Awareness of Alcohol and Cancer Risk and the California Proposition 65 Warning Sign Updates: A Natural Experiment
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Items
2.1.1. Outcomes: Knowledge of Alcohol and Cancer Association
2.1.2. Locations for Comparison
2.1.3. Alcohol Consumption
2.1.4. Covariates
2.1.5. Statistical Analyses
3. Results
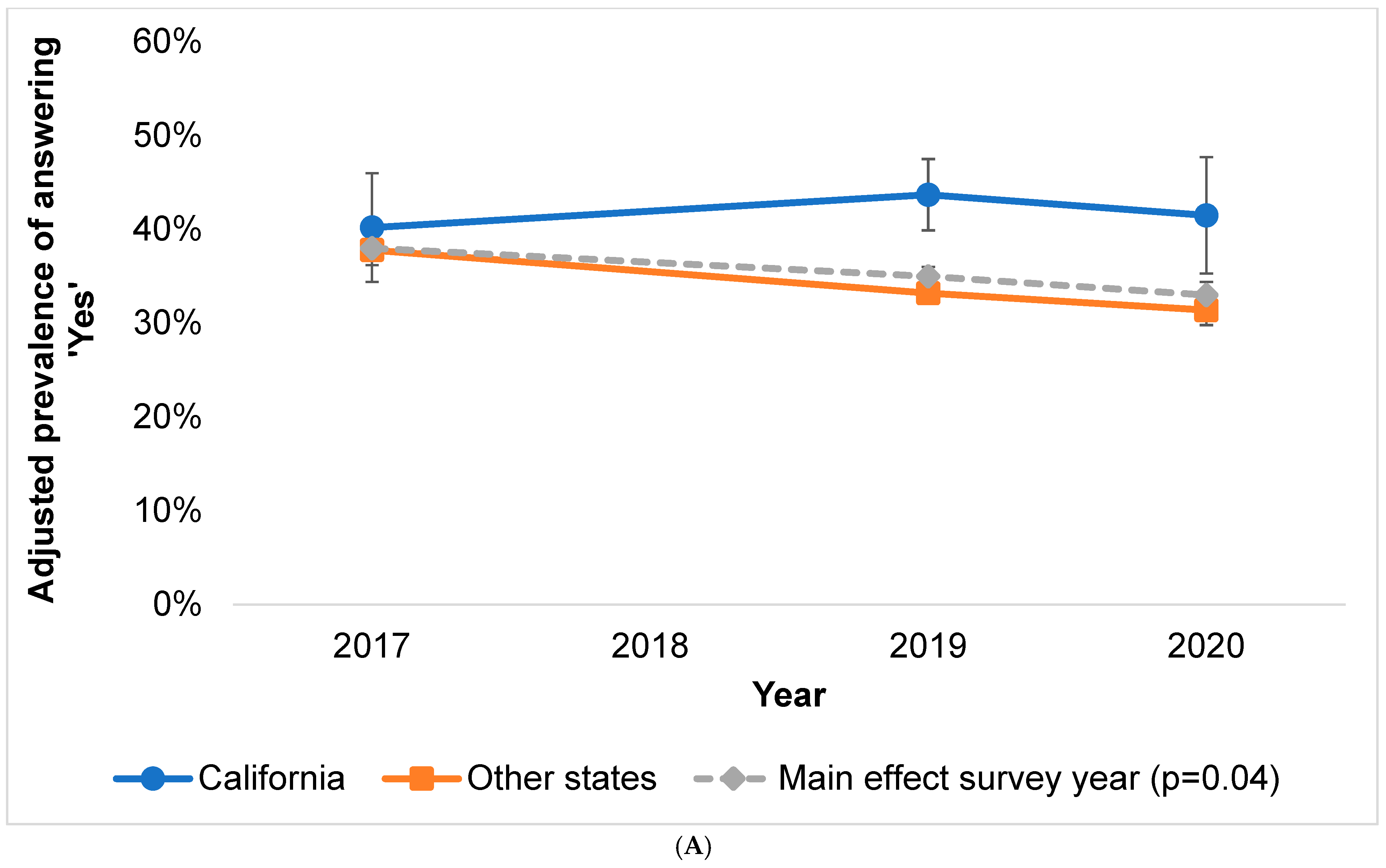
3.1. Alcohol/Cancer Knowledge Levels by Location and Year
3.1.1. Location
3.1.2. Survey Year
3.1.3. Interaction between Location and Year
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Esser, M.B.; Sherk, A.; Liu, Y.; Naimi, T.S.; Stockwell, T.; Stahre, M.; Kanny, D.; Landen, M.; Saitz, R.; Brewer, R.D. Deaths and Years of Potential Life Lost from Excessive Alcohol Use—United States, 2011–2015. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Bagnardi, V.; Rota, M.; Botteri, E.; Tramacere, I.; Islami, F.; Fedirko, V.; Scotti, L.; Jenab, M.; Turati, F.; Pasquali, E.; et al. Alcohol consumption and site-specific cancer risk: A comprehensive dose-response meta-analysis. Br. J. Cancer 2015, 112, 580–593. [Google Scholar] [CrossRef] [PubMed]
- Rumgay, H.; Shield, K.; Charvat, H.; Ferrari, P.; Sornpaisarn, B.; Obot, I.; Islami, F.; Lemmens, V.; Rehm, J.; Soerjomataram, I. Global burden of cancer in 2020 attributable to alcohol consumption: A population-based study. Lancet Oncol. 2021, 22, 1071–1080. [Google Scholar] [CrossRef]
- Goding Sauer, A.; Fedewa, S.A.; Bandi, P.; Minihan, A.K.; Stoklosa, M.; Drope, J.; Gapstur, S.M.; Jemal, A.; Islami, F. Proportion of cancer cases and deaths attributable to alcohol consumption by US state, 2013–2016. Cancer Epidemiol. 2021, 71, 101893. [Google Scholar] [CrossRef]
- Islami, F.; Goding Sauer, A.; Miller, K.D.; Siegel, R.L.; Fedewa, S.A.; Jacobs, E.J.; McCullough, M.L.; Patel, A.V.; Ma, J.; Soerjomataram, I.; et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J. Clin. 2018, 68, 31–54. [Google Scholar] [CrossRef]
- Wiseman, K.P.; Klein, W.M.P. Evaluating Correlates of Awareness of the Association between Drinking Too Much Alcohol and Cancer Risk in the United States. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1195–1201. [Google Scholar] [CrossRef] [PubMed]
