ECG Standards and Formats for Interoperability between mHealth and Healthcare Information Systems: A Scoping Review
Abstract
1. Introduction
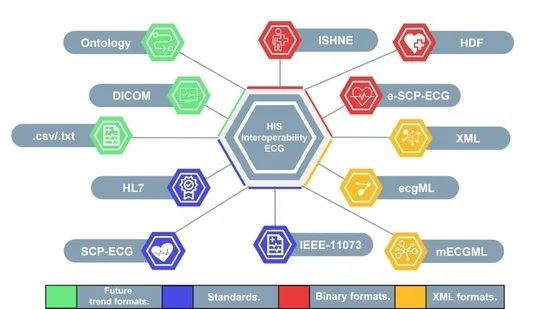
ECG Data Interoperability
2. Materials and Methods
2.1. Research Questions
| Category | Include | Exclude |
|---|---|---|
| Population | Any human population | Non-human populations |
| Concept | Data format or data standard to manage or storage ECG patient information | Data formats or data standards for manage or storage other kind of human biosignals (e.g., EEG, GRS) |
| Context | Mobile health or healthcare systems | Not applicable |
- What digital data formats or data standards have been proposed for the interoperability of electrocardiographic data between traditional healthcare information systems and mobile healthcare information systems?
- What are the advantages and disadvantages of these data formats or data standards?
2.2. Data Sources and Search Strategy
2.3. Eligibility and Exclusion Criteria
2.3.1. Eligibility Criteria
- We selected studies published in the English language in indexed journals or conference articles between 1 January 2009 and 30 April 2022.
