Psychosocial Determinants of Loneliness in the Era of the COVID-19 Pandemic—Cross-Sectional Study
Abstract
:1. Introduction
- What is the level of loneliness in the study group and what are the links between sociodemographic and psychosocial factors?
- Is there a link between feelings of loneliness and the quality of life of the subjects?
- Is there a link between feelings of loneliness, self-efficacy and quality of life and the way you work during the ongoing pandemic?
2. Material and Methods
2.1. Research Material
2.2. Research Methods
2.3. Statistical Analysis
3. Results
3.1. Socio-Demographic Characteristics of the Surveyed Persons
3.2. Level of Loneliness, Quality of Life and Generalized Self-Efficacy in the Study Group
3.3. Feeling Lonely, Linked to Quality of Life and Generalized Self-Efficacy
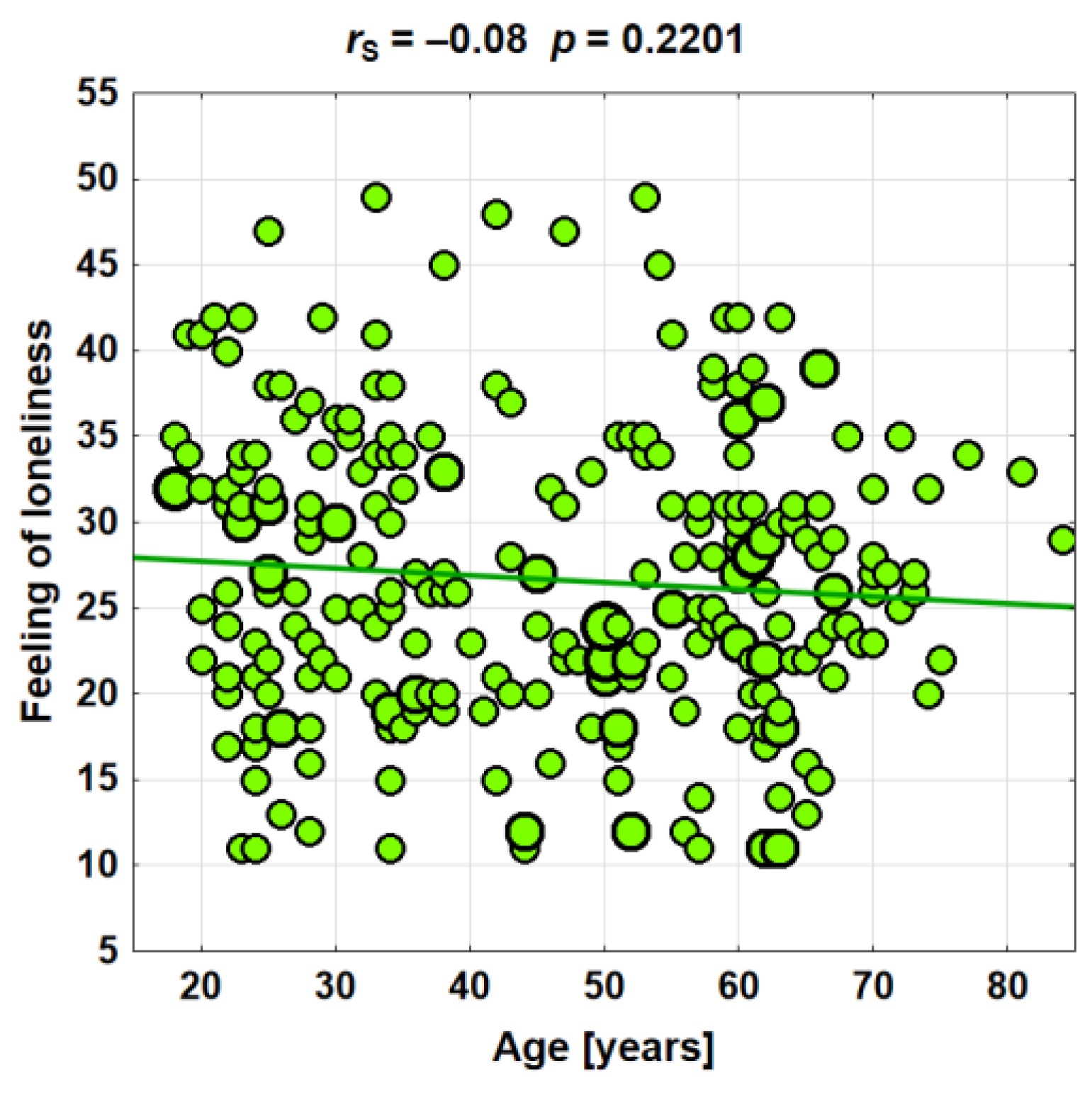
3.4. The Level of Loneliness in Relation to Sociodemographic Factors
3.5. Feelings of Loneliness in Connection with Psychosocial Factors
3.6. Feeling Lonely, Self-Efficacy and Quality of Life in Connection with the Mode of Work Performed
4. Discussion
Limitations Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ayittey, F.K.; Ayittey, M.K.; Chiwero, N.B.; Kamasah, J.S.; Dzuvor, C. Economic impacts of Wuhan 2019-nCoV on China and the world. J. Med. Virol. 2020, 92, 473. [Google Scholar] [CrossRef] [PubMed]
- Sidhom, O. Physical and mental health aspects in COVID-19: Two sides of a coin. Avicenna 2021, 2, 6. [Google Scholar] [CrossRef]
- Kooli, C. COVID-19 and the mental health of professionals in the health sector in the UAE: An analytical study. Avicenna 2021, 2, 9. [Google Scholar] [CrossRef]
- Creese, B.; Khan, Z.; Henley, W.; O’Dwyer, S.; Corbett, A.; Da Silva, M.V.; Mills, K.; Wright, N.; Testad, I.; Aarsland, D.; et al. Loneliness, physical activity, and mental health during COVID-19: A longitudinal analysis of depression and anxiety in adults over the age of 50 between 2015 and 2020. Int. Psychogeriatr. 2021, 33, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Seifert, A.; Hassler, B. Impact of the COVID-19 pandemic on loneliness among older adults. Front. Sociol. 2020, 5, 590935. [Google Scholar] [CrossRef]
- McGinty, E.E.; Presskreischer, R.; Han, H.; Barry, C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA 2020, 324, 93–94. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Maqsood, A.; Saleem, J.; Butt, M.S.; Shahzad, R.B.; Zubair, R.; Ishaq, M. Effects of the COVID-19 pandemic on perceived stress levels of employees working in private organizations during lockdown. Avicenna 2021, 2, 2021. [Google Scholar] [CrossRef]
