quality Improvement Project (ACQUIP). The AUDIT Alcohol Consumption Questions (AUDIT-C). An effective brief screening test for problem drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef]
- Crawford, E.F.; Fulton, J.J.; Swinkels, C.M.; Beckham, J.C.; Calhoun, P.S.; VA Mid-Atlantic MIRECC OEF/OIF Registry Workgroup. Diagnostic efficiency of the AUDIT-C in U.S. veterans with military service since September 11, 2001. Drug Alcohol Depend. 2013, 132, 101–106. [Google Scholar] [CrossRef]
- Booth, B.M.; Davis, T.D.; Cheney, A.M.; Mengeling, M.A.; Torner, J.C.; Sadler, A.G. Physical health status of female veterans: Contributions of sex partnership and in-military rape. Psychosom. Med. 2012, 74, 916–924. [Google Scholar] [CrossRef]
- Frayne, S.M.; Phibbs, C.S.; Saechao, F.; Friedman, S.A.; Shaw, J.G.; Romodan, Y.; Berg, E.; Lee, J.; Lakshmi, A.; Iqbal, S.; et al. Volume 4: Longitudinal trends in sociodemographics, utilization, health profile, and geographic distribution. In Women Veterans in the Veterans Health Administration; Women’s Health Evaluation Initiative, Ed.; Women’s Health Services, Veterans Health Administration, Department of Veterans Affairs: Washington, DC, USA, 2018. [Google Scholar]
- Smith, B.N.; Tyzik, A.L.; Iverson, K.M. Age-related differences in trauma exposure, PTSD symptomatology, and functional health and well-being in women veterans. Traumatology 2015, 21, 128–135. [Google Scholar] [CrossRef]
- Iverson, K.M.; Vogt, D.; Dichter, M.E.; Carpenter, S.L.; Kimerling, R.; Street, A.E.; Gerber, M.R. Intimate partner violence and current mental health needs among female veterans. J. Am. Board Fam. Med. 2015, 28, 772–776. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2012. [Google Scholar]
- Creech, S.K.; Benzer, J.K.; Meyer, E.C.; Debeer, B.B.; Kimbrel, N.A.; Morissette, S.B. Longitudinal associations in the direction and prediction of PTSD symptoms and romantic relationship impairment over one year in post 9/11 veterans: A comparison of theories and exploration of potential gender differences. J. Abnorm. Psychol. 2019, 128, 245–255. [Google Scholar] [CrossRef]
- Cougle, J.R.; Resnick, H.; Kilpatrick, D.G. A prospective examination of PTSD symptoms as risk factors for subsequent exposure to potentially traumatic events among women. J. Abnorm. Psychol. 2009, 118, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Messman-Moore, T.L.; Long, P.J. The role of childhood sexual abuse sequelae in the sexual revictimization of women: An empirical review and theoretical reformulation. Clin. Psychol. Rev. 2003, 23, 537–571. [Google Scholar] [CrossRef]
- Kuijpers, K.F.; van der Knaap, L.M.; Winkel, F.W. PTSD symptoms as risk factors for intimate partner violence revictimization and the mediating role of victims’ violent behavior. J. Trauma. Stress 2012, 25, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Marx, B.P.; Heidt, J.M.; Gold, S.D. Perceived uncontrollability and unpredictability, self-regulation, and sexual revictimization. Rev. Gen. Psychol. 2005, 9, 67–90. [Google Scholar] [CrossRef]
- Breslau, N.; Davis, G.C.; Peterson, E.L.; Schultz, L. Psychiatric sequelae of posttraumatic stress disorder in women. Arch. Gen. Psychiatry 1997, 54, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Waller, M.W.; Iritani, B.J.; Christ, S.L.; Clark, H.K.; Moracco, K.E.; Halpern, C.T.; Flewelling, R.L. Relationships among alcohol outlet density, alcohol use, and intimate partner violence victimization among young women in the United States. J. Interpers. Violence 2012, 27, 2062–2086. [Google Scholar] [CrossRef]
