Craniofacial Growth and Asymmetry in Newborns: A Longitudinal 3D Assessment
Abstract
1. Background
2. Materials and Methods
2.1. Participants
2.2. Acquisition of 3D Images
2.3. Selection of Qualified 3D Images
2.4. Head and Body Measurements
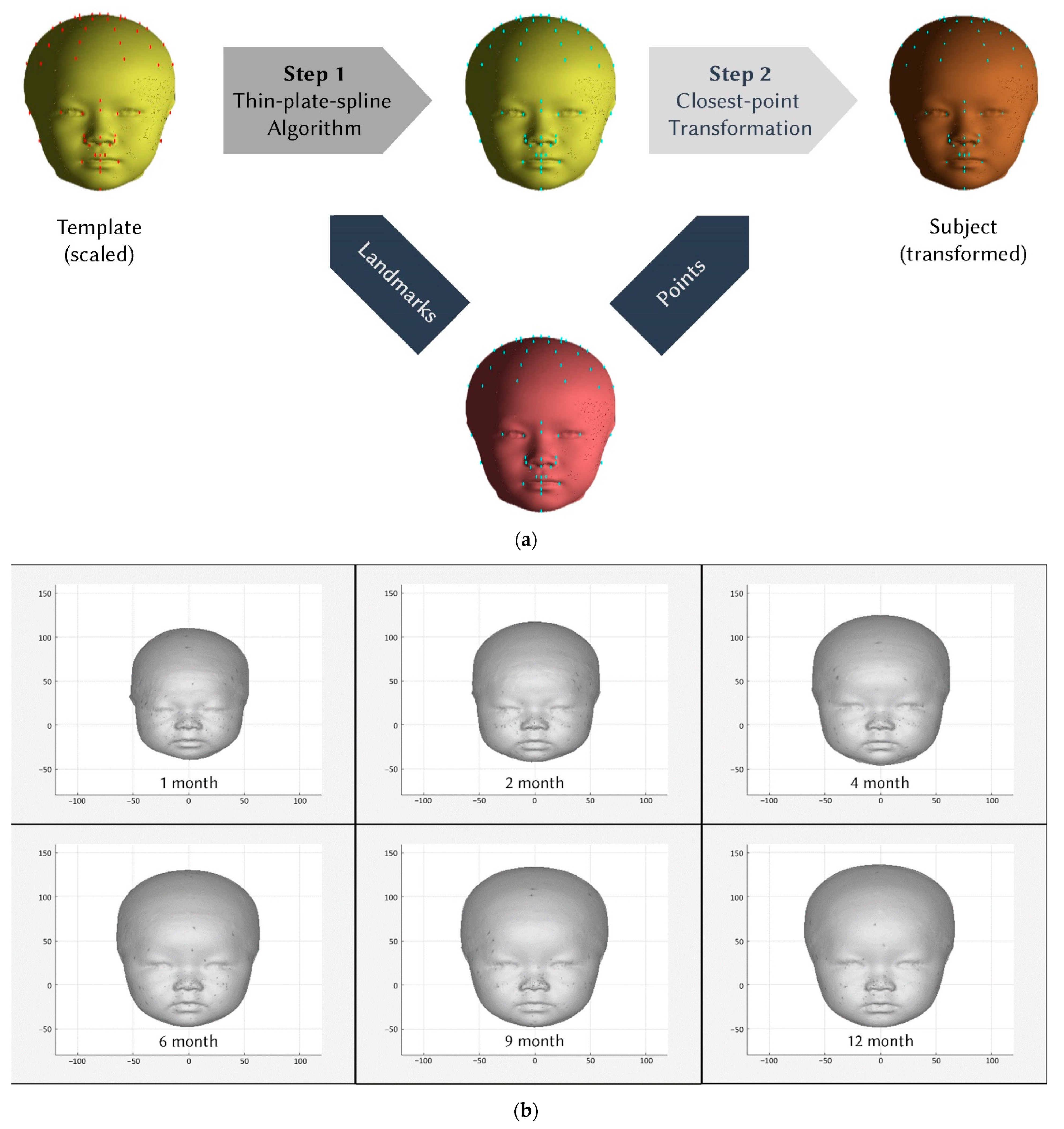
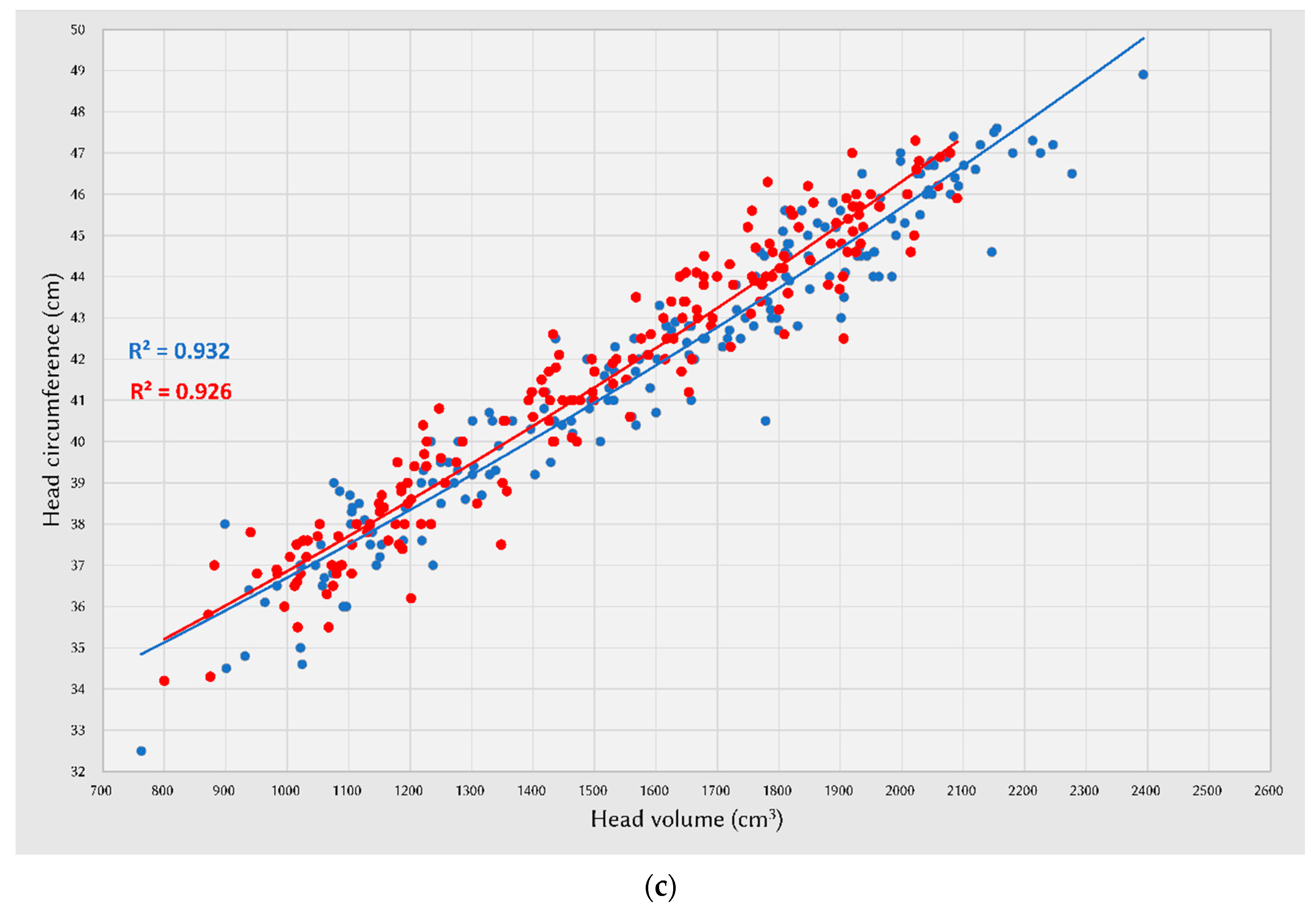
2.5. Whole-Head 3D Image Processing
2.6. Anthropometric Measurements from 3D Scans
2.7. Statistical Analysis
3. Results
4. Discussion
4.1. Data Interpretation of Craniofacial Norms
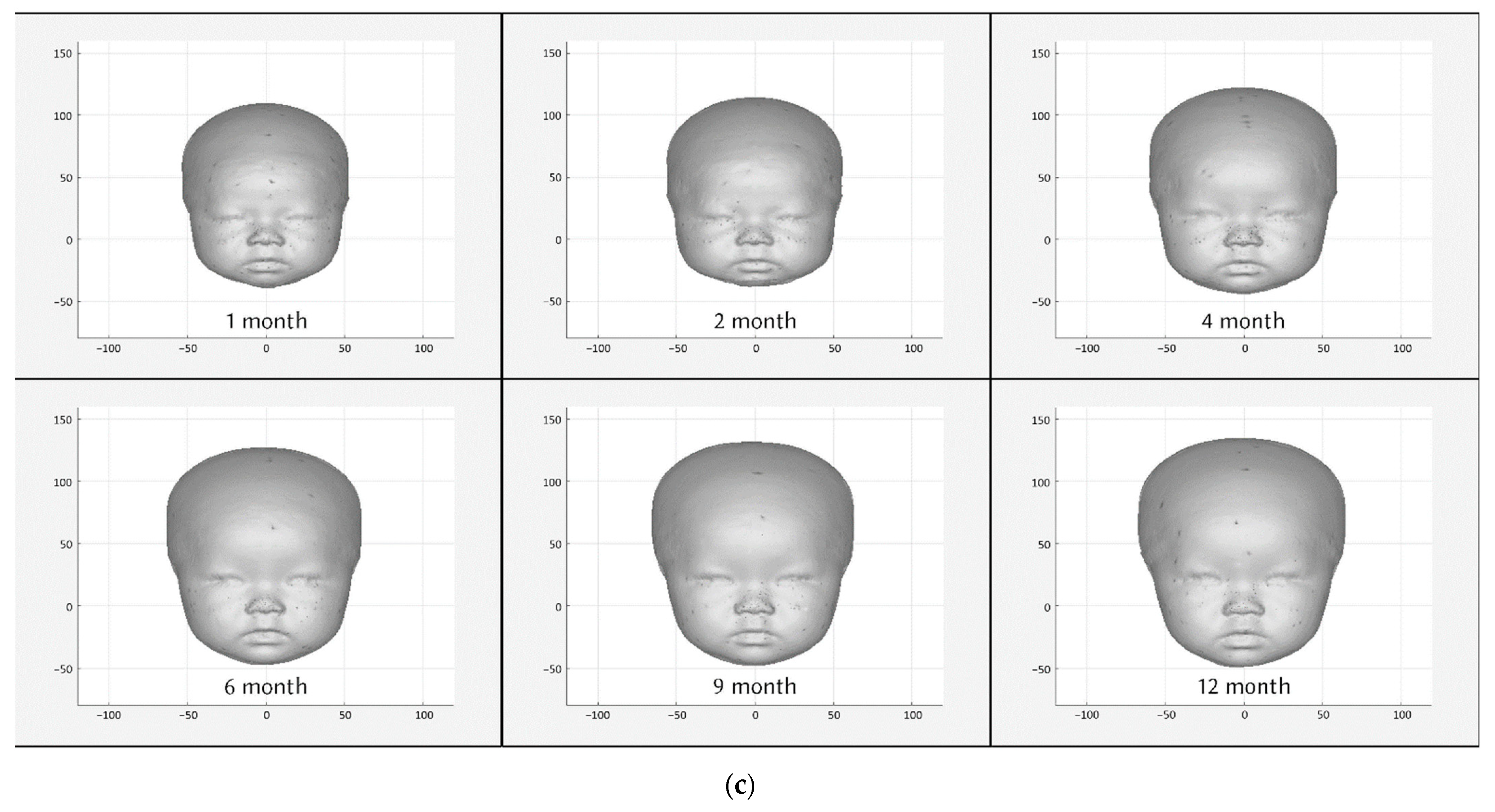
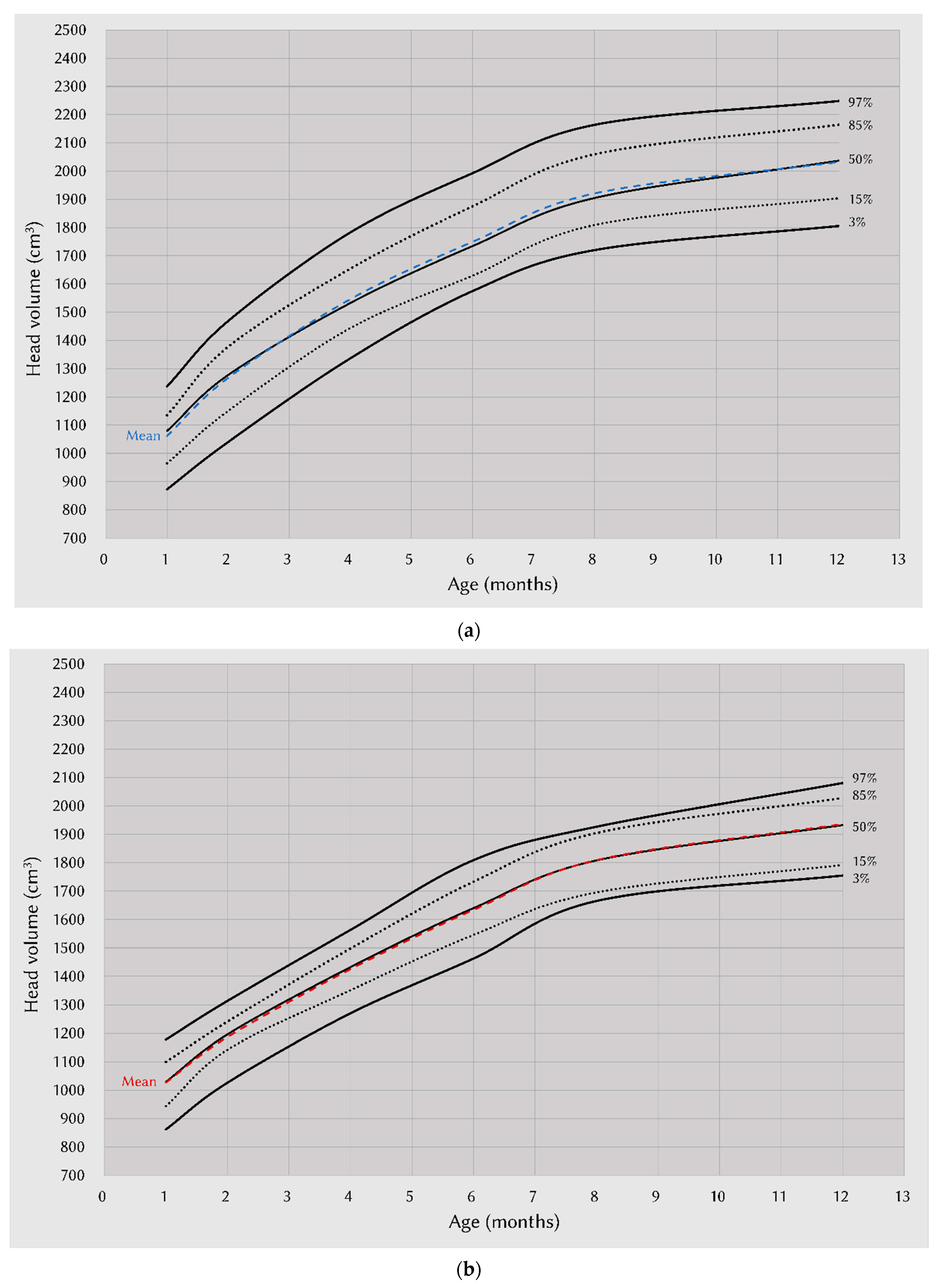
4.2. Growth Charts of Head Volume and Head Circumference
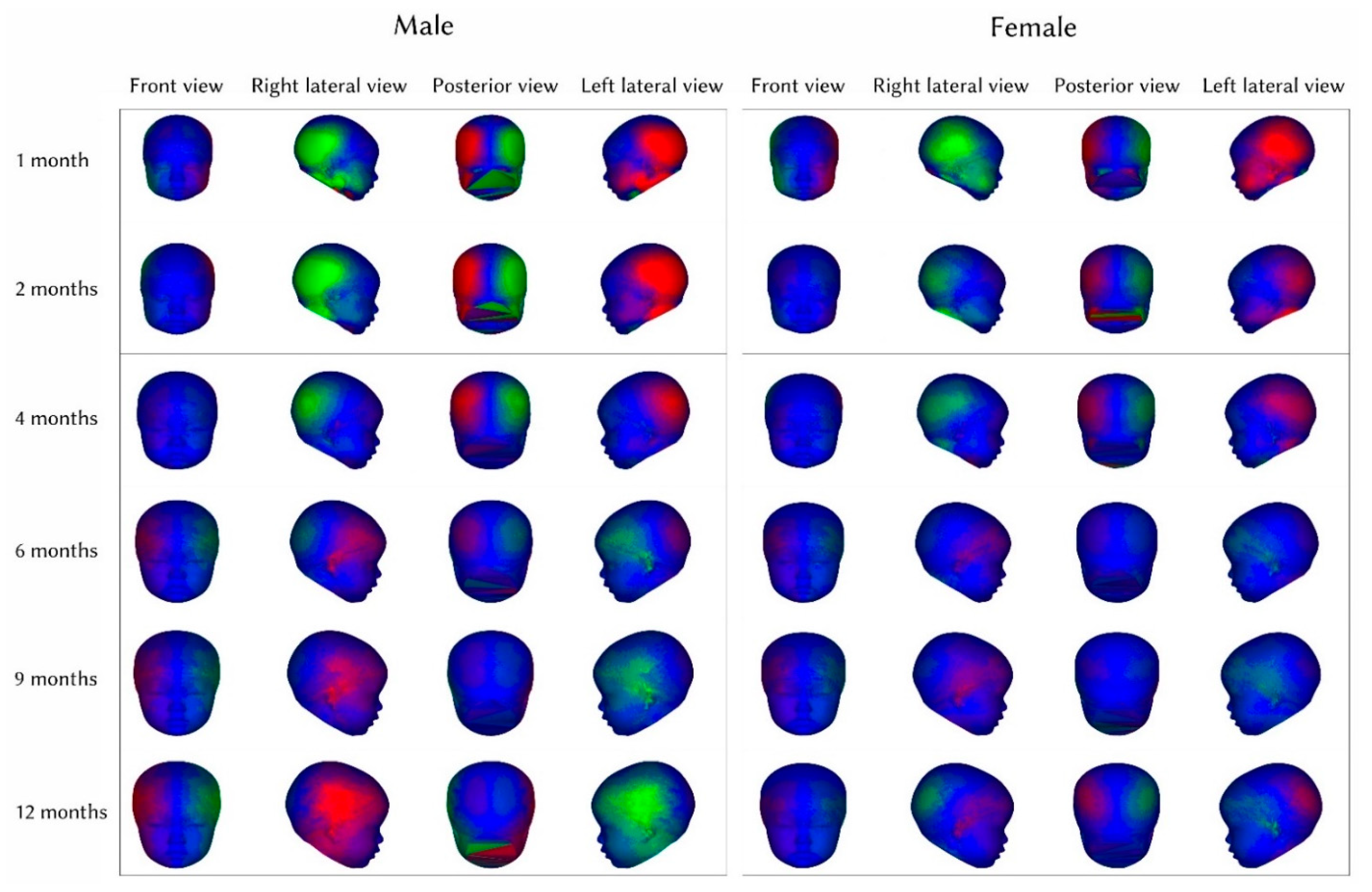
4.3. Interpretations of Craniofacial Asymmetry Score and Color-Asymmetry Maps
4.4. Strengths and Limitations of 3D Stereophotogrammetry
4.5. Application of Study Results
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grayson, B.H.; McCarthy, J.G.; Bookstein, F. Analysis of craniofacial asymmetry by multiplane cephalometry. Am. J. Orthod. 1983, 84, 217–224. [Google Scholar] [CrossRef]
- Ramamurthi, A.; Hallac, R.R.; Kenyon, L.E.; Thrikutam, N.; Warne, C.N.; Derderian, C.A. Three-dimensional Treatment Outcomes of a Virtual Helmet Design Protocol for Sagittal Strip Craniectomy. Plastic and reconstructive surgery. Glob. Open 2019, 7 (Suppl. S8), 55. [Google Scholar] [CrossRef]
- Farkas, L.G.; Bryson, W.; Klotz, J. Is photogrammetry of the face reliable? Plast Reconstr. Surg. 1980, 66, 346–355. [Google Scholar] [CrossRef]
- O’Grady, K.F.; Antonyshyn, O.M. Facial asymmetry: Three-dimensional analysis using laser surface scanning. Plast Reconstr. Surg. 1999, 104, 928–937. [Google Scholar] [CrossRef]
- Launonen, A.M.; Vuollo, V.; Aarnivala, H.; Heikkinen, T.; Pirttiniemi, P.; Valkama, A.M.; Harila, V. Craniofacial Asymmetry from One to Three Years of Age: A Prospective Cohort Study with 3D Imaging. J. Clin. Med. 2019, 9, 70. [Google Scholar] [CrossRef]