- Kooli, C. Perspectives of social policies and programs in the post—COVID-19 era. Avicenna 2022, 2022, 1. [Google Scholar] [CrossRef]
- Dalila Talevi, D.; Valentina Socci, V.; Carai, M.; Carnaghi, G.; Faleri, S.; Trebbi, E.; Di Bernardo, A.; Capelli, F.; Pacitti, F. Mental health outcomes of the COVID-19 pandemic. Riv. Psichiatr. 2020, 55, 137–144. [Google Scholar]
- Banerjee, D.; Rai, M. Social Isolation in COVID-19: The Impact of Loneliness; SAGE Publications Sage UK: London, UK, 2020. [Google Scholar]
- Smith, B.J.; Lim, M.H. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res Pract. 2020, 30, 3022008. [Google Scholar] [CrossRef]
- Heitzman, J. Impact of COVID-19 pandemic on mental health. Psychiatr Pol. 2020, 54, 187–198. [Google Scholar] [CrossRef]
- Kim, H.K. In the COVID-19 Era, Effects of Job Stress, Coping Strategies, Meaning in Life, and Resilience on Psychological Well-Being of Women Workers in the Service Sector. Int. J. Environ. Res. Public Health 2022, 19, 9824. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Zhu, G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 2020, 7, 300–302. [Google Scholar] [CrossRef]
- Li, S.; Zhang, Y. Mental healthcare for psychiatric inpatients during the COVID-19 epidemic. General Psychiatr. 2020, 33, e100216. [Google Scholar] [CrossRef]
- Ernst, M.; Niederer, D.; Werner, A.M.; Czaja, S.J.; Mikton, C.; Ong, A.D.; Rosen, T.; Brähler, E.; Beutel, M.E. Lonelines before and during the COVID-19 pandemic: A systematic review with meta-analysis. Am. Psychol. 2022, 376–377, 756–765. [Google Scholar] [CrossRef]
- Cacioppo, S.; Grippo, A.J.; London, S.; Goossens, L.; Cacioppo, J.T. Loneliness: Clinical import and interventions. Perspect. Psychol. Sci. 2015, 10, 238–249. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.R.; Kadoya, Y. Loneliness during the COVID-19 Pandemic: A Comparison between Older and Younger People. Int. J. Environ. Res. Public Health 2021, 18, 7871. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Patrick, W. (Eds.) Loneliness: Human Nature and the Need for Social Connection; W.W. Norton: New York, NY, USA, 2008; p. 288. [Google Scholar]
- Weiss, R.S. Loneliness: The Experience of Emotional and Social Isolation; MIT Press: Cambridge, UK, 1973. [Google Scholar]
- Leigh-Hunt, N.; Bagguley, B.; Bash, K.; Turner, V.; Turnbull, S.S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef]
- Xia, N.; Li, H. Loneliness, Social Isolation, and Cardiovascular Health. Antioxid. Redox Signal 2018, 28, 837–851. [Google Scholar] [CrossRef]
- Jeste, D.V.; Lee, E.E.; Cacioppo, S. Battling the Modern Behavioral Epidemic of Loneliness: Suggestions for Research and Interventions. JAMA Psychiatry 2020, 77, 553–554. [Google Scholar] [CrossRef] [PubMed]
