Health Promotion Programs Can Mitigate Public Spending on Hospitalizations for Stroke: An Econometric Analysis of the Health Gym Program in the State of Pernambuco, Brazil
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Empirical Strategy
2.2. Databases and Study Variables
2.3. Data Analysis
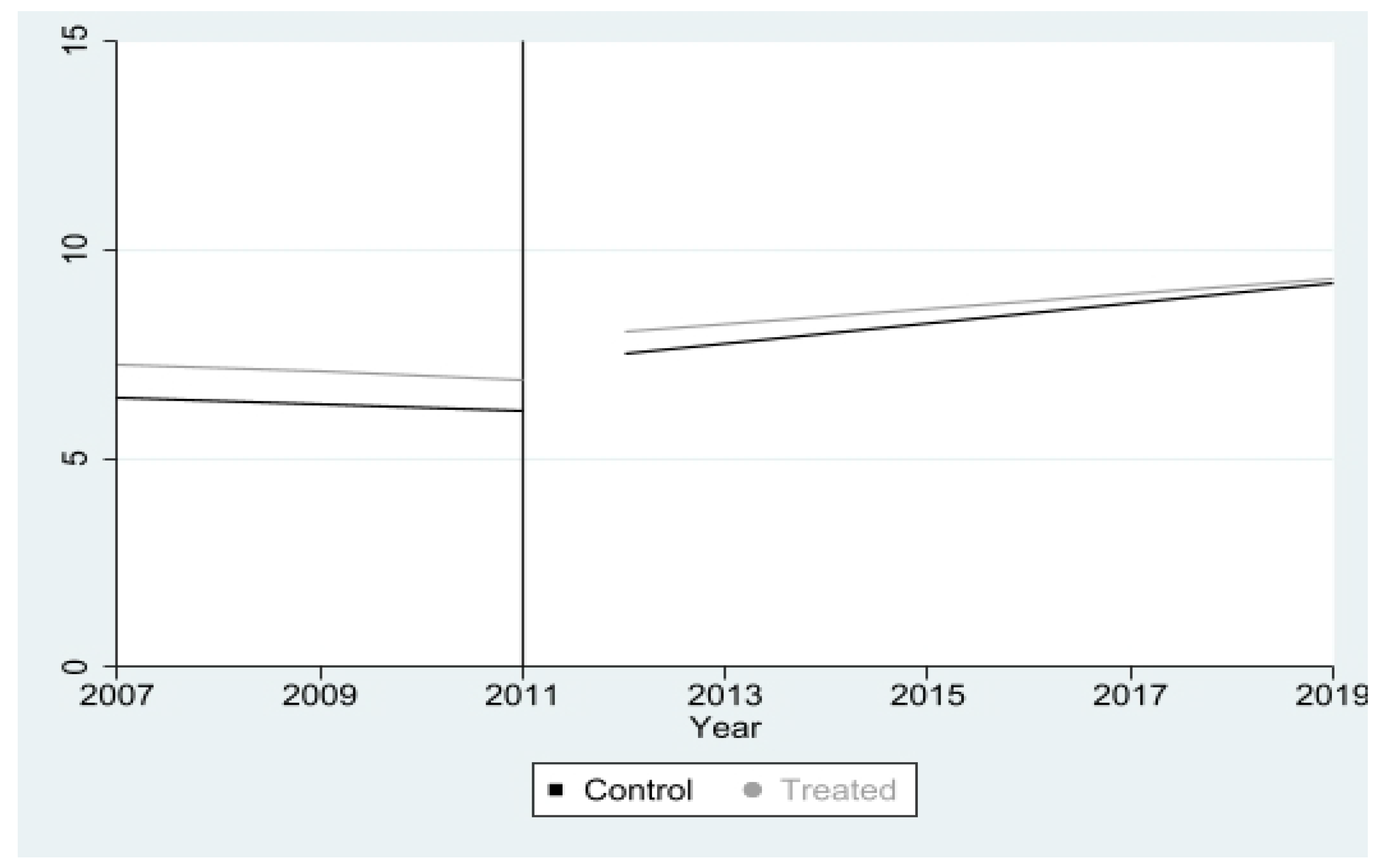
2.3.1. Pre-Tests of the Model
2.3.2. Estimation of the PSM-DID Model
2.3.3. Validation Post-Tests of the Results Found
3. Results
3.1. Health, Demographic, and Socioeconomic Characteristics of the Municipalities
3.2. Model Estimation Pre-Tests
3.3. Estimation of PSM, DID, and PSM-DID Models
3.4. Post-Estimation and Model Robustness Tests
4. Discussion
5. Conclusions
5.1. Limitations and Future Studies
5.2. Implications to Public Health
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, H.; Naghavi, M.; Allen, C.; Barber, R.M.; Bhutta, Z.A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; Coates, M.M.; et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef]
- Avan, A.; Digaleh, H.; Di Napoli, M.; Stranges, S.; Behrouz, R.; Shojaeianbabaei, G.; Amiri, A.; Tabrizi, R.; Mokhber, N.; Spence, J.D.; et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: An ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019, 17, 191. [Google Scholar] [CrossRef]
- Rajsic, S.; Gothe, H.; Borba, H.; Al, E. Economic burden of stroke: A systematic review on post-stroke care. Eur. J. Health Econ. 2018, 20, 107–134. [Google Scholar] [CrossRef] [PubMed]
- Barreto, I.d.J.B.; da Guarda, F.R.B.; da Silva, R.N.; de Farias, S.J.M.; da Silva, A.E.A.; Silva, P.B.C. Gastos Com Internações Hospitalares Por Doenças Relacionadas À Inatividade Física No Brasil. Lect. Educ. Fís. Deportes 2020, 25, 29–43. [Google Scholar] [CrossRef]
- De Santana, N.M.; Dos Santos Figueiredo, F.W.; De Melo Lucena, D.M.; Soares, F.M.; Adami, F.; De Carvalho Pádua Cardoso, L.; Correa, J.A. The burden of stroke in Brazil in 2016: An analysis of the Global Burden of Disease study findings 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Res. Notes 2018, 11, 735. [Google Scholar] [CrossRef]
- Soares, G.P.; Klein, C.H.; Souza e Silva, N.A.; Moraes, G.M. Evolução da mortalidade por doenças do aparelho circulatório e do Produto Interno Bruto per capita nos municípios do Estado do Rio de Janeiro TT—Evolution of mortality from diseases of the circulatory system and of gross domestic product per capita in. Int. J. Cardiovasc. Sci. 2018, 31, 123–132. [Google Scholar]
