Using Path Analysis and Linear Regression to Test for Gender and Participation: Effects in a Culturally Tailored Diabetes Intervention for Latino Adults
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Sample Demographic and Participation Characteristics by Gender
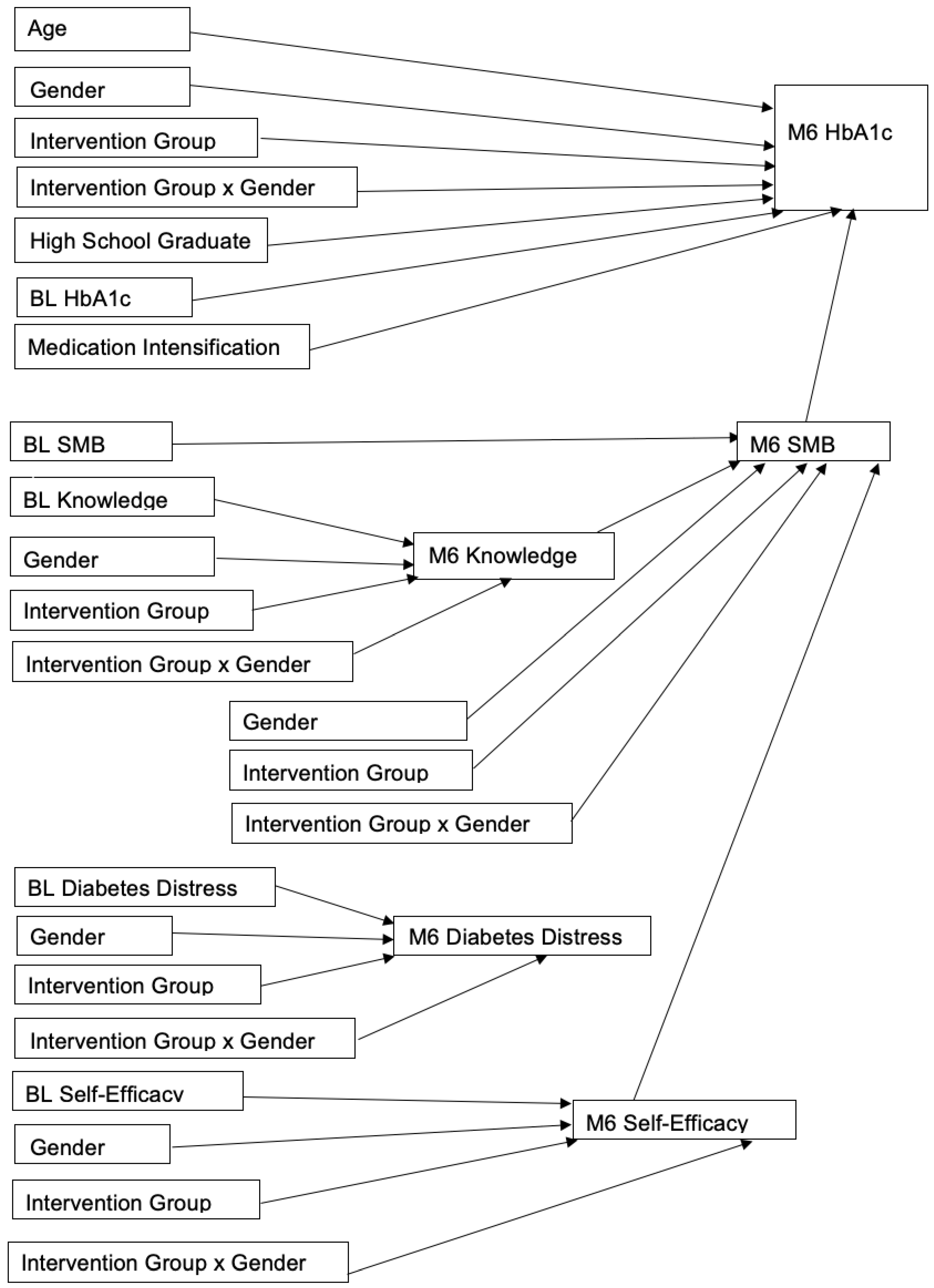
3.2. Path Analysis Results
3.3. Linear Regression Results
3.4. Model Fit Results
3.5. Sample Demographic and Participation Characteristics by Gender
Baseline Measures and Medication Use
3.6. Linear Regression Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. National Diabetes Statistics Report 2020 Website. Available online: https://www.cdc.gov/diabetes/data/statistics-report/index.html (accessed on 8 February 2022).