- Wong, J.Y.; Oh, A.K.; Ohta, E.; Hunt, A.T.; Rogers, G.F.; Mulliken, J.B.; Deutsch, C.K. Validity and Reliability of Craniofacial Anthropometric Measurement of 3D Digital Photogrammetric Images. Cleft Palate-Craniofac. J. 2008, 45, 232–239. [Google Scholar] [CrossRef]
- Lipira, A.B.; Sachanandani, N.S.; Govier, D.; Payne, A.; Wyas, S.; Kleeschulte, W.; Kane, A.A. Craniobank: An Online Collection of Three-Dimensional Normative Craniofacial Images. Plast. Reconstr. Surg. 2010, 126, 70e–72e. [Google Scholar]
- Hsu, C.K.; Hallac, R.R.; Denadai, R.; Wang, S.W.; Kane, A.A.; Lo, L.J.; Chou, P.Y. Quantifying normal head form and craniofacial asymmetry of elementary school students in Taiwan. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 2033–2040. [Google Scholar] [CrossRef]
- Farkas, L.G. Accuracy of Anthropometric Measurements: Past, Present, and Future. Cleft Palate-Craniofacial J. 1996, 33, 10–22. [Google Scholar] [CrossRef]
- Cho, M.J.; Hallac, R.R.; Ramesh, J.; Seaward, J.R.; Hermann, N.V.; Darvann, T.A.; Lipira, A.; Kane, A.A. Quantifying Normal Craniofacial Form and Baseline Craniofacial Asymmetry in the Pediatric Population. Plast. Reconstr. Surg. 2018, 141, 380e–387e. [Google Scholar] [CrossRef]
- Scheffler, C.; Greil, H.; Hermanussen, M. The association between weight, height, and head circumference reconsidered. Pediatr. Res. 2017, 81, 825–830. [Google Scholar] [CrossRef]
- Alherbish, A.; Mouzan, M.; Salloum, A.; Qureshi, M.; Omar, A.; Foster, P.; Kecojevic, T. Body mass index in Saudi Arabian children and adolescents: A national reference and comparison with international standards. Ann. Saudi Med. 2009, 29, 342–347. [Google Scholar] [CrossRef]
- Roy, S.M.; Spivack, J.G.; Faith, M.S.; Chesi, A.; Mitchell, J.A.; Kelly, A.; Grant, S.F.A.; McCormack, S.E.; Zemel, B.S. Infant BMI or Weight-for-Length and Obesity Risk in Early Childhood. Pediatrics 2016, 137, e20153492. [Google Scholar] [CrossRef]