- Studies that present or describe devices and systems that store and retrieve electrocardiographic (ECG) signal data in a data format that allows interoperability between personal medical devices and/or health information systems (HIS).
- Studies that demonstrate the interoperability of data standards or data formats for storing and retrieving ECG data.
2.3.2. Exclusion Criteria
- We have excluded studies that present devices and systems that store and retrieve other biological or physiological data different from the ECG in a format that permits interoperability.
- Studies that report the use of formats or standards for storing electrocardiographic signals but do not demonstrate the interoperability of medical data in health information systems (HIS).
- Studies published and/or reported in documents not disseminated through ordinary commercial publication channels pose access problems (e.g., theses, research reports, book chapters, patents). Studies of this type are commonly called gray literature.
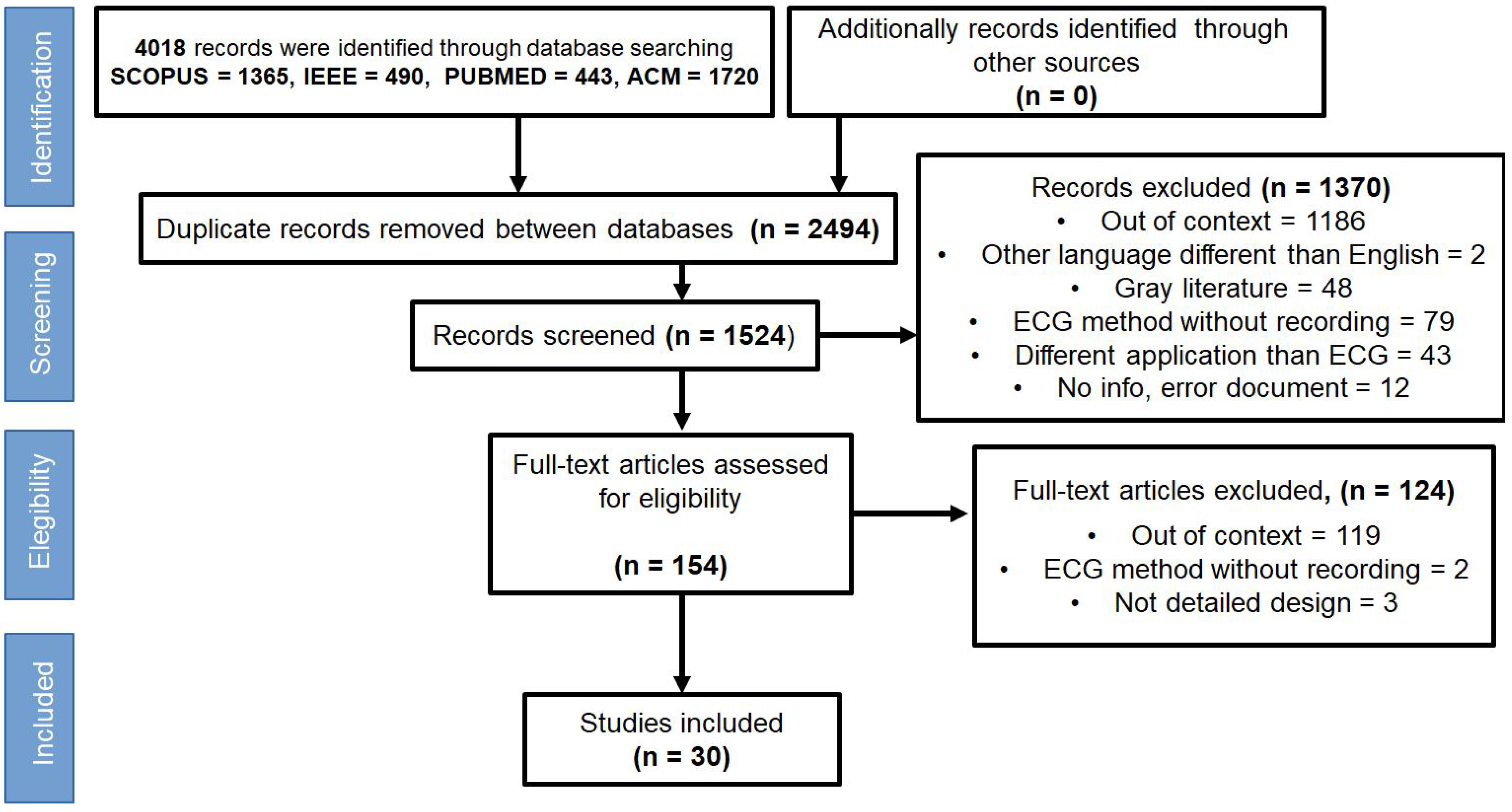
2.4. Study Selection
2.5. Data Extraction
3. Results
3.1. Searches
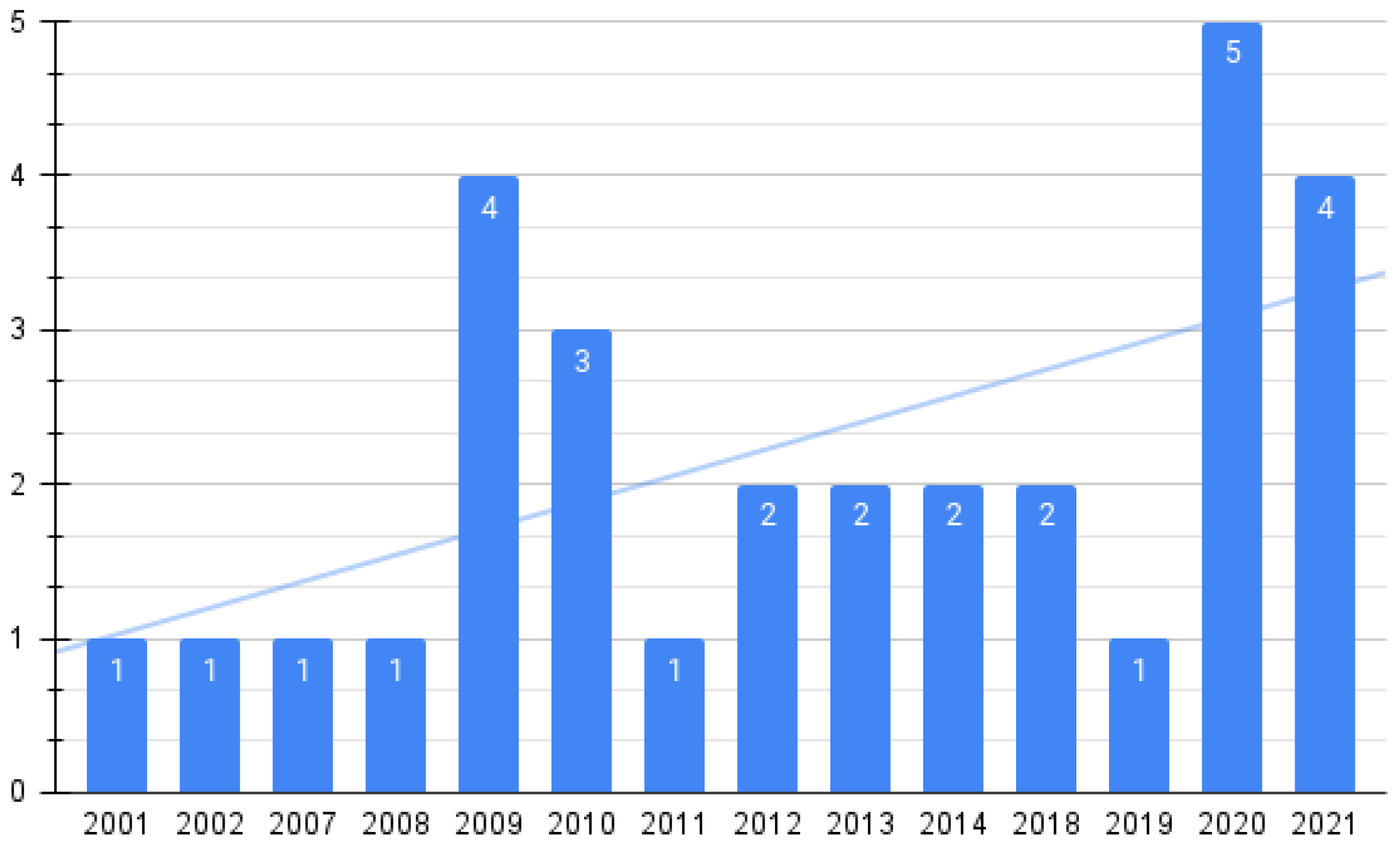
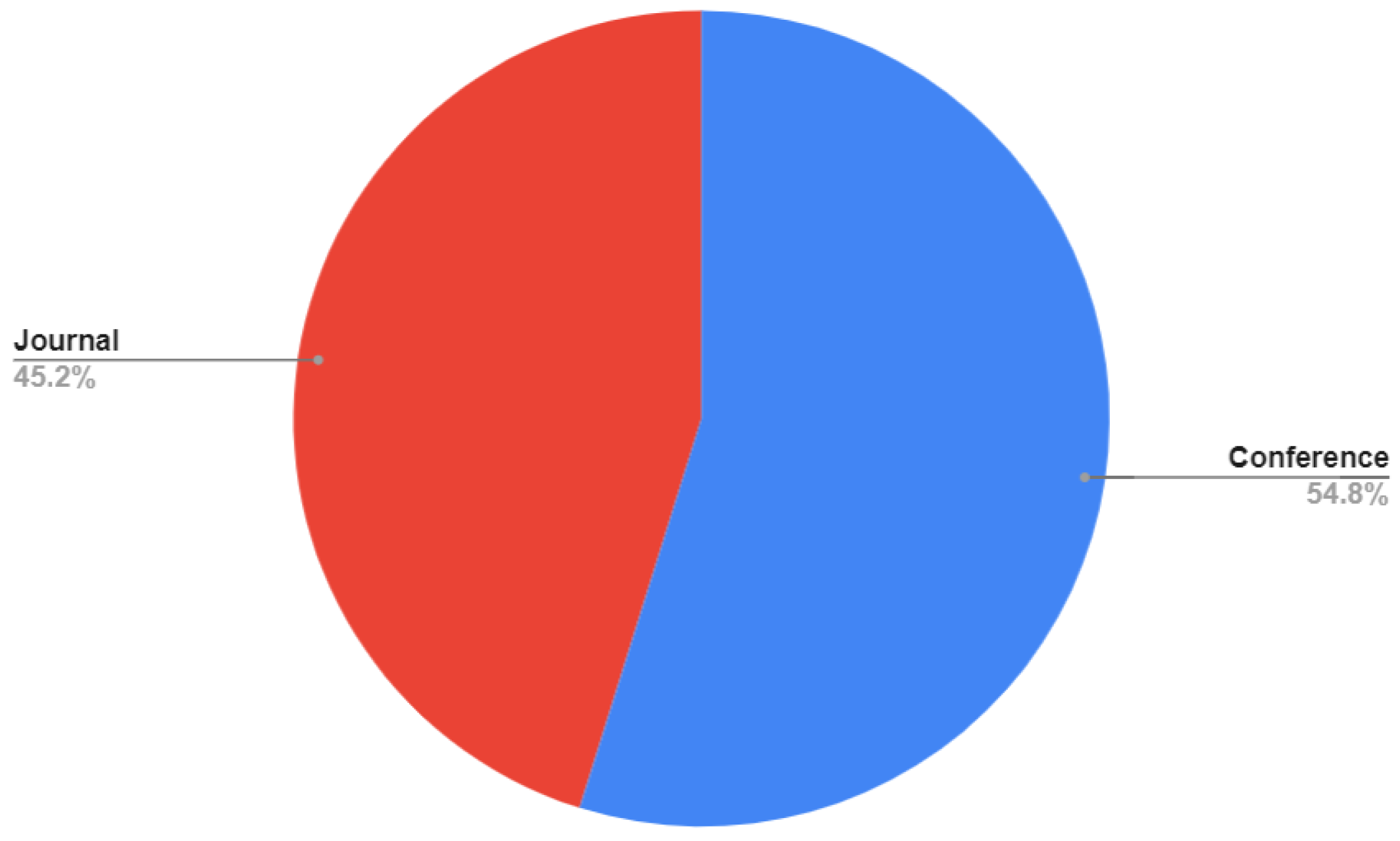
3.2. Study Characteristics
3.3. Data Standards
3.3.1. HL7
3.3.2. SCP-ECG
3.3.3. X73-PHD
3.4. PDF/A
- PDF/A-1 (ISO 19005-1:2005) was published in 2005 and is based on PDF version 1.4.