- Simard, J.; Volicer, L. Loneliness and Isolation in Long-term Care and the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 966–967. [Google Scholar] [CrossRef] [PubMed]
- Anderson, G.O.; Colette, E.T. Loneliness and Social Connections: A National Survey of Adults 45 and Older; American Association of Retired Persons Research: Washington, DC, USA, 2018. [Google Scholar]
- Lew-Koralewicz, A. Psychosocial Functioning and the Educational Experiences of Students with ASD during the COVID-19 Pandemic in Poland. Int. J. Environ. Res. Public Health 2022, 19, 9468. [Google Scholar] [CrossRef]
- Gu, S.; He, Z.; Sun, L.; Jiang, Y.; Xu, M.; Feng, G.; Ma, X.; Wang, F.; Huang, J.H. Effects of Coronavirus-19 Induced Loneliness on Mental Health: Sleep Quality and Intolerance for Uncertainty as Mediators. Front. Psychiatry 2021, 12, 738003. [Google Scholar] [CrossRef] [PubMed]
- Erzen, E.; Çikrikci, Ö. The effect of loneliness on depression: A meta-analysis. Int. J. Soc. Psychiatry 2018, 64, 427–435. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Thisted, R.A.; Masi, C.M.; Cacioppo, J.T. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol. Aging 2010, 25, 132–141. [Google Scholar] [CrossRef]
- AARP Foundation. The Pandemic Effect: A Social Isolation Report; AARP Foundation: Washington, DC, USA, 2020. [Google Scholar]
- Juczyński, Z. Skala uogólnionej wlasnej skuteczności—GSES. In Narzędzia Pomiaru W Promocji I Psychologii Zdrowia; Pracownia Testόw Psychologicznych Polskiego Towarzystwa Psychologicznego: Warsaw, Poland, 2012; p. 188. (In Polish) [Google Scholar]
- Grygiel, P.; Humenny, G.; Rębisz, S.; Świtaj, P.; Sikorska-Grygiel, J. Validating the Polish adaptation of the 11-item De Jong Gierveld Loneliness Scale. Eur. J. Psychol. Assess. 2012, 29, 129–139. [Google Scholar] [CrossRef]
- Jaracz, K.; Kalfoss, M.; Górna, K.; Baczyk, G. Quality of life in Polish respondents: Psychometric properties of the Polish WHOQOL-Bref. Scand. J. Caring Sci. 2006, 20, 251–260. (In Polish) [Google Scholar] [CrossRef]
- Xiao, C. A novel approach of consultation on 2019 novel coronavirus (COVID–19)-Related psychological and mental problems: Structured letter therapy. Psychiatry Investig. 2020, 17, 175–176. [Google Scholar] [CrossRef]
- Kmietowicz, Z. Rules on isolation rooms for suspected COVID–19 cases in GP surgeries to be relaxed. BMJ 2020, 368, m707. [Google Scholar] [CrossRef]
- Kosowski, P.; Mróz, J. Ocena komunikacji a poczucie samotności i satysfakcji z życia w czasie pandemii. The assessment of communication and the sense of loneliness and life satisfaction during the pandemic. Dialog, Komunikacja. Ujęcie interdyscyplinarne. Kwart. Nauk. Fides Ratio 2020, 2, 214–226. (In Polish) [Google Scholar]