- AICR. 2019. Available online: https://www.aicr.org/assets/can-prevent/docs/2019-Survey.pdf (accessed on 12 September 2021).
- Bates, S.; Holmes, J.; Gavens, L.; de Matos, E.G.; Li, J.; Ward, B.; Hooper, L.; Dixon, S.; Buykx, P. Awareness of alcohol as a risk factor for cancer is associated with public support for alcohol policies. BMC Public Health 2018, 18, 688. [Google Scholar] [CrossRef] [PubMed]
- Seidenberg, A.B.; Wiseman, K.P.; Eck, R.H.; Blake, K.D.; Platter, H.N.; Klein, W.M.P. Awareness of Alcohol as a Carcinogen and Support for Alcohol Control Policies. Am. J. Prev. Med. 2021, 62, 174–182. [Google Scholar] [CrossRef]
- Cil, G. Effects of posted point-of-sale warnings on alcohol consumption during pregnancy and on birth outcomes. J. Health Econ. 2017, 53, 131–155. [Google Scholar] [CrossRef]
- Greenfield, T.K.; Graves, K.L.; Kaskutas, L.A. Long-term effects of alcohol warning labels: Findings from a comparison of the United States and Ontario, Canada. Psychol. Mark. 1999, 16, 261–282. [Google Scholar] [CrossRef]
- Wilkinson, C.; Room, R. Warnings on alcohol containers and advertisements: International experience and evidence on effects. Drug Alcohol Rev. 2009, 28, 426–435. [Google Scholar] [CrossRef] [PubMed]
- Louise, J.; Eliott, J.; Olver, I.; Braunack-Mayer, A. Mandatory cancer risk warnings on alcoholic beverages: What are the ethical issues? Am. J. Bioeth. 2015, 15, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.C.M.; Mericle, A.A.; Subbaraman, M.S.; Thomas, S.; Treffers, R.D.; Delucchi, K.L.; Kerr, W.C. State Policies Targeting Alcohol Use during Pregnancy and Alcohol Use among Pregnant Women 1985–2016: Evidence from the Behavioral Risk Factor Surveillance System. Women’s Health Issues 2019, 29, 213–221. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, D.P.; Williams-Avery, R.M.; Wilcox, K.L.; Fenaughty, A.M. Effects of the Arizona alcohol warning poster. J. Public Policy Mark. 1999, 18, 77–88. [Google Scholar] [CrossRef]
- Scully, M.; Morley, B.; Wakefield, M.; Dixon, H. Can point-of-sale nutrition information and health warnings encourage reduced preference for sugary drinks?: An experimental study. Appetite 2020, 149, 104612. [Google Scholar] [CrossRef]