- Greg, E.W.; Zhuo, X.; Cheng, Y.J.; Albright, A.L.; Narayan, K.V.; Thompson, T.J. Trends in lifetime risk and years of life lost due to diabetes in the USA, 1985–2011: A modelling study. Lancet Diabetes Endocrinol. 2014, 2, 867–874. [Google Scholar] [CrossRef]
- Palmas, W.; Findley, S.E.; Mejia, M.; Batista, M.; Teresi, J.; Kong, J.; Silver, S.; Fleck, E.M.; Luchsinger, J.A.; Carrasquillo, O. Results of the northern Manhattan diabetes community outreach project: A randomized trial studying a community health worker intervention to improve diabetes care in Hispanic adults. Diabetes Care 2014, 37, 963–969. [Google Scholar] [CrossRef]
- Kim, K.; Choi, J.S.; Choi, E.; Nieman, C.L.; Joo, J.H.; Lin, F.R.; Gitlin, L.N.; Han, H.R. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: A systematic review. Am. J. Public Health 2016, 106, e28. [Google Scholar] [CrossRef]
- Shah, M.; Kaselitz, E.; Heisler, M. The role of community health workers in diabetes: Update on current literature. Curr. Diabetes Rep. 2013, 13, 163–171. [Google Scholar] [CrossRef]
- Kieffer, E.C.; Willis, S.K.; Odoms-Young, A.M.; Guzman, J.R.; Allen, A.J.; Feathers, J.T.; Loveluck, J. Reducing disparities in diabetes among African-American and Latino residents of Detroit: The essential role of community planning focus groups. Ethn. Dis. 2004, 14 (Suppl. 1), 1. [Google Scholar]
- Feathers, J.T.; Kieffer, E.C.; Palmisano, G.; Anderson, M.; Janz, N.; Spencer, M.S.; Guzman, R.; James, S.A. The development, implementation, and process evaluation of the REACH Detroit partnership’s diabetes lifestyle intervention. Diabetes Educ. 2007, 33, 509–520. [Google Scholar] [CrossRef]
- Spencer, M.S.; Kieffer, E.C.; Sinco, B.; Piatt, G.; Palmisano, G.; Hawkins, J.; Lebron, A.; Espitia, N.; Tang, T.; Funnell, M. Outcomes at 18 months from a community health worker and peer leader diabetes self-management program for Latino adults. Diabetes Care 2018, 41, 1414–1422. [Google Scholar] [CrossRef]
- Two Feathers, J.; Kieffer, E.C.; Palmisano, G.; Anderson, M.; Sinco, B.; Janz, N.; Heisler, M.; Spencer, M.; Guzman, R.; Thompson, J. Racial and ethnic approaches to community health (REACH) Detroit partnership: Improving diabetes-related outcomes among African American and Latino adults. Am. J. Public Health 2005, 95, 1552–1560. [Google Scholar] [CrossRef] [PubMed]
- Spencer, M.S.; Rosland, A.-M.; Kieffer, E.C.; Sinco, B.R.; Valerio, M.; Palmisano, G.; Anderson, M.; Guzman, J.R.; Heisler, M. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: A randomized controlled trial. Am. J. Public Health 2011, 101, 2253–2260. [Google Scholar] [CrossRef]
- American Public Health Association. Community Health Workers. American Public Health Association Web Site. Available online: https://www.apha.org/apha-communities/member-sections/community-health-workers (accessed on 22 March 2017).