- PDF/A-2 (ISO 19005-2:2011) was published in 2011 and is based on PDF version 1.7. This version extended the capabilities of PDF/A-1. The main new capability was to allow embedding of PDF/A compliant attachments.
- PDF/A-3 (ISO 19005-3:2012) was released in 2012. This version extended the capabilities of PDF/A-2. There is a new feature that allows files of any format to be embedded.
- PDF/A-4 (ISO 19005-4:2020) is based on PDF version 2.0. PDF/A-4 introduces the new PDF/A-4e conformance level that supports interactive 3D models for engineering workflows.
| Studies | Data Standard | mHealth Interoperability | Level Interoperability |
|---|---|---|---|
| [17,19,30,36,38,49,51,52,53] | HL7 | Yes | L1, L2, L3 |
| [12,17,19,30,53] | DICOM | No | L1, L3, L4 |
| [12,17,19,43,47,49,53] | SCP-ECG | Yes | L1, L2, L4 |
| [17] | ISHINE | No | L1 |
| [54] | PDF/A | Yes | L1, L3, L4 |
| [12,43,47] | X73-PHD | Yes | L1, L2, L4 |
| [55] | Open ECG Philips | No | L2 |
3.5. Data Formats
| Studies | Data Formats | mHealth Interoperability | Type Format |
|---|---|---|---|
| [17,38,42,50,58,59,60] | XML-ECG | Yes | Open |
| [61] | HL7-XML | Yes | Open |
| [27] | mPCG-XML | Yes | Open |
| [62,63] | Philips-XML | No | Propietary |
| [64,65] | ecgML | No | Open |
| [14,66] | mECGML | Yes | Open |
| [53,67] | JSON | Yes | Open |
| [17] | SaECG | Yes | Open |
| [49,68] | HL7 aECG | Yes | Open |
| [52,69] | CDA R2 | Yes | Open |
| [67] | PDF-ECG | Yes | Open |
| [70,71,72] | MFER | No | Propietary |
| [73] | EDF | No | Open |
| [74] | CSV | Yes | Open |
| [75] | ECGWARE | No | Open |
3.5.1. XML
- mPCG-XML is a markup language specifically designed for the presentation, visualization, and transmission of PCG data and its seamless integration with telecardiology applications. Telemonitoring for remote access to PCG data and transmission of PCG data over the mobile network using mPCG-XML ensure data interoperability and support data mining and semantics.In order to ensure interoperability and support data mining and data semantics, the authors of [27] propose a new method that uses an XML schema exclusively for PCG data exchange and monitoring over mobile devices. This XML schema is called mPCG-XML, which provides fast medical decision assistance. Additionally, it supports a hierarchical structure that captures data, tags, and elements in an efficient way, so that it is human readable and will enable seamless integration of PCG data in healthcare architecture and applications.
- SaECG (Stream-enabled annotated ECG) is an XML-based format that allows the storage of long-duration ECG traces based on the FHIR (Fast Healthcare Interoperability Resources) standard specifications for the HL7 aECG format, however, adding annotations for the time period in which the measurements are taken and divided into several segments, taking into account the periods of sensor reading acquisition and inactivity periods [19].The advantages of the format are that SaECG is compatible with different ECG streaming sensors and is capable to use many and independent channels [19].
- JSON (JavaScript Object Notation) is a format defined at the end of 2002 by Douglas Crockford that emerged from the need for data exchange with web services, based on the data types of JavaScript language [79,80].Files generated from the JSON format are dictionaries that consist of a tree structure nested values identified by key-value pairs, thus supporting two types of data structures: arrays and objects. Branches may or may not have the same key values, allowing data to be standardized by tagging it with specific topics. In that way, data are identified and generated from different sources or further formats, while merging them into one [80,81].To navigate through a JSON document, the notation to be used will vary between systems without ignoring the following principles, previously described in [80]:
- -
- As a JSON object, a specific value is accessed by a key-value pair.
- -
- As a JSON array, a specific element must be accessed by the i-th element of the array.
Among its main advantages are its data exchange with web services through the use of an API (Application Programming Interface) and the ease with which it can be interpreted by both humans and other systems, such as NoSQL or graph databases, due to its nested structure and key-value identifiers [80]. Since it reduces the data volume needed to identify each file element, it is also known to be lighter than other formats. This is due to its size reduction before being transmitted, allowing this format to be used by different programming languages and platforms. Therefore, it is more efficient in transmitting data between the different modules of the same application [79].However, one of its disadvantages when operating with other applications is the impossibility of specifying the data format, making it difficult to transmit files such as images [79]. - Philips XML was published in 2003, and is used by its own electrocardiographs, bedside monitors, and defibrillators. This facilitated the European Commission’s effort to ensure electrocardiograph interoperability and ECG accessibility. W3C XML Schema Language was used to write the Philips XML format, which was available on the Internet and included the electrocardiograph documentation. As part of the Philips XML ECG, the ECG waveform data is compressed using a lossless algorithm and encoded using a base 64 encoding scheme into ASCII characters. To facilitate the easy access to compressed waveform data, Philips also provides a suite of software tools. Furthermore, Philips’ XML format uses Scalable Vector Graphics (SVG) as a display format and is compatible with other standards and initiatives, such as HL7 aECG and Integrating the Healthcare Enterprise (IHE) for displaying ECGs.