- Coady, M.H.; Chan, C.A.; Auer, K.; Farley, S.M.; Kilgore, E.A.; Kansagra, S.M. Awareness and impact of New York City’s graphic point-of-sale tobacco health warning signs. Tob. Control 2013, 22, e51–e56. [Google Scholar] [CrossRef]
- Kim, A.; Nonnemaker, J.; Guillory, J.; Shafer, P.; Parvanta, S.; Holloway, J.; Farrelly, M. Antismoking Ads at the Point of Sale: The Influence of Ad Type and Context on Ad Reactions. J. Health Commun. 2017, 22, 477–487. [Google Scholar] [CrossRef]
- Li, L.; Borland, R.; Yong, H.H.; Hitchman, S.C.; Wakefield, M.A.; Kasza, K.A.; Fong, G.T. The association between exposure to point-of-sale anti-smoking warnings and smokers’ interest in quitting and quit attempts: Findings from the International Tobacco Control Four Country Survey. Addiction 2012, 107, 425–433. [Google Scholar] [CrossRef]
- OEHHA. Proposition 65. 2020. Available online: https://oehha.ca.gov/proposition-65#:~:text%20=%20Proposition%2065%2C (accessed on 12 September 2021).
- Nelson, D.E.; Kreps, G.L.; Hesse, B.W.; Croyle, R.T.; Willis, G.; Arora, N.K.; Rimer, B.K.; Viswanath, K.V.; Weinstein, N.; Alden, S. The Health Information National Trends Survey (HINTS): Development, design, and dissemination. J. Health Commun. 2004, 9, 443–460; discussion 81–84. [Google Scholar] [CrossRef]
- Finney Rutten, L.J.; Blake, K.D.; Skolnick, V.G.; Davis, T.; Moser, R.P.; Hesse, B.W. Data Resource Profile: The National Cancer Institute’s Health Information National Trends Survey (HINTS). Int. J. Epidemiol. 2020, 49, 17-17j. [Google Scholar] [CrossRef]
- Rehm, J.; Gmel, G.E., Sr.; Gmel, G.; Hasan, O.S.M.; Imtiaz, S.; Popova, S.; Probst, C.; Roerecke, M.; Room, R.; Samokhvalov, A.V.; et al. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction 2017, 112, 968–1001. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. Dietary Guidelines for Americans, 8th ed. Available online: https://health.gov/our-work/nutrition-physical-activity/dietary-guidelines/previous-dietary-guidelines/2015 (accessed on 12 September 2021).
- Census Bureau. Quick Facts: 2019. United States. Available online: https://www.census.gov/quickfacts/fact/table/US/PST045219 (accessed on 12 September 2019).