- Norris, S.L.; Chowdhury, F.M.; Van Le, K.; Horsley, T.; Brownstein, J.N.; Zhang, X.; Jack, L., Jr.; Satterfield, D.W. Effectiveness of community health workers in the care of persons with diabetes. Diabetic Med. 2006, 23, 544–556. [Google Scholar] [CrossRef]
- Hawkins, J.; Kieffer, E.C.; Sinco, B.; Spencer, M.; Anderson, M.; Ann-Marie Rosland, A.M. Does gender influence participation? Predictors of participation in a community health worker diabetes management intervention with African American and Latino adults. Diabetes Educ. 2013, 39, 647–654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhodes, S.D.; Daniel, J.; Alonzo, J.; Duck, S.; García, M.; Downs, M.; Hergenrather, K.C.; Alegría-Ortega, J.; Miller, C.; Boeving Allen, A.; et al. A systematic community-based participatory approach to refining an evidence-based community-level intervention: The HOLA intervention for Latino men who have sex with men. Health Promot. Pract. 2013, 14, 607–616. [Google Scholar] [CrossRef]
- Rhodes, S.D.; Leichliter, J.S.; Sun, C.J.; Bloom, F.R. The HoMBReS and HoMBReS Por un Cambio interventions to reduce HIV disparities among immigrant Hispanic/Latino men. MMWR Suppl. 2016, 65, 51. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, J.; Watkins, D.C.; Kieffer, E.; Spencer, M.; Piatt, G.; Nicklett, E.J.; Lebron, A.; Espitia, N.; Palmisano, G. An exploratory study of the impact of gender on health behavior among African American and Latino men with type 2 diabetes. Am. J. Men’s Health 2017, 11, 344–356. [Google Scholar] [CrossRef] [PubMed]
- Mansyur, C.L.; Rustveld, L.O.; Nash, S.G.; Jibaja-Weiss, M.L. Social factors and barriers to self-care adherence in Hispanic men and women with diabetes. Patient Educ. Couns. 2015, 98, 805–810. [Google Scholar] [CrossRef] [PubMed]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care 2000, 23, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Polonsky, W.H.; Fisher, L.; Earles, J.; Dudl, R.J.; Lees, J.; Mullan, J.; Jackson, R.A. Assessing psychosocial distress in diabetes. Diabetes Care 2005, 28, 626–631. [Google Scholar] [CrossRef]
- Beckerle, C.M.; Lavin, M.A. Association of self-efficacy and self-care with glycemic control in diabetes. Diabetes Spectr. 2013, 26, 172–178. [Google Scholar] [CrossRef]
- Fitzgerald, J.T.; Anderson, R.M.; Gruppen, L.D.; Davis, W.K.; Aman, L.C.; Jacober, S.J.; Grunberger, G. The reliability of the diabetes care profile for African Americans. Eval. Health Prof. 1998, 21, 52–65. [Google Scholar] [CrossRef]
- Fitzgerald, J.T.; Davis, W.K.; Connell, C.M.; Hess, G.E.; Funnell, M.M.; Hiss, R.G. Development and validation of the diabetes care profile. Eval. Health Prof. 1996, 19, 208–230. [Google Scholar] [CrossRef]
- Fisher, R.A. The Design of Experiments; Oliver and Boyd: Edinburgh, UK, 1942. [Google Scholar]
- Kalbfleish, J.D.; Prentice, R.L. The Statistical Analysis of Failure Time Data; John Wiley & Sons: Hoboken, NJ, USA, 2011; Volume 360. [Google Scholar]
- Diggle, P. Analysis of Longitudinal Data; Oxford University Press: Oxford, UK, 2002. [Google Scholar]
- West, B.T.; Galecki, A.T.; Welch, K.B. Linear Mixed Models; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- SAS Institute. The MIXED Procedure; SAS Institute: Hong Kong, China, 2012; Volume 9, p. 4. [Google Scholar]
- Van Buuren, S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat. Methods Med. Res. 2007, 16, 219–242. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: Hoboken, NJ, USA, 2004; Volume 81. [Google Scholar]
- Hu, J.; Wallace, D.C.; McCoy, T.P.; Amirehsani, K.A. A family-based diabetes intervention for Hispanic adults and their family members. Diabetes Educ. 2014, 40, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Vincent, D.; McEwen, M.M.; Pasvogel, A. The validity and reliability of a Spanish version of the summary of diabetes self-care activities questionnaire. Nurs. Res. 2008, 57, 101–106. [Google Scholar] [CrossRef]