- Tinggaard, J.; Aksglaede, L.; Sørensen, K.; Mouritsen, A.; Wohlfahrt-Veje, C.; Hagen, C.P.; Mieritz, M.G.; Jørgensen, N.; Wolthers, O.D.; Heuck, C.; et al. The 2014 Danish references from birth to 20 years for height, weight and body mass index. Acta Paediatr. 2014, 103, 214–224. [Google Scholar] [CrossRef]
- Woo, J.G.; Daniels, S.R. Assessment of Body Mass Index in Infancy: It Is Time to Revise Our Guidelines. J. Pediatr. 2019, 204, 10–11. [Google Scholar] [CrossRef]
- Rollins, J.D.; Collins, J.S.; Holden, K.R. United States Head Circumference Growth Reference Charts: Birth to 21 Years. J. Pediatr. 2010, 156, 907–913.e2. [Google Scholar] [CrossRef]
- Fenton, T.R.; Kim, J.H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013, 13, 59. [Google Scholar] [CrossRef]
- Villar, J.; Ismail, L.C.; Victora, C.G.; Ohuma, E.O.; Bertino, E.; Altman, D.G.; Lambert, A.; Papageorghiou, A.T.; Carvalho, M.; Jaffer, Y.A.; et al. International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014, 384, 857–868. [Google Scholar] [CrossRef]
- Lampl, M.; Johnson, M.L. Infant head circumference growth is saltatory and coupled to length growth. Early Hum. Dev. 2011, 87, 361–368. [Google Scholar] [CrossRef]
- Dupont, C.; Castellanos-Ryan, N.; Séguin, J.R.; Muckle, G.; Simard, M.-N.; Shapiro, G.D.; Herba, C.M.; Fraser, W.D.; Lippé, S. The Predictive Value of Head Circumference Growth during the First Year of Life on Early Child Traits. Sci. Rep. 2018, 8, 9828. [Google Scholar] [CrossRef]
- Breakey, R.W.F.; PKnoops, G.M.; Borghi, A.; Rodriguez-Florez, N.; O’Hara, J.; James, G.; Dunaway, D.J.; Schievano, S.; Jeelani, N.U.O. Intracranial Volume and Head Circumference in Children with Unoperated Syndromic Craniosynostosis. Plast Reconstr. Surg. 2018, 142, 708e–717e. [Google Scholar] [CrossRef]
- Hummel, P.; Fortado, D. Impacting infant head shapes. Adv. Neonatal Care 2005, 5, 329–340. [Google Scholar] [CrossRef]
- Hutchison, B.L.; Hutchison, L.A.; Thompson, J.M.; Mitchell, E.A. Plagiocephaly and Brachycephaly in the First Two Years of Life: A Prospective Cohort Study. Pediatrics 2004, 114, 970–980. [Google Scholar] [CrossRef]