- Hobin, E.; Schoueri-Mychasiw, N.; Weerasinghe, A.; Vallance, K.; Hammond, D.; Greenfield, T.K.; McGavock, J.; Paradis, C.; Stockwell, T. Effects of strengthening alcohol labels on attention, message processing, and perceived effectiveness: A quasi-experimental study in Yukon, Canada. Int. J. Drug Policy 2020, 77, 102666. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Billich, N.; George, N.A.; Blake, M.R.; Huse, O.; Backholer, K.; Boelsen-Robinson, T.; Peeters, A. The effect of front-of-package labels or point-of-sale signage on consumer knowledge, attitudes and behavior regarding sugar-sweetened beverages: A systematic review. Nutr. Rev. 2021, 79, 1165–1181. [Google Scholar] [CrossRef]
- Dutra, L.M.; Nonnemaker, J.; Guillory, J.; Bradfield, B.; Taylor, N.; Kim, A. Smokers’ Attention to Point-of-Sale Antismoking Ads: An Eye-tracking Study. Tob. Regul. Sci. 2018, 4, 631–643. [Google Scholar] [CrossRef]
- SAMHSA. 2019 National Survey on Drug Use and Health (NSDUH) Table 2.1B. 2019. Available online: https://www.samhsa.gov/data/sites/default/files/reports/rpt29394/NSDUHDetailedTabs2019/NSDUHDetTabsSect2pe2019.htm#tab2-1b (accessed on 12 September 2021).
- WHO. Global Status Report on Alcohol and Health 2018; WHO: Geneva, Switzerland, 2018; Available online: https://apps.who.int/iris/handle/10665/274603 (accessed on 12 September 2021).
- Al-Hamdani, M.; Smith, S.M. Alcohol health-warning labels: Promises and challenges. J. Public Health 2017, 39, 3–5. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hay, J.L.; Orom, H.; Kiviniemi, M.T.; Waters, E.A. “I don’t know” my cancer risk: Exploring deficits in cancer knowledge and information-seeking skills to explain an often-overlooked participant response. Med. Decis. Mak. 2015, 35, 436–445. [Google Scholar] [CrossRef]
- Waters, E.A.; Kiviniemi, M.T.; Orom, H.; Hay, J.L. “I don’t know” My Cancer Risk: Implications for Health Behavior Engagement. Ann. Behav. Med. 2016, 50, 784–788. [Google Scholar] [CrossRef]
- Krosnick, J.A. Response strategies for coping with the cognitive demands of attitude measures in surveys. Appl. Cogn. Psychol. 1991, 5, 213–236. [Google Scholar] [CrossRef]
- Czajka, J.L.; Beyler, A. Declining Response Rates in Federal Surveys: Trends and Implications. Math. Policy Res. 2016, 1, 1–86. [Google Scholar]
- Maitland, A.; Lin, A.; Cantor, D.; Jones, M.; Moser, R.P.; Hesse, B.W.; Davis, T.; Blake, K.D. A Nonresponse Bias Analysis of the Health Information National Trends Survey (HINTS). J. Health Commun. 2017, 22, 545–553. [Google Scholar] [CrossRef]