- Figueiredo, F.S.F.; da Silva Rodrigues, T.F.C.; da Silva Rêgo, A.; de Andrade, L.; de Oliveira, R.R.; Radovanovic, C.A.T. Distribution and spatial autocorrelation of the hospitalizations for cardiovascular diseases in adults in Brazil. Rev. Gaúch. Enferm. 2020, 41, e20190314. [Google Scholar] [CrossRef]
- Reis, M.; Chaoubah, A.; Mármora, C.; Liebel, G. Análise do gasto ambulatorial do acidente vascular cerebral na perspectiva do sistema público. J. Bras. Econ. Saúde 2018, 10, 219–225. [Google Scholar] [CrossRef]
- Poorthuis, M.; Algra, A.M.; Algra, A.; Kappelle, L.J.; Klijn, C. Female- and Male-Specific Risk Factors for Stroke: A Systematic Review and Meta-analysis. JAMA Neurol. 2017, 74, 75–81. [Google Scholar] [CrossRef]
- Rodrigues, M.D.S.; Fernandes e Santana, L.; Galvão, I.M. Fatores de risco modificáveis e não modificáveis do AVC isquêmico: Uma abordagem descritiva. Rev. Med. 2017, 96, 187. [Google Scholar] [CrossRef]
- Ministério de Saúde. Diretrizes de Atenção à Reabilitação da Pessoa com Acidente Vascular Cerebral; Ministério de Saúde: Brasília, Brazil, 2013. [Google Scholar]
- Kyu, H.H.; Bachman, V.F.; Alexander, L.T.; Mumford, J.E.; Afshin, A.; Estep, K.; Veerman, J.L.; Delwiche, K.; Iannarone, M.L.; Moyer, M.L.; et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: Systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ 2016, 354, i3857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eckermann, S.; Willan, A.R. Active Lives South Australia health economic analysis: An evidence base for the potential of health promotion strategies supporting physical activity guidelines to reduce public health costs while improving wellbeing. J. Public Health 2021, 30, 1791–1807. [Google Scholar] [CrossRef] [PubMed]
- de Cássia Franciele Lima, R.; Rodrigues, B.L.S.; de Farias, S.J.M.; Lippo, B.R.D.S.; da Guarda, F.R.B. Impacto do Programa Academia da Saúde sobre gastos com internações hospitalares por doenças cerebrovasculares. Rev. Bras. Ativ. Fís. Saúde 2020, 25, 1–8. [Google Scholar] [CrossRef]
- da Silva, R.N.; da Guarda, F.R.B.; Hallal, P.C.; de Lima Martelli, P.J. Avaliabilidade do Programa Academia da Saúde no Município do Recife, Pernambuco, Brasil. Cad. Saúde Pública 2017, 33, e00159415. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.P.; Andrade, A.C.D.S.; Costa, D.A.D.S.; Dias, M.A.D.S.; Malta, D.C.; Caiaffa, W.T. Programa academias da saúde e a promoção da atividade física na cidade: A experiência de Belo Horizonte, MG, Brasil. Cienc. Saude Coletiva 2017, 22, 3903–3914. [Google Scholar] [CrossRef]