- Nicholson, L. Caput Succedaneum and Cephalohematoma: The Cs that Leave Bumps on the Head. Neonatal Netw. 2007, 26, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Ditthakasem, K.; Kolar, J.C. Deformational Plagiocephaly: A Review. Pediatr. Nurs. 2017, 43, 59–64. [Google Scholar]
- Branch, L.G.; Kesty, K.; Krebs, E.; Wright, L.; Leger, S.; David, L.R. Deformational plagiocephaly and craniosynostosis: Trends in diagnosis and treatment after the “back to sleep” campaign. J. Craniofacial Surg. 2015, 26, 147–150. [Google Scholar] [CrossRef]
- Turk, A.E.; McCarthy, J.G.; Thorne, C.H.; Wisoff, J.H. The “back to sleep campaign” and deformational plagiocephaly: Is there cause for concern? J. Craniofac. Surg. 1996, 7, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Lottering, N.; Alston, C.L.; Barry, M.D.; MacGregor, D.M.; Gregory, L.S. Temporal mapping of the closure of the anterior fontanelle and contiguous sutures using computed tomography, in silico models of modern infants. J. Anat. 2020, 237, 379–390. [Google Scholar] [CrossRef]
- Vu, G.H.; Xu, W.; Go, B.C.; Humphries, L.S.; Kalmar, C.L.; Taylor, J.A.; Bartlett, S.P.; Vossough, A.; Nah-Cederquist, H.-D.; Swanson, J.W. Physiologic Timeline of Cranial-Base Suture and Synchondrosis Closure. Plast. Reconstr. Surg. 2021, 148, 973e–982e. [Google Scholar] [CrossRef] [PubMed]
- Mendonca, D.A.; Naidoo, S.D.; Skolnick, G.; Skladman, R.; Woo, A.S. Comparative Study of Cranial Anthropometric Measurement by Traditional Calipers to Computed Tomography and Three-dimensional Photogrammetry. J. Craniofacial Surg. 2013, 24, 1106–1110. [Google Scholar] [CrossRef]
- Lee, S. Three-Dimensional Photography and Its Application to Facial Plastic Surgery. Arch. Facial Plast. Surg. 2004, 6, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yang, X.; Li, D. The Application of Three-Dimensional Surface Imaging System in Plastic and Reconstructive Surgery. Ann. Plast. Surg. 2016, 77 (Suppl. S1), S76–S83. [Google Scholar] [CrossRef] [PubMed]