- Weerasinghe, A.; Schoueri-Mychasiw, N.; Vallance, K.; Stockwell, T.; Hammond, D.; McGavock, J.; Greenfield, T.K.; Paradis, C.; Hobin, E. Improving Knowledge that Alcohol Can Cause Cancer is Associated with Consumer Support for Alcohol Policies: Findings from a Real-World Alcohol Labelling Study. Int. J. Environ. Res. Public Health 2020, 17, 398. [Google Scholar] [CrossRef] [PubMed]

| HINTS Sample | California | Other States | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Years | 2017 | 2019 | 2020 | 2017 | 2019 | 2020 | ||||||||
| N | % a | N | % a | N | % a | N | % a | N | % a | N | % a | N | % a | |
| Total | 10,562 | - | 348 | - | 612 | - | 471 | - | 2394 | - | 3867 | - | 2870 | - |
| Aware of relationship between alcohol and cancer | ||||||||||||||
| Yes | 3671 | 35.0 | 145 | 42.4 | 248 | 46.0 | 171 | 42.5 | 886 | 37.9 | 1358 | 32.9 | 863 | 30.9 |
| No | 2304 | 23.8 | 94 | 24.8 | 158 | 26.6 | 82 | 16.1 | 537 | 26.0 | 890 | 26.4 | 543 | 19.7 |
| Don’t know | 4587 | 41.2 | 109 | 32.9 | 206 | 27.3 | 218 | 41.4 | 971 | 36.1 | 1619 | 40.7 | 1464 | 49.3 |
| Gender | ||||||||||||||
| Male | 4472 | 49.6 | 151 | 47.7 | 259 | 47.0 | 205 | 55.4 | 996 | 50.4 | 1659 | 49.7 | 1202 | 48.6 |
| Female | 6090 | 50.4 | 197 | 52.3 | 353 | 53.0 | 266 | 44.6 | 1398 | 49.6 | 2208 | 50.3 | 1668 | 51.4 |
| Age | ||||||||||||||
| 18–39 | 2090 | 32.9 | 80 | 44.0 | 158 | 35.7 | 88 | 34.6 | 440 | 30.1 | 766 | 32.1 | 558 | 34.0 |
| 40–59 | 3581 | 40.9 | 141 | 36.2 | 202 | 42.7 | 163 | 40.3 | 856 | 43.5 | 1289 | 41.6 | 930 | 38.5 |
| 60+ | 4891 | 26.2 | 127 | 19.8 | 252 | 21.6 | 220 | 25.1 | 1098 | 26.4 | 1812 | 26.3 | 1382 | 27.5 |
| Education | ||||||||||||||
| High school or less | 2409 | 28.7 | 75 | 29.5 | 123 | 25.5 | 116 | 25.5 | 566 | 28.4 | 845 | 28.6 | 684 | 29.7 |
| Post high school/some college | 3117 | 37.8 | 120 | 29.4 | 188 | 39.4 | 131 | 39.1 | 702 | 34.5 | 1129 | 40.2 | 847 | 39.4 |
| College graduate or more | 5036 | 33.5 | 153 | 41.1 | 301 | 35.1 | 224 | 35.4 | 1126 | 37.1 | 1893 | 31.2 | 1339 | 30.9 |
| Race | ||||||||||||||
| Black/African American | 1535 | 11.4 | 26 | 5.1 | 54 | 6.3 | 42 | 8.3 | 365 | 11.6 | 589 | 12.2 | 459 | 12.5 |
| White | 7991 | 78.3 | 233 | 71.8 | 439 | 69.6 | 336 | 71.9 | 1834 | 79.8 | 2989 | 80.0 | 2160 | 78.2 |
| Other/multiple | 1036 | 10.3 | 89 | 23.1 | 119 | 24.1 | 93 | 19.8 | 195 | 8.7 | 289 | 7.8 | 251 | 9.3 |
| Hispanic ethnicity | ||||||||||||||
| Hispanic | 1514 | 15.4 | 95 | 37.8 | 167 | 31.7 | 140 | 37.5 | 265 | 11.2 | 447 | 13.4 | 400 | 13.2 |
| Not Hispanic | 9048 | 84.6 | 253 | 62.2 | 445 | 68.3 | 331 | 62.5 | 2129 | 88.8 | 3420 | 86.6 | 2470 | 86.8 |
| Sexual orientation | ||||||||||||||
| Heterosexual | 10,118 | 95.2 | 330 | 93.3 | 569 | 89.7 | 449 | 94.9 | 2304 | 95.4 | 3725 | 96.2 | 2741 | 95.1 |