- Ministério da Saúde. Manuais Técnicos de Implantação do Programa Academia da Saúde, 1st ed.; Ministério da Saúde: Brasília, Brazil, 2014. [Google Scholar]
- de Sá, G.B.A.R.; Dornelles, G.C.; Cruz, K.G.; de Araújo Amorim, R.C.; de Araújo Andrade, S.S.C.; Oliveira, T.P.; da Silva, M.M.A.; Malta, D.C.; de Souza, M.d.F.M. O Programa Academia da Saúde como estratégia de promoção da saúde e modos de vida saudáveis: Cenário nacional de implementação. Cienc. Saude Coletiva 2016, 21, 1849–1860. [Google Scholar] [CrossRef]
- Ministério da Saúde. Cadastro Nacional de Estabelecimentos de Saúde. Estabelecimentos por Tipo—Pernambuco. 2022. Available online: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?cnes/cnv/estabpe.def (accessed on 19 July 2022).
- Simões, E.J.; Hallal, P.C.; Siqueira, F.V.; Schmaltz, C.; Menor, D.; Malta, D.C.; Duarte, H.; Hino, A.A.; Mielke, G.I.; Pratt, M.; et al. Effectiveness of a scaled up physical activity intervention in Brazil: A natural experiment. Prev. Med. 2017, 103, S66–S72. [Google Scholar] [CrossRef]
- Rodrigues, B.L.S.; da Silva, R.N.; de Arruda, R.G.; Silva, P.B.C.; da Silva Feitosa, D.K.; da Guarda, F.R.B. Impact of the Health Gym Program on mortality from Systemic Arterial Hypertension in Pernambuco state, Brazil. Cienc. Saude Coletiva 2021, 26, 6199–6210. [Google Scholar] [CrossRef]
- da Guarda, F.R. A Brief Overview on the Methods of Impact Evaluation of Public Policies. Biomed. J. Sci. Tech. Res. 2021, 37, 29707–29711. [Google Scholar] [CrossRef]
- Lechner, M. The estimation of causal effects by difference-in-difference methods. Found. Trends Econom. 2010, 4, 165–224. [Google Scholar] [CrossRef]
- Fredriksson, A.; de Oliveira, G.M. Impact evaluation using Difference-in-Differences. RAUSP Manag. J. 2019, 54, 519–532. [Google Scholar] [CrossRef]
- Athey, S.; Imbens, G.W. The state of applied econometrics: Causality and policy evaluation. J. Econ. Perspect. 2017, 31, 3–32. [Google Scholar] [CrossRef]
- Angrist, J.; Pischke, J.-S. Mostly Harmless Econometrics: An Empiricist’s Companion; Princeton University Press: Princeton, NJ, USA, 2008. [Google Scholar]
- Heckman, J.; Ichimura, H.; Smith, J.; Todd, P. Characterizing Selection Bias Using Experimental Data. Econometrica 1998, 66, 1017–1098. [Google Scholar] [CrossRef]
- Becker, S.O.; Ichino, A. Estimation of Average Treatment Effects Based on Propensity Scores. Stata J. Promot. Commun. Stat. Stata 2002, 2, 1–19. [Google Scholar] [CrossRef]