- Hajeer, M.Y.; Ayoub, A.F.; Millett, D.T.; Bock, M.; Siebert, J.P. Three-dimensional imaging in orthognathic surgery: The clinical application of a new method. Int. J. Adult Orthod. Orthognath. Surg. 2002, 17, 318–330. [Google Scholar]
- Heike, C.L.; Upson, K.; Stuhaug, E.; Weinberg, S.M. 3D digital stereophotogrammetry: A practical guide to facial image acquisition. Head Face Med. 2010, 6, 18. [Google Scholar] [CrossRef]
- Petrides, G.; Clark, J.R.; Low, H.; Lovell, N.; Eviston, T.J. Three-dimensional scanners for soft-tissue facial assessment in clinical practice. J. Plast. Reconstr. Aesthetic Surg. 2020, 74, 605–614. [Google Scholar] [CrossRef]
- Babczyńska, A.; Kawala, B.; Sarul, M. Genetic Factors That Affect Asymmetric Mandibular Growth—A Systematic Review. Symmetry 2022, 14, 490. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A. MSX1 gene in the etiology orofacial deformities. Postepy Hig. Med. Dosw. 2015, 69, 1499–1504. [Google Scholar]
- Georgakis, M.K.; Kalogirou, E.I.; Liaskas, A.; Karalexi, M.A.; Papathoma, P.; Ladopoulou, K.; Kantzanou, M.; Tsivgoulis, G.; Petridou, E.T. Anthropometrics at birth and risk of a primary central nervous system tumour: A systematic review and meta-analysis. Eur. J. Cancer 2017, 75, 117–131. [Google Scholar] [CrossRef]
- Harris, S.R. Measuring head circumference: Update on infant microcephaly. Can. Fam. Physici. 2015, 61, 680–684. [Google Scholar]
- Filteau, S.; Kumar, G.T.; Cole, T.J.; Sachdev, H.S.; de Stavola, B.L. Steady Growth in Early Infancy Is Associated with Greater Anthropometry in Indian Children Born Low Birth Weight at Term. J. Nutr. 2019, 149, 1633–1641. [Google Scholar] [CrossRef]
- Collett, B.R.; Starr, J.R.; Kartin, D.; Heike, C.L.; Berg, J.; Cunningham, M.L.; Speltz, M.L. Development in Toddlers With and Without Deformational Plagiocephaly. Arch. Pediatr. Adolesc. Med. 2011, 165, 653–658. [Google Scholar] [CrossRef] [PubMed]