| Homosexual/gay/lesbian | 253 | 2.7 | 12 | 4.4 | 25 | 6.7 | 13 | 2.9 | 51 | 3.0 | 90 | 1.9 | 62 | 2.4 |
| Bisexual | 191 | 2.1 | 6 | 2.3 | 18 | 3.6 | 9 | 2.2 | 39 | 1.6 | 52 | 1.9 | 67 | 2.6 |
| History of cancer | ||||||||||||||
| Yes | 1680 | 8.9 | 42 | 6.1 | 75 | 6.2 | 71 | 8.9 | 381 | 9.0 | 640 | 9.4 | 471 | 8.9 |
| No | 8882 | 91.1 | 306 | 93.9 | 537 | 93.8 | 400 | 91.1 | 2013 | 91.0 | 3227 | 90.6 | 2399 | 91.1 |
| Family cancer history | ||||||||||||||
| Yes | 7668 | 70.5 | 232 | 61.1 | 449 | 70.1 | 321 | 62.9 | 1753 | 71.4 | 2802 | 70.7 | 2111 | 71.9 |
| No | 2211 | 22.5 | 95 | 30.4 | 125 | 23.3 | 112 | 28.2 | 526 | 23.0 | 813 | 22.2 | 540 | 20.4 |
| Not sure | 683 | 7.0 | 21 | 8.4 | 38 | 6.6 | 38 | 8.9 | 115 | 5.6 | 252 | 7.1 | 219 | 7.8 |
| Smoking/e-cigarette use | ||||||||||||||
| Current smoker/user | 1421 | 17.4 | 35 | 14.3 | 67 | 12.0 | 46 | 11.2 | 355 | 18.6 | 525 | 16.1 | 393 | 19.3 |
| Not current smoker/user | 9141 | 82.6 | 313 | 85.7 | 545 | 88.0 | 425 | 88.8 | 2039 | 81.4 | 3342 | 83.9 | 2477 | 80.7 |
| Total HINTS Sample | California | Other States | ||||
|---|---|---|---|---|---|---|
| N | % a (SE) b | N | % a (SE) | N | % a (SE) | |
| Non-drinking | 1631 | 48.2 (1.8) | 220 | 50.7 (5.0) | 1411 | 47.9 (1.8) |
| Some drinking | 834 | 23.8 (1.2) | 125 | 24.3 (3.8) | 709 | 23.7 (1.3) |
| Risky drinking | 671 | 22.8 (1.0) | 91 | 17.4 (3.3) | 580 | 23.5 (1.1) |
| Missing | 205 | 5.1 (0.6) | 35 | 7.6 (2.2) | 170 | 4.8 (0.6) |
| Yes | No | Don’t Know | |
|---|---|---|---|
| Adjusted Prevalence (%) (95% CI) | Adjusted Prevalence (%) (95% CI) | Adjusted Prevalence (%) (95% CI) | |
| Survey year | |||
| 2017 | 38.0 (34.6–41.6) | 35.9 (32.8–39.1) | 26.1 (23.4–28.9) |
| 2019 | 34.5 (32.5–36.5) | 39.1 (36.7–41.5) | 26.4 (23.9–29.1) |
| 2020 | 32.6 (29.8–35.5) | 19.3 (17.1–21.8) | 48.1 (45.2–50.9) |
| Location | |||
| California | 41.6 (35.5–48.0) | 26.7 (22.6–31.3) | 31.7 (26.8–36.9) |
| Other states | 34.1 (32.4–35.7) | 31.8 (30.2–33.4) | 34.1 (32.4–35.9) |
| History of cancer | |||
| Yes | 37.2 (33.1–41.4) | 28.8 (25.5–32.4) | 34.0 (30.2–38.1) |
| No | 34.8 (33.1–36.5) | 31.4 (29.9–33.0) | 33.8 (32.1–35.5) |
| Family cancer history | |||
| Yes | 36.2 (34.1–38.3) | 31.1 (29.3–33.0) | 32.7 (30.8–34.6) |
| No | 33.9 (30.7–37.2) | 30.9 (27.6–34.5) | 35.2 (31.7–38.8) |
| Not sure | 26.3 (19.7–34.2) | 32.9 (26.7–39.8) | 40.8 (33.2–48.9) |
| Gender | |||
| Male | 35.7 (33.2–38.3) | 30.8 (28.4–33.4) | 33.5 (30.9–36.2) |
| Female | 34.3 (32.2–36.4) | 31.6 (29.7–33.4) | 34.2 (32.3–36.0) |
| Cigarette/e-cigarette use | |||
| Current smoker/user | 31.3 (27.7–35.2) | 32.0 (27.8–36.7) | 36.7 (31.9–41.6) |