- Wooldridge, J. Introdução à Econometria: Uma Abordagem Moderna, 3rd ed.; Cengage Learning: São Paulo, Brasil, 2016. [Google Scholar]
- Machado, C.S.R.; da Cruz Lima, A.C. Distribuição Espacial do sus e Determinantes das Despesas. Rev. Econ. Nordeste 2021, 52, 121–145. [Google Scholar]
- Oliveira, T.L.; Santos, C.M.; Miranda, L.D.P.; Nery, M.L.F.; Caldeira, A.P. Fatores associados ao custo das internações hospitalares por doenças sensíveis à Atenção Primária no Sistema Único de Saúde. Cien. Saude Coletiva 2021, 26, 4541–4552. [Google Scholar] [CrossRef]
- de Sousa Botelho, T.; Neto, C.D.M.; de Araújo, F.L.C.; de Assis, S.C. Epidemiologia do acidente vascular cerebral no Brasil Epidemiology. Temas Saúde 2016, 16, 361–377. [Google Scholar]
- Canavire-Bacarreza, G.; Peñarrieta, L.C.; Ontiveros, D.U. Outliers in semi-parametric estimation of treatment effects. Econometrics 2021, 9, 19. [Google Scholar] [CrossRef]
- Brooks, C. Introductory Econometrics for Finance; Cambridge University Press: Cambridge, UK, 2019. [Google Scholar] [CrossRef]
- Khandker, S.R.; Koolwal, G.B.; Samad, H.A. Handbook on Impact Evaluation: Quantitative Methods and Practices; The World Bank: Washington, DC, USA, 2010. [Google Scholar]
- Gertler, P.; Martinez, S.; Premand, P.; Rawlings, L.; Vermeersch, C. Impact Evaluation in Practice; The World Bank: Washington, DC, USA, 2010. [Google Scholar] [CrossRef]
- Greene, W. Econometric Analysis, 8th ed.; Pearson: London, UK, 2017. [Google Scholar]
- Stuart, E.A. Matching methods for causal inference: A review and a look forward. Stat. Sci. 2010, 25, 1–21. [Google Scholar] [CrossRef]
- Rubin, D.B.; Thomas, N. Matching Using Estimated Propensity Scores: Relating Theory to Practice. Biometrics 1996, 52, 249–264. [Google Scholar] [CrossRef]
- Stock, J.H.; Watson, M.W. Heteroskedasticity-robust standard errors for fixed effects panel data regression. Econometrica 2008, 76, 155–174. [Google Scholar] [CrossRef] [Green Version]
- Imbens, G.W.; Kolesár, M. Robust standard errors in small samples: Some practical advice. Rev. Econ. Stat. 2016, 98, 701–712. [Google Scholar] [CrossRef]
- Hoechle, D. Robust standard errors for panel regressions with cross-sectional dependence. Stata J. 2007, 7, 281–312. [Google Scholar] [CrossRef]
- Cameron, C.A.; Gelbach, J.B.; Miller, D.L. Bootstrap-based improvements for inference with clustered errors. Rev. Econ. Stat. 2008, 90, 414–427. [Google Scholar] [CrossRef]