- Zhou, H.; Yue, X.D.; Zhang, X.; Shangguan, F.; Zhang, X.Y. Self-efficacy and mental health problems during COVID-19 pandemic: A multiple mediation model based on the Health Belief Model. Pers. Individ. Differ. 2021, 179, 110893. [Google Scholar] [CrossRef]
- Gu, S.; Wang, F.; Cao, C.; Wu, E.; Tang, Y.Y.; Huang, J.H. An integrative way for studying neural basis of basic emotions with fMRI. Front Neurosci. 2019, 13, 628. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Zhang, D.; Wu, M.; Yang, Y.; Xie, H.; Li, Y.; Jia, J.; Su, Y. Loneliness and depression symptoms among the elderly in nursing homes: A moderated mediation model of resilience and social support. Psychiatry Res. 2018, 268, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Vanhalst, J.; Luyckx, K.; Van Petegem, S.; Soenens, B. The detrimental effects of adolescents’ chronic loneliness on motivation and emotion regulation in social situations. J. Youth Adolesc. 2018, 47, 162–176. [Google Scholar] [CrossRef]
- Gu, S.; Wang, F.; Patel, N.P.; Bourgeois, J.A.; Huang, J.H. A model for basic emotions using observations of behavior in Drosophila. Front Psychol. 2019, 10, 781. [Google Scholar] [CrossRef]
- Giuntella, O.; Hyde, K.; Saccardo, S.; Sadoff, S. Lifestyle and mental health disruptions during COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2016632118. [Google Scholar] [CrossRef]
- Brodeur, A.; Clark, A.E.; Fleche, S.; Powdthavee, N. COVID-19, lockdowns and well-being: Evidence from google trends. J Public Econ. 2021, 193, 104346. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID–19 outbreak. Asian J. Psychiatr. 2020, 51, 102076. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G. The psychological impact of the COVID–19 epidemic on college students in China. Psychiat. Res. 2020, 287, 112934. [Google Scholar] [CrossRef] [PubMed]
- Sareen, J.; Erickson, J.; Medved, M.I.; Asmundson, G.J.G.; Enns, M.W.; Stein, M.; Leslie, W.; Doupe, M.; Logsetty, S. Risk factors for post-injury mental health problems. Depress. Anxiety 2013, 30, 321–327. [Google Scholar] [CrossRef]
- Casale, S. Interpersonally-based fears during the COVID-19 pandemic: Reflections on the fear of missing out and the fear of not mattering constructs. Clin. Neuropsychiatry 2020, 17, 88–93. [Google Scholar] [CrossRef]
- Perlman, D.; Landolt, M.A. Examination of loneliness in children–adolescents and in adults: Two solitudes or unified enterprise? In Loneliness in Childhood and Adolescence; Rotenberg, K.J., Hymel, S., Eds.; Cambridge University Press: Cambridge, UK, 1999; pp. 325–347. [Google Scholar]