- HL7 aECG is an XML-based standard for medical data digitization created by HL7 RCRIM (Regulated Clinical Research Information Management) which was accept in 2004 by American National Standards Institute, where HL7 aECG is a sub-standard that supports the storage and display of ECG data [28,43,51,54,77]. The format includes one or more time-bound ECG waveform data sets and annotations for that time. The message model is derived from HL7 RIM (Reference Information Model). The aECG R-MIM (Refined Information Model) forms the basis for defining messages and XML schema. Different ECG annotations can be defined with it (e.g., QRS wave, T-offset, P wave, peak R time, R peak amplitude, QT interval, QTc interval annotation, etc.). It supports a 12-channel ECG with a maximum sampling time of 30 seconds. Unfortunately, it does not support the ECG data stream [51].
- ecgML is another XML-based standard for presentation and storage of ECG and effective XML transformations using Extensible Stylesheet Language Transformation technology in various formats such as comma-separated files and scalable vector graphics (SVG) [27].
- XML-ECG The XML-ECG format was published in 2007. This standard uses only six modules, making it much more readable. Although the structure is simple, it can describe the complete ECG information, including waveform, patient demographics, annotation, and measurement, to name a few. In addition, it is also expandable with the explicit rule of separating the basic part and the expandable part in the structure [60].
- CDA R2 In May 2005, the Clinical Document Architecture Release two, became an ANSI-approved HL7 standard. CDA documents consist of text, images, sounds, and other multimedia content. It can be transferred within a message and can exist independently, outside the transferring message [82]. It is important to note that CDA documents are encoded in eXtensible Markup Language (XML) and they derive their machine-processable meaning from the Reference Information Model [82]. The CDA R2 document includes a document header and the document body. As a result, the document contains several sections that contain human-readable narrative forms or coded structures for automatic processing [83]. In CDA R2, health data can be easily integrated into databases of healthcare facilities.
3.5.2. PDF-ECG
3.5.3. CSV
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Search Strategy
References
- Cruz-Ramos, N.A.; Alor-Hernández, G.; Colombo-Mendoza, L.O.; Sánchez-Cervantes, J.L.; Rodríguez-Mazahua, L.; Guarneros-Nolasco, L.R. mHealth Apps for Self-Management of Cardiovascular Diseases: A Scoping Review. Healthcare 2022, 10, 322. [Google Scholar] [CrossRef] [PubMed]
- mHealth Solutions Market by Connected Devices (Glucose & Blood Pressure Monitor, Peak Flow Meter, Pulse Oximeter), Apps (Weight Loss, Women Health, Diabetes Management, Mental Health), Services (Remote Monitoring, Consultation)-Global Forecast to 2025. 2022. Available online: https://www.marketsandmarkets.com/PressReleases/mhealth-apps-and-solutions.asp (accessed on 28 May 2022).
- Gurupur, V.P.; Wan, T.T. Challenges in implementing mHealth interventions: A technical perspective. Mhealth 2017, 3, 32. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, R.J.; Risk, A. eHealth in Latin America and the Caribbean: Development and policy issues. J. Med. Internet Res. 2003, 5, e877. [Google Scholar] [CrossRef] [PubMed]
- Weber-Jahnke, J.; Peyton, L.; Topaloglou, T. eHealth system interoperability. Inf. Syst. Front. 2012, 14, 1–3. [Google Scholar] [CrossRef]
- Lehne, M.; Sass, J.; Essenwanger, A.; Schepers, J.; Thun, S. Why digital medicine depends on interoperability. NPJ Digit. Med. 2019, 2, 1–5. [Google Scholar] [CrossRef]
- Gaynor, M.; Yu, F.; Andrus, C.H.; Bradner, S.; Rawn, J. A general framework for interoperability with applications to healthcare. Health Policy Technol. 2014, 3, 3–12. [Google Scholar] [CrossRef]
- Mykkänen, J.A.; Tuomainen, M.P. An evaluation and selection framework for interoperability standards. Inf. Softw. Technol. 2008, 50, 176–197. [Google Scholar] [CrossRef]
- Kuziemsky, C.E.; Peyton, L. A framework for understanding process interoperability and health information technology. Health Policy Technol. 2016, 5, 196–203. [Google Scholar] [CrossRef]
- Whitman, L.E.; Panetto, H. The missing link: Culture and language barriers to interoperability. Annu. Rev. Control 2006, 30, 233–241. [Google Scholar] [CrossRef][Green Version]
- Byambasuren, O.; Sanders, S.; Beller, E.; Glasziou, P. Prescribable mHealth apps identified from an overview of systematic reviews. NPJ Digit. Med. 2018, 1, 1–12. [Google Scholar] [CrossRef]
- Trigo, J.D.; Alesanco, A.; Martínez, I.; García, J. A review on digital ECG formats and the relationships between them. IEEE Trans. Inf. Technol. Biomed. 2011, 16, 432–444. [Google Scholar] [CrossRef]
- Hurst, J.W. The rise, fall, and rise again of the ECG as a diagnostic tool. Chest 1997, 111, 800–802. [Google Scholar] [CrossRef] [PubMed]
- Bond, R.R.; Finlay, D.D.; Nugent, C.D.; Moore, G. A review of ECG storage formats. Int. J. Med. Inform. 2011, 80, 681–697. [Google Scholar] [CrossRef] [PubMed]
- Badilini, F.; Young, B.; Brown, B.; Vaglio, M. Archiving and exchange of digital ECGs: A review of existing data formats. J. Electrocardiol. 2018, 51, S113–S115. [Google Scholar] [CrossRef] [PubMed]
- Olamidipupo, S.A.; Danas, K. Review of interoperability techniques in data acquisition of wireless ECG devices. IOSR J. Mob. Comput. Appl. 2015, 2, 19–25. [Google Scholar]