- Wilkins, A.S. To lag or not to lag?: Re-evaluating the use of lagged dependent variables in regression analysis. Polit. Sci. Res. Methods 2018, 6, 393–411. [Google Scholar] [CrossRef]
- Malani, A.; Reif, J. Interpreting pre-trends as anticipation: Impact on estimated treatment effects from tort reform. J. Public Econ. 2015, 124, 1–17. [Google Scholar] [CrossRef]
- Dantas, L.F.; Marchesi, J.F.; Peres, I.T.; Hamacher, S.; Bozza, F.A.; Quintano Neira, R.A. Public hospitalizations for stroke in Brazil from 2009 to 2016. PLoS ONE 2019, 14, e0213837. [Google Scholar] [CrossRef]
- Foguel, M. Modelo de Resultados Potenciais. In Avaliação Econômica de Projetos Sociais, 3rd ed.; Menezes-Filho, N.A., Pinto, C.C.X., Eds.; Fundação Itaú Social: São Paulo, Brazil, 2017. [Google Scholar]
- Collischon, M. Methods to estimate causal effects An Overview on IV, DiD, and RDD and a Guide on How to Apply them in Practice. Work. Pap. 2022. [Google Scholar] [CrossRef]
- Lopes, J.M.; Sanchis, G.J.B.; de Medeiros, J.L.A.; Dantas, F.G. Hospitalização por acidente vascular encefálico isquêmico no Brasil: Estudo ecológico sobre possível impacto do Hiperdia. Rev. Bras. Epidemiol. 2016, 19, 122–134. [Google Scholar] [CrossRef]
- Pazó, R.G.; de Oliveira Frauches, D.; Maria, D.C.B.M.; Cade, N.V. Modelagem hierárquica de determinantes associados a internações por condições sensíveis à atenção primária no Espírito Santo, Brasil. Cad. Saude Publica 2014, 30, 1891–1901. [Google Scholar] [CrossRef]
- Caliendo, M.; Kopeinig, S. Some practical guidance for the implementation of propensity score matching. J. Econ. Surv. 2008, 22, 31–72. [Google Scholar] [CrossRef] [Green Version]
- Rubin, D.B. Using propensity scores to help design observational studies: Application to the tobacco litigation. Health Serv. Outcomes Res. Methodol. 2001, 2, 169–188. [Google Scholar] [CrossRef]
- Pernambuco. Receita da Secretaria de Estado da Saúde em 2019. Portal Da Transparência Painel Receitas 2019. Website of the Transparency Program in the Public Accounts of the State of Pernambuco, Brazil. Available online: http://web.transparencia.pe.gov.br/receitas/painel-de-receitas/ (accessed on 14 September 2022).
- SIOPSSistema de Informações de Orçamentos Públicos. Indicadores Municipais. Despesa Total em Saúde dos Municípios de Pernambuco em 2019. TabNet Win32 30 Indicadores Munic 2019. Available online: datasus.gov.br (accessed on 14 September 2022).