- Dichter, M.E.; Marcus, S.C.; Wagner, C.; Bonomi, A.E. Associations between psychological, physical, and sexual intimate partner violence and health outcomes among women veteran VA patients. Soc. Work Ment. Health 2014, 12, 411–428. [Google Scholar] [CrossRef]
- Straus, M.A.; Hamby, S.L.; Boney-McCoy, S.; Sugarman, D.B. The revised Conflict Tactics Scales (CTS2) development and preliminary psychometric data. J. Fam. Issues 1996, 17, 283–316. [Google Scholar] [CrossRef]
- Smith, P.H.; Earp, J.A.; DeVellis, R. Measuring battering: Development of the Women’s Experience with Battering (WEB) scale. Womens Health Res. Gend. Behav. Policy 1995, 1, 273–288. [Google Scholar]
- Tol, W.A.; Murray, S.M.; Lund, C.; Bolton, P.; Murray, L.K.; Davies, T.; Haushofer, J.; Orkin, K.; Witte, M.; Salama, L.; et al. Can mental health treatments help prevent or reduce intimate partner violence in low- and middle-income countries? A systematic review. BMC Womens Health 2019, 19, 34. [Google Scholar] [CrossRef]
- Ogbe, E.; Harmon, S.; Van den Bergh, R.; Degomme, O. A systematic review of intimate partner violence interventions focused on improving social support and/ mental health outcomes of survivors. PLoS ONE 2020, 15, e0235177. [Google Scholar] [CrossRef] [PubMed]
- Trabold, N.; McMahon, J.; Alsobrooks, S.; Whitney, S.; Mittal, M. A systematic review of intimate partner violence interventions: State of the field and implications for practitioners. Trauma Violence Abus. 2020, 21, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Iverson, K.M.; Danitz, S.B.; Shayani, D.R.; Vogt, D.; Stirman, S.W.; Hamilton, A.B.; Mahoney, C.T.; Gerber, M.R.; Dichter, M.E. Recovering from Intimate Partner Violence through Strengths and Empowerment: Findings from a randomized clinical trial. J. Clin. Psychiatry 2022, 83, 38188. [Google Scholar] [CrossRef]
- Iverson, K.M.; Danitz, S.B.; Low, S.K.; Knetig, J.A.; Doyle, K.W.; Bruce, L.E. Recovering from Intimate Partner Violence through Strengths and Empowerment (RISE): Initial valuation of the clinical effects of RISE administered in routine care in the US Veterans Health Administration. Int. J. Environ. Res. Public Health 2022, 19, 8793. [Google Scholar] [CrossRef] [PubMed]
- Creech, S.K.; Pulverman, C.S.; Shin, M.E.; Roe, K.T.; Wernette, G.T.; Orchowski, L.M.; Kahler, C.W.; Shea, M.T.; Zlotnick, C. An open trial to test participant satisfaction with and feasibility of a computerized intervention for women veterans with sexual trauma histories seeking primary care treatment. Violence Against Women 2021, 27, 597–614. [Google Scholar] [CrossRef] [PubMed]
- Creech, S.K.; Pulverman, C.S.; Kahler, C.W.; Orchowski, L.M.; Shea, M.T.; Wernette, G.T.; Zlotnick, C. Computerized intervention in primary care for women veterans with sexual assault histories and psychosocial health risks: A randomized clinical trial. J. Gen. Intern. Med. 2022, 37, 1097–1107. [Google Scholar] [CrossRef]
- Shayani, D.R.; Danitz, S.B.; Low, S.K.; Hamilton, A.B.; Iverson, K.M. Women tell all: A comparative thematic analysis of women’s perspectives on two brief counseling interventions for intimate partner violence. Int. J. Environ. Res. Public Health 2022, 19, 2513. [Google Scholar] [CrossRef]
- Cowlishaw, S.; Sbisa, A.; Freijah, I.; Kartal, D.; Mulligan, A.; Notarianni, M.; Iverson, K.; Couineau, A.-L.; Forbes, D.; O’Donnell, M.; et al. Health service interventions for intimate partner violence among military personnel and veterans: A framework and scoping review. Int. J. Environ. Res. Public Health 2022, 19, 3551. [Google Scholar] [CrossRef]
- Department of Veterans. Intimate Partner Violence Assistance Program. VHA Directive 1198; Department of Veterans Affairs, Veterans Health Administration: Washington, DC, USA, 2019.