- Hilbel, T.; Alhersh, T.; Stein, W.; Doman, L.; Schultz, J.H. Analysis and postprocessing of ECG or heart rate data from wearable devices beyond the proprietary cloud and app infrastructure of the vendors. Cardiovasc. Digit. Health J. 2021, 2, 323–330. [Google Scholar] [CrossRef]
- Hur, S.; Lee, J.; Kim, T.; Choi, J.S.; Kang, M.; Chang, D.K.; Cha, W.C. An Automated Fast Healthcare Interoperability Resources-Based 12-Lead Electrocardiogram Mobile Alert System for Suspected Acute Coronary Syndrome. Yonsei Med. J. 2020, 61, 416. [Google Scholar] [CrossRef]
- Benhamida, A.; Kanas, A.; Vincze, M.; Papp, K.T.; Abbassi, M.; Kozlovszky, M. SaECG: A new FHIR Data format revision to enable continuous ECG storage and monitoring. In Proceedings of the 2020 IEEE 20th International Symposium on Computational Intelligence and Informatics (CINTI), Budapest, Hungary, 5–7 November 2020; pp. 000115–000120. [Google Scholar]
- Benhamida, A.; Slimani, G.; Kukarov, M.D.; Abbassi, M.; Koroknai, E.; Szarvák, A.; Ogbolu, M.; Vincze, M.; Kozlovszky, M. Effective ECG data conversion solution to solve ECG data interoperability problems. In Proceedings of the 2021 IEEE 21st International Symposium on Computational Intelligence and Informatics (CINTI), Budapest, Hungary, 18–20 November 2021; pp. 000067–000072. [Google Scholar]
- Munn, Z.; Peters, M.D.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. JBI Evid. Implement. 2015, 13, 132–140. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Buxton, A.E.; Calkins, H.; Callans, D.J.; DiMarco, J.P.; Fisher, J.D.; Leon Greene, H.; Haines, D.E.; Hayes, D.L.; Heidenreich, P.A.; Miller, J.M.; et al. ACC/AHA/HRS 2006 key data elements and definitions for electrophysiological studies and procedures: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (ACC/AHA/HRS Writing Committee to Develop Data Standards on Electrophysiology). J. Am. Coll. Cardiol. 2006, 48, 2360–2396. [Google Scholar] [PubMed]
- Koncar, M. HL7 standard–features, principles, and methodology. Acta Medica Croat. Cas. Hravatske Akad. Med. Znan. 2005, 59, 273–276. [Google Scholar]
- Patil, K.K.; Kumar, V.B.; Nagabhushan, B. A markup language mPCG-xml for mobile health care systems. In Proceedings of the 2009 7th International Conference on Information, Communications and Signal Processing (ICICS), Macau, China, 8–10 December 2009; pp. 1–4. [Google Scholar]
- Stamenov, D.; Gusev, M.; Armenski, G. Interoperability of ECG standards. In Proceedings of the 2018 41st International Convention on Information and Communication Technology, Electronics and Microelectronics (MIPRO), Opatija, Croatia, 21–25 May 2018; pp. 0319–0323. [Google Scholar]
- Braunstein, M.L. Healthcare in the age of interoperability: The promise of fast healthcare interoperability resources. IEEE Pulse 2018, 9, 24–27. [Google Scholar] [CrossRef]
- Joyia, G.J.; Akram, M.U.; Akbar, C.N.; Maqsood, M.F. Evolution of health level-7: A survey. In Proceedings of the 2018 International Conference on Software Engineering and Information Management, Casablanca, Morocco, 27–29 January 2018; pp. 118–123. [Google Scholar]
- Nikolidakis, S.A.; Georgakakis, E.; Giotsas, V.; Vergados, D.D.; Douligeris, C. A secure ubiquitous healthcare system based on IMS and the HL7 standards. In Proceedings of the 3rd International Conference on PErvasive Technologies Related to Assistive Environments, Corfu, Greece, 29 June–1 July 2022; pp. 1–7. [Google Scholar]
- Rubel, P.; Fayn, J.; Macfarlane, P.W.; Pani, D.; Schlögl, A.; Värri, A. The History and Challenges of SCP-ECG: The Standard Communication Protocol for Computer-Assisted Electrocardiography. Hearts 2021, 2, 384–409. [Google Scholar] [CrossRef]
- Mandellos, G.J.; Papaioannou, M.; Panagiotakopoulos, T.; Lymberopoulos, D.K. e-SCP-ECG+ v2 protocol: Expanding the e-SCP-ECG+ protocol. In International Conference on Broadband Communications, Networks and Systems; Springer: New York, NY, USA, 2018; pp. 125–135. [Google Scholar]
- Hsieh, J.c.; Hsu, M.W. A cloud computing based 12-lead ECG telemedicine service. BMC Med. Inform. Decis. Mak. 2012, 12, 1–12. [Google Scholar] [CrossRef]
- Mei, H.; Beijnum, B.J.; Wijsman, J.; Hermens, H. Medical Information Representation Framework for Mobile Healthcare. In Health Information Systems: Concepts, Methodologies, Tools, and Applications; IGI Global: Hershey, PA, USA, 2010; pp. 489–509. [Google Scholar]
- Aliakbarpoor, Y.; Comai, S.; Pozzi, G. Designing a HL7 compatible personal health record for mobile devices. In Proceedings of the 2017 IEEE 3rd International Forum on Research and Technologies for Society and Industry (RTSI), Modena, Italy, 11–13 September 2017; pp. 1–6. [Google Scholar]
- Badilini, F.; Force, I.S.O.F.T. The ISHNE holter standard output file format. Ann. Noninvasive Electrocardiol. 1998, 3, 263–266. [Google Scholar] [CrossRef]
- Trigo, J.D.; Chiarugi, F.; Alesanco, Á.; Martínez-Espronceda, M.; Serrano, L.; Chronaki, C.E.; Escayola, J.; Martínez, I.; García, J. SCP-ECG in an ISO/IEEE 11073-PHD world: Store-and-forward transmission and messaging part. In Proceedings of the 2009 9th International Conference on Information Technology and Applications in Biomedicine, Larnaka, Cyprus, 4–7 November 2009; pp. 1–4. [Google Scholar]
- Fischer, R.; Chiarugi, F.; Schmid, J.; Norgall, T.; Zywietz, C. Communication and Retrieval of ECG data: How many standards do we need? In Proceedings of the Computers in Cardiology, Thessaloniki, Greece, 21–24 September 2003; pp. 21–24. [Google Scholar]