- De Jong, G.; Bijlsma, E.; Meulstee, J.; Wennen, M.; van Lindert, E.; Maal, T.; Aquarius, R.; Delye, H. Combining deep learning with 3D stereophotogrammetry for craniosynostosis diagnosis. Sci. Rep. 2020, 10, 15346. [Google Scholar] [CrossRef] [PubMed]
- Paris, C.A.; Remler, R.; Daling, J.R. Risk factors for sudden infant death syndrome: Changes associated with sleep position recommendations. J. Pediatr. 2001, 139, 771–777. [Google Scholar] [CrossRef] [PubMed]
- AAP Task Force on Infant Positioning and SIDS. Positioning and SIDS. Pediatrics 1992, 89, 1120–1126. [Google Scholar] [CrossRef]
- Dwyer, T.; Ponsonby, A.L.; Newman, N.M.; Gibbons, L.E. Prospective cohort study of prone sleeping position and sudden infant death syndrome. Lancet 1991, 337, 1244–1247. [Google Scholar] [CrossRef]
- De Ribaupierre, S.; Vernet, O.; Rilliet, B.; Cavin, B.; Kalina, D.; Leyvraz, P. Posterior positional plagiocephaly treated with cranial remodeling orthosis. Swiss Med. Wkly. 2007, 137, 368–372. [Google Scholar] [PubMed]
- Kluba, S.; Kraut, W.; Reinert, S.; Krimmel, M. What is the optimal time to start helmet therapy in positional plagiocephaly? Plast Reconstr. Surg. 2011, 128, 492–498. [Google Scholar] [CrossRef]
- Blecher, J.C.; Howaldt, H.P. Treatment of non-synostotic head deformity in infants with dynamic orthosis. Mund. Kiefer Gesichtschir. 1998, 2 (Suppl. S1), S81–S85. [Google Scholar] [CrossRef]
- Wilbrand, J.-F.; Wilbrand, M.; Pons-Kuehnemann, J.; Blecher, J.-C.; Christophis, P.; Howaldt, H.-P.; Schaaf, H. Value and reliability of anthropometric measurements of cranial deformity in early childhood. J. Cranio-Maxillofac. Surg. 2011, 39, 24–29. [Google Scholar] [CrossRef]
- Torrey, E.F.; Dhavale, D.; Lawlor, J.P.; Yolken, R.H. Autism and head circumference in the first year of life. Biol. Psychiatry 2004, 56, 892–894. [Google Scholar] [CrossRef]
- Kamochi, H.; Sunaga, A.; Chi, D.; Asahi, R.; Nakagawa, S.; Mori, M.; Uda, H.; Sarukawa, S.; Sugawara, Y.; Yoshimura, K. Growth curves for intracranial volume in normal Asian children fortify management of craniosynostosis. J. Cranio-Maxillofac. Surg. 2017, 45, 1842–1845. [Google Scholar] [CrossRef] [PubMed]

