Exploring the Influence of a Community-Based Peer-Led Wheelchair Skills Training on Satisfaction with Participation in Children and Adolescents with Cerebral Palsy and Spina Bifida: A Pilot Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Intervention
2.4. Data Collection
2.4.1. Sociodemographic and Wheelchair Use Information
2.4.2. Outcome Measures
Primary Outcome
Secondary Outcomes
2.5. Analyses
3. Results
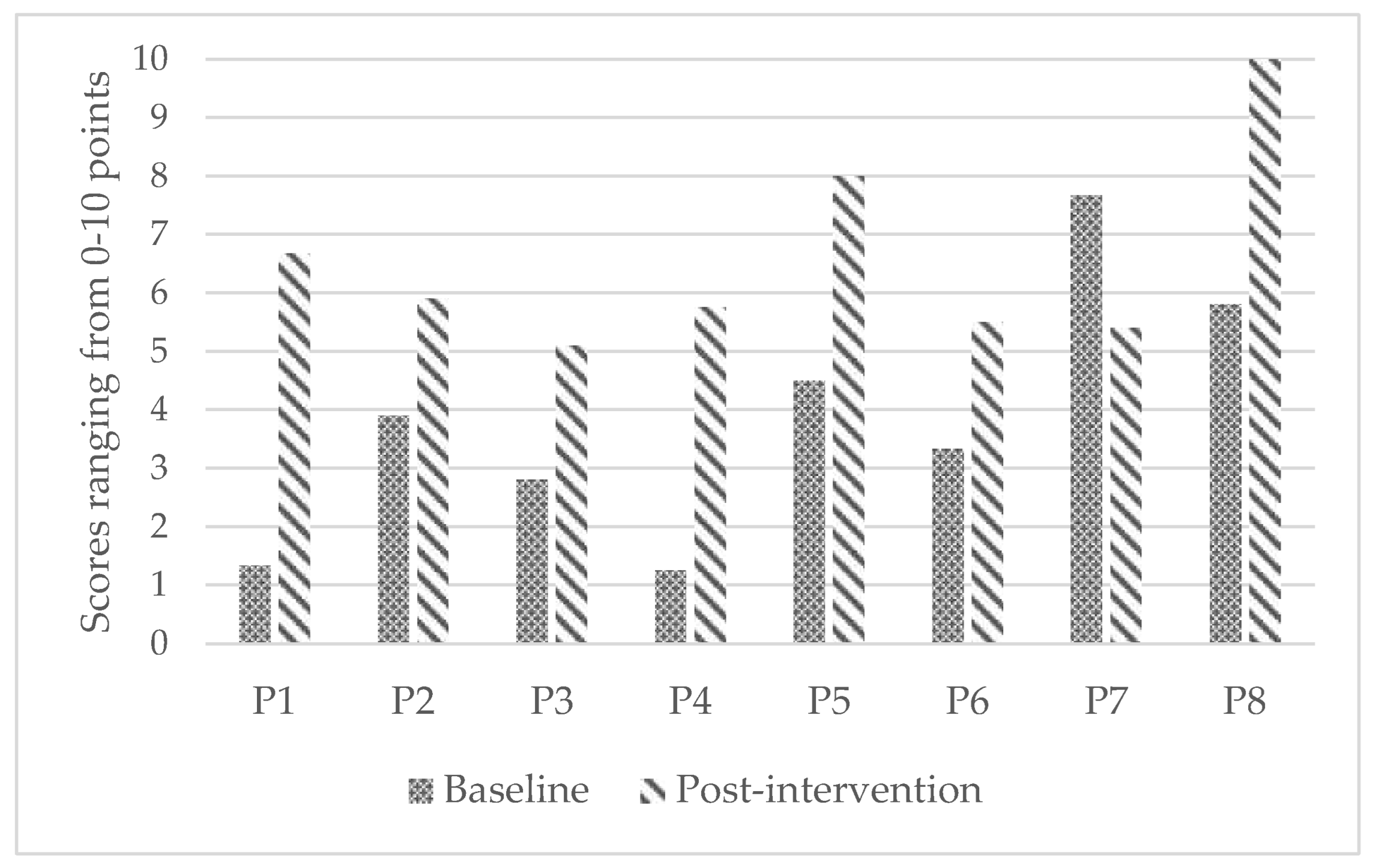
3.1. Primary Outcome
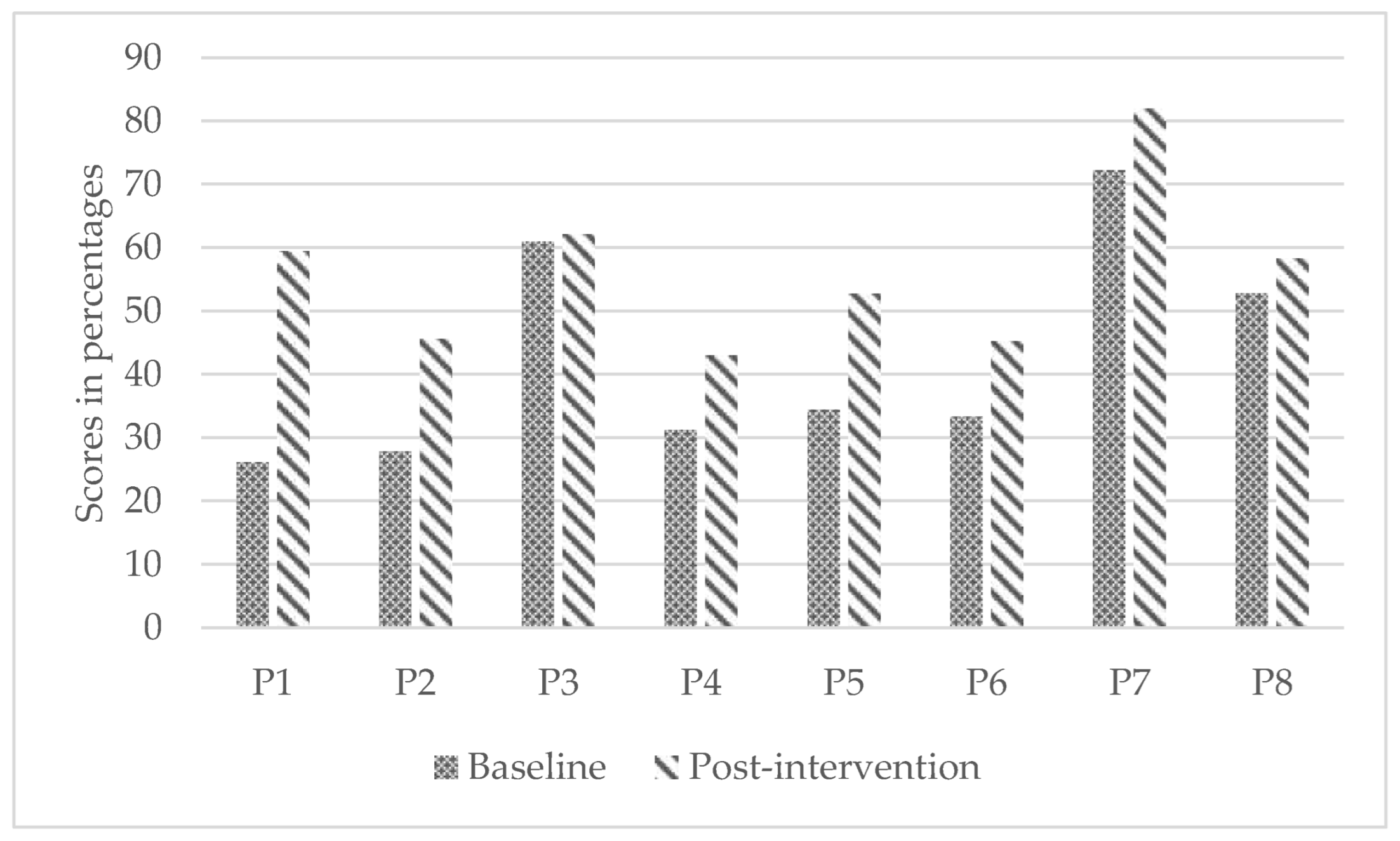
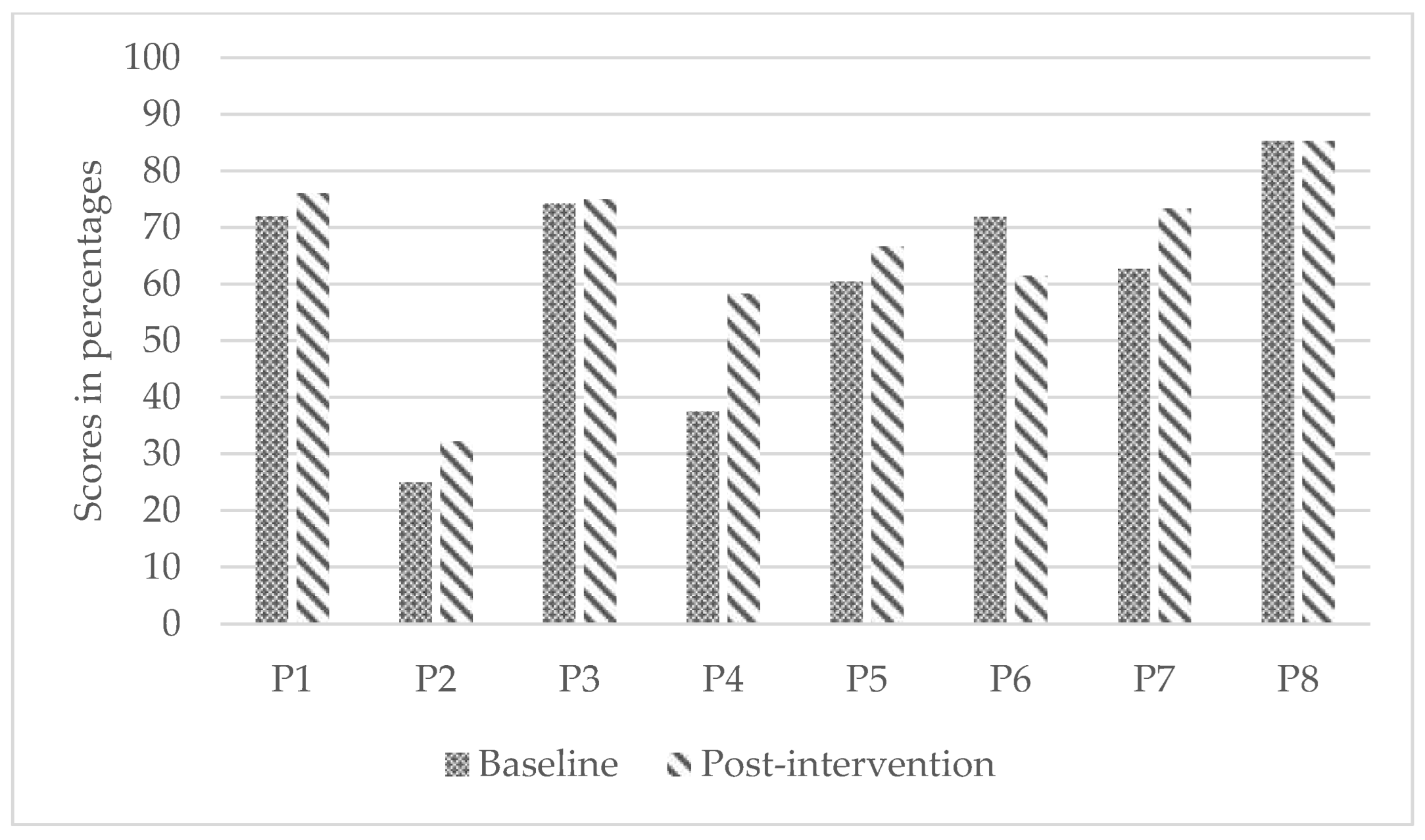
3.2. Secondary Outcomes
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oskoui, M.; Coutinho, F.; Dykeman, J.; Jetté, N.; Pringsheim, T. An Update on the Prevalence of Cerebral Palsy: A Systematic Review and Meta-Analysis. Dev. Med. Child Neurol. 2013, 55, 509–519. [Google Scholar] [CrossRef]
- Stavsky, M.; Mor, O.; Mastrolia, S.A.; Greenbaum, S.; Than, N.G.; Erez, O. Cerebral Palsy—Trends in Epidemiology and Recent Development in Prenatal Mechanisms of Disease, Treatment, and Prevention. Front. Pediatr. 2017, 5, 21. [Google Scholar] [CrossRef]
- Atta, C.A.M.; Fiest, K.M.; Frolkis, A.D.; Jette, N.; Pringsheim, T.; St Germaine-Smith, C.; Rajapakse, T.; Kaplan, G.G.; Metcalfe, A. Global Birth Prevalence of Spina Bifida by Folic Acid Fortification Status: A Systematic Review and Meta-Analysis. Am. J. Public Health 2016, 106, 159. [Google Scholar] [CrossRef]
- Kancherla, V.; Wagh, K.; Pachón, H.; Oakley, G.P. A 2019 Global Update on Folic Acid-Preventable Spina Bifida and Anencephaly. Birth Defects Res. 2021, 113, 77–89. [Google Scholar] [CrossRef]
- Lepage, C.; Noreau, L.; Bernard, P.-M. Association between Characteristics of Locomotion and Accomplishment of Life Habits in Children with Cerebral Palsy. Phys. Ther. 1998, 78, 458–469. [Google Scholar] [CrossRef]
- Simeonsson, R.J.; McMillen, J.S.; Huntington, G.S. Secondary Conditions in Children with Disabilities: Spina Bifida as a Case Example. Ment. Retard. Dev. Disabil. Res. Rev. 2002, 8, 198–205. [Google Scholar] [CrossRef]
- Bakanienė, I.; Žiukienė, L.; Vasiliauskienė, V.; Prasauskienė, A. Participation of Children with Spina Bifida: A Scoping Review Using the International Classification of Functioning, Disability and Health for Children and Youth (ICF-CY) as a Reference Framework. Medicina 2018, 54, 40. [Google Scholar] [CrossRef]