| Characteristics, M (SD) | M | SD |
|---|---|---|
| Age | 36.5 | 7.6 |
| Characteristics, n (%) | n | % |
| Race | ||
| White (alone) | 1177 | 62.5 |
| Black (alone) | 559 | 29.7 |
| Asian (alone) | 91 | 4.8 |
| Another/Multiple Races | 418 | 22.2 |
| Hispanic/Latino | 228 | 12 |
| Annual Income | ||
| No income | 26 | 1.4 |
| Less than USD 15k | 127 | 6.9 |
| USD 15k to <USD 25k | 189 | 10.2 |
| USD 25k to <USD 35k | 193 | 10.5 |
| USD 35k to <USD 45k | 188 | 10.2 |
| USD 45k to <USD 55k | 189 | 10.2 |
| USD 55k to <USD 75k | 266 | 14.4 |
| USD 75k to <USD 100k | 265 | 14.4 |
| USD 100k to <USD 150k | 242 | 13.1 |
| USD 150k or more | 159 | 8.6 |
| Relationship Status | ||
| Married | 826 | 43.8 |
| Divorced or separated | 496 | 26.3 |
| Widowed | 15 | 0.8 |
| Never Married | 547 | 29 |
| Education Level | ||
| High school or less | 117 | 6.3 |
| Vocational or technical training | 54 | 2.9 |
| Associates degree or some college | 718 | 38.5 |
| Bachelor’s degree | 549 | 29.4 |
| Graduate or professional degree | 430 | 23 |
| Work Status | ||
| Work for pay (part or full time) | 1425 | 76.7 |
| Homemaker/Caregiver | 198 | 10.7 |
| Retired | 69 | 3.7 |
| Not working | 350 | 18.8 |
| Living Situation | ||
| Own apartment/house | 775 | 41.7 |
| Rent apartment/house/room | 912 | 49 |
| Live with relative/friend | 120 | 6.5 |
| Homeless | 11 | 0.6 |
| Branch of Service | ||
| Army | 959 | 50.6 |
| Marine Corps | 102 | 5.4 |
| Navy | 310 | 16.3 |
| Air Force | 491 | 25.8 |
| Coast Guard | 32 | 1.7 |
| Primary Military Occupation | ||
| Combat Arms | 104 | 5.7 |
| Combat Support | 646 | 35.7 |
| Service Support | 1060 | 58.6 |
| Times Deployed | ||
| 0 | 338 | 27.9 |
| 1 | 474 | 39.1 |
| 2 or more | 399 | 32.9 |
| Sexual Assault During Military Service | 534 | 28.7 |
| Combat Experience | 766 | 40.3 |
| Variable | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | M | SD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 IPV | 0.17 ** | 0.21 ** | 0.10 ** | 0.40 ** | 0.14 ** | 0.16 ** | 0.06 | 0.21 ** | 0.12 ** | 0.16 ** | 0.07 * | -- | -- |
| 2. T1 PTSD | — | 0.72 ** | 0.10 ** | 0.21 ** | 0.75 ** | 0.61 ** | 0.03 | 0.19 ** | 0.70 ** | 0.61 ** | −0.01 | 28.40 | 22.63 |
| 3. T1 Depression | — | 0.11 ** | 0.21 ** | 0.65 ** | 0.74 ** | 0.01 | 0.21 ** | 0.64 ** | 0.71 ** | −0.01 | 7.81 | 7.03 | |
| 4. T1 Alcohol use | — | 0.09 * | 0.04 | 0.09 ** | 0.71 ** | 0.09 * | 0.07 | 0.12 ** | 0.67 ** | 3.18 | 2.20 | ||
| 5. T2 IPV | — | 0.23 ** | 0.25 ** | 0.05 | 0.26 ** | 0.24 ** | 0.20 ** | 0.04 | -- | -- | |||
| 6. T2 PTSD | — | 0.77 ** | 0.02 | 0.20 ** | 0.77 ** | 0.68 ** | −0.09 * | 22.08 | 20.24 | ||||
| 7. T2 Depression | — | 0.04 | 0.21 ** | 0.67 ** | 0.75 ** | 0.00 | 6.81 | 6.50 | |||||
| 8. T2 Alcohol use | — | 0.04 | 0.00 | 0.01 | 0.78 ** | 2.30 | 2.21 | ||||||
| 9. T3 IPV | — | 0.25 ** | 0.26 ** | 0.01 | -- | -- | |||||||
| 10. T3 PTSD | — | 0.79 ** | 0.00 | 20.67 | 20.01 | ||||||||
| 11. T3 Depression | — | 0.00 | 6.52 | 6.23 | |||||||||
| 12. T3 Alcohol use | — | 3.83 | 3.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iverson, K.M.; Rossi, F.S.; Nillni, Y.I.; Fox, A.B.; Galovski, T.E. PTSD and Depression Symptoms Increase Women’s Risk for Experiencing Future Intimate Partner Violence. Int. J. Environ. Res. Public Health 2022, 19, 12217. https://doi.org/10.3390/ijerph191912217
Iverson KM, Rossi FS, Nillni YI, Fox AB, Galovski TE. PTSD and Depression Symptoms Increase Women’s Risk for Experiencing Future Intimate Partner Violence. International Journal of Environmental Research and Public Health. 2022; 19(19):12217. https://doi.org/10.3390/ijerph191912217
Chicago/Turabian StyleIverson, Katherine M., Fernanda S. Rossi, Yael I. Nillni, Annie B. Fox, and Tara E. Galovski. 2022. "PTSD and Depression Symptoms Increase Women’s Risk for Experiencing Future Intimate Partner Violence" International Journal of Environmental Research and Public Health 19, no. 19: 12217. https://doi.org/10.3390/ijerph191912217
APA StyleIverson, K. M., Rossi, F. S., Nillni, Y. I., Fox, A. B., & Galovski, T. E. (2022). PTSD and Depression Symptoms Increase Women’s Risk for Experiencing Future Intimate Partner Violence. International Journal of Environmental Research and Public Health, 19(19), 12217. https://doi.org/10.3390/ijerph191912217