- Baig, A.A.; Benitez, A.; Locklin, C.A.; Gao, Y.; Lee, S.M.; Quinn, M.T.; Solomon, M.C.; Sánchez-Johnsen, L.; Burnet, D.L.; Chin, M.H. Picture good health: A church-based self-management intervention among Latino adults with diabetes. J. Gen. Intern. Med. 2015, 30, 1481–1490. [Google Scholar] [CrossRef]
- Martinez-Vega, I.P.; Doubova, S.V.; Aguirre-Hernandez, R.; Infante-Castañeda, C. Adaptation and validation of the Distress Scale for Mexican patients with type 2 diabetes and hypertension: A cross-sectional survey. BMJ Open 2016, 6, e009723. [Google Scholar] [CrossRef]
- Qin, W.; Blanchette, J.E.; Yoon, M. Self-Efficacy and diabetes self-management in middle-aged and older adults in the United States: A systematic review. Diabetes Spectr. 2020, 33, 315–323. [Google Scholar] [CrossRef]
- Funnell, M.M.; Anderson, R.M. Empowerment and self-management of diabetes. Clin. Diabetes 2004, 22, 123–128. [Google Scholar] [CrossRef] [Green Version]

| Characteristic | Women (n = 135) | Men (n = 87) | Total (n = 222) | p-Value for Women & Men |
|---|---|---|---|---|
| Demographic Characteristics | ||||
| Age, years | 48.2 (10.3) | 49.9 (11.0) | 48.9 (10.6) | 0.242 i |
| High school graduate | 33 (24.4%) | 35 (40.2%) | 68 (30.6%) | 0.013 j |
| Intervention Group | 86 (63.7%) | 63 (72.4%) | 149 (67.1%) | 0.178 j |
| Diabetes Medication Characteristics | ||||
| Diabetes Medications | 0.190 k | |||
| No medications | 8 (5.9%) | 2 (2.3%) | 10 (4.5%) | |
| Only oral diabetes medications | 97 (71.9%) | 61 (70.1%) | 158 (71.2%) | |
| Insulin, with or without oral medication | 30 (22.2%) | 24 (27.6%) | 54 (24.3%) | |
| Diabetes Med Intensification a | 40 (34.8%) | 21 (30.4%) | 61 (33.2%) | 0.544 j |
| Outcome Values at Baseline | ||||
| HbA1 c | 7.64 (1.78) | 8.13 (1.99) | 7.83 (1.88) | 0.058 i |
| Knowledge b | 2.76 (0.79) | 2.84 (0.88) | 2.79 (0.83) | 0.493 i |
| Diabetes Distressc | 2.20 (1.02) | 1.87 (0.94) | 2.07 (1.00) | 0.019 i |
| Self-Efficacy d | 6.94 (1.72) | 7.28 (1.56) | 7.07 (1.67) | 0.139 i |
| Self-management behavior e | 3.43 (1.21) | 3.42 (1.21) | 3.42 (1.21) | 0.944 i |
| Intervention Participation Measures (n = 149) | ||||
| Characteristic | Women (n = 86) | Men (n = 63) | Total (n = 149) | p-Value for Women & Men |
| Class Attendance | 8.0 (3.6) | 7.1 (3.9) | 7.6 (3.7) | 0.113 l |
| All Journey-to-Health f Classes in Group Format | 37 (43.0%) | 39 (61.9%) | 76 (51.0%) | 0.023 j |
| All Self-Management g Classes in Group Format | 48 (55.8%) | 46 (73.0%) | 94 (63.1%) | 0.032 j |
| Number of CHW h Home Visits | 1.2 (1.3) | 0.8 (1.0) | 1.1 (1.2) | 0.077 l |
| At Least One CHW-Accompanied Doctor Visit | 74 (86.0%) | 51 (81.0%) | 125 (83.9%) | 0.403 j |
| Predictor | Coefficient (95% CI) | p-Value |
|---|---|---|
| Baseline Self-Efficacy (Stanford Scale) | 0.61 (0.49, 0.74) | <0.001 |
| Male gender referenced to female | 0.24 (−0.18, 0.67) | 0.262 |
| Age (years) | 0.00 (−0.014, 0.02) | 0.615 |
| High School Graduate | −0.01 (−0.44, 0.43) | 0.972 |
| Class attendance (0–11) | 0.06 (0.00, 0.12) | 0.037 |
| All JTH classes in group format | 0.14 (−0.37, 0.65) | 0.597 |
| All self-management classes in group format | 0.44 (−0.10, 0.97) | 0.112 |
| CHW Home Visits | 0.24 (0.01, 0.47) | 0.042 |
| Predictor | Coefficient (95% CI) | p-Value |
| Baseline Understanding of Diabetes Management | 0.50 (0.36, 0.64) | <0.001 |
| Male gender referenced to female | 0.06 (−0.18, 0.30) | 0.602 |
| Age (years) | 0.01 (0.001, 0.02) | 0.037 |
| High School Graduate | 0.45 (0.19, 0.71) | 0.001 |
| Class attendance (0–11) | 0.03 (−0.01, 0.08) | 0.181 |
| All JTH classes in group format | −0.07 (−0.32, 0.18) | 0.560 |