- Grazioli, E.; Dimauro, I.; Mercatelli, N.; Wang, G.; Pitsiladis, Y.; Di Luigi, L.; Caporossi, D. Physical activity in the prevention of human diseases: Role of epigenetic modifications. BMC Genom. 2017, 18, 802. [Google Scholar] [CrossRef]
- Tusset, D.; Olkoski, M.; Merchan-Hamann, E.; Calmon, P.C.D.P.; dos Santos, L. Programa Academia da Saúde: Um olhar quantitativo das adesões entre 2011 a 2017. Rev. Bras. Ativ. Fis. Saúde 2020, 25, 1–9. [Google Scholar] [CrossRef]
- Austin, P.C. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm. Stat. 2011, 10, 150–161. [Google Scholar] [CrossRef]
- Haque, M.; Islam, T.; Rahman, N.A.A.; McKimm, J.; Abdullah, A.; Dhingra, S. Strengthening Primary Health-Care Services to Help Prevent and Control Long-Term (Chronic) Non-Communicable Diseases in Low- and Middle-Income Countries. Risk Manag. Healthc. Policy 2020, 13, 409–426. [Google Scholar] [CrossRef] [PubMed]
- Malta, D.C.; Morais Neto, O.L.; da Silva, M.M.A.; Rocha, D.; de Castro, A.M.; dos Reis, A.A.C.; Akerman, M. Política Nacional de Promoção da Saúde (PNPS): Capítulos de uma caminhada ainda em construção. Cien. Saude Coletiva 2016, 21, 1683–1694. [Google Scholar] [CrossRef] [Green Version]
| Variables | Control (0) | Treated (1) | Relative Difference in Mean * (0/1) | p-Value | ||
|---|---|---|---|---|---|---|
| Mean * | SD | Mean * | SD | |||
| Health | ||||||
| Hosp spend per stroke ** | 4621.18 | 1155.20 | 11,886.13 | 1169.94 | −7264.94 | <0.001 |
| No. of doctors ** | 14.22 | 0.92 | 68.94 | 9.3 | −54.71 | <0.001 |
| No. of beds | 38.32 | 2.01 | 115.51 | 13.07 | −77.19 | <0.001 |
| Demographic | ||||||
| Pop > 40 years *** | 3847.14 | 119.76 | 8690.88 | 587.06 | −4843.74 | <0.001 |
| Rt pass HS | 86.27 | 0.33 | 86.72 | 0.2 | −0.45 | 0.244 |
| Socioeconomic | ||||||
| GDP per capita | 275,452.22 | 16,022.33 | 289,650.13 | 10,824.95 | −14,197.90 | 0.480 |
| Total Health Expenditure | 4,848,757.54 | 151,985.75 | 11,150,605.58 | 904,148.96 | −6,301,848.04 | <0.001 |
| Variables | Before Matching | % Bias Reduction | After Matching | ||||
|---|---|---|---|---|---|---|---|
| Treated | Control | p-Value | Treated | Control | p-Value | ||
| >40 years/10,000 inhab | 3154 | 3005.4 | <0.001 | 97.9 | 3138.7 | 3141.8 | 0.811 |
| Log no. of doctors | 2.52 | 2.064 | <0.001 | 94.8 | 2.305 | 2.329 | 0.551 |
| No. of hosp beds. SUS | 116.56 | 39.452 | 0.001 | 95.8 | 53.416 | 50.187 | 0.218 |
| Presence of NASF | 0.586 | 0.561 | 0.292 | −1.4 | 0.568 | 0.593 | 0.161 |
| Total Health Expenditure | 105,912,295.91 | 44,314,883.50 | <0.001 | 99.1 | 55,848,149.88 | 55,507,149.30 | 0.780 |
| Rt pass HS | 86.138 | 85.631 | 0.211 | 92.6 | 86.286 | 86.324 | 0.902 |
| GDP per capita | 2,753,400.11 | 2,816,644.81 | 0.481 | 90.7 | 2,731,272.41 | 2,727,414.55 | 0.923 |
| Balancing Conditions (Rubin statistics) | |||||||
| B | 19.0 | ||||||
| R | 0.83 | ||||||
| Panel B—Common support of matching between treated and untreated groups | |||||||
| Out of Support | Common Support | Total | % of Participation | ||||
| Control | 0 | 606 | 606 | 100 | |||
| Treated | 92 | 1509 | 1601 | 94.25 | |||
| Total | 92 | 2115 | 2207 | 95.83 | |||
| Variables | DID | PSM-DID | Placebo Regression | |||
|---|---|---|---|---|---|---|