- Palisano, R.J.; Kang, L.-J.; Chiarello, L.A.; Orlin, M.; Oeffinger, D.; Maggs, J. Social and Community Participation of Children and Youth with Cerebral Palsy Is Associated with Age and Gross Motor Function Classification. Phys. Ther. 2009, 89, 1304–1314. [Google Scholar] [CrossRef]
- Shikako-Thomas, K.; Majnemer, A.; Law, M.; Lach, L. Determinants of Participation in Leisure Activities in Children and Youth with Cerebral Palsy: Systematic Review. Phys. Occup. Ther. Pediatr. 2008, 28, 155–169. [Google Scholar] [CrossRef]
- Pituch, E.; Rushton, P.W.; Ngo, M.; Heales, J.; Arguin, A.P. Powerful or Powerless? Children’s, Parents’, and Occupational Therapists’ Perceptions of Powered Mobility. Phys. Occup. Ther. Pediatr. 2019, 39, 276–291. [Google Scholar] [CrossRef]
- Rousseau-Harrison, K.; Rochette, A. Impacts of Wheelchair Acquisition on Children from a Person-Occupation-Environment Interactional Perspective. Disabil. Rehabil. Assist. Technol. 2013, 8, 1–10. [Google Scholar] [CrossRef]
- Bloemen, M.A.; Verschuren, O.; van Mechelen, C.; Borst, H.E.; de Leeuw, A.J.; van der Hoef, M.; de Groot, J.F. Personal and Environmental Factors to Consider When Aiming to Improve Participation in Physical Activity in Children with Spina Bifida: A Qualitative Study. BMC Neurol. 2015, 15, 11. [Google Scholar] [CrossRef]
- Rodby-Bousquet, E.; Paleg, G.; Casey, J.; Wizert, A.; Livingstone, R. Physical Risk Factors Influencing Wheeled Mobility in Children with Cerebral Palsy: A Cross-Sectional Study. BMC Pediatr. 2016, 16, 165. [Google Scholar] [CrossRef]
- Daoust, G.; Rushton, P.W.; Demers, L. Bridging the Gap in Wheelchair Skills Testing and Training in a Canadian Paediatric Rehabilitation Context; Oceania Seating Symposium: Melbourne, Australia, 2019. [Google Scholar]
- Palisano, R.J.; Tieman, B.L.; Walter, S.D.; Bartlett, D.J.; Rosenbaum, P.L.; Russell, D.; Hanna, S.E. Effect of Environmental Setting on Mobility Methods of Children with Cerebral Palsy. Dev. Med. Child Neurol. 2003, 45, 113–120. [Google Scholar] [CrossRef]
- Evans, S.; Neophytou, C.; de Souza, L.; Frank, A.O. Young People’s Experiences Using Electric Powered Indoor—Outdoor Wheelchairs (EPIOCs): Potential for Enhancing Users’ Development? Disabil. Rehabil. 2007, 29, 1281–1294. [Google Scholar] [CrossRef]
- Barnard, A.M.; Nelson, N.G.; Xiang, H.; McKenzie, L.B. Pediatric Mobility Aid-Related Injuries Treated in US Emergency Departments from 1991 to 2008. Pediatrics 2010, 125, 1200–1207. [Google Scholar] [CrossRef]