- Stockbridge, N.; Brown, B.D. Annotated ECG waveform data at FDA1. J. Electrocardiol. 2004, 37, 63. [Google Scholar] [CrossRef]
- Rubio, Ó.J.; Alesanco, Á.; García, J. A robust and simple security extension for the medical standard SCP-ECG. J. Biomed. Inform. 2013, 46, 142–151. [Google Scholar] [CrossRef]
- Hsieh, J.C.; Lo, H.C. The clinical application of a PACS-dependent 12-lead ECG and image information system in E-medicine and telemedicine. J. Digit. Imaging 2010, 23, 501–513. [Google Scholar] [CrossRef]
- Trigo, J.D.; Chiarugi, F.; Alesanco, Á.; Martínez-Espronceda, M.; Chronaki, C.E.; Escayola, J.; Martínez, I.; García, J. Standard-compliant real-time transmission of ECGs: Harmonization of ISO/IEEE 11073-PHD and SCP-ECG. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 4635–4638. [Google Scholar]
- Trigo, J.D.; Martínez, I.; Alesanco, A.; Kollmann, A.; Escayola, J.; Hayn, D.; Schreier, G.; García, J. An integrated healthcare information system for end-to-end standardized exchange and homogeneous management of digital ECG formats. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 518–529. [Google Scholar] [CrossRef] [PubMed]
- Badawi, H.F.; Laamarti, F.; El Saddik, A. ISO/IEEE 11073 personal health device (X73-PHD) standards compliant systems: A systematic literature review. IEEE Access 2018, 7, 3062–3073. [Google Scholar] [CrossRef]
- Schmitt, L.; Espina, J.; Falck, T.; Wang, D. Biosensor communication technology and standards. In Handbook of Biomedical Telemetry; John Wiley & Sons: Hoboken, NJ, USA, 2014; pp. 330–367. [Google Scholar]
- Trigo, J.D.; Chiarugi, F.; Alesanco, A.; Martínez-Espronceda, M.; Serrano, L.; Chronaki, C.E.; Escayola, J.; Martínez, I.; García, J. Interoperability in digital electrocardiography: Harmonization of ISO/IEEE x73-PHD and SCP-ECG. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 1303–1317. [Google Scholar] [CrossRef]
- PDF Association. 2022. Available online: https://www.pdfa.org/resource/iso-19005-pdfa/ (accessed on 5 September 2022).
- Chronaki, C.; Chiarugi, F.; Fischer, R. OpenECG: Promoting interoperability through the consistent implementation of the SCP-ECG standard in electrocardiography. Stud. Health Technol. Inform. 2007, 129, 1484. [Google Scholar]
- Faro, A.; Giordano, D.; Kavasidis, I.; Spampinato, C. A web 2.0 telemedicine system integrating TV-centric services and Personal Health Records. In Proceedings of the 10th IEEE International Conference on Information Technology and Applications in Biomedicine, Corfu, Greece, 3–5 November 2010; pp. 1–4. [Google Scholar]
- Benhamida, A.; Zouaoui, A.; Gábor, S.; Karóczkai, K.; Slimani, G.; Kozlovszky, M. Problems in archiving long-term continuous ECG data–a review. In Proceedings of the 2019 IEEE 17th World Symposium on Applied Machine Intelligence and Informatics (SAMI), Herlany, Slovakia, 24–26 January 2019; pp. 263–268. [Google Scholar]
- Laakko, T.; Leppänen, J.; Lähteenmäki, J.; Nummiaho, A. Mobile health and wellness application framework. Methods Inf. Med. 2008, 47, 217–222. [Google Scholar] [PubMed]
- Benhamida, A.; Kozlovzky, M. Human ECG data collection, digitalization, streaming and storing. In Proceedings of the 2020 IEEE 18th World Symposium on Applied Machine Intelligence and Informatics (SAMI), Herlany, Slovakia, 23–25 January 2020; pp. 105–110. [Google Scholar]
- Sassi, R.; Sparagino, L.; Stockbridge, N.L.; Guadiana, J.M.; Badilini, F. Proof of concept for an international long-time preservation ECG format. In Proceedings of the Computing in Cardiology 2014, Cambridge, MA, USA, 7–10 September 2014; pp. 461–464. [Google Scholar]
- Long, N. Open ECG data standard: Philips medical systems perspective. J. Electrocardiol. 2003, 36, 167. [Google Scholar] [CrossRef]
- Baranova, O. Open data formats in building information modeling. In E3S Web of Conferences; EDP Sciences: Paris, France, 2021; Volume 263, p. 04062. [Google Scholar]
- Goode, A.; Gilbert, B.; Harkes, J.; Jukic, D.; Satyanarayanan, M. OpenSlide: A vendor-neutral software foundation for digital pathology. J. Pathol. Inform. 2013, 4, 27. [Google Scholar] [CrossRef]
- Yuan, S.; Wei, D.; Xu, W. An architecture for cross-hospital access to electrocardiogram data. Telemed. e-Health 2011, 17, 553–559. [Google Scholar] [CrossRef]
- Kumar, M.A.; Srinivasan, A.; Bussa, N. HTML5 powered web application for telecardiology: A case study using ECGs. In Proceedings of the 2013 IEEE Point-of-Care Healthcare Technologies (PHT), Bangalore, India, 16–18 January 2013; pp. 156–159. [Google Scholar]
- Lu, X.; Duan, H.; Zheng, H. XML-ECG: An XML-based ECG presentation for data exchanging. In Proceedings of the 2007 1st International Conference on Bioinformatics and Biomedical Engineering, Wuhan, China, 6–8 July 2007; pp. 1141–1144. [Google Scholar]
- Feltus, C.; Nicolas, D.; Poupart, C. Towards a HL7 based Metamodeling Integration Approach for Embracing the Privacy of Healthcare Patient Records Administration. In Proceedings of the Proceedings of the 7th International Conference on Security of Information and Networks, Glasgow, UK, 9–11 September 2014; pp. 109–116. [Google Scholar]
- Helfenbein, E.; Gregg, R.; Zhou, S. Philips medical systems support for open ECG and standardization efforts. In Proceedings of the Computers in Cardiology, Chicago, IL, USA, 19–22 September 2004; pp. 393–396. [Google Scholar]