| Head Height, mm (m ± SD) | Head Depth, mm (m ± SD) | Head Width, mm (m ± SD) | Head Volume, cm3 (m ± SD) | |||||
|---|---|---|---|---|---|---|---|---|
| Age/Sex | Male | Female | Male | Female | Male | Female | Male | Female |
| 1 month | 148.85 ± 7.38 | 146.28 ± 5.26 | 119.45 ± 7.09 | 119.55 ± 6.88 | 117.91 ± 5.34 | 115.46 ± 5.56 | 1061.10 ± 103.24 | 1027.38 ± 89.25 |
| 2 months | 158.50 ± 6.18 * | 152.41 ± 4.43 | 124.42 ± 6.15 | 122.35 ± 6.18 | 126.75 ± 6.58 * | 122.66 ± 6.96 | 1267.04 ± 130.18 * | 1186.42 ± 74.18 |
| 4 months | 168.01 ± 6.44 * | 162.32 ± 4.40 | 130.59 ± 5.97 | 128.97 ± 5.85 | 137.48 ± 6.02 * | 129.57 ± 6.35 | 1545.80 ± 129.74 * | 1425.21 ± 78.78 |
| 6 months | 175.51 ± 5.49 * | 170.11 ± 5.13 | 135.80 ± 6.17 | 134.66 ± 6.73 | 140.84 ± 6.70 * | 134.06 ± 7.44 | 1748.97 ± 133.23 * | 1634.00 ± 91.88 |
| 9 months | 179.81 ± 5.59 * | 175.07 ± 5.46 | 141.39 ± 6.52 | 140.40 ± 6.09 | 144.71 ± 7.64 * | 138.80 ± 7.38 | 1920.66 ± 153.04 * | 1809.08 ± 88.14 |
| 12 months | 183.17 ± 5.45 * | 178.67 ± 4.97 | 145.68 ± 6.97 | 145.49 ± 5.72 | 144.46 ± 8.08 | 141.41 ± 7.57 | 2031.78 ± 133.02 * | 1935.86 ± 100.18 |
| Body Height, cm (m ± SD) | Body Weight, kg (m ± SD) | BMI, kg/m2 (m ± SD) | Head Circumference, cm (m ± SD) | |||||
| Age/Sex | Male | Female | Male | Female | Male | Female | Male | Female |
| 1 month | 53.30 ± 2.00 | 52.75 ± 2.03 | 4.46 ± 0.72 | 4.18 ± 0.53 | 15.62 ± 1.78 | 15.00 ± 1.37 | 37.09 ± 1.58 | 36.81 ± 0.98 |
| 2 months | 57.60 ± 2.25 * | 56.51 ± 1.73 | 5.79 ± 0.86 * | 5.16 ± 0.53 | 17.38 ± 1.77 * | 16.16 ± 1.36 | 39.05 ± 1.54 | 38.54 ± 1.04 |
| 4 months | 62.88 ± 2.33 * | 61.56 ± 2.26 | 7.31 ± 0.78 * | 6.57 ± 0.67 | 18.48 ± 1.43 * | 17.34 ± 1.67 | 41.39 ± 1.26 * | 40.76 ± 1.02 |
| 6 months | 67.10 ± 1.97 * | 65.93 ± 2.37 | 8.41 ± 1.21 * | 7.51 ± 0.77 | 18.63 ± 1.98 * | 17.25 ± 1.39 | 43.24 ± 1.44 * | 42.61 ± 0.91 |