- Lampraki, C.; Hoffman, A.; Roquet, A.; Jopp, D.S. Loneliness during COVID-19: Development and influencing factors. PLoS ONE 2022, 17, e0265900. [Google Scholar] [CrossRef] [PubMed]
- Losada-Baltar, A.; Jiménez-Gonzalo, L.; Gallego-Alberto, L.; Pedroso-Chaparro, M.D.S.; Fernandes-Pires, J.; Márquez-González, M. “We are staying at home” Association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 76, e10–e16. [Google Scholar] [CrossRef]
- Pai, N.; Shae-Leigh Vella, S.-L. COVID-19 and loneliness: A rapid systematic review. Aust. N. Z. J. Psychiatry 2021, 55, 1144–1156. [Google Scholar] [CrossRef]
- Wang, B.; Liu, Y.; Qia, J.; Parker, S.K. Achieving Effective Remote Working During the COVID-19 Pandemic: A Work Design Perspective. Appl. Psychol. 2021, 70, 16–59. [Google Scholar] [CrossRef] [PubMed]
- Kooli, C. Challenges of working from home during the COVID-19 pandemic for women in the UAE. J. Public Aff. 2022, e2829. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, R.; Burns, A.; Leavey, G.; Leroi, I.; Burholt, V.; Lubben, J.; Holt-Lunstad, J.; Victor, C.; Brian Lawlor, B.; Vilar-Compte, M.; et al. Impact of the COVID-19 Pandemic on Loneliness and Social Isolation: A Multi-Country Study. Int. J. Environ. Res. Public Health 2021, 18, 9982. [Google Scholar] [CrossRef]


| Variables | Total n = 262 |
|---|---|
| Age in years, | |
| Mean ± SD | 45.8 ± 16.6 |
| Min. | 18 |
| Max. | 84 |
| Median (Q1–Q3) | 47.5 (30–60) |
| Gender, (%) | |
| -women | 80.9 |
| -men | 19.1 |
| Education, (%) | |
| -vocational | 3.0 |
| -medium | 21.4 |
| -higher | 75.6 |
| Place of residence, (%) | |
| -city | 82.1 |
| -village | 17.9 |
| Marital status, (%) | |
| -in a relationship | 71.4 |
| -single person | 28.6 |
| Having children, (%) | |
| -yes | 33.2 |
| Social status, (%) | |
| -working person | 65.3 |
| -pensioner | 24.0 |
| -student | 9.6 |
| -unemployed | 1.1 |
| Living with a loved one (%) | |
| -yes | 85.5 |
| Change in activity professional during the pandemic, (%) | |
| -no change | 43.7 |
| -work/remote learning | 49.3 |
| -restriction or suspension of work | 7.0 |
| Impact of the pandemic to limit the possibilities earnings, (%) | |
| -very large/large | 16.1 |
| -medium/to a small extent | 25.2 |
| -no impact | 58.7 |
| The level of stress felt, (%) | |
| -very high/high | 37.4 |
| -medium | 34.0 |
| -light/none | 28.6 |
| Degree of limitation social contacts, (%) | |
| -very | 26.0 |
| -quite significantly/medium | 57.6 |
| -to a small extent/no impact | 16.4 |
| Self-assessment of health, (%) | |