- Tu, C.-J.; Liu, L.; Wang, W.; Du, H.-P.; Wang, Y.-M.; Xu, Y.-B.; Li, P. Effectiveness and Safety of Wheelchair Skills Training Program in Improving the Wheelchair Skills Capacity: A Systematic Review. Clin. Rehabil. 2017, 31, 1573–1582. [Google Scholar] [CrossRef]
- Keeler, L.; Kirby, R.L.; Parker, K.; McLean, K.D.; Hayden, J.A. Effectiveness of the Wheelchair Skills Training Program: A Systematic Review and Meta-Analysis. Disabil. Rehabil. Assist. Technol. 2019, 14, 391–409. [Google Scholar] [CrossRef]
- Smith, E.M.; Sakakibara, B.M.; Miller, W.C. A Review of Factors Influencing Participation in Social and Community Activities for Wheelchair Users. Disabil. Rehabil. Assist. Technol. 2016, 11, 361–374. [Google Scholar] [CrossRef]
- Sawatzky, B.; Rushton, P.W.; Denison, I.; McDonald, R. Wheelchair Skills Training Programme for Children: A Pilot Study. Aust. Occup. Ther. J. 2012, 59, 2–9. [Google Scholar] [CrossRef]
- Sol, M.E.; Verschuren, O.; Horemans, H.; Westers, P.; Visser-Meily, J.M.A.; De Groot, J.F. The Effects of Wheelchair Mobility Skills and Exercise Training on Physical Activity, Fitness, Skills and Confidence in Youth Using a Manual Wheelchair. Disabil. Rehabil. 2021, 44, 4398–4407. [Google Scholar] [CrossRef]
- Kenyon, L.K.; Hesse, E.N.; Pakkala, K.J.; Vanderest, S. Outcomes of a Child-Based Manual Wheelchair Skills Peer Training Program: An Exploratory Case Report. Disabil. Rehabil. Assist. Technol. 2021, 1–5. [Google Scholar] [CrossRef]
- Gowran, R.J.; Collins, M.B.; McGlanaghy, J.; Shanahan, E.; Cleary, Y. Wheelchair Skills Education and Training for Children with Spina Bifida and/or Hydrocephalus and Their Parents: A Pilot Study. Disabilities 2022, 2, 96–118. [Google Scholar] [CrossRef]
- Kenyon, L.K.; Hostnik, L.; McElroy, R.; Peterson, C.; Farris, J.P. Power Mobility Training Methods for Children: A Systematic Review. Pediatr. Phys. Ther. 2018, 30, 2–8. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines on the Provision of Manual Wheelchairs in Less Resourced Settings; World Health Organization (WHO): Geneva, Switzerland, 2008.
- Best, K.L.; Routhier, F.; Miller, W.C. A Description of Manual Wheelchair Skills Training: Current Practices in Canadian Rehabilitation Centers. Disabil. Rehabil. Assist. Technol. 2015, 10, 393–400. [Google Scholar] [CrossRef]