| Not current smoker/user | 35.8 (33.9–37.7) | 31.0 (29.4–32.7) | 33.2 (31.5–35.0) |
| Age group | |||
| 18–39 | 38.8 (35.2–42.4) | 25.0 (21.4–28.9) | 36.3 (32.8–39.9) |
| 40–59 | 34.4 (31.9–36.9) | 32.7 (30.6–34.9) | 32.9 (30.3–35.6) |
| 60+ | 31.2 (29.1–33.3) | 36.5 (34.2–38.8) | 32.3 (30.3–34.5) |
| Education | |||
| High school degree or less | 29.4 (26.4–32.6) | 33.1 (30.2–36.0) | 37.6 (34.4–40.8) |
| Post high school/some college | 34.1 (31.0–37.4) | 32.0 (29.3–34.7) | 33.9 (31.1–36.9) |
| College graduate or more | 40.5 (38.1–43.0) | 28.8 (26.7–31.0) | 30.6 (28.4–32.9) |
| Race | |||
| White | 34.8 (33.0–36.6) | 31.4 (29.8–33.1) | 33.8 (32.0–35.6) |
| Black/African American | 29.2 (25.4–33.3) | 32.8 (28.7–37.1) | 38.1 (33.4–43.0) |
| Other/multiple | 42.8 (37.4–48.4) | 27.7 (23.7–32.1) | 29.5 (25.2–34.2) |
| Hispanic ethnicity | |||
| Hispanic | 33.3 (29.0–37.8) | 32.1 (28.2–36.3) | 34.6 (30.2–39.4) |
| Not Hispanic | 35.3 (33.6–37.1) | 31.0 (29.4–32.7) | 33.7 (31.9–35.4) |
| Sexual orientation | |||
| Heterosexual | 34.7 (33.0–36.4) | 31.4 (29.9–33.0) | 33.9 (32.3–35.5) |
| Homosexual/gay/lesbian | 41.1 (32.1–50.6) | 25.6 (17.4–36.0) | 33.3 (23.5–44.8) |
| Bisexual | 40.8 (29.3–53.5) | 26.7 (14.8–43.2) | 32.5 (19.5–48.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Budenz, A.; Moser, R.P.; Eck, R.; Agurs-Collins, T.; McNeel, T.S.; Klein, W.M.P.; Berrigan, D. Awareness of Alcohol and Cancer Risk and the California Proposition 65 Warning Sign Updates: A Natural Experiment. Int. J. Environ. Res. Public Health 2022, 19, 11862. https://doi.org/10.3390/ijerph191911862
Budenz A, Moser RP, Eck R, Agurs-Collins T, McNeel TS, Klein WMP, Berrigan D. Awareness of Alcohol and Cancer Risk and the California Proposition 65 Warning Sign Updates: A Natural Experiment. International Journal of Environmental Research and Public Health. 2022; 19(19):11862. https://doi.org/10.3390/ijerph191911862
Chicago/Turabian StyleBudenz, Alexandra, Richard P. Moser, Raimee Eck, Tanya Agurs-Collins, Timothy S. McNeel, William M. P. Klein, and David Berrigan. 2022. "Awareness of Alcohol and Cancer Risk and the California Proposition 65 Warning Sign Updates: A Natural Experiment" International Journal of Environmental Research and Public Health 19, no. 19: 11862. https://doi.org/10.3390/ijerph191911862
APA StyleBudenz, A., Moser, R. P., Eck, R., Agurs-Collins, T., McNeel, T. S., Klein, W. M. P., & Berrigan, D. (2022). Awareness of Alcohol and Cancer Risk and the California Proposition 65 Warning Sign Updates: A Natural Experiment. International Journal of Environmental Research and Public Health, 19(19), 11862. https://doi.org/10.3390/ijerph191911862