| -very good/good | 55.0 |
| -average | 34.7 |
| -very bad/bad | 10.3 |
| Does he have a chronic disease? | |
| -yes (%) | 40.8 |
| Degree of limitation of mobility in connection with the disease, (%) | |
| -very high/high | 14.0 |
| -medium | 11.2 |
| -small/none | 74.8 |
| Variables | (95%) | Me | SD | Q1 | Q3 | Min | Max |
|---|---|---|---|---|---|---|---|
| WHOQoL-BREF (0–20) | |||||||
| Somatic, mean ± SD | 14.7 (14.4–15.0) | 14.9 | 2.4 | 13.1 | 16.0 | 6.3 | 20.0 |
| Psychological field, mean ± SD | 12.8 (12.4–13.1) | 12.7 | 2.8 | 10.7 | 14.7 | 5.3 | 19.3 |
| Social field, mean ± SD | 13.9 (13.5–14.3) | 14.7 | 3.6 | 12.0 | 16.0 | 4.0 | 20.0 |
| Environment, mean ± SD | 12.6 (12.3–12.9) | 12.5 | 2.5 | 11.0 | 14.0 | 6.5 | 19.5 |
| Feeling lonely (PSS-10), mean ± SD (11–55) | 26.7 (25.7–27.7) | 26 | 8.4 | 21 | 32 | 11 | 49 |
| Self-efficacy (GSES), mean ± SD (10–40) | 29.4 (28.9–29.9) | 30 | 4.1 | 27 | 31 | 13 | 40 |
| Variables | Feeling of Loneliness |
|---|---|
| WHOQoL-BREF | |
| Somatic domain | −0.37 (p = 0.0000 ***) |
| Psychological domain | −0.54 (p = 0.0000 ***) |
| Social domain | −0.56 (p = 0.0000 ***) |
| Environment | −0.38 (p = 0.000 ***) |
| GSES | −0.35 (p = 0.0000 ***) |
| Variables | Feeling of Loneliness (p = 0.4887) | |||||
| Sex | N | Me | SD | Min | Max | |
| woman | 212 | 26.8 | 26.5 | 8.2 | 11 | 49 |
| man | 50 | 26.2 | 24.5 | 9.1 | 11 | 49 |
| Place of Residence | Feeling of Loneliness (p = 0.5806) | |||||
| N | Me | SD | Min | Max | ||
| village | 47 | 27.8 | 28 | 7.8 | 15 | 47 |
| city up to 100 thousand residents | 45 | 27.1 | 26 | 8.8 | 11 | 49 |
| city over 100 thousand residents | 170 | 26.3 | 26 | 8.4 | 11 | 49 |
| Education | Feeling of Loneliness (p = 0.4357) | |||||
| N | Me | SD | Min | Max | ||
| other | 64 | 27.4 | 27 | 8.2 | 11 | 45 |
| higher | 198 | 26.5 | 26 | 8.5 | 11 | 49 |
| Marital Status | Feeling of Loneliness (p = 0.0090 **) | |||||
| N | Me | SD | Min | Max | ||
| In a relationship | 187 | 25.8 | 25 | 8.3 | 11 | 49 |
| Single person | 75 | 28.8 | 29 | 8.3 | 12 | 49 |
| Children | Feeling of Loneliness (p = 0.6227) | |||||
| N | Me | SD | Min | Max | ||
| yes | 87 | 26.5 | 25 | 9.3 | 11 | 49 |
| no | 175 | 26.7 | 26 | 7.9 | 11 | 49 |
| Living with a Significant Other | Feeling of Loneliness (p = 0.0088 **) | |||||
| N | Me | SD | Min | Max | ||
| yes | 224 | 26.1 | 25 | 8.4 | 11 | 49 |
| no | 38 | 29.9 | 30 | 7.8 | 11 | 49 |
| Chronic Disease | Feeling of Loneliness (p = 0.3030) | |||||
| N | Me | SD | Min | Max | ||
| yes | 155 | 26.2 | 26 | 8.6 | 11 | 49 |
| no | 107 | 27.3 | 27 | 8.1 | 11 | 49 |
| Age [in Years] N; % | Sense of Lonliness (p = 0.0119 *) | ||