- Kenyon, L.K.; Jones, M.; Livingstone, R.; Breaux, B.; Tsotsoros, J.; Williams, K.M. Power Mobility for Children: A Survey Study of American and Canadian Therapists’ Perspectives and Practices. Dev. Med. Child Neurol. 2018, 60, 1018–1025. [Google Scholar] [CrossRef]
- Kirby, R.L.; Smith, C.; Parker, K.; Han, L.; Theriault, C.J.; Doucette, S.P. Practices and Views of Occupational Therapists in Nova Scotia Regarding Wheelchair-Skills Training for Clients and Their Caregivers: An Online Survey. Disabil. Rehabil. Assist. Technol. 2020, 15, 773–780. [Google Scholar] [CrossRef]
- Lau, H.; Tam, E.W.C.; Cheng, J.C.Y. An Experience on Wheelchair Bank Management. Disabil. Rehabil. Assist. Technol. 2008, 3, 302–308. [Google Scholar] [CrossRef]
- Best, K.L.; Arbour-Nicitopoulos, K.P.; Sweet, S.N. Community-Based Physical Activity and Wheelchair Mobility Programs for Individuals with Spinal Cord Injury in Canada: Current Reflections and Future Directions. J. Spinal Cord Med. 2017, 40, 777–782. [Google Scholar] [CrossRef]
- Giesbrecht, E.; Faieta, J.; Best, K.; Routhier, F.; Miller, W.C.; Laberge, M. Impact of the TEAM Wheels eHealth Manual Wheelchair Training Program: Study Protocol for a Randomized Controlled Trial. PLoS ONE 2021, 16, e0258509. [Google Scholar] [CrossRef]
- Best, K.L.; Miller, W.C.; Huston, G.; Routhier, F.; Eng, J.J. Pilot Study of a Peer-Led Wheelchair Training Program to Improve Self-Efficacy Using a Manual Wheelchair: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2016, 97, 37–44. [Google Scholar] [CrossRef]
- Miller, W.C.; Best, K.L.; Eng, J.J.; Routhier, F. Influence of Peer-Led Wheelchair Training on Wheelchair Skills and Participation in Older Adults: Clinical Outcomes of a Randomized Controlled Feasibility Trial. Arch. Phys. Med. Rehabil. 2019, 100, 1023–1031. [Google Scholar] [CrossRef]
- Beaudoin, M.; Best, K.L.; Raymond, É.; Routhier, F. Influence of Roulez Avec Confiance, a Peer-Led Community-Based Wheelchair Skills Training Program, on Manual Wheelchair Users. Disabil. Rehabil. Assist. Technol. 2021, 1–8. [Google Scholar] [CrossRef]
- Kirby, R.L.; Rushton, P.W.; Smith, C.; Routhier, F.; Best, K.L.; Boyce, J.; Cowan, R.; Giesbrecht, E.M.; Kenyon, L.K.; Koontz, A.; et al. Wheelchair Skills Program Manual Version 5.0; Dalhousie University: Halifax, NS, Canada, 2019. [Google Scholar]