- Helfenbein, E.; Gregg, R.; Zhou, S. Philips Medical Systems support for open access and use of electrocardiographic data. J. Electrocardiol. 2005, 38, 35. [Google Scholar] [CrossRef]
- Wang, H.; Jung, B.; Azuaje, F.; Black, N. ecgml: Tools and technologies for multimedia ECG presentation. In Conference Proceedings XML Europe; DeepX Ltd.: Tokyo, Japan, 2003. [Google Scholar]
- Wang, H.; Azuaje, F.; Jung, B.; Black, N. A markup language for electrocardiogram data acquisition and analysis (ecgML). BMC Med. Inform. Decis. Mak. 2003, 3, 1–13. [Google Scholar] [CrossRef][Green Version]
- Fang, Q.; Sufi, F.; Cosic, I. A mobile device based ECG analysis system. Data Min. Med. Biol. Res. 2008, 320. [Google Scholar]
- Saikia, A.; Sill, S.; Baruah, S.M.; Roy, S.; Das, B.R. Android interface for handling ECG data from GE MAC 600 ECG system. In Proceedings of the 2020 International Conference on Computational Performance Evaluation (ComPE), Shillong, India, 2–4 July 2020; pp. 771–776. [Google Scholar]
- Mittal, S.; Movsowitz, C.; Steinberg, J.S. Ambulatory external electrocardiographic monitoring: Focus on atrial fibrillation. J. Am. Coll. Cardiol. 2011, 58, 1741–1749. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.J.; Hwang, H.J. Dynamic Message Server for Personal Health Data Transmission in u-Health Service Environment. In International Conference on Hybrid Information Technology; Springer: New York, NY, USA, 2011; pp. 459–466. [Google Scholar]
- Kimura, E.; Norihiko, T.; Ishihara, K. Development MFER (medical waveform format encoding rules) parser. In AMIA Annual Symposium Proceedings; American Medical Informatics Association: Bethesda, MD, USA, 2006; Volume 2006, p. 985. [Google Scholar]
- Kim, J.P.; Choi, M.S.; Park, H.K.; Choi, J. Development of Biosignal Telemonitoring System Based on HL7 and MFER Standard. J. Korean Soc. Med. Inform. 2004, 10, 387–395. [Google Scholar] [CrossRef]
- Hiraia, M.; Masudab, G. ECG description in MFER and HL7 version 3. In Proceedings of the APAMI&CJKMI-KOSMI Conf, Beijing, China, 22–27 July 2007; Volume 9, p. 2. [Google Scholar]
- Villamil, C.A.; Landínez, S.F.; López, D.M.; Blobel, B. A Mobile ECG System for the Evaluation of Cardiovascular Risk. In Proceedings of the MIE, Munich, Germany, 28 August–2 September 2016; pp. 210–214. [Google Scholar]
- Bravo-Zanoguera, M.; Cuevas-González, D.; Reyna, M.A.; García-Vázquez, J.P.; Avitia, R.L. Fabricating a Portable ECG Device Using AD823X Analog Front-End Microchips and Open-Source Development Validation. Sensors 2020, 20, 5962. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, B.; Pereira Filho, J.G.; Andreão, R.V. ECGWARE: An ECG Markup Language for Ambulatory Telemonitoring and Decision Making Support. In HEALTHINF (2); Springer: Funchal, Portugal, 2008; pp. 37–43. [Google Scholar]
- Shishedjiev, B.; Goranova, M.; Georgieva, J. XML-based language for specific scientific data description. In Proceedings of the 2010 Fifth International Conference on Internet and Web Applications and Services, Barcelona, Spain, 9–15 May 2010; pp. 345–350. [Google Scholar]
- Li, X.; Vojisavljevic, V.; Fang, Q. An XML based middleware for ECG format conversion. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 1691–1694. [Google Scholar]
- Mahesh, V.; Kandaswamy, A.; Venkatesan, R. Telecardiology for rural health care. Int. J. Recent Trends Eng. 2009, 2, 6. [Google Scholar]
- Sourd, F.P. XML, JSON y el intercambio de información. Anu. Cienc. UNAH 2022, 18, 1–10. [Google Scholar]
- Bourhis, P.; Reutter, J.L.; Vrgoč, D. JSON: Data model and query languages. Inf. Syst. 2020, 89, 101478. [Google Scholar] [CrossRef]
- Pramukantoro, E.S.; Gofuku, A. Prototype of Multi-Layer Personal Cardiac Monitoring System for Data Interoperability Problem. In Proceedings of the SIET ’20: 5th International Conference on Sustainable Information Engineering and Technology, Malang, Indonesia, 16–17 November 2020; Association for Computing Machinery: New York, NY, USA, 2020; pp. 84–89. [Google Scholar] [CrossRef]
- Dolin, R.H.; Alschuler, L.; Boyer, S.; Beebe, C.; Behlen, F.M.; Biron, P.V.; Shabo, A. HL7 clinical document architecture, release 2. J. Am. Med. Inform. Assoc. 2006, 13, 30–39. [Google Scholar] [CrossRef]
- Finet, P.; Gibaud, B.; Dameron, O.; Jeannès, R.L.B. Interoperable infrastructure and implementation of a health data model for remote monitoring of chronic diseases with comorbidities. IRBM 2018, 39, 151–159. [Google Scholar] [CrossRef]
- Sassi, R.; Bond, R.R.; Cairns, A.; Finlay, D.D.; Guldenring, D.; Libretti, G.; Isola, L.; Vaglio, M.; Poeta, R.; Campana, M.; et al. Pdf–ecg in clinical practice: A model for long–term preservation of digital 12–lead ecg data. J. Electrocardiol. 2017, 50, 776–780. [Google Scholar] [CrossRef]
- Javed, A.; Sundrani, A.; Malik, N.; Prescott, S.M. CSV Automation. In Robotic Process Automation using UiPath StudioX: A Citizen Developer’s Guide to Hyperautomation; Apress: Berkeley, CA, USA, 2021; pp. 413–428. [Google Scholar] [CrossRef]
- Ramsdale, A.; Shiaeles, S.; Kolokotronis, N. A comparative analysis of cyber-threat intelligence sources, formats and languages. Electronics 2020, 9, 824. [Google Scholar] [CrossRef]
- Haider, N.; Hossain, F. CSV2RDF: Generating RDF data from CSV file using semantic web technologies. J. Theor. Appl. Inf. Technol. 2018, 96, 6889–6902. [Google Scholar]