|---|---|---|---|
| Me | SD | ||
| <35 (90; 34.4) | 28.5 | 30 | 8.6 |
| 35–54 (87; 33.2) | 25.0 | 23 | 8.5 |
| ≥55 (85; 32.4) | 26.6 | 27 | 7.9 |
| Assessement of Life Domains (1–5) | Feeling of Loneliness |
|---|---|
| Social distancing | 0.40 (p = 0.0000 ***) |
| Experiencing negative emotions | 0.31 (p = 0.0000 ***) |
| Level of stress | 0.28 (p = 0.0000 ***) |
| Lack of emotional control, aggressive behavior | 0.18 (p = 0.0040 **) |
| The impact of the pandemic on the reduction in work | 0.16 (p = 0.0092 **) |
| Health assessment | −0.33 (p = 0.0000 ***) |
| Mode of Work | Sense of Lonliness (p = 0.1907) | |||||
| N | Me | SD | Min | Max | ||
| No change | 103 | 25.9 | 24 | 8.4 | 11 | 49 |
| Remote work | 117 | 27.5 | 27 | 9.0 | 11 | 49 |
| General Self-Efficacy (p = 0.0941) | ||||||
| N | Me | SD | Min | Max | ||
| No change | 103 | 30.0 | 30 | 3.7 | 19 | 40 |
| Remote work | 117 | 29.1 | 29 | 4.4 | 13 | 40 |
| Quality of life | ||||||
| Somatic Domain (p = 0.1969) | ||||||
| N | Me | SD | Min | Max | ||
| No change | 103 | 15.1 | 15.4 | 2.2 | 8.0 | 20.0 |
| Remote work | 117 | 14.6 | 14.9 | 2.5 | 7.4 | 19.4 |
| Psychological Domain (p = 0.0413 *) | ||||||
| N | Me | SD | Min | Max | ||
| No change | 103 | 13.3 | 13.3 | 2.8 | 6.0 | 18.7 |
| Remote work | 117 | 12.4 | 12.7 | 2.9 | 5.3 | 19.3 |
| Social Domain (p = 0.3833) | ||||||
| N | Me | SD | Min | Max | ||
| No change | 103 | 14.0 | 14.7 | 3.7 | 4.0 | 20.0 |
| Remote work | 117 | 13.6 | 14.7 | 3.9 | 4.0 | 20.0 |
| Environment (p = 0.4837) | ||||||
| N | Me | SD | Min | Max | ||
| No change | 103 | 12.7 | 12.5 | 2.5 | 6.5 | 19.5 |
| Remote work | 117 | 12.5 | 12.0 | 2.5 | 6.5 | 18.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sierakowska, M.; Doroszkiewicz, H. Psychosocial Determinants of Loneliness in the Era of the COVID-19 Pandemic—Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 11935. https://doi.org/10.3390/ijerph191911935
Sierakowska M, Doroszkiewicz H. Psychosocial Determinants of Loneliness in the Era of the COVID-19 Pandemic—Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(19):11935. https://doi.org/10.3390/ijerph191911935
Chicago/Turabian StyleSierakowska, Matylda, and Halina Doroszkiewicz. 2022. "Psychosocial Determinants of Loneliness in the Era of the COVID-19 Pandemic—Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 19: 11935. https://doi.org/10.3390/ijerph191911935
APA StyleSierakowska, M., & Doroszkiewicz, H. (2022). Psychosocial Determinants of Loneliness in the Era of the COVID-19 Pandemic—Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(19), 11935. https://doi.org/10.3390/ijerph191911935