| Log Stroke Expenditure * | Standard Error | Stroke Expenditure * | Standard Error | Hosp for Hypertension | Standard Error | |
| HGP | −0.1793 b | 0.089 | −0.1785 b | 0.089 | 0.1447 | −2.302 |
| Propensity Score | - | - | 1.228 | −1.051 | −7.631 | 30.65 |
| >40 years/10,000 inhab | 0.002 a | <0.001 | 0.002 a | 0.001 | −0.011 | 0.019 |
| Log no. of doctors | −0.093 | 0.065 | −0.118 c | 0.067 | −0.442 | 0.993 |
| No. of hosp. Beds. | −0.000 | 0.001 | −0.001 | 0.001 | 0.005 | 0.017 |
| Presence of NASF-AB | −0.014 | 0.086 | 0.088 | 0.111 | −2.784 | −3.115 |
| Total Health Expenditure | 0.000 a | <0.001 | <0.001 a | 0.000 | −0.000 b | <0.001 |
| Rt pass high school | 0.014 a | 0.005 | 0.014 a | 0.005 | −0.024 | 0.122 |
| GBP per capita | 0.000 a | <0.001 | <0.001 a | <0.001 | <0.001 | <0.001 |
| outlier | −7.208 a | 0.140 | −7.176 a | 0.145 | 0.760 | −1.890 |
| Time of Exposure | ||||||
| 1st Year | −0.436 c | 0.251 | −0.346 | 0.258 | −1.780 | −8.426 |
| 2nd Year | −0.487 a | 0.233 | −0.408 c | 0.237 | −1.328 | −7.388 |
| 3rd Year | 0.108 | 0.195 | 0.174 | 0.201 | −1.324 | −6.066 |
| 4th Year | 0.366 b | 0.168 | 0.416 b | 0.173 | −0.695 | −4.713 |
| 5th Year | 0.222 | 0.148 | 0.268 c | 0.153 | −2.372 | −3.842 |
| 6th Year | −0.034 | 0.110 | 0.003 | 0.116 | −1.719 | −2.491 |
| 7th Year | 0.092 | 0.0913 | 0.121 | 0.097 | −0.874 | −1.588 |
| 8th Year | −0.452 | 0.411 | −0.581 | 0.421 | 0.140 | 11.155 |
| Constant | 0.962 | 1.842 | 0.962 | 1.842 | 65.03 | 56.18 |
| R2 | 0.855 | 0.855 | 0.134 | |||
| Stroke | Coeficiente | Standard-Error | z | p-Value | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| lead2 | 0.252 | 0.197 | 10.28 | 0.201 | −0.134 | 0.64 |
| lead1 | 0.081 | 0.193 | 0.42 | 0.675 | −0.298 | 0.461 |
| treat | −0.023 | 0.191 | −0.12 | 0.904 | −0.398 | 0.352 |
| lag1 | −0.45 | 0.191 | −20.35 | 0.019 | −0.825 | −0.075 |
| lag2 | −0.596 | 0.191 | −30.12 | 0.002 | −0.971 | −0.222 |
| _cons | 7.95 | 0.128 | 61.86 | <0.001 | 7.703 | 8.207 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Guarda, F.R.B. Health Promotion Programs Can Mitigate Public Spending on Hospitalizations for Stroke: An Econometric Analysis of the Health Gym Program in the State of Pernambuco, Brazil. Int. J. Environ. Res. Public Health 2022, 19, 12174. https://doi.org/10.3390/ijerph191912174
da Guarda FRB. Health Promotion Programs Can Mitigate Public Spending on Hospitalizations for Stroke: An Econometric Analysis of the Health Gym Program in the State of Pernambuco, Brazil. International Journal of Environmental Research and Public Health. 2022; 19(19):12174. https://doi.org/10.3390/ijerph191912174
Chicago/Turabian Styleda Guarda, Flávio Renato Barros. 2022. "Health Promotion Programs Can Mitigate Public Spending on Hospitalizations for Stroke: An Econometric Analysis of the Health Gym Program in the State of Pernambuco, Brazil" International Journal of Environmental Research and Public Health 19, no. 19: 12174. https://doi.org/10.3390/ijerph191912174
APA Styleda Guarda, F. R. B. (2022). Health Promotion Programs Can Mitigate Public Spending on Hospitalizations for Stroke: An Econometric Analysis of the Health Gym Program in the State of Pernambuco, Brazil. International Journal of Environmental Research and Public Health, 19(19), 12174. https://doi.org/10.3390/ijerph191912174