- Tapsai, C. Information Processing and Retrieval from CSV File by Natural Language. In Proceedings of the 2018 IEEE 3rd International Conference on Communication and Information Systems (ICCIS), Singapore, 28–30 December 2018; pp. 212–216. [Google Scholar] [CrossRef]
- Dagliati, A.; Malovini, A.; Tibollo, V.; Bellazzi, R. Health informatics and EHR to support clinical research in the COVID-19 pandemic: An overview. Brief. Bioinform. 2021, 22, 812–822. [Google Scholar] [CrossRef]
- Ge, C.; Li, Y.; Eilebrecht, E.; Chandramouli, B.; Kossmann, D. Speculative Distributed CSV Data Parsing for Big Data Analytics. In Proceedings of the SIGMOD ’19: 2019 International Conference on Management of Data, Amsterdam, The Netherlands, 30 June–5 July 2019; Association for Computing Machinery: New York, NY, USA, 2019; pp. 883–899. [Google Scholar] [CrossRef]
- Mahmud, S.M.H.; Hossin, M.A.; Hasan, M.R.; Jahan, H.; Noori, S.R.H.; Ahmed, M.R. Publishing CSV Data as Linked Data on the Web. In Proceedings of the ICETIT 2019; Singh, P.K., Panigrahi, B.K., Suryadevara, N.K., Sharma, S.K., Singh, A.P., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 805–817. [Google Scholar]
- Ndlovu, K.; Scott, R.E.; Mars, M. Interoperability opportunities and challenges in linking mHealth applications and eRecord systems: Botswana as an exemplar. BMC Med. Inform. Decis. Mak. 2021, 21, 246. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, M.M.; Farooq, A.; Qureshi, M.M. Current eHealth Challenges and recent trends in eHealth applications. arXiv 2021, arXiv:2103.01756. [Google Scholar]
- Hamberger, M.; Ikonomi, N.; Schwab, J.D.; Werle, S.D.; Fürstberger, A.; Kestler, A.M.; Holderried, M.; Kaisers, U.X.; Steger, F.; Kestler, H.A.; et al. Interaction Empowerment in Mobile Health: Concepts, Challenges, and Perspectives. JMIR mHealth uHealth 2022, 10, e32696. [Google Scholar] [CrossRef]
- Valdivia, R.; Navarrete, M. Open standards and interoperability: GTFS case. Ingeniare Rev. Chil. Ing. 2016, 24, 184. [Google Scholar]
- Landman, A.B.; Rokos, I.C.; Burns, K.; Van Gelder, C.M.; Fisher, R.M.; Dunford, J.V.; Cone, D.C.; Bogucki, S. An open, interoperable, and scalable prehospital information technology network architecture. Prehosp. Emerg. Care 2011, 15, 149–157. [Google Scholar] [CrossRef]
- Kurnia Wibowo, D. Perbandingan Format Data Json, XML DAN CSV Pada Proses Replikasi Multi-Master Server Nosql Database Berbasis Document Stored. Ph.D. Thesis, Universitas Siliwangi, Tasikmalaya, Indonesia, 2020. [Google Scholar]
- Mahmud, S.M.H.; Hossin, M.A.; Jahan, H.; Noori, S.R.H.; Bhuiyan, T. CSV-ANNOTATE: Generate annotated tables from CSV file. In Proceedings of the 2018 International Conference on Artificial Intelligence and Big Data (ICAIBD), Chengdu, China, 26–28 May 2018; pp. 71–75. [Google Scholar] [CrossRef]
- Truică, C.O.; Apostol, E.S.; Darmont, J.; Pedersen, T.B. The Forgotten Document-Oriented Database Management Systems: An Overview and Benchmark of Native XML DODBMSes in Comparison with JSON DODBMSes. Big Data Res. 2021, 25, 100205. [Google Scholar] [CrossRef]
- Zermeño-Campos, N.A.; Cuevas-González, D.; García-Vázquez, J.P.; López-Avitia, R.; Bravo-Zanoguera, M.E.; Reyna, M.A.; Díaz-Ramírez, A. PÉEK: A cloud-based application for automatic electrocardiogram pre-diagnosis. SoftwareX 2022, 19, 101124. [Google Scholar] [CrossRef]
- Cuevas-González, D.; García-Vázquez, J.P.; Bravo-Zanoguera, M.; López-Avitia, R.; Reyna, M.A.; Amezquita-García, J.A. System for Continuous and Prolonged Ambulatory ECG Monitoring with Hosting and Visualization on the Cloud. Eng. Proc. 2021, 10, 57. [Google Scholar]
- Church, G.M.; Gao, Y.; Kosuri, S. Next-generation digital information storage in DNA. Science 2012, 337, 1628. [Google Scholar] [CrossRef] [PubMed]
- Bornholt, J.; Lopez, R.; Carmean, D.M.; Ceze, L.; Seelig, G.; Strauss, K. A DNA-based archival storage system. In Proceedings of the Twenty-First International Conference on Architectural Support for Programming Languages and Operating Systems, Atlanta, GA, USA, 2–6 April 2016; pp. 637–649. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuevas-González, D.; García-Vázquez, J.P.; Bravo-Zanoguera, M.; López-Avitia, R.; Reyna, M.A.; Zermeño-Campos, N.A.; González-Ramírez, M.L. ECG Standards and Formats for Interoperability between mHealth and Healthcare Information Systems: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 11941. https://doi.org/10.3390/ijerph191911941
Cuevas-González D, García-Vázquez JP, Bravo-Zanoguera M, López-Avitia R, Reyna MA, Zermeño-Campos NA, González-Ramírez ML. ECG Standards and Formats for Interoperability between mHealth and Healthcare Information Systems: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(19):11941. https://doi.org/10.3390/ijerph191911941
Chicago/Turabian StyleCuevas-González, Daniel, Juan Pablo García-Vázquez, Miguel Bravo-Zanoguera, Roberto López-Avitia, Marco A. Reyna, Nestor Alexander Zermeño-Campos, and María Luisa González-Ramírez. 2022. "ECG Standards and Formats for Interoperability between mHealth and Healthcare Information Systems: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 19: 11941. https://doi.org/10.3390/ijerph191911941
APA StyleCuevas-González, D., García-Vázquez, J. P., Bravo-Zanoguera, M., López-Avitia, R., Reyna, M. A., Zermeño-Campos, N. A., & González-Ramírez, M. L. (2022). ECG Standards and Formats for Interoperability between mHealth and Healthcare Information Systems: A Scoping Review. International Journal of Environmental Research and Public Health, 19(19), 11941. https://doi.org/10.3390/ijerph191911941