| All self-management classes in group format | 0.05 (−0.20, 0.30) | 0.687 |
| CHW Home Visits | 0.05 (−0.06, 0.16) | 0.365 |
| Predictor | Coefficient (95% CI) | p-Value |
| Baseline Distress | 0.47 (0.35, 0.58) | <0.001 |
| Male gender referenced to female | −0.08 (−0.31, 0.15) | 0.502 |
| Age (years) | 0.00 (−0.01, 0.01) | 0.682 |
| High School Graduate | 0.03 (−0.20, 0.27) | 0.793 |
| Class attendance (0–11) | −0.04 (−0.08, −0.01) | 0.007 |
| All JTH classes in group format | −0.27 (−0.55, 0.01) | 0.059 |
| All self-management classes in group format | −0.12 (−0.41, 0.16) | 0.399 |
| CHW Home Visits | −0.08 (−0.21, 0.04) | 0.188 |
| Predictor | Coefficient (95% CI) | p-Value |
| Baseline Self-Management Behavior | 0.41 (0.27, 0.55) | <0.001 |
| Male gender referenced to female | 0.18 (−0.19, 0.56) | 0.335 |
| Age (years) | 0.00 (−0.02, 0.02) | 0.997 |
| High School Graduate | 0.37 (−0.05, 0.79) | 0.083 |
| Month 6 Baseline Knowledge of Diabetes Management | −0.26 (−0.52, 0.00) | 0.053 |
| Month 6 Diabetes Distress | −0.09 (−0.39, 0.20) | 0.536 |
| Month 6 Self-Efficacy | 0.20 (0.04, 0.35) | 0.017 |
| Class attendance (0–11) | 0.04 (−0.04, 0.11) | 0.314 |
| All JTH classes in group format | −0.18 (−0.57, 0.21) | 0.366 |
| All self-management classes in group format | −0.38 (−0.77, 0.00) | 0.054 |
| CHW Home Visits | 0.14 (−0.03, 0.31) | 0.113 |
| Predictor | Coefficient (95% CI) | p-Value |
| Baseline HbA1c | 0.59 (0.47, 0.71) | <0.001 |
| Male gender referenced to female | −0.10 (−0.53, 0.33) | 0.646 |
| Age (years) | −0.01 (−0.03, 0.00) | 0.141 |
| High school graduate | −0.36 (−0.82, 0.09) | 0.120 |
| 6-Month Self-Management Behavior | 0.01 (−0.17, 0.19) | 0.897 |
| Medication Intensification | 0.00 (−0.42, 0.42) | 0.993 |
| Class attendance (0–11) | −0.10 (−0.19, −0.02) | 0.023 |
| All JTH classes in group format | 0.03 (−0.42, 0.48) | 0.899 |
| All self-management classes in group format | −0.19 (−0.64, 0.26) | 0.402 |
| CHW Home Visits | −0.06 (−0.26, 0.13) | 0.539 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hawkins, J.; Kieffer, E.C.; Sinco, B.; Piatt, G.; Jones, L.; Mitchell, J.; Espitia, N.; LeBron, A.; Kloss, K.A.; Kurnick, K.; et al. Using Path Analysis and Linear Regression to Test for Gender and Participation: Effects in a Culturally Tailored Diabetes Intervention for Latino Adults. Int. J. Environ. Res. Public Health 2022, 19, 11982. https://doi.org/10.3390/ijerph191911982
Hawkins J, Kieffer EC, Sinco B, Piatt G, Jones L, Mitchell J, Espitia N, LeBron A, Kloss KA, Kurnick K, et al. Using Path Analysis and Linear Regression to Test for Gender and Participation: Effects in a Culturally Tailored Diabetes Intervention for Latino Adults. International Journal of Environmental Research and Public Health. 2022; 19(19):11982. https://doi.org/10.3390/ijerph191911982
Chicago/Turabian StyleHawkins, Jaclynn, Edith C. Kieffer, Brandy Sinco, Gretchen Piatt, Lenette Jones, Jamie Mitchell, Nicolaus Espitia, Alana LeBron, Katherine A. Kloss, Katie Kurnick, and et al. 2022. "Using Path Analysis and Linear Regression to Test for Gender and Participation: Effects in a Culturally Tailored Diabetes Intervention for Latino Adults" International Journal of Environmental Research and Public Health 19, no. 19: 11982. https://doi.org/10.3390/ijerph191911982
APA StyleHawkins, J., Kieffer, E. C., Sinco, B., Piatt, G., Jones, L., Mitchell, J., Espitia, N., LeBron, A., Kloss, K. A., Kurnick, K., Palmsiano, G., & Spencer, M. S. (2022). Using Path Analysis and Linear Regression to Test for Gender and Participation: Effects in a Culturally Tailored Diabetes Intervention for Latino Adults. International Journal of Environmental Research and Public Health, 19(19), 11982. https://doi.org/10.3390/ijerph191911982