- Kim, J.; Kim, J.; Ko, E. The Effect of the Action Observation Physical Training on the Upper Extremity Function in Children with Cerebral Palsy. J. Exerc. Rehabil. 2014, 10, 176–183. [Google Scholar] [CrossRef]
- Buccino, G.; Arisi, D.; Gough, P.; Aprile, D.; Ferri, C.; Serotti, L.; Tiberti, A.; Fazzi, E. Improving Upper Limb Motor Functions through Action Observation Treatment: A Pilot Study in Children with Cerebral Palsy: Action Observation Treatment in CP. Dev. Med. Child Neurol. 2012, 54, 822–828. [Google Scholar] [CrossRef]
- Mohammadi, Z.; Hajloo, N.; Seifi-Skishahr, F. The Effect of Reciprocal Imitation Training on the Function of Upper Limbs and Motor Skills of Children with Cerebral Palsy. Int. J. Mot. Control Learn. 2021, 3, 25–31. [Google Scholar] [CrossRef]
- Field, D.A.; Miller, W.C. The Wheelchair Outcome Measure for Young People (WhOM-YP): Modification and Metrics for Children and Youth with Mobility Limitations. Disabil. Rehabil. Assist. Technol. 2020, 17, 192–200. [Google Scholar] [CrossRef]
- Miller, W.C.; Garden, J.; Mortenson, W.B. Measurement Properties of the Wheelchair Outcome Measure in Individuals with Spinal Cord Injury. Spinal Cord 2011, 49, 995–1000. [Google Scholar] [CrossRef]
- Kirby, R.L.; Dupuis, D.J.; MacPhee, A.H.; Coolen, A.L.; Smith, C.; Best, K.L.; Newton, A.M.; Mountain, A.D.; MacLeod, D.A.; Bonaparte, J.P. The Wheelchair Skills Test (Version 2.4): Measurement Properties. Arch. Phys. Med. Rehabil. 2004, 85, 794–804. [Google Scholar] [CrossRef]
- Kirby, R.L.; Rushton, P.W.; Smith, C.; Routhier, F.; Archambault, P.S.; Axelson, P.W.; Best, K.L.; Betz, K.; Burrola-Mendez, Y.; Contepomi, S.; et al. Wheelchair Skills Program Manual: Version 5.2; Dalhousie University: Halifax, NS, Canada, 2021. [Google Scholar]
- Huegel, M.; Otieno, S.; Kenyon, L.K. Validity of the WST and the WST-Q in Children with Spina Bifida: A Pilot Project. Disabil. Rehabil. Assist. Technol. 2019, 14, 744–750. [Google Scholar] [CrossRef]
- Rushton, P.W.; Kirby, R.L.; Miller, W.C. Manual Wheelchair Skills: Objective Testing versus Subjective Questionnaire. Arch. Phys. Med. Rehabil. 2012, 93, 2313–2318. [Google Scholar] [CrossRef]
- Rushton, P.; Miller, W.; Kirby, R.; Eng, J. Measure for the Assessment of Confidence with Manual Wheelchair Use (WheelCon-M) Version 2.1: Reliability and Validity. J. Rehabil. Med. 2013, 45, 61–67. [Google Scholar] [CrossRef]