| 9 months | 70.88 ± 2.47 | 70.58 ± 2.67 | 9.19 ± 1.36 | 8.60 ± 1.02 | 18.27 ± 2.14 * | 17.24 ± 1.61 | 44.95 ± 1.43 * | 44.37 ± 0.80 |
| 12 months | 74.71 ± 2.53 | 73.94 ± 2.68 | 9.71 ± 1.00 | 9.22 ± 1.14 | 17.39 ± 1.49 | 16.86 ± 1.83 | 45.99 ± 1.43 | 45.74 ± 0.86 |
| Craniofacial Asymmetry Score(mm ± SD) | ||||||||
| Age/Sex | Male | Female | p Value | |||||
| 1 month | 3.21 ± 2.04 | 2.87 ± 1.74 | 0.490 | |||||
| 2 months | 2.90 ± 1.38 | 2.71 ± 1.45 | 0.586 | |||||
| 4 months | 2.60 ± 1.36 | 2.31 ± 1.31 | 0.382 | |||||
| 6 months | 2.52 ± 1.44 | 2.16 ± 1.03 | 0.265 | |||||
| 9 months | 2.47 ± 1.26 | 1.91 ± 1.19 | 0.069 | |||||
| 12 months | 2.13 ± 1.08 | 1.88 ± 0.87 | 0.326 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo, A.-L.; Hallac, R.R.; Chen, S.-H.; Hsu, K.-H.; Wang, S.-W.; Chen, C.-H.; Lien, R.-Y.; Lo, L.-J.; Chou, P.-Y. Craniofacial Growth and Asymmetry in Newborns: A Longitudinal 3D Assessment. Int. J. Environ. Res. Public Health 2022, 19, 12133. https://doi.org/10.3390/ijerph191912133
Lo A-L, Hallac RR, Chen S-H, Hsu K-H, Wang S-W, Chen C-H, Lien R-Y, Lo L-J, Chou P-Y. Craniofacial Growth and Asymmetry in Newborns: A Longitudinal 3D Assessment. International Journal of Environmental Research and Public Health. 2022; 19(19):12133. https://doi.org/10.3390/ijerph191912133
Chicago/Turabian StyleLo, Ai-Lun, Rami R. Hallac, Shih-Heng Chen, Kai-Hsiang Hsu, Sheng-Wei Wang, Chih-Hao Chen, Rei-Yin Lien, Lun-Jou Lo, and Pang-Yun Chou. 2022. "Craniofacial Growth and Asymmetry in Newborns: A Longitudinal 3D Assessment" International Journal of Environmental Research and Public Health 19, no. 19: 12133. https://doi.org/10.3390/ijerph191912133
APA StyleLo, A.-L., Hallac, R. R., Chen, S.-H., Hsu, K.-H., Wang, S.-W., Chen, C.-H., Lien, R.-Y., Lo, L.-J., & Chou, P.-Y. (2022). Craniofacial Growth and Asymmetry in Newborns: A Longitudinal 3D Assessment. International Journal of Environmental Research and Public Health, 19(19), 12133. https://doi.org/10.3390/ijerph191912133






_周(Chou).jpg)