- Rushton, P.W.; Routhier, F.; Miller, W.C. Measurement Properties of the WheelCon for Powered Wheelchair Users. Disabil. Rehabil. Assist. Technol. 2018, 13, 614–619. [Google Scholar] [CrossRef]
- Noguchi, K.; Gel, Y.R.; Brunner, E.; Konietschke, F. NparLD: An R Software Package for the Nonparametric Analysis of Longitudinal Data in Factorial Experiments. J. Stat. Softw. 2012, 50, 1–23. [Google Scholar] [CrossRef]
- Vargha, A.; Delaney, H.D. A Critique and Improvement of the “CL” Common Language Effect Size Statistics of McGraw and Wong. J. Educ. Behav. Stat. 2000, 25, 101–132. [Google Scholar]
- Novak, I.; Honan, I. Effectiveness of Paediatric Occupational Therapy for Children with Disabilities: A Systematic Review. Aust. Occup. Ther. J. 2019, 66, 258–273. [Google Scholar] [CrossRef]
- Kenny, S.; Gowran, R.J. Outcome Measures for Wheelchair and Seating Provision: A Critical Appraisal. Br. J. Occup. Ther. 2014, 77, 67–77. [Google Scholar] [CrossRef]
- King, G.; Chiarello, L.A.; Ideishi, R.; D’Arrigo, R.; Smart, E.; Ziviani, J.; Pinto, M. The Nature, Value, and Experience of Engagement in Pediatric Rehabilitation: Perspectives of Youth, Caregivers, and Service Providers. Dev. Neurorehabilit. 2020, 23, 18–30. [Google Scholar] [CrossRef]
- King, G.; Williams, L.; Goldberg, S.H. Family-Oriented Services in Pediatric Rehabilitation: A Scoping Review and Framework to Promote Parent and Family Wellness: Family-Oriented Services. Child Care Health Dev. 2017, 43, 334–347. [Google Scholar] [CrossRef]
- Lopes, P.B.; Shikako-Thomas, K.; Cardoso, R.; Matsukura, T.S. Social Participation: The Perspectives of Adolescents with Cerebral Palsy and Their Mothers. Int. J. Dev. Disabil. 2021, 67, 263–272. [Google Scholar] [CrossRef]
- Michelsen, S.I.; Flachs, E.M.; Uldall, P.; Eriksen, E.L.; McManus, V.; Parkes, J.; Parkinson, K.N.; Thyen, U.; Arnaud, C.; Beckung, E.; et al. Frequency of Participation of 8–12-Year-Old Children with Cerebral Palsy: A Multi-Centre Cross-Sectional European Study. Eur. J. Paediatr. Neurol. 2009, 13, 165–177. [Google Scholar] [CrossRef]
- Mei, C.; Reilly, S.; Reddihough, D.; Mensah, F.; Green, J.; Pennington, L.; Morgan, A.T. Activities and Participation of Children with Cerebral Palsy: Parent Perspectives. Disabil. Rehabil. 2015, 37, 2164–2173. [Google Scholar] [CrossRef]
- Piškur, B.; Beurskens, A.J.; Jongmans, M.J.; Ketelaar, M.; Norton, M.; Frings, C.A.; Hemmingsson, H.; Smeets, R.J. Parents’ Actions, Challenges, and Needs While Enabling Participation of Children with a Physical Disability: A Scoping Review. BMC Pediatr. 2012, 12, 177. [Google Scholar] [CrossRef]
- Standal, Ø.F.; Jespersen, E. Peers as Resources for Learning: A Situated Learning Approach to Adapted Physical Activity in Rehabilitation. Adapt. Phys. Act. Q. 2008, 25, 208–227. [Google Scholar] [CrossRef]
- Ginis, K.A.M.; Nigg, C.R.; Smith, A.L. Peer-Delivered Physical Activity Interventions: An Overlooked Opportunity for Physical Activity Promotion. Behav. Med. Pract. Policy Res. 2013, 3, 434–443. [Google Scholar] [CrossRef]
- Pellichero, A.; Best, K.L.; Routhier, F.; Miller, W.C. Exploring Older Adults’ Experiences and Perceptions with a Peer-Led Wheelchair Training Program. Can. J. Occup. Ther. 2020, 87, 192–199. [Google Scholar] [CrossRef]
- Sakakibara, B.M.; Miller, W.C.; Eng, J.J.; Backman, C.L.; Routhier, F. Influences of Wheelchair-Related Efficacy on Life-Space Mobility in Adults Who Use a Wheelchair and Live in the Community. Phys. Ther. 2014, 94, 1604–1613. [Google Scholar] [CrossRef]
- Lindquist, N.J.; Loudon, P.E.; Magis, T.F.; Rispin, J.E.; Kirby, R.L.; Manns, P.J. Reliability of the Performance and Safety Scores of the Wheelchair Skills Test Version 4.1 for Manual Wheelchair Users. Arch. Phys. Med. Rehabil. 2010, 91, 1752–1757. [Google Scholar] [CrossRef]
- Sol, M.E.; Bloemen, M.A.T.; Verschuren, O.; Rushton, P.W.; Visser-Meily, J.M.A.; de Groot, J.F. Wheelchair Mobility Confidence Scale for Dutch Youth Using a Manual Wheelchair. Disabil. Rehabil. Assist. Technol. 2020, 15, 684–691. [Google Scholar] [CrossRef]
- Daoust, G.; Rushton, P.W.; Racine, M.; Leduc, K.; Assila, N.; Demers, L. Adapting the Wheelchair Skills Program for Pediatric Rehabilitation: Recommendations from Key Stakeholders. BMC Pediatr. 2021, 21, 103. [Google Scholar] [CrossRef]

| N = 8 | Median (IQR) 1 | Frequency (%) |
|---|---|---|
| Age (years) | 10 (2.5) | |
| Sex (male) | 7 (87.5) | |
| Diagnoses: | ||
| Cerebral palsy | 4 (50) | |
| Spina Bifida | 4 (50) | |
| WC 2 Type: | ||
| Manual WC | 4 (50) | |
| Power WC | 4 (50) | |
| Previous Experience | 7.5 (4) | |
| Daily WC use (hours): | ||
| >8 | 3 (37.5) | |
| 5–8 | 2 (25) | |
| 2–5 | 2 (25) | |
| <2 | 1 (12.5) | |
| WC use: | ||
| Everywhere | 7 (87.5) | |
| School | 1 (12.5) | |
| Accidents in Past Years | 2 (25) | |
| Previous WC Training | 6 (75) | |
| Used Other Devices | 7 (87.5) |
| Children Goals | Parent Goals |
|---|---|
| Get in/out of the house independently | Clean room |
| Stay on footpath outside | Transfer |
| Pop a wheelie at grandparents’ house | Help mother with baking |
| Chase sisters and cousins | Get a drink from the fridge |
| Get to/from school | Brush teeth independently |
| Access a local park | Participate in physical education |
| Feed rabbit | Get on the floor at Lego club |
| Wash hands independently |
| Outcome Measure | T1 Median (IQR) | T2 Median (IQR) | T1 RTE 1 | T2 RTE | p-Value | Adjusted p-Value |
|---|---|---|---|---|---|---|
| WhOM-YP; (out of 10) | 3.6 (2.4) | 5.8 (1.5) | 0.34 | 0.66 | 0.006 | * 0.02 |
| WST (%) | 33.9 (24.5) | 55.5 (14.6) | 0.38 | 0.62 | 0.002 | * 0.02 |
| WST-Q—Parent (%) | 67.3 (17.9) | 70.0 (14.6) | 0.45 | 0.55 | 0.07 | 0.13 |
| WheelCon (%) | 64.7 (13.1) | 79.4 (16.6) | 0.38 | 0.62 | 0.01 | * 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ouellet, B.; Best, K.L.; Wilson, D.; Miller, W.C. Exploring the Influence of a Community-Based Peer-Led Wheelchair Skills Training on Satisfaction with Participation in Children and Adolescents with Cerebral Palsy and Spina Bifida: A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 11908. https://doi.org/10.3390/ijerph191911908
Ouellet B, Best KL, Wilson D, Miller WC. Exploring the Influence of a Community-Based Peer-Led Wheelchair Skills Training on Satisfaction with Participation in Children and Adolescents with Cerebral Palsy and Spina Bifida: A Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(19):11908. https://doi.org/10.3390/ijerph191911908
Chicago/Turabian StyleOuellet, Béatrice, Krista L. Best, Deb Wilson, and William C. Miller. 2022. "Exploring the Influence of a Community-Based Peer-Led Wheelchair Skills Training on Satisfaction with Participation in Children and Adolescents with Cerebral Palsy and Spina Bifida: A Pilot Study" International Journal of Environmental Research and Public Health 19, no. 19: 11908. https://doi.org/10.3390/ijerph191911908
APA StyleOuellet, B., Best, K. L., Wilson, D., & Miller, W. C. (2022). Exploring the Influence of a Community-Based Peer-Led Wheelchair Skills Training on Satisfaction with Participation in Children and Adolescents with Cerebral Palsy and Spina Bifida: A Pilot Study. International Journal of Environmental Research and Public Health, 19(19), 11908. https://doi.org/10.3390/ijerph191911908








